Abstract
Renal transplantation is the best option in the treatment of end-stage renal disease However these patients are under the risk of developing malignancies particularly due to effects of immune supression. These malignancies tend to be more agressive compared to the general population. Here, we present a case of urothelial carcinoma develoing in the ureter of allograft kidney.
Keywords: Nephroureterectomy, renal transplantation, urothelial carcinoma
Introduction
Renal transplantation is the best option in the treatment of end-stage renal disease and offers improved survival rates and quality of life.[1,2] Development of malignancy is an important issue after renal transplantation which might be related to immunosuppressive therapy. Renal cell carcinoma developing in the native kidney is the most common genitourinary malignancy after renal transplantation, however rare cases of de novo urothelial carcinoma in the pelvis or ureter of allograft kidney have also been reported. [3–8] Here, we present a renal allograft recipient who developed urothelial carcinoma in the upper ureter of allograft kidney.
Case presentation
A 30-year-old man admitted to the hospital because of asymptomatic macroscopic hematuria. At the age of 23, he had undergone cadaveric renal transplantation for end-stage renal disease. Laboratory tests revealed increased creatinine levels (baseline 1.9 mg/dL to 3.47 mg/dL). Ultrasonography was performed and grade III hydronephrosis in the transplanted kidney and a soft tissue with suspected blood flow in the upper ureter was detected. Percutanous nephrostomy was placed in the renal pelvis and creatinine level was decreased.
Computed tomography (CT) was performed which revealed soft tissue in the upper ureter possibly related to malignancy of inflammatory conditions (Figure 1a, b). Urothelial carcinoma of the ureter was suspected due to inconclusive results of imaging modalities. Then antegrade ureteroscopy was performed and a papillary lesion of about 2 cm was observed in the proximal ureter. Biopsy was performed and biopsy report revealed high grade urothelial carcinoma with lamina propria infiltration. Cystoscopy was performed in the same session and no pathological lesions were observed in the bladder. Nephroureterectomy together with bladder cuff incision was performed and gross view of the material is given in Figure 2. The final pathology also revealed high grade urothelial carcinoma ureter in the allograft kidney with the stage pT3 disease. The patient is followed up after cessation of the immunosuppressive therapy. Informed consent of the patient was taken from the patient.
Figure 1.
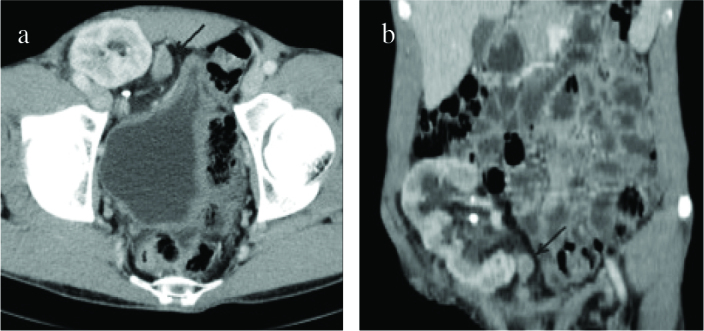
a, b. Computed tomography images of the mass in the upper ureter. (a) Transverse plane. (b) Coronal plane
Figure 2.
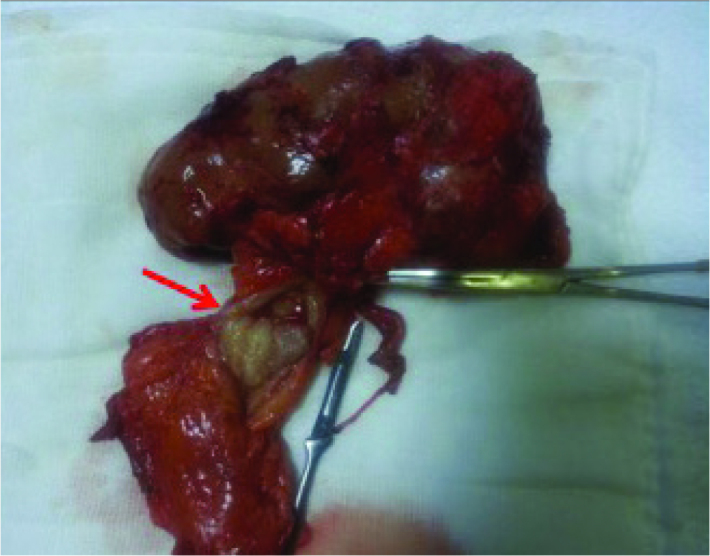
Gross view of the nephroureterectomy material
Discussion
Immune suppression is routinely performed after transplantation with various agents.[9] Following renal transplantation a marked increase in the risk of some cancers develops, and increasing evidence supports the role of immune suppression in the development of this increased risk.[10] Risk of developing urothelial cancers was shown to be three times greater in patients who underwent renal transplantation relative to the general population.[11] Incidence of urothelial carcinomas shows significant geographic variations. In a study from China 1420 patients who had undergone renal transplantation were followed up and 27 patients (1.9%) had been found to develop urothelial carcinoma.[12] This incidence was significantly higher compared to data from United States in which 5 cases of bladder urothelial carcinoma were reported in 6288 patients with follow up over 30 years.[13] Chinese herbs containing aristolochic acid were blamed to be responsible for this discrepancy in incidence.
Patient characteristics during the diagnosis of cancer are also distinct compared to the general population. Patients generally present in younger age. In one series of 5920 renal transplantation patients, 11 patients were diagnosed with urothelial cancer and only one of these patients were found to have urothelial carcinoma of the upper tract. Mean age of patients in this cohort was 55 (36–73) years, and the patient with upper tract cancer was 67 years old.[6] Our patient was 30 years old at the time of diagnosis which further verifies the early onset of the disease compared with the the expected age of >70 years for upper tract urothelial carcinoma.
Another important parameter during diagnosis is the tumor stage which is also very important for disease prognosis. Patients developing urothelial cancer following renal transplantation were found to have higher stage of disease[6] and our patient was also diagnosed with pT3 disease following nephroureterectomy. These findings suggest the early onset and aggressive nature of the disease in this specific patient population. Therefore hematuria- the most common initial symptom of urothelial cancer- should be investigated thoroughly as for suspect urothelial carcinoma of the bladder, collecting system and ureter of renal allograft and native upper urinary tract as well. Ureter and collecting system of the allograft is a very rare site for the development of the urothelial carcinoma. However when it occurs, as in our case, it results in extirpation of the allograft besides its oncological outcomes.
In conclusion, patients diagnosed with urothelial carcinoma after renal transplantation, in the entire urinary system have tendency to be at a younger age than patients in the general population. Additionally tumors have more aggressive characteristics that lead to higher stage at diagnosis. Immune suppression following transplantation is the most important contributor to these aggressive characteristics. Most common sign of urothelial carcinoma is hematuria, and therefore patients with complaint of hematuria should undergo precise evaluation to rule out urothelial carcinoma in the urinary system.
Footnotes
Informed Consent: Written informed consent was obtained from patient who participated in this case.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – M.İ.G., A.T.; Design - M.İ.G., A.F.K.; Supervision – S.A., A.T.; Resources - M.İ.G., A.F.K.; Materials - M.İ.G., A.F.K.; Data Collection and/or Processing - M.İ.G., A.F.K.; Analysis and/or Interpretation - M.İ.G., A.F.K., S.A., A.T.; Literature Search – M.İ.G., S.A., A.T.; Writing Manuscript – M.İ.G.; Critical Review – A.F.K., S.A., A.T.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Wolfe RA, Ashby VB, Milford EL, Ojo AO, Ettenger RE, Agodoa LY, et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N Engl J Med. 1999;341:1725–896. doi: 10.1056/NEJM199912023412303. http://dx.doi.org/10.1056/NEJM199912023412303. [DOI] [PubMed] [Google Scholar]
- 2.Bayazıt Y, Arıdoğan IA, Tansuğ Z, Yaman M, Doran S, Erken U. The results of 147 renal transplant patients. Turk J Urol. 2001;27:184–9. [Google Scholar]
- 3.Vervloessem I, Oyen R, Vanrenterghem Y, Van Poppel H, Van Hover P, Debakker G, et al. Transitional cell carcinoma in a renal allograft. Eur Radiol. 1998;8:936–8. doi: 10.1007/s003300050491. http://dx.doi.org/10.1007/s003300050491. [DOI] [PubMed] [Google Scholar]
- 4.Jensen P, Ulhoi BP, Nielsen EH. Transitional-cell carcinoma in a 25-year-old renal allograft. Nephrol Dial Transplant. 1998;13:3240–1. doi: 10.1093/ndt/13.12.3240. http://dx.doi.org/10.1093/ndt/13.12.3240. [DOI] [PubMed] [Google Scholar]
- 5.Penn I. Primary kidney tumors before and after renal transplantation. Transplantation. 1995;59:480–5. http://dx.doi.org/10.1097/00007890-199559040-00006. [PubMed] [Google Scholar]
- 6.Cox J, Colli JL. Urothelial cancers after renal transplantation. Int Urol Nephrol. 2011;43:681–6. doi: 10.1007/s11255-011-9907-z. http://dx.doi.org/10.1007/s11255-011-9907-z. [DOI] [PubMed] [Google Scholar]
- 7.Mokos I, Pasini J, Stern-Padovan R, Mrsic S, Ries S. Conservative surgical treatment of low-grade urothelial carcinoma in the renal allograft recipient: a case report. Transplant Proc. 2006;38:1363–5. doi: 10.1016/j.transproceed.2006.02.085. http://dx.doi.org/10.1016/j.transproceed.2006.02.085. [DOI] [PubMed] [Google Scholar]
- 8.Takaoka E, Miyazaki J, Kimura T, Kojima T, Kawai K, Murata Y, et al. Concurrent urothelial carcinoma in the renal pelvis of an allograft kidney and native recipient bladder: evidence of donor origin. Jpn J Clin Oncol. 2014;44:366–9. doi: 10.1093/jjco/hyu015. http://dx.doi.org/10.1093/jjco/hyu015. [DOI] [PubMed] [Google Scholar]
- 9.Ekmekçioğlu O, Turkan S, Yıldız Ş, Güneş ZE. Comparison of tacrolimus with a cyclosporine microemulsion for immunosuppressive therapy in kidney transplantation. Turk J Urol. 2013;39:16–21. doi: 10.5152/tud.2013.004. http://dx.doi.org/10.5152/tud.2013.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vajdic CM, McDonald SP, McCredie MR, van Leeuwen MT, Stewart JH, Law M, et al. Cancer incidence before and after kidney transplantation. JAMA. 2006;296:2823–31. doi: 10.1001/jama.296.23.2823. http://dx.doi.org/10.1001/jama.296.23.2823. [DOI] [PubMed] [Google Scholar]
- 11.Buzzeo BD, Heisey DM, Messing EM. Bladder cancer in renal transplant recipients. Urology. 1997;50:525–8. doi: 10.1016/S0090-4295(97)00305-1. http://dx.doi.org/10.1016/S0090-4295(97)00305-1. [DOI] [PubMed] [Google Scholar]
- 12.Li XB, Xing NZ, Wang Y, Hu XP, Yin H, Zhang XD. Transitional cellcarcinoma in renal transplant recipients: a single center experience. Int J Urol. 2008;15:53–7. doi: 10.1111/j.1442-2042.2007.01932.x. http://dx.doi.org/10.1111/j.1442-2042.2007.01932.x. [DOI] [PubMed] [Google Scholar]
- 13.Master VA, Meng MV, Grossfeld GD, Koppie TM, Hirose R, Carroll PR. Treatment and outcome of invasive bladder cancer in patients after renal transplantation. J Urol. 2004;171:1085–8. doi: 10.1097/01.ju.0000110612.42382.0a. http://dx.doi.org/10.1097/01.ju.0000110612.42382.0a. [DOI] [PubMed] [Google Scholar]


