Abstract
Accurate prediction of lymph node (LN) status is crucially important for appropriate treatment planning in patients with early gastric cancer (EGC). However, consensus on patient and tumor characteristics associated with LN metastasis are yet to be reached. Through systematic search, we identified several independent variables associated with LN metastasis in EGC, which should be included in future research to assess which of these variables remain as significant predictors of LN metastasis. On the other hand, even if we use these promising parameters, we should realize the limitation and the difficulty of predicting LN metastasis accurately. The sentinel LN (SLN) is defined as first possible site to receive cancer cells along the route of lymphatic drainage from the primary tumor. The absence of metastasis in SLN is believed to correlate with the absence of metastasis in downstream LNs. In this review, we have attempted to focus on several independent parameters which have close relationship between tumor and LN metastasis in EGC. In addition, we evaluated the history of sentinel node navigation surgery and the usefulness for EGC.
Keywords: Early-stage gastric cancer, Sentinel node navigation surgery, Prediction of lymph node metastasis
Core tip: In this review, we have attempted to focus on several independent parameters which have close relationship between tumor and lymph node metastasis in early gastric cancer. In addition, we evaluated the usefulness of sentinel node navigation surgery (SNNS) for patients with gastric cancer, in particular technical procedure of SNNS using Infrared Ray Electronic Endoscopes combined with Indocyanine Green injection.
INTRODUCTION
Newly developing patients with gastric cancer are estimated as 951000 per year and is the fifth most common cancer in the world[1]. The chance of detecting early gastric cancer (EGC) is increasing especially in South Korea and Japan thanks to development in function of endoscopy and the national screening systems[2-5]. In Japan and South Korea, patients with EGC has been blessed with superior prognosis after surgical treatment[5]. In general, lymph node (LN) metastasis in patients with EGC has been reported about 10%-15%, and it is one of the strongest prognostic parameters[1,6-8]. Gastrectomy with D2 lymphadenectomy is recognized as a standard surgical procedure for patients with advanced gastric cancer according to the Dutch trial[9]. Standard D2 lymphadenectomy is appropriate procedure for patients with advanced gastric cancer. On the other hand, more limited lymphadenectomy such as D1 or D1+ for patients with EGC is also available according to the Japanese Gastric Cancer Association[10]. The relationship between pathological parameters and LN metastasis for patients with EGC has been deeply inquired. Meanwhile, the connection between preoperative parameters and LN metastasis of EGC has not been fully investigated[11-14]. Furthermore, the involvement between preoperative and postoperative diagnostic parameters has not been widely evaluated.
The “less invasive” theory behind sentinel LN (SLN) biopsy concept has benefits based on the limitation of morbidity because of avoiding unnecessary LN dissection. At least theoretically, combination of SLN and less invasive surgical procedures such as laparoscopic surgery seems attractive. SNNS has potential to change the current surgical treatment of gastric cancer.
The aim of this review is to clarify the reliability of preoperative prediction of LN metastasis for patients with EGC and evaluate the clinical usefulness of SNNS.
PREOPERATIVE PREDICTION OF LN METASTASIS OF EGC
Mönig et al[15] investigated 1253 LNs of 31 specimens and reported that the mean diameter of the LNs which is negative for metastasis was 4.1 mm. On the contrary, mean diameter of LNs which is positive for metastasis was 6.0 mm. Eighty percent of LNs which is negative for metastasis were less than 5 mm in diameter. However 55% of LNs which is positive for metastasis were less than 5 mm in diameter. In addition, 71% of patients who had LN metastasis had at least one node that was 10 mm or greater in diameter. Furthermore, 70% of patients who were free for LN metastasis had at least one node that was 10 mm or greater in diameter. According to these results, they concluded that size of LN is not a reliable parameter for LN metastasis in patients with gastric cancer. In this point, prediction of LN metastasis using CT can’t be trustworthy examination for ECG. Fluorodeoxyglucose positron emission tomography (FDG-PET) and EUS are alternative methods for detecting LN metastasis. FDG-PET is a useful preoperative diagnostic instrument to investigate metastasis. However, it has been reported that FDG-PET is not reliable tool to predict LN metastasis because of the low sensitivity[16-18]. In addition, accuracy of prediction for LN presence by EUS was only 64%[19]. These reports suggest that FDG-PET and EUS are not credible tool to predict LN metastasis up to now. Nakagawa et al[20] analyzed 1042 patients with EGC who underwent gastrectomy with standard LN dissection. They constructed two receiver operating characteristics (ROC) curves consisting of postoperative independent factors and preoperative independent factors to predict LN metastasis. Comparing with areas produced by the two ROC curves, they investigated which is more reliable factors to predict LN metastasis. As a result, produced areas under the ROC curve made of postoperative parameters including pathological data was 0.824. However, the area under the ROC curve made of preoperative factors obtained from CT or endoscopic examination was 0.660. Hence, they concluded that prediction of LN metastasis for EGC using preoperative parameters is not credible as compared with using postoperative factors[20].
RELATIONSHIP BETWEEN PATHOLOGICAL PARAMETERS AND LN METASTASIS
Many studies have been carried out to evaluate relationship between pathological parameters and LN metastasis in EGC. We have surveyed numerous published articles which describe an association between pathological parameters and LN metastasis in EGC after year 2001. From these articles, we selected 28 articles (Table 1), which investigated relationships between pathological risk factors and LN metastasis in EGC at least using multiple variate analysis. Song et al[21] have demonstrated that increased submucosal vascularity, histological differentiation, invasion of tumor cells into the muscularis mucosae had significant relation to LN metastasis in intramucosal gastric carcinoma. Depth of tumor invasion and tumor size had also significant correlation with LN metastasis in EGC[22]. Furthermore, An et al[6] also demonstrated that lymphatic system invasion and tumor size had strong relationship to LN metastasis in submucosa invading EGC with submucosal invasion. Of the 28 articles, 23 (82.1%) authors concluded lymphatic invasion or lymphovascular invasion as independent risk factors for LN metastasis and tumor depth and tumor size were also confirmed as LN risk factors in 17 (60.7%) articles, respectively. These results are suggesting that lymphovascular invasion, tumor depth and tumor size are strong predictors of LN metastasis for EGC. Furthermore, Fujii et al[23] described that lymphatic invasion and absence of clear lymphoid follicle formation at the site of submucosal invasion (lymphocystic infiltration) were independent risk factors for LN metastasis. Immunohistochemical (IH) research is also useful for predicting LN metastasis. Yi Kim et al[24] demonstrated that abnormal expression of E-cadherin and lymphatic invasion were independent, statistically significant parameters which is associated with LN metastasis for patients with EGC. Recently, Park et al[25] revealed not only larger tumor size (greater than 2 cm), deeper level of submucosal invasion, lymphovascular invasion but also Epstein-Barr virus negativity were independent risk factors for LNM in submucosa invaded EGC using a large series (n = 756) of patients with EGC. In addition, Amioka et al[26] investigated clinicopathological relationship between Vascular Endothelial Growth Factor (VEGF) - C expression in submucosa-invading gastric carcinoma and LN metastasis. They demonstrated VEGF-C expression in submucosa-invading gastric carcinoma had significant correlation to LN metastasis.
Table 1.
Published articles which refer to independent risk factors for lymph node metastasis of early gastric cancer after 2001
| Ref. | Year | Country | Number of patients | Independent parameters which affect LN metastasis | Odds ratio | 95%CI |
| Folli et al[40] | 2001 | Japan | m: 285, sm: 215 | Tumor size | 1.34 | 1.13-1.59 |
| Tumor depth (pT1b vs pT1a) | 2.29 | 1.56-3.36 | ||||
| Histological differentiation (Diffuse vs Intestinal) | 5.70 | 2.88-11.31 | ||||
| Histological differentiation (Mixed vs Intestinal) | 4.19 | 1.89-9.32 | ||||
| Kodama Type (Pen A vs Not Pen A) | 1.36 | 1.17-1.58 | ||||
| Amioka et al[26] | 2002 | Japan | sm: 139 | Lymphatic invasion | 3.48 | 1.17-10.40 |
| VEGF-C (positive vs negative) | 4.18 | 1.38-12.70 | ||||
| Abe et al[41] | 2002 | Japan | m: 136, sm: 178 | Gender (female vs male) | 3.23 | 1.33-7.88 |
| Tumor size (≥ 20 mm vs < 20 mm) | 3.39 | 1.26-9.13 | ||||
| Tumor depth (pT1b vs pT1a) | 4.94 | 1.49-16.27 | ||||
| Lymphovascular invasion | 7.54 | 3.01-19.04 | ||||
| Matsuzaki et al[42] | 2003 | Japan | sm: 92 | Volume of lesions | 1.27 | 2.49-13.51 |
| Abe et al[43] | 2003 | Japan | sm: 104 | Gender (female vs male) | 2.90 | 1.2-6.9 |
| Tumor depth (pT1b vs pT1a) | 29.20 | 3.9-216.3 | ||||
| Lymphatic invasion | 50.80 | 8.1-317.3 | ||||
| Song et al[21] | 2004 | South Korea | m: 120 | Lymphatic invasion | 21.39 | 10.41-43.95 |
| Tumor depth (sm massive vs sm shallow) | 2.56 | 1.30-5.03 | ||||
| Park et al[22] | 2004 | South Korea | sm: 105 | Tumor size (> 40 mm) | 4.80 | 1.05-22.06 |
| Tumor depth (> 2000 μm) | 6.81 | 1.36-34.17 | ||||
| Hyung et al[44] | 2004 | South Korea | m: 295, sm: 271 | Histological differentiation (Undifferentiated vs Differentiated) | 2.28 | 1.14-4.56 |
| Tumor size (≥ 20 mm vs < 20 mm) | 1.045 | 1.36-5.93 | ||||
| Tumor depth (pT1b vs pT1a) | 3.68 | 1.67-8.13 | ||||
| Lymphovascular invasion | 26.56 | 12.77-55.23 | ||||
| Son et al[45] | 2005 | South Korea | sm: 248 | Lymphatic invasion | 21.39 | 10.41-43.96 |
| Tumor depth (sm massive vs sm shallow) | 2.56 | 1.30-5.03 | ||||
| Lo et al[46] | 2007 | Taiwan | m: 272, sm: 203 | Lymphovascular invasion | 8.61 | 4.43-16.72 |
| Tumor depth (pT1b vs pT1a) | 3.05 | 1.47-6.33 | ||||
| Tumor size | 1.68 | 1.13-2.51 | ||||
| Kunisaki et al[47] | 2007 | Japan | sm: 615 | Tumor size (40 mm < 80 mm vs < 20 mm) | 2.71 | 1.31-5.61 |
| Tumor size (≥ 80 mm vs < 20 mm) | 3.20 | 1.02-10.09 | ||||
| Lymphatic invasion | 15.92 | 9.52-26.63 | ||||
| An et al[6] | 2007 | South Korea | sm: 1043 | Tumor size (20 mm < 40 mm vs < 10 mm) | 1.88 | 1.03-3.45 |
| Tumor size (≥ 40 mm vs < 10 mm) | 1.96 | 1.34-2.88 | ||||
| Lymphatic invasion | 8.41 | 5.76-12.29 | ||||
| Yi Kim et al[24] | 2007 | South Korea | m: 9, sm: 51 | Lymphatic invasion | 8.11 | 1.61-40.77 |
| E-Cadherin (abnormal expression vs normal expression) | 2.62 | 0.917-7.457 | ||||
| Li et al[48] | 2008 | South Korea | m: 356, sm: 270 | Tumor size (≥ 20 mm vs < 20 mm) | 2.04 | 1.12-3.73 |
| Tumor depth (pT1b vs pT1a) | 2.84 | 1.48-5.44 | ||||
| Lymphovascular invasion | 15.11 | 7.41-30.80 | ||||
| Park et al[49] | 2008 | South Korea | Only poorly diff. | Tumor depth (500-1000 μm invasion to submucosa) | 14.69 | 2.54-85.09 |
| adenocarcinoma | Tumor depth (1000-2000 μm invasion to submucosa) | 6.20 | 1.57-24.52 | |||
| m: 118, sm: 116 | Tumor depth (> 2000 μm invasion to submucosa) | 6.37 | 1.35-30.14 | |||
| Tumor size (> 30 mm in diameter ) | 4.53 | 1.13-18.20 | ||||
| Lymphovascular invasion | 12.63 | 4.05-39.37 | ||||
| Shen et al[50] | 2009 | China | sm: 144 | Histological differentiation (Undifferentiated vs Differentiated) | 2.70 | 1.18-6.17 |
| Tumor size (≥ 20 mm vs < 20 mm) | 2.93 | 1.32-6.54 | ||||
| Morita et al[51] | 2009 | Japan | sm: 70 | Tumor size | 1.04 | 1.01-1.08 |
| Lymphatic invasion | 5.22 | 1.84-20.74 | ||||
| VEGF-C (positive vs negative) | 3.31 | 1.00-0.95 | ||||
| Kunisaki et al[52] | 2009 | Japan | m: 269, sm: 304 | Tumor size (≥ 20 mm vs < 20 mm) | 3.34 | 1.39-8.01 |
| Tumor depth (SM1 vs M) | 2.96 | 1.03-8.52 | ||||
| Tumor depth (SM2 vs M) | 4.53 | 1.69-12.18 | ||||
| Lymphovascular invasion | 9.37 | 4.78-18.37 | ||||
| Sung et al[53] | 2010 | Taiwan | m: 293, sm: 263 | Tumor size (≥ 2 mm in diameter vs < 2 cm) | 2.28 | 1.20-4.17 |
| Lymphatic invasion | 27.20 | 10.3-74.8 | ||||
| Tumor depth (pT1b vs pT1a) | 4.91 | 2.44-9.89 | ||||
| Lee et al[54] | 2010 | South Korea | m: 39, sm: 85 | Lymphatic invasion | 15.33 | 5.06-46.44 |
| Tumor size (≥ 30 mm vs < 30 mm) | 4.16 | 1.52-11.45 | ||||
| Tumor depth (M/SM1 vs SM2/SM3) | 3.11 | 1.21-7.98 | ||||
| Intratumoral vessel density | 3.57 | 1.20-10.64 | ||||
| Lim et al[55] | 2011 | South Korea | sm: 163 | Lymphovascular invasion | 4.57 | 1.74-12.24 |
| Macroscopic type (elevated vs flat) | 9.09 | 1.75-50.0 | ||||
| Macroscopic type (elevated vs depressed) | 5.89 | 1.69-20.0 | ||||
| Macroscopic type (elevated vs mixed) | 20.00 | 0.00-2.70 | ||||
| Lee et al[56] | 2012 | South Korea | Only poorly diff. | Tumor size (≥ 20 mm vs < 20 mm) | 2.47 | 1.39-4.40 |
| adenocarcinoma | Tumor depth (pT1b vs pT1a) | 2.42 | 1.46-3.99 | |||
| m: 510, sm: 495 | Lymphatic invasion | 6.50 | 4.14-10.19 | |||
| Ren et al[57] | 2013 | China | m: 122, sm: 80 | Tumor depth (pT1b vs pT1a) | 2.74 | 2.32-3.17 |
| Fujii et al[23] | 2013 | Japan | sm: 130 | Lymphatic invasion | 8.07 | NA |
| Lymphocytic infiltration (absent vs present) | 7.94 | NA | ||||
| Shida et al[27] | 2014 | Japan | sm: 145 | Lymphatic invasion | 3.11 | 1.71-5.67 |
| Vascular invasion | 2.44 | 1.05-5.67 | ||||
| Lee et al[12] | 2015 | South Korea | m: 847 | Tumor size | 1.36 | 1.10-1.69 |
| Lymphovascular invasion | 27.52 | 7.40-102.20 | ||||
| Ulceration (present vs absent) | 7.54 | 1.90-29.90 | ||||
| Undifferntiated type of component (present vs absent) | 4.39 | 1.08-17.89 | ||||
| Park et al[25] | 2015 | South Korea | sm: 756 | Tumor size (≥ 2 cm in diameter vs < 2 cm) | 1.57 | 1.04-2.36 |
| Tumor depth (sm2 vs sm1) | 2.96 | 1.55-5.64 | ||||
| Tumor depth (sm3 vs sm1) | 2.91 | 1.61-5.29 | ||||
| Lymphovascular invasion, | 7.45 | 4.93-11.25 | ||||
| Negative for EB virus | 4.24 | 1.26-14.32 | ||||
| Feng et al[58] | 2016 | China | m: 339, sm: 237 | Tumor depth | 2.94 | 1.82-4.77 |
| Ulceration (present vs absent) | 2.55 | 1.21-5.38 | ||||
| Lymphovascular invasion | 4.40 | 1.19-16.3 |
LN METASTASIS PREDICTING SCORE
One hundred forty-five consecutive patients with submucosa-invaded EGC were analyzed using multivariate analysis, and a formula which predicts LN metastasis was developed by linear discriminant analysis. Additionally, prospective validation study was carried out to estimate if the formula is reliable to predict LN metastasis. Lymphatic system invasion and venous system invasion were selected as independent parameters correlated with LN metastasis for EGC. The LN metastasis predicting formula was developed using these two factors by linear discriminant analysis. The formula is as follows: Y = 0.12 × (venous system invasion: 0, 1, 2 or 3) + 0.19 × (lymphatic system invasion: 0, 1, 2, or 3) - 0.14. If Y > 0, we judge that a patient with gastric cancer is susceptible LN metastasis. Prospective study demonstrated that sensitivity and specificity rates of this formula were 70% and 61.6%, respectively[27]. Flow chart for submucosa-invading gastric cancer after ESD is shown in Figure 1. This flow chart is indicating that if resected tumor through ESD invaded 500 μm below the muscularis mucosae, the LN metastasis predicting score is available. Y > 0 indicates that the tumor in question would be prone to LN metastasis. We defined patients who are satisfied with Y > 0 as a high-risk group (HRG) for LN metastasis and Y < 0 patients as a low-risk group (LRG) for LN metastasis. The flow chart means patients with HRG should undergo additional conventional gastrectomy. However, we think that less invasive treatment like as SNNS is more desirable for patients with LRG.
Figure 1.
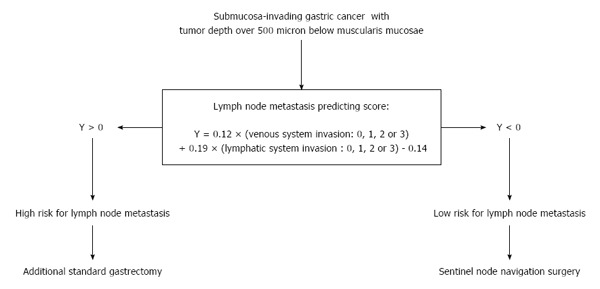
Flow chart for submucosa-invading gastric cancer after ESD. Quoted from Prediction of lymph node metastasis in patients with submucosa-invading early gastric cancer. Adapted from Ref. [27].
Fujii et al[23] investigated 130 submucosa-invaded gastric cancer. Absence of lymphoid infiltration and lymphatic system invasion were selected as independent significant factors which affect LN metastasis. They also developed LN metastasis predicting score and advocated a scoring system for additional gastrectomy following ESD based on prediction of LN metastasis (Figure 2). Lymphoid infiltration and the presence of lymphatic system invasion were scored as follows: +2 for lymphatic system invasion and -2 for involvement of lymphocystic infiltration, which was considered as a LN metastasis-inhibiting parameter. Next five pathological factors [minor axis length ≥ 2 cm, submucosal invasion depth ≥ 2000 μm, histological classification (undifferentiated) of submucosal cancer at the site of invasion, ulceration or scar in the lesion, and venous invasion] were scored +1 each when present. They concluded that a patient with total score 3 and more should be treated as high risk for LN metastasis and such patients are recommended to undergo additional gastrectomy. On the other hand, patients with total score less than 3 should be considered as low risk for LN metastasis and they don’t need to undergo additional gastrectomy.
Figure 2.
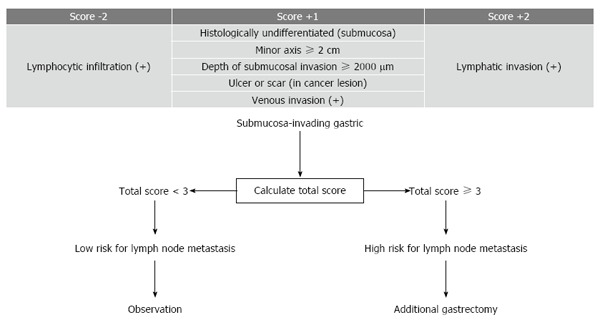
Scoring to predict lymph node metastasis and scoring system for additional gastrectomy following endoscopic resection based on prediction of lymph node metastasis. Quoted from Pathological factors related to lymph node metastasis of submucosally invasive gastric cancer: criteria for additional gastrectomy after endoscopic resection. Adapted from Ref. [23].
These predictive scores and treatment of flow chart after ESD seem innovative and original strategy for EGC. However, we need further additional clinical trials to validate clinical usefulness of the flow charts.
SNNS AS A SOLUTION TO PREDICT LN METASTASIS OF EGC
In spite of these constant efforts to predict LN metastasis using pathological parameters, it has been still difficult to predict LN metastasis accurately. Meanwhile, SNNS for EGC may become another possible and promising solution to resolve this problem. From early 2000s, articles which focused on SNNS for EGC have been published. Hiratsuka et al[28] demonstrated the usefulness of indocyanine green (ICG) for SNNS in particular T1 gastric cancer because of the high successful rate to predict SLNs. Kitagawa et al[29] showed the effectiveness of radio-guided surgery using gamma detection probe technology for SNNS. Technetium-99m-radiolabelled tin colloid was injected endoscopically before the surgery, and radioactive SNs were identified with a gamma probe. They concluded that the radioisotope is useful even for obese patients because it remains for enough time in the SNs after injection. In addition, Miwa et al[30] demonstrated the results of a regional multicenter clinical trial of SN mapping for gastric cancer using the dye-guided method. This was the first multicenter trial of SN mapping for gastric cancer. Miwa demonstrated that sentinel lymphatic basins contain truly positive nodes, even in cases with a false negative SN biopsy. Hence, they concluded that the sentinel lymphatic basins dissection are adequate procedure for LN dissection in patients with EGC.
We have reported the clinical usefulness of infrared ray electronic endoscopy (IREE) combined with ICG to detect illuminated SLN in patients with gastric cancer and duodenal tumors as compared with dye alone (Figure 3)[31-37]. Infrared ray has a wave length of around 805 nm. It is able to penetrate fatty tissues up to a depth from 3 to 5 mm. In brief, before the ICG injection, the gastrocolic ligament is opened using ultrasonic coagulation incision device without disrupting the gastro-epiploic vessels. After that 0.5 mL ICG (5 mg/mL; Diagnogreen; Daiichi Phar- maceutical, Tokyo, Japan) is injected endoscopically in four points of the submucosa surrounding the tumor with an endoscopic puncture needle. Twenty minutes after the injection, SN’s stained with ICG were observed with the naked eye and with IREE (Olympus Optical, Tokyo, Japan).
Figure 3.
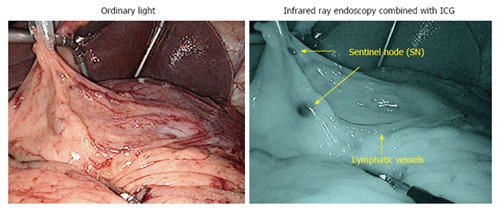
Sentinel node navigation surgery using infrared ray electronic endoscopy. ICG: Indocyanine green.
Nimura et al[31] reported SNNS for gastric cancer by IREE with ICG injection for the first time. They investigated 84 patients with gastric cancer and 11 of the 84 patients had LN metastasis. All of the 11 patients were detected by IREE with ICG injection. However, SLNs detected by ICG injection alone did not include metastasis in 4 of the 11 patients. This result seems to support the usefulness of IREE with ICG injection as compared to ICG injection alone. In addition, Kelder et al[33] investigated 212 patients with gastric cancer who underwent SNNS by IREE with ICG injection. The detection rate and sensitivity of SLNs by IREE with ICG injection were 99.5% and 97%, respectively. Meanwhile, those of SLNs with ICG injection alone were 85.8% and 48.4%. Predominance of SLNs by IREE with ICG injection over ICG injection alone is supported by these results.
Ohdaira et al[32] focused on lymphatic drainage using IREE with ICG. One of the advantage of this procedure is that SNNS by IREE with ICG injection enables us to detect lymphatic vessels from the tumor easily. They investigated 161 patients with gastric cancer using IREE with ICG and revealed that the most common locations of the SNs, in each of the upper, middle and lower thirds of the stomach, were station No. 7 which is defined as LNs along the trunk of left gastric artery between its root and the origin of its ascending branch by Japanese Gastric Cancer Association. Yano et al[34] investigated 130 patients with gastric cancer (3381 LNs) who underwent SNNS by IREE with ICG injection and evaluated LNs by immunohistochemistry (IH) with anti-cytokeratin antibody staining. They reported that 15 patients (27 nodes) were diagnosed without metastasis by hematoxylin and eosin (HE) staining, which turned to metastatic by IH staining. However, all the 27 nodes with micrometastasis were inside the lymphatic basins. They concluded that even if LN micrometastasis is overlooked by intraoperative frozen section with HE staining, micrometastasis can be completely removed by lymphatic basins dissection.
Benefit of SNNS is not only to avoid unnecessary LN dissection but also to enable us performing local resection (LR) of stomach for patients with EGC with curability. Kitaoka et al[38], was the first to report the use of LR for treating early gastric cancer. Maintenance of curability and quality of life are essential to introducing LR for early gastric cancer clinically. Kawamura et al[39] described the usefulness of partial resection of stomach as compared to conventional gastrectomy. They assessed gastric emptying by 13C-acetate breath test in 60 patients who underwent distal gastrectomy with Billroth I reconstruction (DGBI) in 26 patients, LR in 34 patients. For the 13C breath test, 100 mg of 13C-acetate sodium salt was mixed in a test meal. Dietary intake and body weight change were significantly more reduced in the DGBI group than the LR group. In addition, significant acceleration of gastric emptying was observed in the DGBI group compared to that in the LR group by 13C breath test. They concluded that LR is an option for selected patients with EGC.
SN mapping concept seems reasonable approach to determine appropriate indications including pylorus-preserving gastrectomy, proximal gastrectomy and LR for cT1N0 gastric cancer. In particular, laparoscopic function-preserving surgeries should be performed for patients with negative for LN metastasis confirmed by SNNS. Earlier recovery after surgery and preservation of quality of life in the late disease phases can be achieved by limited laparoscopic gastrectomy with SNNS.
CONCLUSION
When we predict LN metastasis for ECG, we need at least pathological information derived from resected tumor through ESD. In particular, lymphovascular invasion, tumor depth and tumor size are the strongest LN metastasis predicting parameters for EGC. Basic strategy of additional treatment after ESD for patients with EGC is conventional gastrectomy. However, providing less invasive surgery such as SNNS for patients with EGC has potentiality to improve the quality of life of patients after surgery by preserving gastric function as compared to conventional gastrectomy.
Footnotes
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
Conflict-of-interest statement: Authors declare no conflict of interests for this article.
Peer-review started: March 29, 2016
First decision: May 12, 2016
Article in press: July 6, 2016
P- Reviewer: Coccolini F, Ilson DH, Sendur MAN S- Editor: Ma YJ L- Editor: A E- Editor: Ma S
References
- 1.Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136:E359–E386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 2.Hamashima C, Shibuya D, Yamazaki H, Inoue K, Fukao A, Saito H, Sobue T. The Japanese guidelines for gastric cancer screening. Jpn J Clin Oncol. 2008;38:259–267. doi: 10.1093/jjco/hyn017. [DOI] [PubMed] [Google Scholar]
- 3.Choi KS, Jun JK, Lee HY, Park S, Jung KW, Han MA, Choi IJ, Park EC. Performance of gastric cancer screening by endoscopy testing through the National Cancer Screening Program of Korea. Cancer Sci. 2011;102:1559–1564. doi: 10.1111/j.1349-7006.2011.01982.x. [DOI] [PubMed] [Google Scholar]
- 4.Pasechnikov V, Chukov S, Fedorov E, Kikuste I, Leja M. Gastric cancer: prevention, screening and early diagnosis. World J Gastroenterol. 2014;20:13842–13862. doi: 10.3748/wjg.v20.i38.13842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nashimoto A, Akazawa K, Isobe Y, Miyashiro I, Katai H, Kodera Y, Tsujitani S, Seto Y, Furukawa H, Oda I, et al. Gastric cancer treated in 2002 in Japan: 2009 annual report of the JGCA nationwide registry. Gastric Cancer. 2013;16:1–27. doi: 10.1007/s10120-012-0163-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.An JY, Baik YH, Choi MG, Noh JH, Sohn TS, Kim S. Predictive factors for lymph node metastasis in early gastric cancer with submucosal invasion: analysis of a single institutional experience. Ann Surg. 2007;246:749–753. doi: 10.1097/SLA.0b013e31811f3fb7. [DOI] [PubMed] [Google Scholar]
- 7.Roviello F, Rossi S, Marrelli D, Pedrazzani C, Corso G, Vindigni C, Morgagni P, Saragoni L, de Manzoni G, Tomezzoli A. Number of lymph node metastases and its prognostic significance in early gastric cancer: a multicenter Italian study. J Surg Oncol. 2006;94:275–280; discussion 274. doi: 10.1002/jso.20566. [DOI] [PubMed] [Google Scholar]
- 8.Pelz J, Merkel S, Horbach T, Papadopoulos T, Hohenberger W. Determination of nodal status and treatment in early gastric cancer. Eur J Surg Oncol. 2004;30:935–941. doi: 10.1016/j.ejso.2004.07.016. [DOI] [PubMed] [Google Scholar]
- 9.Songun I, Putter H, Kranenbarg EM, Sasako M, van de Velde CJ. Surgical treatment of gastric cancer: 15-year follow-up results of the randomised nationwide Dutch D1D2 trial. Lancet Oncol. 2010;11:439–449. doi: 10.1016/S1470-2045(10)70070-X. [DOI] [PubMed] [Google Scholar]
- 10.Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2010 (ver. 3) Gastric Cancer. 2011;14:113–123. doi: 10.1007/s10120-011-0042-4. [DOI] [PubMed] [Google Scholar]
- 11.Gotoda T, Yanagisawa A, Sasako M, Ono H, Nakanishi Y, Shimoda T, Kato Y. Incidence of lymph node metastasis from early gastric cancer: estimation with a large number of cases at two large centers. Gastric Cancer. 2000;3:219–225. doi: 10.1007/pl00011720. [DOI] [PubMed] [Google Scholar]
- 12.Lee JH, Choi IJ, Han HS, Kim YW, Ryu KW, Yoon HM, Eom BW, Kim CG, Lee JY, Cho SJ, et al. Risk of lymph node metastasis in differentiated type mucosal early gastric cancer mixed with minor undifferentiated type histology. Ann Surg Oncol. 2015;22:1813–1819. doi: 10.1245/s10434-014-4167-7. [DOI] [PubMed] [Google Scholar]
- 13.Kim BS, Oh ST, Yook JH, Kim BS. Signet ring cell type and other histologic types: differing clinical course and prognosis in T1 gastric cancer. Surgery. 2014;155:1030–1035. doi: 10.1016/j.surg.2013.08.016. [DOI] [PubMed] [Google Scholar]
- 14.Son SY, Park JY, Ryu KW, Eom BW, Yoon HM, Cho SJ, Lee JY, Kim CG, Lee JH, Kook MC, et al. The risk factors for lymph node metastasis in early gastric cancer patients who underwent endoscopic resection: is the minimal lymph node dissection applicable? A retrospective study. Surg Endosc. 2013;27:3247–3253. doi: 10.1007/s00464-013-2901-z. [DOI] [PubMed] [Google Scholar]
- 15.Mönig SP, Zirbes TK, Schröder W, Baldus SE, Lindemann DG, Dienes HP, Hölscher AH. Staging of gastric cancer: correlation of lymph node size and metastatic infiltration. AJR Am J Roentgenol. 1999;173:365–367. doi: 10.2214/ajr.173.2.10430138. [DOI] [PubMed] [Google Scholar]
- 16.Dassen AE, Lips DJ, Hoekstra CJ, Pruijt JF, Bosscha K. FDG-PET has no definite role in preoperative imaging in gastric cancer. Eur J Surg Oncol. 2009;35:449–455. doi: 10.1016/j.ejso.2008.11.010. [DOI] [PubMed] [Google Scholar]
- 17.Mochiki E, Kuwano H, Katoh H, Asao T, Oriuchi N, Endo K. Evaluation of 18F-2-deoxy-2-fluoro-D-glucose positron emission tomography for gastric cancer. World J Surg. 2004;28:247–253. doi: 10.1007/s00268-003-7191-5. [DOI] [PubMed] [Google Scholar]
- 18.Mukai K, Ishida Y, Okajima K, Isozaki H, Morimoto T, Nishiyama S. Usefulness of preoperative FDG-PET for detection of gastric cancer. Gastric Cancer. 2006;9:192–196. doi: 10.1007/s10120-006-0374-7. [DOI] [PubMed] [Google Scholar]
- 19.Cardoso R, Coburn N, Seevaratnam R, Sutradhar R, Lourenco LG, Mahar A, Law C, Yong E, Tinmouth J. A systematic review and meta-analysis of the utility of EUS for preoperative staging for gastric cancer. Gastric Cancer. 2012;15 Suppl 1:S19–S26. doi: 10.1007/s10120-011-0115-4. [DOI] [PubMed] [Google Scholar]
- 20.Nakagawa M, Choi YY, An JY, Chung H, Seo SH, Shin HB, Bang HJ, Li S, Kim HI, Cheong JH, et al. Difficulty of predicting the presence of lymph node metastases in patients with clinical early stage gastric cancer: a case control study. BMC Cancer. 2015;15:943. doi: 10.1186/s12885-015-1940-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Song SY, Park S, Kim S, Son HJ, Rhee JC. Characteristics of intramucosal gastric carcinoma with lymph node metastatic disease. Histopathology. 2004;44:437–444. doi: 10.1111/j.1365-2559.2004.01870.x. [DOI] [PubMed] [Google Scholar]
- 22.Park DJ, Lee HK, Lee HJ, Lee HS, Kim WH, Yang HK, Lee KU, Choe KJ. Lymph node metastasis in early gastric cancer with submucosal invasion: feasibility of minimally invasive surgery. World J Gastroenterol. 2004;10:3549–3552. doi: 10.3748/wjg.v10.i24.3549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fujii M, Egashira Y, Akutagawa H, Nishida T, Nitta T, Edagawa G, Kurisu Y, Shibayama Y. Pathological factors related to lymph node metastasis of submucosally invasive gastric cancer: criteria for additional gastrectomy after endoscopic resection. Gastric Cancer. 2013;16:521–530. doi: 10.1007/s10120-012-0215-9. [DOI] [PubMed] [Google Scholar]
- 24.Yi Kim D, Kyoon Joo J, Kyu Park Y, Yeob Ryu S, Soo Kim H, Kyun Noh B, Hwa Lee K, Hyuk Lee J. E-cadherin expression in early gastric carcinoma and correlation with lymph node metastasis. J Surg Oncol. 2007;96:429–435. doi: 10.1002/jso.20732. [DOI] [PubMed] [Google Scholar]
- 25.Park JH, Kim EK, Kim YH, Kim JH, Bae YS, Lee YC, Cheong JH, Noh SH, Kim H. Epstein-Barr virus positivity, not mismatch repair-deficiency, is a favorable risk factor for lymph node metastasis in submucosa-invasive early gastric cancer. Gastric Cancer. 2015 doi: 10.1007/s10120-015-0565-1. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 26.Amioka T, Kitadai Y, Tanaka S, Haruma K, Yoshihara M, Yasui W, Chayama K. Vascular endothelial growth factor-C expression predicts lymph node metastasis of human gastric carcinomas invading the submucosa. Eur J Cancer. 2002;38:1413–1419. doi: 10.1016/s0959-8049(02)00106-5. [DOI] [PubMed] [Google Scholar]
- 27.Shida A, Fujioka S, Kawamura M, Takahashi N, Ishibashi Y, Nakada K, Mitsumori N, Omura N, Yanaga K. Prediction of lymph node metastasis in patients with submucosa-invading early gastric cancer. Anticancer Res. 2014;34:4471–4474. [PubMed] [Google Scholar]
- 28.Hiratsuka M, Miyashiro I, Ishikawa O, Furukawa H, Motomura K, Ohigashi H, Kameyama M, Sasaki Y, Kabuto T, Ishiguro S, et al. Application of sentinel node biopsy to gastric cancer surgery. Surgery. 2001;129:335–340. doi: 10.1067/msy.2001.111699. [DOI] [PubMed] [Google Scholar]
- 29.Kitagawa Y, Fujii H, Mukai M, Kubota T, Otani Y, Kitajima M. Radio-guided sentinel node detection for gastric cancer. Br J Surg. 2002;89:604–608. doi: 10.1046/j.1365-2168.2002.02065.x. [DOI] [PubMed] [Google Scholar]
- 30.Miwa K, Kinami S, Taniguchi K, Fushida S, Fujimura T, Nonomura A. Mapping sentinel nodes in patients with early-stage gastric carcinoma. Br J Surg. 2003;90:178–182. doi: 10.1002/bjs.4031. [DOI] [PubMed] [Google Scholar]
- 31.Nimura H, Narimiya N, Mitsumori N, Yamazaki Y, Yanaga K, Urashima M. Infrared ray electronic endoscopy combined with indocyanine green injection for detection of sentinel nodes of patients with gastric cancer. Br J Surg. 2004;91:575–579. doi: 10.1002/bjs.4470. [DOI] [PubMed] [Google Scholar]
- 32.Ohdaira H, Nimura H, Mitsumori N, Takahashi N, Kashiwagi H, Yanaga K. Validity of modified gastrectomy combined with sentinel node navigation surgery for early gastric cancer. Gastric Cancer. 2007;10:117–122. doi: 10.1007/s10120-007-0419-6. [DOI] [PubMed] [Google Scholar]
- 33.Kelder W, Nimura H, Takahashi N, Mitsumori N, van Dam GM, Yanaga K. Sentinel node mapping with indocyanine green (ICG) and infrared ray detection in early gastric cancer: an accurate method that enables a limited lymphadenectomy. Eur J Surg Oncol. 2010;36:552–558. doi: 10.1016/j.ejso.2010.04.007. [DOI] [PubMed] [Google Scholar]
- 34.Yano K, Nimura H, Mitsumori N, Takahashi N, Kashiwagi H, Yanaga K. The efficiency of micrometastasis by sentinel node navigation surgery using indocyanine green and infrared ray laparoscopy system for gastric cancer. Gastric Cancer. 2012;15:287–291. doi: 10.1007/s10120-011-0105-6. [DOI] [PubMed] [Google Scholar]
- 35.Mitsumori N, Nimura H, Takahashi N. Sentinel node navigation surgery for early malignant tumor of the duodenum. Jikeikai Med J. 2009;56:11–17. [Google Scholar]
- 36.Ryu KW, Eom BW, Nam BH, Lee JH, Kook MC, Choi IJ, Kim YW. Is the sentinel node biopsy clinically applicable for limited lymphadenectomy and modified gastric resection in gastric cancer? A meta-analysis of feasibility studies. J Surg Oncol. 2011;104:578–584. doi: 10.1002/jso.21995. [DOI] [PubMed] [Google Scholar]
- 37.Mitsumori N, Nimura H, Takahashi N, Kawamura M, Aoki H, Shida A, Omura N, Yanaga K. Sentinel lymph node navigation surgery for early stage gastric cancer. World J Gastroenterol. 2014;20:5685–5693. doi: 10.3748/wjg.v20.i19.5685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kitaoka H, Yoshikawa K, Hirota T, Itabashi M. Surgical treatment of early gastric cancer. Jpn J Clin Oncol. 1984;14:283–293. [PubMed] [Google Scholar]
- 39.Kawamura M, Nakada K, Konishi H, Iwasaki T, Murakami K, Mitsumori N, Hanyu N, Omura N, Yanaga K. Assessment of motor function of the remnant stomach by ¹³C breath test with special reference to gastric local resection. World J Surg. 2014;38:2898–2903. doi: 10.1007/s00268-014-2660-6. [DOI] [PubMed] [Google Scholar]
- 40.Folli S, Morgagni P, Roviello F, De Manzoni G, Marrelli D, Saragoni L, Di Leo A, Gaudio M, Nanni O, Carli A, et al. Risk factors for lymph node metastases and their prognostic significance in early gastric cancer (EGC) for the Italian Research Group for Gastric Cancer (IRGGC) Jpn J Clin Oncol. 2001;31:495–499. doi: 10.1093/jjco/hye107. [DOI] [PubMed] [Google Scholar]
- 41.Abe N, Watanabe T, Suzuki K, Machida H, Toda H, Nakaya Y, Masaki T, Mori T, Sugiyama M, Atomi Y. Risk factors predictive of lymph node metastasis in depressed early gastric cancer. Am J Surg. 2002;183:168–172. doi: 10.1016/s0002-9610(01)00860-1. [DOI] [PubMed] [Google Scholar]
- 42.Matsuzaki H, Kikuchi S, Kakita A. Evaluation of the morphology of submucosal tumor invasion and its volume in early gastric cancer. In Vivo. 2003;17:41–44. [PubMed] [Google Scholar]
- 43.Abe N, Sugiyama M, Masaki T, Ueki H, Yanagida O, Mori T, Watanabe T, Atomi Y. Predictive factors for lymph node metastasis of differentiated submucosally invasive gastric cancer. Gastrointest Endosc. 2004;60:242–245. doi: 10.1016/s0016-5107(04)01682-7. [DOI] [PubMed] [Google Scholar]
- 44.Hyung WJ, Cheong JH, Kim J, Chen J, Choi SH, Noh SH. Application of minimally invasive treatment for early gastric cancer. J Surg Oncol. 2004;85:181–185; discussion 186. doi: 10.1002/jso.20018. [DOI] [PubMed] [Google Scholar]
- 45.Son HJ, Song SY, Kim S, Noh JH, Sohn TS, Kim DS, Rhee JC. Characteristics of submucosal gastric carcinoma with lymph node metastatic disease. Histopathology. 2005;46:158–165. doi: 10.1111/j.1365-2559.2005.02049.x. [DOI] [PubMed] [Google Scholar]
- 46.Lo SS, Wu CW, Chen JH, Li AF, Hsieh MC, Shen KH, Lin HJ, Lui WY. Surgical results of early gastric cancer and proposing a treatment strategy. Ann Surg Oncol. 2007;14:340–347. doi: 10.1245/s10434-006-9077-x. [DOI] [PubMed] [Google Scholar]
- 47.Kunisaki C, Akiyama H, Nomura M, Matsuda G, Otsuka Y, Ono HA, Takagawa R, Nagahori Y, Takahashi M, Kito F, et al. Lymph node status in patients with submucosal gastric cancer. Ann Surg Oncol. 2006;13:1364–1371. doi: 10.1245/s10434-006-9061-5. [DOI] [PubMed] [Google Scholar]
- 48.Li C, Kim S, Lai JF, Oh SJ, Hyung WJ, Choi WH, Choi SH, Zhu ZG, Noh SH. Risk factors for lymph node metastasis in undifferentiated early gastric cancer. Ann Surg Oncol. 2008;15:764–769. doi: 10.1245/s10434-007-9707-y. [DOI] [PubMed] [Google Scholar]
- 49.Park YD, Chung YJ, Chung HY, Yu W, Bae HI, Jeon SW, Cho CM, Tak WY, Kweon YO. Factors related to lymph node metastasis and the feasibility of endoscopic mucosal resection for treating poorly differentiated adenocarcinoma of the stomach. Endoscopy. 2008;40:7–10. doi: 10.1055/s-2007-966750. [DOI] [PubMed] [Google Scholar]
- 50.Shen L, Huang Y, Sun M, Xu H, Wei W, Wu W. Clinicopathological features associated with lymph node metastasis in early gastric cancer: analysis of a single-institution experience in China. Can J Gastroenterol. 2009;23:353–356. doi: 10.1155/2009/462678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Morita H, Ishikawa Y, Akishima-Fukasawa Y, Ito K, Akasaka Y, Nishimura C, Igarashi Y, Miki K, Ishii T. Histopathological predictor for regional lymph node metastasis in gastric cancer. Virchows Arch. 2009;454:143–151. doi: 10.1007/s00428-008-0717-3. [DOI] [PubMed] [Google Scholar]
- 52.Kunisaki C, Takahashi M, Nagahori Y, Fukushima T, Makino H, Takagawa R, Kosaka T, Ono HA, Akiyama H, Moriwaki Y, et al. Risk factors for lymph node metastasis in histologically poorly differentiated type early gastric cancer. Endoscopy. 2009;41:498–503. doi: 10.1055/s-0029-1214758. [DOI] [PubMed] [Google Scholar]
- 53.Sung CM, Hsu CM, Hsu JT, Yeh TS, Lin CJ, Chen TC, Su MY, Chiu CT. Predictive factors for lymph node metastasis in early gastric cancer. World J Gastroenterol. 2010;16:5252–5256. doi: 10.3748/wjg.v16.i41.5252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lee K, Park DJ, Choe G, Kim HH, Kim WH, Lee HS. Increased intratumoral lymphatic vessel density correlates with lymph node metastasis in early gastric carcinoma. Ann Surg Oncol. 2010;17:73–80. doi: 10.1245/s10434-009-0707-y. [DOI] [PubMed] [Google Scholar]
- 55.Lim MS, Lee HW, Im H, Kim BS, Lee MY, Jeon JY, Yang DH, Lee BH. Predictable factors for lymph node metastasis in early gastric cancer-analysis of single institutional experience. J Gastrointest Surg. 2011;15:1783–1788. doi: 10.1007/s11605-011-1624-5. [DOI] [PubMed] [Google Scholar]
- 56.Lee JH, Choi MG, Min BH, Noh JH, Sohn TS, Bae JM, Kim S. Predictive factors for lymph node metastasis in patients with poorly differentiated early gastric cancer. Br J Surg. 2012;99:1688–1692. doi: 10.1002/bjs.8934. [DOI] [PubMed] [Google Scholar]
- 57.Ren G, Cai R, Zhang WJ, Ou JM, Jin YN, Li WH. Prediction of risk factors for lymph node metastasis in early gastric cancer. World J Gastroenterol. 2013;19:3096–3107. doi: 10.3748/wjg.v19.i20.3096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Feng H, Wang Y, Cao L, Zhang C, Sun B, Zhao Y, Xu J. Lymph node metastasis in differentiated-type early gastric cancer: a single-center retrospective analysis of surgically resected cases. Scand J Gastroenterol. 2016;51:48–54. doi: 10.3109/00365521.2015.1054425. [DOI] [PubMed] [Google Scholar]


