Abstract
Objective
To quantify the trends in imaging use for the diagnosis of appendicitis.
Methods
Retrospective study at an academic medical center over a 22-year period. Patients were identified by ICD-9 diagnosis code for appendicitis. Medical record data extraction of these patients included imaging test used (ultrasound, CT, or MRI), gender, age, and body mass index (BMI). The proportion of patients undergoing each scan was calculated by year. Regression analysis was performed to determine whether age, gender, or BMI affected the imaging choice.
Results
There were 2108 patients in this study, including 967 (43.5%) females and 599 (27%) children (<18 years old). CT use increased over time for the entire cohort (2.9% to 82.4%, p<0.0001) and each subgroup (males, females, adults, pediatrics, p<0.0001 for each). CT use increased more in females and adults than males and pediatric patients, though the differences in trends were not statistically significant (male vs. female p=0.8, adult vs. pediatric p=0.1). The percentage of patients who had no imaging used for the diagnosis of appendicitis decreased over time (p<0.0001 overall and each subgroup), and there was no difference in trends between complementary subgroups (males vs. female p=0.53, adults vs pediatrics p=0.66). There were no statistically significant changes in the use of ultrasound or MRI over the study period. With increasing BMI, CT was more frequently used.
Conclusion
Of those diagnosed with appendicitis at an academic medical center, CT use increased over 20-fold. However, there was not a statistically significant trend towards increased use of ultrasound or MRI.
Keywords: Computed tomography, Ultrasound, Magnetic Resonance Imaging, Appendicitis, Appendectomy
INTRODUCTION
Appendicitis is a common cause of abdominal pain in patients seen in the emergency department (ED); 267,585 cases were diagnosed in the United States in 2012 (1). Historically, the diagnosis of appendicitis has been based on history and physical examination alone, but this is incorrect up to 30% of the time (2). Although clinical scoring systems such as the Alvarado score improve the risk stratification of patients with possible appendicitis, a “negative” score misses 13.3% of patients with appendicitis (3). A missed diagnosis of appendicitis can have significant consequences including appendiceal rupture, abscess formation, peritonitis, sepsis, and death. The desire to prevent these outcomes is balanced by physicians’ goal to also minimize the negative laparotomy (appendectomy) rate (NLR) for those patients suspected of having appendicitis. Though this rate has previously been cited to be acceptable at 10–20% (4), the diagnostic accuracy of medical imaging has dramatically lowered this acceptability threshold to less than 5%. As a result, the evaluation of patients with possible appendicitis frequently involves the use of cross-sectional imaging, particularly computed tomography (CT).
Though a few studies have documented no change in NLR when CT is used pre-operatively (5), most have shown that the NLR for appendicitis is lowered substantially when CT imaging is used to confirm the diagnosis. For example, one study found that when no imaging was used, the negative laparotomy rate was 26.6%, compared with 6.6% when CT was used (6). Another single-center study found that the NLR decreased from 23% in 1990 to 1.7% in 2007 when there was a corresponding increase in pre-operative CT from 1% to 97.5% of patients (7). Moreover, the use of CT allows for the diagnosis of other non-appendicitis pathologies. Pooler et al. found that for adults referred to the ED for evaluation of appendicitis, 23.6% were found to have appendicitis while another 31.6% had another alternative diagnosis, 41.1% of which required hospitalization and 22% required a surgical intervention (8).
Less well documented is the effect of ultrasound and MRI on negative laparotomy rates, though their use in the diagnosis of appendicitis is recommended in specific circumstances, particularly for children and pregnant women (9). Since the accuracy of ultrasound has been shown to be inferior to CT (10–12), its effect on negative laparotomy rates may be less when compared with CT. For example, a state-level registry study showed that NLR was 9.8% for patients with no imaging, 8.1% for those who had an ultrasound, and 4.5% for those who had a CT (13). Few studies have demonstrated the effect of MRI on NLR, though its accuracy for diagnosing appendicitis has been shown to be similar to CT (14–16). One center found that the NLR for pregnant women dropped from 55% to 29% when MRI was introduced into the diagnostic pathway (17).
While several studies have documented the increase in CT imaging utilization for ED patients with abdominal pain over time (18–21), these studies have not examined whether MRI or ultrasound utilization has also increased. This is a particularly significant issue given the mounting attention to the potential harm from ionizing radiation associated with CT. Ionizing radiation is hypothesized to increase the lifetime risk of cancer by approximately one case for every 2000 abdominal CT scans performed (22), though some have debated the true severity of harm from CT (23). Assuming that these theoretical projections are correct, up to 1.5–2% of all current cancers could potentially be related to the use of CT scans (24). Alternatively, MRI and ultrasound use no ionizing radiation, obviating this potential risk. Furthermore, the use of imaging in general has been suggested to be too high, with one study suggesting that 20% of cases of appendicitis should be able to be diagnosed without the use of any type of imaging test (25).
There are currently several recommendations that outline the appropriate use of imaging tests for the evaluation of right lower quadrant abdominal pain (i.e. – evaluating for appendicitis), including the American College of Radiology’s Appropriateness Criteria (26). A combination of CT, ultrasound, and/or MRI is suggested, depending on the patient characteristics and pre-test probability of appendicitis. However, the trend in imaging utilization among these modalities has not previously been reported in a single population. The aim of this study, therefore, is to characterize the use of imaging tests for the diagnosis of appendicitis over a 22-year period at a large, academic, tertiary care medical center. Secondarily, we aim to evaluate whether age group (adults: ≥18 years old, pediatrics: <18 years old), gender, or body mass index (BMI) may affect the choice of imaging test used.
METHODS
Study design and setting
This is a HIPAA-compliant, IRB-approved retrospective study of patients diagnosed with appendicitis at a single academic medical center in the Midwest with an annual ED census of approximately 50,000. The study includes data from patients seen in the ED between 1992 and 2014.
Selection of Participants
The hospital’s billing database was used to identify patients with an International Classification of Disease – Ninth Edition (ICD-9) diagnosis code for appendicitis. Once identified, the electronic health record was queried for each patient to extract data related to their ED visit. Since our hospital’s electronic health record began in 1992, this study was limited to patients seen after that year. Patients who were inappropriately identified by the automated ICD-9 database query (did not have appendicitis diagnosed) or those with no documentation in their medical record regarding their care for the index visit were excluded from the study. Since we were evaluating trends in imaging utilization over time, we extracted data from the first two years and then every 2–3 years rather than each individual year. The years included in our data extraction were 1992, 1993, 1996, 1998, 2001, 2003, 2006, 2008, 2011, 2012, 2013, and 2014.
Methods and Measurements
Patients were initially identified by a billing database query based on ICD-9 codes for appendicitis. Once identified, one investigator abstracted demographic data (age at index visit, year of diagnosis, gender, weight, height, BMI), type of medical imaging used (CT, ultrasound, MRI, no imaging), and outcome data (imaging report, pathology report, surgical report). If there was no test result or mention of a test in the patient’s notes, it was presumed that no imaging study was performed. Patients were classified as having appendicitis if surgical or histological reports confirmed the diagnosis, or if there was a discharge diagnosis of appendicitis.
The data abstractor was a medical student who was trained in data abstraction by the principal investigator. A standardized data reporting form was used for the study and was tested on the first 25 patients to ensure that reporting was unambiguous. Missing data were flagged by the data abstractor for review by the principal investigator. The abstractor knew the general question of the study, though it was felt that this was unlikely to bias his findings. The principal investigator randomly selected five percent of charts for review to verify the data abstracted. Discordant data were resolved by discussion between the abstractor and the principal investigator until consensus was reached.
Outcomes
The outcome of interest was the percentage of patients undergoing medical imaging (CT, ultrasound, and/or MRI) or no imaging per year. This percentage was calculated using the number of patients undergoing each imaging test as the numerator and the number of patients diagnosed with appendicitis as the denominator. We also included categories for patients who underwent more than one imaging test (e.g. – CT and ultrasound). This diagnosis was confirmed by chart review (pathology results, surgical findings, and discharge diagnosis). Additional parameters that were collected include age, gender, height, weight, and body mass index (BMI).
Analysis
Statistical analysis consisted of a comparison of percentages over time using regression analysis. Percentages were calculated by dividing the number of patients undergoing each imaging test (or no test) in a selected year by the total number of patients diagnosed with appendicitis in that given year. These percentages were trended over time to characterize the change in utilization over the 22-year period. Secondarily, we evaluated the trend in utilization of medical imaging for patients in specific subgroups (male vs. female and adults vs. pediatrics). Additionally, since obesity can influence the ability to visualize the appendix on ultrasound, we evaluated the effect of BMI on choice of imaging test using the Cochran-Armitage Trend Test. Analyses were performed using SAS 9.4 for Windows (SAS Institute, Cary, North Carolina, USA). All tests of significance were at the p<0.05 level and p-values were two-tailed.
RESULTS
Characteristics of study subjects
There were 2222 patient identified during the study period who had an ICD-9 diagnosis of appendicitis, though only 2108 (94.9%) of patients had complete data. Of these, there were 918 (43.5%) women and 573 (27.2%) children. The mean age was 10.9 years (95%CI 10.6–11.3) for pediatric patients, 38 years (95%CI 37.2–38.8) for adults, and 30.8 years (95%CI 30–31.5) for the entire population. BMI values were available on 535 (55.3%) females and 634 (50.5%) males. The mean BMI was 25.7 (95%CI 25–26.3) for females, 25.6 (95%CI 24.8–26.4) for males, and 25.6 (95%CI 25.1–26.1) for the entire population.
Main results
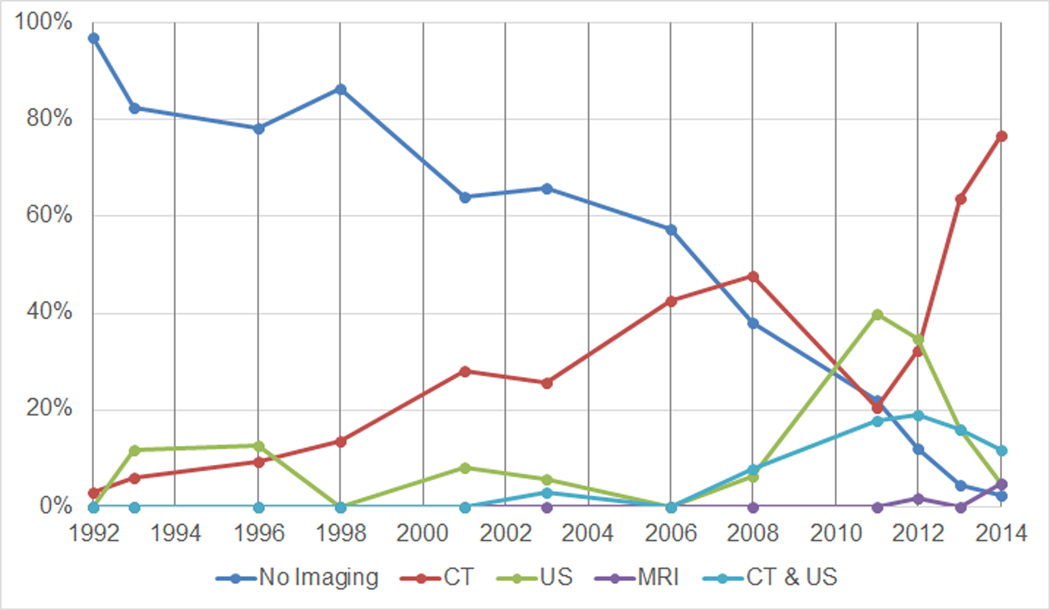
In the overall cohort, there was a significant increase in the number of patients with appendicitis diagnosed by CT alone during the study period, from 2.9% in 1992 to 83.1% in 2014 (p<0.0001 for trend). Correspondingly, the diagnosis of appendicitis without any form of imaging decreased for the entire cohort from 91.2% in 1992 to 2.5% in 2014 (p<0.0001 for trend, Figure 1). The change in utilization of ultrasound (4.4% to 2.5%), MRI (0% to 1.7%), and a combination of CT and US (1.5% to 10.2%) was not statistically significant.
Figure 1.
Percentage of patients undergoing each type of imaging test, by year.
Results by age group
We also stratified patients by age group (adults: ≥18 years, pediatrics: <18 years). CT use in adult patients trended higher than in pediatric patients over time (2.9% vs 2.9% in 1992, 86.7% vs 76.7% in 2014), though this difference was not statistically significant (p=0.1). In each group, however, there was a significant increase in the use of CT over time (p<0.0001 for trend). There was also no significant difference in the trend of ultrasound use when comparing adult and pediatric patients (5.8% vs 0% in 1992, 1.3% vs 4.7% in 2014). Though there did appear to be an increase in ultrasound use for pediatric patients in 2011, there was a subsequent reduction in its use (Figure 2). Similarly, when comparing adult versus pediatric patients, there was no difference in the trends of MRI use (0% vs 0% in 1992, 0% vs 4.7% in 2014), combined CT and ultrasound use (1.9% vs 0% in 1992, 9.3% vs 11.6% in 2014), or use of no imaging (89.3% vs 97.1% in 1992, 2.7% vs 2.3% in 2014). However, there was a statistically significant decrease in the proportion of patients diagnosed with appendicitis without imaging for each individual group (p<0.0001 for both groups).
Figure 2.
Percentage of pediatric patients undergoing each type of imaging test, by year.
Results by gender
Both male and female cohorts experienced an increase in CT utilization over the study period (p<0.0001 for both groups) and there was no significant difference between the two groups (5.1% vs 0% in 1992, 87.1% vs 78.6% in 2014). Additionally, when comparing males to females over the study period, there was no statistically significant difference in the trend of using ultrasound (2.5% vs 6.9% in 1992, 0% vs 5.4% in 2014), MRI (0% vs 0% in 1992, 3.2% vs 0% in 2014), or combined CT and ultrasound (1.3% vs 1.7% in 1992, 8.1% vs 12.5% in 2014). While there was a significant decrease in the proportion of patients diagnosed without the use of imaging for each group (males 91.1% to 1.6%, females 91.4% to 3.6%, p<0.0001 for both groups), there was no significant difference found when comparing the trend between these groups.
Results by body mass index
We also stratified patients by BMI to assess whether this impacted the choice of imaging test used to diagnose appendicitis. The categories used correspond to the World Health Organization standard definitions of underweight (BMI<18.5), normal weight (BMI 18.5–24.99), overweight (BMI 25–29.99), and obese (BMI>30) (27). For the overall cohort and for each subgroup (age, gender), CT was preferentially ordered regardless of BMI. As BMI increased, there was a corresponding increase in the use of CT from 48% to 79% with P<0.0001 and significant decrease in the use of ultrasound from 24% to 1% (Figure 3).
Figure 3.
Percentage of patients undergoing each type of imaging test, by body mass index category.
Use of MRI
There were only seven cases of MRI being used during the years evaluated in this study, with the first case occurring in 2006. Five of these patients were male and five had other imaging performed in addition to the MRI scan.
DISCUSSION
This study aimed to characterize the change in imaging test utilization for the diagnosis of appendicitis at a large, academic, tertiary care medical center. In particular, we aimed to evaluate the use of CT, ultrasound, and MRI from 1992 to 2014. As previously reported (18–20,28), we found a statistically significant (p<0.0001) trend of increasing CT use for the overall cohort as well as each subgroup (adults, pediatrics, males, females). Correspondingly, we found a statistically significant downward trend in the diagnosis of appendicitis without use of medical imaging for the overall cohort as well as each subgroup. However, there was no significant difference detected between the trends of complementary subgroups (adults vs pediatrics, males vs females), nor was there a difference observed in the trend of ultrasound, MRI, or combined CT and ultrasound use for the overall cohort or any of the subgroups. Overall, it appears that referring physicians are now almost universally incorporating medical imaging into the routine evaluation of patients suspected of having appendicitis.
As mentioned previously, increased use of CT has an associated increase in exposure to ionizing radiation, which is a risk factor for developing cancer. This is of particular importance for pediatric patients, who are more radiosensitive and have a longer time to develop cancer. The American College of Radiology’s Appropriateness Criteria “Right Lower Quadrant Pain – Suspected Appendicitis” addresses this concern by recommending the use of ultrasound to avoid ionizing radiation exposure in younger patients (29). This has helped to stem the previous increasing use of CT for pediatric patients (5,30), although CT scanning is still on the rise at some centers – as much as 49% over a 6-year period (28). Recent data show that many children’s hospitals have adopted an “ultrasound first” philosophy (31), decreasing the use of CT for the evaluation of appendicitis (32,33) and reducing negative laparotomy rates (34). Although we found a trend toward less CT imaging for women and children, it was not statistically significant. New innovations in CT technology, particularly iterative reconstruction and low-dose protocols, have dramatically reduced CT dose and may explain, in part, the continued use of CT in children and young adults. Reviewing figure 2, it is apparent that there was the beginning of a shift in imaging test choice from CT to ultrasound in pediatric patients, but that was reversed toward the end of the study period. This correlated with a change in protocol at our center due to concerns of too many false positive ultrasound exams when evaluating for appendicitis.
On occasion, CT and ultrasound were both used in the evaluation of a single patient. In most cases, the ultrasound was the first imaging modality used. Previous studies have demonstrated this finding as well, particularly in obese patients where ultrasound is frequently non-diagnostic (35) or female patients where additional pelvic pathology must be considered (33).
Despite one study suggesting that the use of abdominal MRI for the diagnosis of appendicitis is increasing, we did not find this trend in our data (36). In fact, there were only seven occurrences of its use in our study period. This utilization could possibly shift, however, given the number of recent articles highlighting the test accuracy of MRI in this situation (14–16). Additionally, our medical center does not have a labor and delivery service; pregnant patients are directed to another local hospital affiliated with our center. Since the strongest recommendations regarding MR use to diagnose appendicitis are for the pregnant population, the low level of MR utilization for appendicitis is partially explained by this operational issue.
It is important to note that our reported imaging utilization trends refer to patients who ultimately prove to have acute appendicitis, and does not include the larger subset of patients where appendicitis is excluded by imaging. One large CT-based study found that fewer than 25% of adults with suspected acute appendicitis ultimately prove to have this diagnosis (37), similar to the prevalence in older trials. Imaging utilization trends in this larger, negative group without appendicitis were not assessed by the current study, but would be worthy of further investigation.
Finally, we evaluated the possibility of BMI affecting the selection of imaging test used for patients in this study. In all BMI categories, CT was preferentially used, and the utilization increased with increasing BMI. This is likely due to the fact that ultrasound has generally poorer diagnostic accuracy when compared with CT as body habitus increases (10–12).
We recognize that there are a number of limitations to this study. First, due to the time and resources required to abstract data from thousands of patients’ charts, we only selected a subset of years within the study period. It is possible that there were large variations in image test ordering for the years in which data were not abstracted. However, given the consistency of the observed trends in this study, we feel this is highly unlikely. Secondly, while we attempted to capture cases of negative laparotomies by including admission and discharge diagnoses, we were unable to identify any such cases. We hypothesize this was due to limitations inherent to the automated data query based on ICD-9 code, preferentially identifying patients discharged with a diagnosis of appendicitis, and therefore not having a negative laparotomy. Third, the associated limitation of not addressing the larger negative imaging cohort without appendicitis was discussed above. Fourth, there was a change in the diagnostic protocol recommended for the evaluation of pediatric appendicitis late in our study period, shifting away from ultrasound and toward CT, which is reflected in our results. Additionally, the implementation of low-dose CT protocols likely had an impact. Had these changes not happened, we likely would have seen a statistically significant trend to increasing use of ultrasound for pediatric patients. Finally, this is a single-center study, limiting external validity, and relying on chart review methodology, which is prone to information bias. We tried to counteract this bias by following the recommendations described by Kaji et al (38).
In summary, the use of CT for the diagnosis of appendicitis has increased dramatically in the past 2 decades at our large academic medical center; it was used in 94% of patients in 2014 (82% as the single imaging test, 10% in combination with US) as opposed to 4.4% in 1992 (2.9% as a single imaging test, 1.5% in combination with US). Conversely, ultrasound was only used in the evaluation of approximately 4% of patients and MRI was rarely used (7 instances over the study period). This pattern of imaging utilization is not congruent with current imaging guidelines regarding the evaluation of possible appendicitis, which advocate for the use of ultrasound and MRI in select populations. Future research should focus on either identifying the barriers to the implementation of evidence-based guidelines or, alternatively, re-evaluating the guideline recommendations to account for the limitations of utilizing ultrasound and MRI outside of the tertiary care, academic medical center setting.
SUMMARY STATEMENT.
The use of CT for the diagnosis of appendicitis has increased dramatically in the past 2 decades, being used in 94% of patients in 2014 as opposed to 4.4% in 1992. Conversely, ultrasound was only used in the evaluation of approximately 4% of patients and MRI was rarely used.
Acknowledgments
Grant Support: National Center for Advancing Translational Sciences (NCATS) grant UL1TR000427 and KL2TR000428, National Institute on Aging grant K23AG038352, National Institute on Drug Abuse grant K23DA032306, and the National Institute for Diabetes and Digestive and Kidney Diseases grant K24DK102595. The University of Wisconsin – Madison Department of Radiology receives research support from GE Healthcare and Bracco Diagnostics.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Conflicts: Perry J. Pickhardt, MD has the following financial disclosures: Co-founder, VirtuoCTC and shareholder, Cellectar Biosciences. The other authors have no financial conflicts. Scott B. Reeder, MD, PhD is a shareholder of Cellectar Biosciences and Neuwave Medical.
REFERENCES
- 1. [cited 2015 Aug 17];HCUPnet: A tool for identifying, tracking, and analyzing national hospital statistics [Internet] Available from: http://hcupnet.ahrq.gov/HCUPnet.jsp?Id=1E1EE590A4752BF5&Form=DispTab&JS=Y&Acti on=Accept.
- 2.Birnbaum BA, Wilson SR. Appendicitis at the millennium. Radiology. 2000 May;215(2):337–348. doi: 10.1148/radiology.215.2.r00ma24337. [DOI] [PubMed] [Google Scholar]
- 3.Apisarnthanarak P, Suvannarerg V, Pattaranutaporn P, Charoensak A, Raman SS, Apisarnthanarak A. Alvarado score: can it reduce unnecessary CT scans for evaluation of acute appendicitis? Am J Emerg Med. 2015 Feb;33(2):266–270. doi: 10.1016/j.ajem.2014.11.056. [DOI] [PubMed] [Google Scholar]
- 4.Velanovich V, Satava R. Balancing the normal appendectomy rate with the perforated appendicitis rate: implications for quality assurance. Am Surg. 1992 Apr;58(4):264–269. [PubMed] [Google Scholar]
- 5.Partrick DA, Janik JE, Janik JS, Bensard DD, Karrer FM. Increased CT scan utilization does not improve the diagnostic accuracy of appendicitis in children. J Pediatr Surg. 2003 May;38(5):659–662. doi: 10.1016/jpsu.2003.5017. [DOI] [PubMed] [Google Scholar]
- 6.Kim K, Lee CC, Song K-J, Kim W, Suh G, Singer AJ. The impact of helical computed tomography on the negative appendectomy rate: a multi-center comparison. J Emerg Med. 2008 Jan;34(1):3–6. doi: 10.1016/j.jemermed.2007.05.042. [DOI] [PubMed] [Google Scholar]
- 7.Raja AS, Wright C, Sodickson AD, Zane RD, Schiff GD, Hanson R, et al. Negative appendectomy rate in the era of CT: an 18-year perspective. Radiology. 2010 Aug;256(2):460–465. doi: 10.1148/radiol.10091570. [DOI] [PubMed] [Google Scholar]
- 8.Pooler BD, Lawrence EM, Pickhardt PJ. Alternative diagnoses to suspected appendicitis at CT. Radiology. 2012 Dec;265(3):733–742. doi: 10.1148/radiol.12120614. [DOI] [PubMed] [Google Scholar]
- 9.Rankey D, Leach JL, Leach SD. Emergency MRI utilization trends at a tertiary care academic medical center: baseline data. Acad Radiol. 2008 Apr;15(4):438–443. doi: 10.1016/j.acra.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 10.van Randen A, Bipat S, Zwinderman AH, Ubbink DT, Stoker J, Boermeester MA. Acute appendicitis: meta-analysis of diagnostic performance of CT and graded compression US related to prevalence of disease. Radiology. 2008 Oct;249(1):97–106. doi: 10.1148/radiol.2483071652. [DOI] [PubMed] [Google Scholar]
- 11.Doria AS, Moineddin R, Kellenberger CJ, Epelman M, Beyene J, Schuh S, et al. US or CT for Diagnosis of Appendicitis in Children and Adults? A Meta-Analysis. Radiology. 2006 Oct;241(1):83–94. doi: 10.1148/radiol.2411050913. [DOI] [PubMed] [Google Scholar]
- 12.Al-Khayal KA, Al-Omran MA. Computed tomography and ultrasonography in the diagnosis of equivocal acute appendicitis. A meta-analysis. Saudi Med J. 2007 Feb;28(2):173–180. [PubMed] [Google Scholar]
- 13.SCOAP Collaborative. Cuschieri J, Florence M, Flum DR, Jurkovich GJ, Lin P, et al. Negative appendectomy and imaging accuracy in the Washington State Surgical Care and Outcomes Assessment Program. Ann Surg. 2008 Oct;248(4):557–563. doi: 10.1097/SLA.0b013e318187aeca. [DOI] [PubMed] [Google Scholar]
- 14.Leeuwenburgh MMN, Wiezer MJ, Wiarda BM, Bouma WH, Phoa SSKS, Stockmann HBAC, et al. Accuracy of MRI compared with ultrasound imaging and selective use of CT to discriminate simple from perforated appendicitis. Br J Surg. 2014 Jan;101(1):e147–e155. doi: 10.1002/bjs.9350. [DOI] [PubMed] [Google Scholar]
- 15.Cobben L, Groot I, Kingma L, Coerkamp E, Puylaert J, Blickman J. A simple MRI protocol in patients with clinically suspected appendicitis: results in 138 patients and effect on outcome of appendectomy. Eur Radiol. 2009 May;19(5):1175–1183. doi: 10.1007/s00330-008-1270-9. [DOI] [PubMed] [Google Scholar]
- 16.Repplinger MD, Levy JF, Peethumnongsin E, Gussick ME, Svenson JE, Golden SK, et al. Systematic review and meta-analysis of the accuracy of MRI to diagnose appendicitis in the general population. J Magn Reson Imaging JMRI. 2015 Dec 22; doi: 10.1002/jmri.25115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rapp EJ, Naim F, Kadivar K, Davarpanah A, Cornfeld D. Integrating MR imaging into the clinical workup of pregnant patients suspected of having appendicitis is associated with a lower negative laparotomy rate: single-institution study. Radiology. 2013 Apr;267(1):137–144. doi: 10.1148/radiol.12121027. [DOI] [PubMed] [Google Scholar]
- 18.Agarwal R, Bergey M, Sonnad S, Butowsky H, Bhargavan M, Bleshman MH. Inpatient CT and MRI utilization: trends in the academic hospital setting. J Am Coll Radiol JACR. 2010 Dec;7(12):949–955. doi: 10.1016/j.jacr.2010.08.015. [DOI] [PubMed] [Google Scholar]
- 19.Levin DC, Rao VM, Parker L, Frangos AJ, Sunshine JH. Recent trends in utilization rates of abdominal imaging: the relative roles of radiologists and nonradiologist physicians. J Am Coll Radiol JACR. 2008 Jun;5(6):744–747. doi: 10.1016/j.jacr.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 20.Rao VM, Levin DC, Parker L, Frangos AJ, Sunshine JH. Trends in utilization rates of the various imaging modalities in emergency departments: nationwide Medicare data from 2000 to 2008. J Am Coll Radiol JACR. 2011 Oct;8(10):706–709. doi: 10.1016/j.jacr.2011.04.004. [DOI] [PubMed] [Google Scholar]
- 21.Korley FK, Pham JC, Kirsch TD. Use of advanced radiology during visits to US emergency departments for injury-related conditions, 1998–2007. JAMA J Am Med Assoc. 2010 Oct 6;304(13):1465–1471. doi: 10.1001/jama.2010.1408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dixon AK, Dendy P. Spiral CT: how much does radiation dose matter? Lancet. 1998 Oct 3;352(9134):1082–1083. doi: 10.1016/S0140-6736(05)79751-8. [DOI] [PubMed] [Google Scholar]
- 23.Harvey HB, Brink JA, Frush DP. Informed Consent for Radiation Risk from CT Is Unjustified Based on the Current Scientific Evidence. Radiology. 2015 May;275(2):321–325. doi: 10.1148/radiol.2015142859. [DOI] [PubMed] [Google Scholar]
- 24.Berrington de González A, Mahesh M, Kim K-P, Bhargavan M, Lewis R, Mettler F, et al. Projected cancer risks from computed tomographic scans performed in the United States in 2007. Arch Intern Med. 2009 Dec 14;169(22):2071–2077. doi: 10.1001/archinternmed.2009.440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tan WJ, Acharyya S, Goh YC, Chan WH, Wong WK, Ooi LL, et al. Prospective comparison of the Alvarado score and CT scan in the evaluation of suspected appendicitis: a proposed algorithm to guide CT use. J Am Coll Surg. 2015 Feb;220(2):218–224. doi: 10.1016/j.jamcollsurg.2014.10.010. [DOI] [PubMed] [Google Scholar]
- 26.Rosen MP, Ding A, Blake MA, Baker ME, Cash BD, Fidler JL, et al. ACR Appropriateness Criteria® right lower quadrant pain--suspected appendicitis. J Am Coll Radiol JACR. 2011 Nov;8(11):749–755. doi: 10.1016/j.jacr.2011.07.010. [DOI] [PubMed] [Google Scholar]
- 27.WHO. [cited 2015 Aug 19];Global Database on Body Mass Index [Internet] Available from: http://apps.who.int/bmi/index.jsp?introPage=intro_3.html.
- 28.Broder J, Fordham LA, Warshauer DM. Increasing utilization of computed tomography in the pediatric emergency department, 2000–2006. Emerg Radiol. 2007 Sep;14(4):227–232. doi: 10.1007/s10140-007-0618-9. [DOI] [PubMed] [Google Scholar]
- 29.Smith MP, Katz DS, Lalani T, Carucci LR, Cash BD, Kim DH, et al. ACR Appropriateness Criteria® Right Lower Quadrant Pain-Suspected Appendicitis. Ultrasound Q. 2014 Oct 31; doi: 10.1097/RUQ.0000000000000118. [DOI] [PubMed] [Google Scholar]
- 30.Fahimi J, Herring A, Harries A, Gonzales R, Alter H. Computed tomography use among children presenting to emergency departments with abdominal pain. Pediatrics. 2012 Nov;130(5):e1069–e1075. doi: 10.1542/peds.2012-0739. [DOI] [PubMed] [Google Scholar]
- 31.Kotagal M, Richards MK, Chapman T, Finch L, McCann B, Ormazabal A, et al. Improving ultrasound quality to reduce computed tomography use in pediatric appendicitis: the Safe and Sound campaign. Am J Surg. 2015 May;209(5):896–900. doi: 10.1016/j.amjsurg.2014.12.029. discussion 900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Neff LP, Ladd MR, Becher RD, Jordanhazy RA, Gallaher JR, Pranikoff T. Computerized tomography utilization in children with appendicitis-differences in referring and children’s hospitals. Am Surg. 2011 Aug;77(8):1061–1065. [PubMed] [Google Scholar]
- 33.Saito JM, Yan Y, Evashwick TW, Warner BW, Tarr PI. Use and accuracy of diagnostic imaging by hospital type in pediatric appendicitis. Pediatrics. 2013 Jan;131(1):e37–e44. doi: 10.1542/peds.2012-1665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bachur RG, Hennelly K, Callahan MJ, Monuteaux MC. Advanced radiologic imaging for pediatric appendicitis, 2005–2009: trends and outcomes. J Pediatr. 2012 Jun;160(6):1034–1038. doi: 10.1016/j.jpeds.2011.11.037. [DOI] [PubMed] [Google Scholar]
- 35.Sulowski C, Doria AS, Langer JC, Man C, Stephens D, Schuh S. Clinical outcomes in obese and normal-weight children undergoing ultrasound for suspected appendicitis. Acad Emerg Med Off J Soc Acad Emerg Med. 2011 Feb;18(2):167–173. doi: 10.1111/j.1553-2712.2010.00993.x. [DOI] [PubMed] [Google Scholar]
- 36.Quaday KA, Salzman JG, Gordon BD. Magnetic resonance imaging and computed tomography utilization trends in an academic ED. Am J Emerg Med. 2014 Feb 4; doi: 10.1016/j.ajem.2014.01.054. [DOI] [PubMed] [Google Scholar]
- 37.Pickhardt PJ, Lawrence EM, Pooler BD, Bruce RJ. Diagnostic performance of multidetector computed tomography for suspected acute appendicitis. Ann Intern Med. 2011 Jun 21;154(12):789–796. doi: 10.7326/0003-4819-154-12-201106210-00006. W – 291. [DOI] [PubMed] [Google Scholar]
- 38.Kaji AH, Schriger D, Green S. Looking through the retrospectoscope: reducing bias in emergency medicine chart review studies. Ann Emerg Med. 2014 Sep;64(3):292–298. doi: 10.1016/j.annemergmed.2014.03.025. [DOI] [PubMed] [Google Scholar]