SUMMARY
There are multiple reasons for the failure to successfully translate new drugs to the clinics. One reason, noted by others, is the lack of reproducibility of studies and the problems with accuracy and rigor. However, another reason for translational failure has not been emphasized by others, i.e., the lack of state-of-the-art cardiovascular measurements, due to effects of anesthesia, lack of direct measurements of cardiovascular function, and problems of species differences. In part, this is due to the impact of molecular medicine on traditional physiology, which not only affects priority for publication in top tier journals, but also funding priorities for NIH study sections, resulting in the closure of almost all cardiovascular physiology laboratories, leaving the cardiovascular physiology in many molecular publications to incidental data that are not peer reviewed and in many cases are inaccurate. It is the plea of this Viewpoint to correct this deficiency in expertise in our scientific community, a project with no simple solutions.
Keywords: Pharmacology, Cardiovascular Physiology, Academic Fraud
It is widely recognized that relatively few cardiovascular therapeutic modalities are emerging from the plethora of studies in genetically altered mouse models over the past quarter century, e.g., the success rate for new drug development projects in Phase II trials fell from 28 to 18%1. The most popular explanation has been irreproducibility of data in that only in 20–25% of projects repeated in industry where the data were completely in line with what was in the literature, often because published data were incorrect1. The current Viewpoint offers a novel reason for failure of translation, i.e., the difficulties, limitations and errors in studying cardiovascular physiology in the 21st century.
The goal of this Viewpoint is not to dwell on papers with false or inaccurate data, but rather to offer other reasons for problems in data that lead to failure of clinical translation. Because the numbers of citations are limited by the Viewpoint format and because of the sensitivity of pointing out errors in other papers or errors in judgement of the pharmaceutical industry, no names of authors with incorrect data or names of complicit institutions will be identified.
DATA FRAUD AND INSTITUTIONAL COMPLICITY
One of the most egregious examples occurred when I was Editor of Circulation Research, where the authors had plagiarized another paper on the effects of a circulating hormone word for word and substituted only the name of the circulating hormone throughout the paper and obviously also changed the authors names and the university from which it came. Another example involved manufactured data; the authors never responded to this criticism and just published it in another journal. It turns out that the problem of rejecting a paper, even if the data are false does not prevent the data from being published in another journal. Another point is that institutions such as the Universities involved, the American Heart Association and NIH were hesitant to pursue either of these issues.
SPECIES DIFFERENCES
Species differences is one reason why drugs are not successfully translated to patients. There is an overwhelming reliance on studies in rodents, with rare studies being conducted in large mammalian models, and most importantly, primates, even though their physiology is closest to humans, e.g., primates, but not rodents, go through menopause, and for research on aging, it is difficult to extrapolate from the rodent’s 2–4 year life span to that of a human, whereas monkeys can live 30–40 years,. However, rodents remain the overwhelmingly favorite model for cardiovascular research. The reasons for this are manifold, ranging from prohibitive costs for large animal research, excessive regulatory restrictions, to lack of experience with large animal research to potentially the most important reason, i.e., that the vast majority of research that is approved for funding by NIH involves genetically altered mouse models and therefore these models are studied most extensively.
Another example is that of beta 3-adrenergic receptor stimulation. About 20 years ago there was considerable interest in translating the exciting basic research to the clinics, with several multimillion dollar clinical trials failing, which could have been due to species differences. Our laboratory had published on the efficacy of beta 3 stimulation in rodents, and even dogs, but failed to demonstrate efficacy in non-human primates2. Even though after one of the coauthors took a position at a major pharmaceutical company and tried to explain the negative results, the company went forward with the clinical trials and also published a paper in non-human primates that purportedly showed the beneficial vasodilator actions of the drug3. That paper used facial flushing as their data for peripheral vasodilation, rather than direct measurements of arterial pressure and regional blood flows.
EFFECTS OF ANESTHESIA
The overwhelming number of cardiovascular research studies are in acutely prepared or anesthetized animal models, despite the fact that there are profound direct effects of anesthesia on cardiovascular function, but more importantly, anesthesia alters responses to common interventions, such as drugs, e.g., cardiac glycosides neural cardiovascular control4. Thus, it is not difficult to imagine how anesthesia may modify results and also understanding the effects of drugs for translation to the clinics. A recent example occurred with a new drug which increases sarcomere contraction in the heart, a novel mechanism to improve cardiac performance5. Studies in chronically instrumented, conscious animals with heart failure found that this drug was superior to sympathomimetic amines, since it improved myocardial function without an increase in MVO26. Quite different results were reported in anesthetized animals, where the drug no longer had the salutary action on protecting MVO26, which is most critical for success of any inotropic agent in patients with heart failure.
LACK OF PHYSIOLOGICAL EXPERTISE
A major problem for the accuracy of cardiovascular measurements relates to lack of ability to use direct and continuous measurements of left ventricular (LV) dimensions, pressures, and arterial pressure and regional blood flows. There are only a handful of laboratories in the world where this expertise still exists. As noted above, most laboratories, particularly those studying mice, rely on indirect techniques, e.g., echocardiography, to assess LV function. Although this technique generally requires anesthesia, which can affect circulatory dynamics markedly as already discussed, these studies rely on measurements of LV ejection fraction or fractional shortening to assess LV function, disregarding effects of preload and afterload which can affect these measurements significantly. Furthermore, stroke volume, calculated from published echo data of diameters, often is opposite to the conclusions of these papers, based only on fractional shortening.
INADVERTENT NEGATIVE IMPACT OF THE ERA OF MOLECULAR BIOLOGY ON TRADITIONAL PHYSIOLOGY
Sometimes major advances have unintended consequences. Such is the case for the advances in cardiovascular research induced by the molecular biology revolution a quarter century ago, resulting in the decline of physiology laboratories due to the inability for them to compete for publication space in top tier journals and for the limited NIH funding. I was complicit by transforming the major emphasis of Circulation Research from physiology to molecular biology.
WISHFUL THINKING
Another reason for failure of drug development is “wishful thinking”, i.e., assuming a mechanism from indirect data or based on data from inadequate measurements. One example is apoptosis. Since its discovery in 1972 as a novel mediator of cell death, studies of apoptosis mushroomed. One reason for the explosion of studies relates to the ease of measuring apoptosis by the TUNEL technique, which does not require extensive training to learn. When increased apoptosis was correlated with heart failure, this mechanism became widely recognized as a major factor in mediating heart failure. This conclusion was based on the assumption that apoptosis only occurred in myocytes in the heart and the resulting loss of myocytes is an important mechanism for the development of heart failure, but was never documented. Since over 70% of cells in the heart are non-myocytes, it would be easy to exaggerate the importance of apoptosis on cardiac function, if its occurrence was in non-myocytes, which has been recently documented7.
Another example is “Hibernating Myocardium”, a complex syndrome, which refers to severely and chronically depressed myocardial function, which gradually recovers, but not always completely, after revascularization8. Since acute reduction in blood flow reduces myocardial function, it was assumed that blood flow was severely reduced to the dysfunctional myocardium in patients with chronic coronary artery disease. However, these studies did not measure blood flow to the hibernating myocardium. Our studies in chronically instrumented conscious pigs with chronic myocardial ischemia, supported by studies in patients with hibernating myocardium, where blood flow was also actually measured, found that blood flow was not severely depressed in the myocardium that eventually recovered after revascularization9, 10, and that the reduced function resembled that which was described originally for “stunned myocardium”.
A third example comes from stem cell therapy, a major focus of cardiovascular research supported by the NIH and the pharmaceutical industry over the past two decades. Everyone had wished for successful translation of this breakthrough technology to patients with chronic coronary artery disease. The results have been disappointing and a recent article by Rosen et al.11, summarizes the multifactorial reasons for the failure, which include errors in infarct zone assessment and need to retract papers, based on wishful thinking.
It is interesting to note that these problems are not limited to cardiovascular research but are also noted in cancer research, and even political science. One of the most highly cited political science articles recently concluded that politically conservative individuals have higher Psychotocism scores, which relate to less highly desirable socio-economic traits, with the reverse for liberals12. Unfortunately, it was pointed out to the authors that they made a simple mistake and reversed the codes for conservative and liberal data and then had to print a retraction13.
SHIFTING BASELINES
A major problem leading to irreproducibility of data is the wide variance of baseline measurements in the same animal model with the same intervention. One example is infarct/area at risk measurements in mouse wild type models of the same strain and time for coronary occlusion and reperfusion, ranging from 15% to 67% in papers from different laboratories. More disturbing is when from the same laboratory reports in different publications markedly different baseline infarct size in the wild type mice, differing from 15% when the transgenic model is supposed to show increase to as high as 40% in the wild type, when the transgenic is supposed to show a decrease in infarct size.
THE POWER OF THE PURSE
Many laboratories depend on financial support from the pharmaceutical industry. It is understandable that the industry wants to see favorable effects of their drugs and it is widely recognized that they prefer to support laboratories for their studies, where the likelihood of positive results is more predictable. The lure of funding is an important reason why data can be biased and irreproducible. Two experiences from our laboratory support this concept. Our laboratory was supported for several years by a company involved in developing calcium channel blockers, until the support was cut off after we found in chronically instrumented conscious baboons that there was no reduction in infarct size with these drugs14. Another example is support our laboratory received from the American Medical Association (AMA) to study the effects of nicotine on the coronary circulation, when we found in 1975 that it induced coronary vasodilation15, but later, in 1984, when we found that nicotine also caused reflex vasoconstriction16, the AMA no longer funded our laboratory; maybe to no surprise as the funds were given to the AMA from the cigarette industry.
It is not only industry funding that can bias research reporting, but also the power of NIH funding. It would also be important to determine how many studies supported by NIH published irreproducible results. A simple way of examining this issue would be to examine the NIH funding supporting all those retracted papers, which were published in top tier journals. It does not require much imagination to figure out the link between publication in journals of the highest impact factor and future NIH funding, and the link to “Publish or Perish”.
PUBLICATION IN PRESTIGIOUS JOURNALS
Randy Schekman, the Nobel Laureate, recently published a paper on why he does not publish in prestige journals, indicating that the editors are more interested in flashy articles, which sometimes are not based on solid data17. This point is substantiated by the number of articles that have been retracted from these prestigious journals1.
SUMMARY
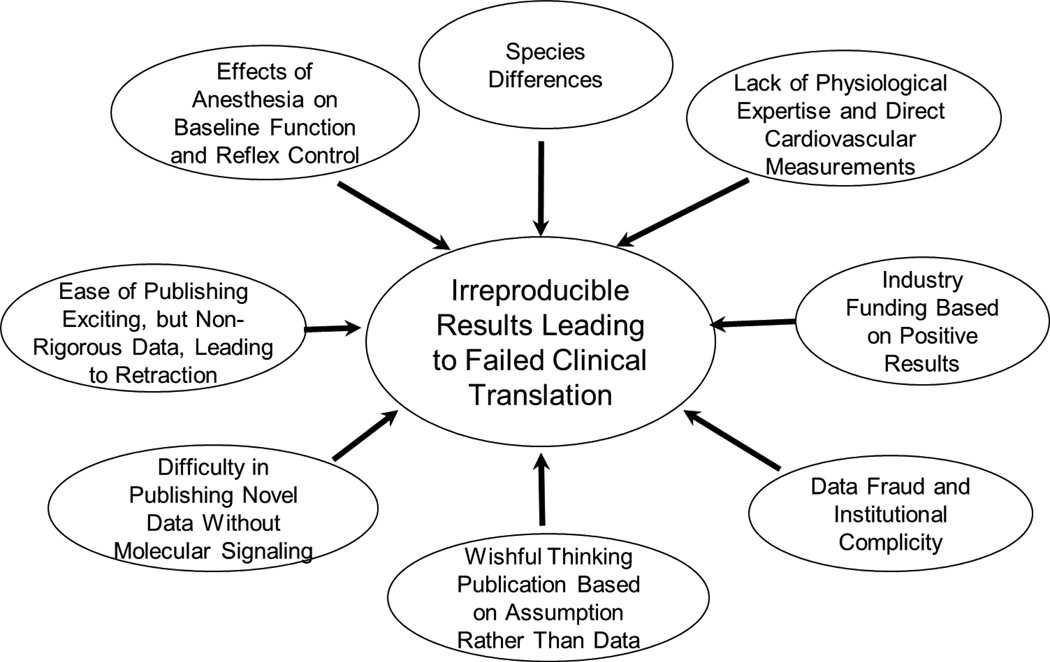
In conclusion, this viewpoint has put forth multiple new reasons for the failure to successfully translate new drugs to the clinics from the bench (Figure 1). Several of the concepts proposed have also been noted by others, e.g., the lack of reproducibility of studies and the problems with accuracy and rigor1. However, one of the reasons for translational failure has not been emphasized by others, i.e., the lack of state-of-the-art cardiovascular measurements. Several reasons have been proposed in this viewpoint, e.g., effects of anesthesia, lack of direct measurements of cardiovascular function, problems of species differences. One final point needs to be mentioned and that is the impact of molecular medicine on traditional physiology. The priorities of prestigious journals and NIH have moved away from traditional physiology over the past quarter century, resulting in lack of state-of-the-art physiology laboratories, leaving the cardiovascular physiology in many molecular publications to incidental data that are not peer reviewed and are in many cases inaccurate. It is the plea of this Viewpoint to correct this deficiency in expertise in our scientific community, a project with no simple solutions.
Figure 1.
Nonstandard Abbreviations and Acronyms
- AMA
American Medical Association
- LV
Left Ventricular
References
- 1.Prinz F, Schlange T, Asadullah K. Believe it or not: How much can we rely on published data on potential drug targets? Nature Reviews Drug Discovery. 2011;10:U712–U781. doi: 10.1038/nrd3439-c1. [DOI] [PubMed] [Google Scholar]
- 2.Shen YT, Cervoni P, Claus T, Vatner SF. Differences in beta 3-adrenergic receptor cardiovascular regulation in conscious primates, rats and dogs. J Pharmacol Exp Ther. 1996;278:1435–1443. [PubMed] [Google Scholar]
- 3.Hom GJ, Forrest MJ, Bach TJ, Brady E, Candelore MR, Cascieri MA, Fletcher DJ, Fisher MH, Iliff SA, Mathvink R, Metzger J, Pecore V, Saperstein R, Shih T, Weber AE, Wyvratt M, Zafian P, MacIntyre DE. Beta(3)-adrenoceptor agonist-induced increases in lipolysis, metabolic rate, facial flushing, and reflex tachycardia in anesthetized rhesus monkeys. J Pharmacol Exp Ther. 2001;297:299–307. [PubMed] [Google Scholar]
- 4.Vatner SF, Braunwald E. Cardiovascular control mechanisms in the conscious state. New Engl J Med. 1975;293:970–976. doi: 10.1056/NEJM197511062931906. [DOI] [PubMed] [Google Scholar]
- 5.Shen YT, Malik FI, Zhao X, Depre C, Dhar SK, Abarzua P, Morgans DJ, Vatner SF. Improvement of cardiac function by a cardiac myosin activator in conscious dogs with systolic heart failure. Circ Heart Fail. 2010;3:522–527. doi: 10.1161/CIRCHEARTFAILURE.109.930321. [DOI] [PubMed] [Google Scholar]
- 6.Bakkehaug JP, Kildal AB, Engstad ET, Boardman N, Naesheim T, Ronning L, Aasum E, Larsen TS, Myrmel T, How OJ. Myosin activator omecamtiv mecarbil increases myocardial oxygen consumption and impairs cardiac efficiency mediated by resting myosin atpase activity. Circ Heart Fail. 2015;8:766–775. doi: 10.1161/CIRCHEARTFAILURE.114.002152. [DOI] [PubMed] [Google Scholar]
- 7.Jose CJ, Vatner DE, Vatner SF. Myocardial apoptosis in heart disease: Does the emperor have clothes? Basic Res Cardiol. 2016;111:31. doi: 10.1007/s00395-016-0549-2. [DOI] [PubMed] [Google Scholar]
- 8.Rahimtoola SH. The hibernating myocardium. Am Heart J. 1989;117:211–221. doi: 10.1016/0002-8703(89)90685-6. [DOI] [PubMed] [Google Scholar]
- 9.Shen YT, Vatner SF. Mechanism of impaired myocardial function during progressive coronary stenosis in conscious pigs. Hibernation versus stunning? Circ Res. 1995;76:479–488. doi: 10.1161/01.res.76.3.479. [DOI] [PubMed] [Google Scholar]
- 10.Wijns W, Vatner SF, Camici PG. Hibernating myocardium. N Engl J Med. 1998;339:173–181. doi: 10.1056/NEJM199807163390307. [DOI] [PubMed] [Google Scholar]
- 11.Rosen MR, Myerburg RJ, Francis DP, Cole GD, Marban E. Translating stem cell research to cardiac disease therapies: Pitfalls and prospects for improvement. J Am Coll Cardiol. 2014;64:922–937. doi: 10.1016/j.jacc.2014.06.1175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Verhulst B, Eaves LJ, Hatemi PK. Correlation not causation: The relationship between personality traits and political ideologies. Am J Pol Sci. 2012;56:34–51. doi: 10.1111/j.1540-5907.2011.00568.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Verhulst B, Eaves LJ, Hatemi PK. Erratum to “correlation not causation: The relationship between personality traits and political ideologies” american journal of political science 56 (1), 34–51. Am J Pol Sci. 2016;60:E3–E4. doi: 10.1111/j.1540-5907.2011.00568.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vatner SF, Patrick TA, Knight DR, Manders WT, Fallon JT. Effects of calcium channel blocker on responses of blood flow, function, arrhythmias, and extent of infarction following reperfusion in conscious baboons. Circ Res. 1988;62:105–115. doi: 10.1161/01.res.62.1.105. [DOI] [PubMed] [Google Scholar]
- 15.Vatner SF, McRitchie RJ. Interaction of the chemoreflex and the pulmonary inflation reflex in the regulation of coronary circulation in conscious dogs. Circ Res. 1975;37:664–673. doi: 10.1161/01.res.37.5.664. [DOI] [PubMed] [Google Scholar]
- 16.Murray PA, Lavallee M, Vatner SF. Alpha-adrenergic-mediated reduction in coronary blood flow secondary to carotid chemoreceptor reflex activation in conscious dogs. Circ Res. 1984;54:96–106. doi: 10.1161/01.res.54.1.96. [DOI] [PubMed] [Google Scholar]
- 17.Schekman R. How journals like nature, cell and science are damaging science. The Guardian. 2013 [Google Scholar]