Abstract
Objective
To evaluate the relationships between tongue pressure and different aspects of the oral-phase swallowing function.
Methods
We included 96 stroke patients with dysphagia, ranging in age from 40 to 88 years (mean, 63.7 years). Measurements of tongue pressure were obtained with the Iowa Oral Performance Instrument, a device with established normative data. Three trials of maximum performance were performed for lip closure pressure (LP), anterior hard palate-to-tongue pressure (AP), and posterior hard palate-to-tongue pressure (PP); buccal-to-tongue pressures on both sides were also recorded (buccal-to-tongue pressure, on the weak side [BW]; buccal-to-tongue pressure, on the healthy side [BH]). The average pressure in each result was compared between the groups. Clinical evaluation of the swallowing function was performed with a videofluoroscopic swallowing study.
Results
The average maximum AP and PP values in the intact LC group were significantly higher than those in the inadequate lip closure group (AP, p=0.003; PP, p<0.001). AP and PP showed significant relationships with bolus formation (BF), mastication, premature bolus loss (PBL), tongue to palate contact (TP), and oral transit time (OTT). Furthermore, LP, BW, and BH values were significantly higher in the groups with intact mastication, without PBL and intact TP.
Conclusion
These findings indicate that the tongue pressure appears to be closely related to the oral-phase swallowing function in post-stroke patients, especially BF, mastication, PBL, TP and OTT.
Keywords: Dysphagia, Stroke, Tongue pressure, VFSS, Iowa Oral Performance Instrument
INTRODUCTION
Dysphagia is a common complication in post-stroke patients, with reported incidences varying between 29% and 67% [1]. Post-stroke dysphagia is associated with serious complications such as aspiration, a prolonged length of hospital stay, and increased mortality. Early detection and treatment of dysphagia are crucial issues in post-stroke patients [2].
The process of normal swallowing consists of a three-stage sequential model. The swallowing process is divided into the oral, pharyngeal, and esophageal stages according to the location of the bolus [3]. The movement of the tongue is an important contributor to the oral-stage swallowing. It plays a crucial role in maintaining a cohesive bolus while manipulating the bolus during mastication, and propelling the bolus out of the oral cavity and through the larynx. In stroke patients, dysfunctions of lower tongue pressure such as lingual discoordination can cause a range of problems in the oral-phase swallowing [4]. Clinically, tongue pressure has been reported to be a good predictor of the presence of oral-phase dysphagia [5,6,7,8]. Until now, there have been few studies that evaluated tongue pressure in relation to different aspects of the oral-phase swallowing function in patients with post-stroke dysphagia.
Various bedside tests have been applied for evaluating dysphagia after a stroke. However, almost half of the patients continue to suffer from silent aspiration. In such cases, a videofluoroscopic swallowing study (VFSS) is the gold standard for detecting dysphagia [9,10]. Clinical evaluation of swallowing function was performed with a VFSS, which provided visual assessment of the entire process of deglutitive movement and bolus transport [11].
In addition to the oral-phase swallowing function, we also assessed the relationship between tongue pressure and the patients' functional outcomes. Previous studies have found that patients with dysphagia had significantly lower cognitive function as well as functional evaluation score [12]. In this study, the Korean version of Mini Mental State Examination (K-MMSE) and the Korean version of Modified Barthel Index (K-MBI) scores were used to evaluate cognitive function and activities of daily living (ADL), respectively.
The aims of this study were (1) to evaluate the relationships between tongue pressure and different aspects of the oral-phase swallowing function and (2) to evaluate the relationships between tongue pressure and functional outcomes.
MATERIALS AND METHODS
Subjects were recruited from a group of patients referred to the Department of Rehabilitation and Physical Medicine, Kyung-Hee Medical Center, Seoul, Korea for swallowing evaluation between May 2011 and January 2013. Both inpatients and outpatients were included in the study. The subjects included stroke patients (1) who had a first-ever unilateral stroke, confirmed by MRI and/or CT and were older than 50 years of age; (2) who had symptoms and/or signs of dysphagia after onset of the stroke (choking, cough, wet voice after swallowing or a history of aspiration pneumonia); (3) who were evaluated by VFSS; and (4) who could follow the physiotherapist's orders.
All patients were alert, had an adequate level of consciousness and were able to complete the tasks required for the study. Analysis was performed in 96 patients with non-traumatic cerebral infarction or hemorrhage. The patients ranged in age from 40 to 88 years, with a mean age of 63.75 years. The mean age of the 45 male participants was 63.57 years (range, 41–88 years), and that of the 51 female patients was 63.91 years (range, 40–82 years). Measurements were performed 1–12 months after the stroke (median, 3.8 months post-onset). The dysphagic group included 40 patients (41.6%) with cerebral infarction and 56 patients (58.3%) with cerebral hemorrhage. Of these patients, 38 (39.5%) had right hemiplegic stroke and 58 (60.4%) had left hemiplegia (Table 1).
Table 1. Characteristics of stroke patients (n=96).
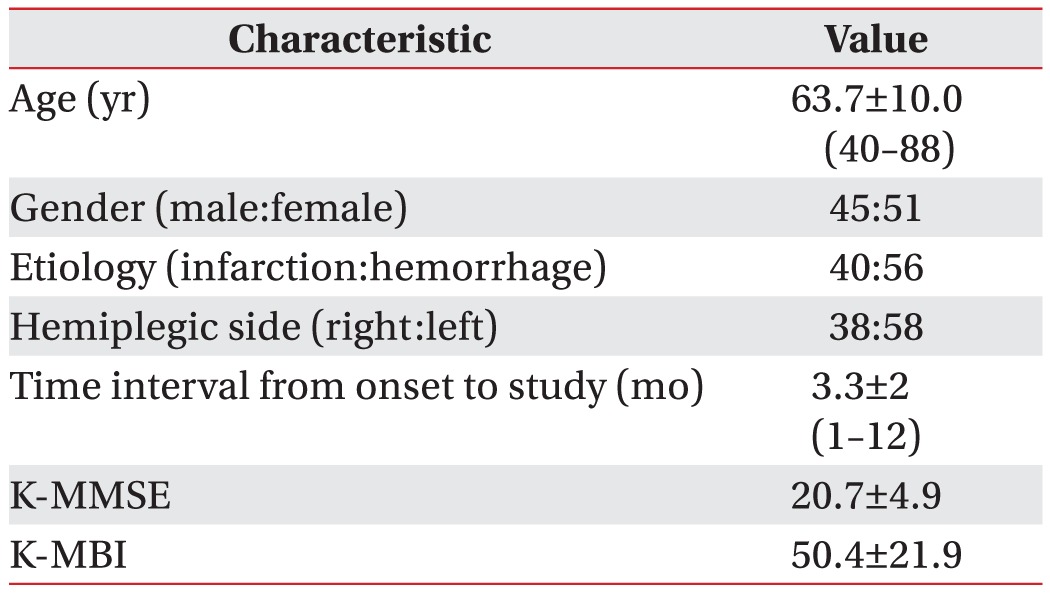
Values are presented as mean±standard deviation (range).
K-MMSE, the Korean version of Mini-Mental State Examination; K-MBI, the Korean version of Modified Barthel Index.
VFSS protocol
The swallowing ability of patients with stroke was evaluated by a VFSS, which was performed as described below [5,13]. A modified version of Logemann [14] protocol was used. Patients were initially instructed to sit upright for 5 seconds to assess their ability to maintain posture. The videofluoroscopy instrument was positioned lateral to the patient. Liquid barium (40% weight/volume, barium sulfate, Solotop suspension) was diluted with yogurt (the viscosity was around 1,000 centipoise [cP]). First, the patients were given 5 mL of yogurt to swallow using a syringe. Afterwards, 4 g of cooked rice with barium was given using a spoon (the viscosity was above 1,750 cP). If the patients swallowed without aspiration or penetration, 5 mL of water with diluted barium (the viscosity was 1–50 cP) was given using a syringe. The entire clinical procedure was recorded with a video camera. Results of the first videofluoroscopy procedure were used for our analysis.
Interpretation
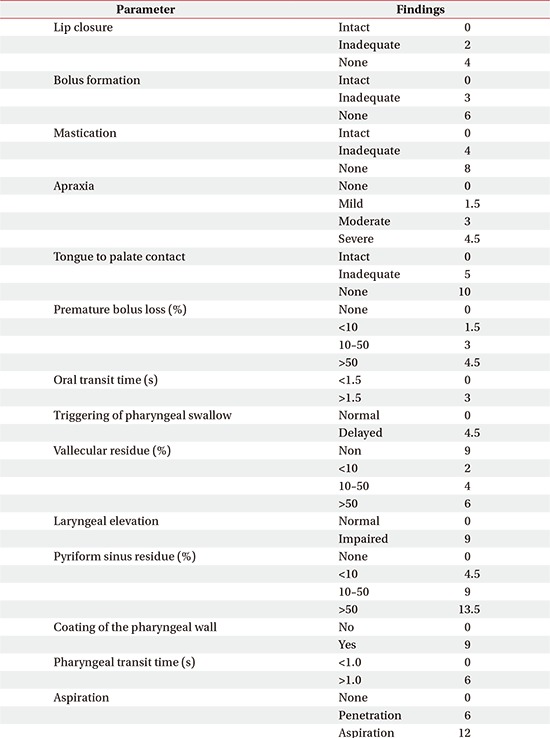
The swallowing process in the oral phase was evaluated with the videofluoroscopic dysphagia scale (VDS) (Appendix 1) [15], which consists of the following 14 items: oral phase (lip closure, bolus formation, mastication, apraxia, premature bolus loss, and oral transit time) and pharyngeal phase (pharyngeal triggering, vallecular and pyriform sinus residues, laryngeal elevation and epiglottic closure, pharyngeal coating, pharyngeal transit time, and aspiration) that can be assessed by the VFSS. All of the outcome scales were rated by two skilled physicians who had been trained in VFSS for at least 3 years. The physicians analyzed the video files and drew consensual conclusions.
In the oral phase, the completeness of lip closure (LC), bolus formation (BF), mastication, and tongue-to-palate contact (TP) were measured. The examiner categorized the results into three levels according to the degree (intact, 0; inadequate, 4; none, 8). Oral transit time (OTT) was also measured from the time the bolus started to move from the oral cavity to the lower edge of the mandibular ramus. More than 1.5 seconds of OTT was defined as the delayed oral phase. The degree of apraxia was evaluated in terms of four levels (none, 0; mild, 1.5; moderate, 3; severe, 4.5).
The amount of premature bolus loss (PBL), which pertains to the bolus drop into the pharynx from the oral cavity before the swallowing reflex, was classified into four levels (grade 0, none; grade 1, 10% of bolus; grade 2, from 10% to 50% of bolus; grade 3, >50% of bolus) [15]. To minimize the examiners' subjective error, we also compared the results by dividing the group based on the presence of PBL.
Measurement of tongue pressure
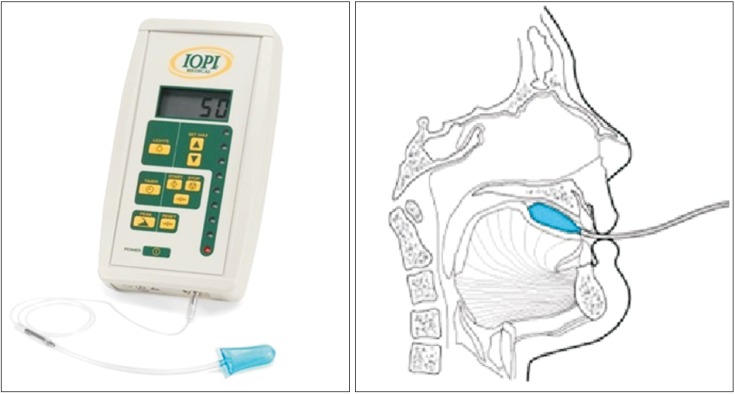
Subjective measures of tongue pressure were obtained using the Iowa Oral Performance Instrument (IOPI), a device that has been described in several previous reports [16,17]. The IOPI consists of a pressure transducer and an amplifier that displays, in kilopascals (kPa), the pressure exerted on an air-filled bulb (Fig. 1).
Fig. 1. Positioning of the air-filled lingual pressure sensor of the Iowa Oral Performance Instrument between the tongue and an oral structure.
Subjects were seated upright and asked to press their tongue against the IOPI bulb as hard as possible. Only valid (i.e., the bulb was properly positioned and pressure was applied by the tongue) trials of maximum performance for lip closure pressure (LP), anterior hard palate-to-tongue pressure (AP), posterior hard palate-to-tongue pressure (PP), and buccal pressure on both sides were recorded (buccal-to-tongue pressure on the weak side [BW]; buccal-to-tongue pressure on the healthy side [BH]). Each parameter was evaluated separately. The average pressure in the three trials was compared between the groups.
Functional outcomes
Scores on the MBI were used to evaluate ADL. The K-MBI score is commonly used as a valid and reliable measure to determine functional ability with respect to 10 domains, and total scores range from 0 (totally dependent) to 100 (totally independent) [18]. K-MMSE, which was used to evaluate cognitive function, tests five domains of cognitive function: orientation, attention, calculation, language, and construction. Total scores range from 0 to 30, and higher K-MMSE scores indicate better cognition [19].
Statistical analysis
We compared the groups statistically using the SPSS software ver. 20.0 K for Windows (SPSS Inc., Chicago, IL, USA).
The Mann–Whitney U-test was used to analyze the relationships between tongue pressure and different aspects of the oral-phase swallowing function. The Jonckheere–Terpstra test was used to compare the linear correlation between PBL and tongue pressure. Statistical significance was set at p<0.05.
RESULTS
The patients were divided into groups based on the intactness of the oral phase according to the VDS scale. The average differences in tongue pressure were observed between the groups. Apraxia was not compared in this study because only 1 patient had oral-phase apraxia.
Lip closure
Patients were classified into three groups (intact, 0; inadequate, 2; none, 4), but none of the patients met the criteria for the 'none' group. The intact and inadequate groups were compared. The average maximum LP was 13.8 kPa (SD=4.1) in the intact LC group (n=81) and 12.0 kPa (SD=5.3) in the inadequate LC group (n=15); this difference was not statistically significant (p=0.181). However, the average maximum AP and PP values in the intact LC group were significantly higher than those in the inadequate LC group (AP, p=0.003; PP, p<0.001). The two groups did not differ significantly with respect to K-MMSE and MBI scores (Table 2).
Table 2. The relationships of LP, tongue pressure, and functional outcome with lip closure and bolus formation (unit, kPa).
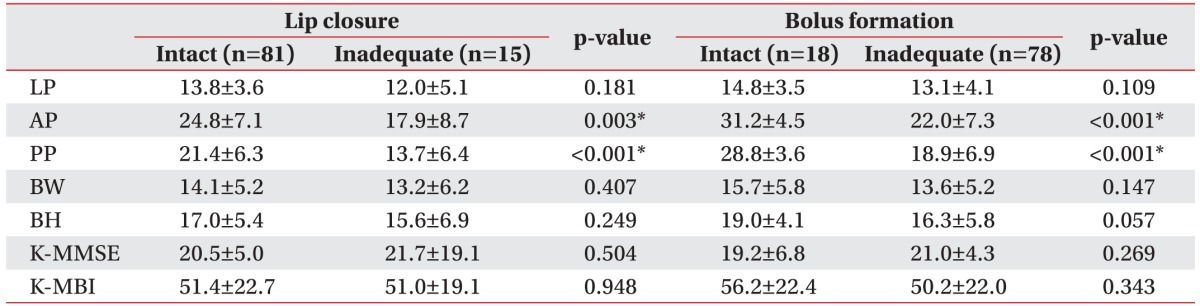
Values are presented as mean±standard deviation.
LP, lip pressure; AP, anterior hard palate-to-tongue pressure; PP, posterior hard palate-to-tongue pressure; BW, buccal-to-tongue pressure on the weak side; BH, buccal-to-tongue pressure on the healthy side; K-MMSE, the Korean version of Mini-Mental State Examination; K-MBI, the Korean version of Modified Barthel Index.
*p<0.05, Mann–Whitney U test.
Bolus formation
Eighteen patients showed intact BF and 78 patients showed inadequate BF. BF was significantly correlated with AP and PP. The average maximum AP and PP values were significantly higher in the intact BF group than in the inadequate BF group (AP, p<0.001; PP, p<0.001). However, there was no significant difference between the groups with respect to the other parameters (Table 2).
Mastication
Patients with normal mastication (n=82) had significantly higher AP and PP values than patients with inadequate mastication (n=14; AP, p<0.001; PP, p<0.001). Additionally, there was a significant difference in buccal-totongue pressure on both sides and LP between the intact mastication and inadequate mastication groups (Table 3).
Table 3. The relationships of LP, tongue pressure, and functional outcome with mastication and oral transit time (unit, kPa).
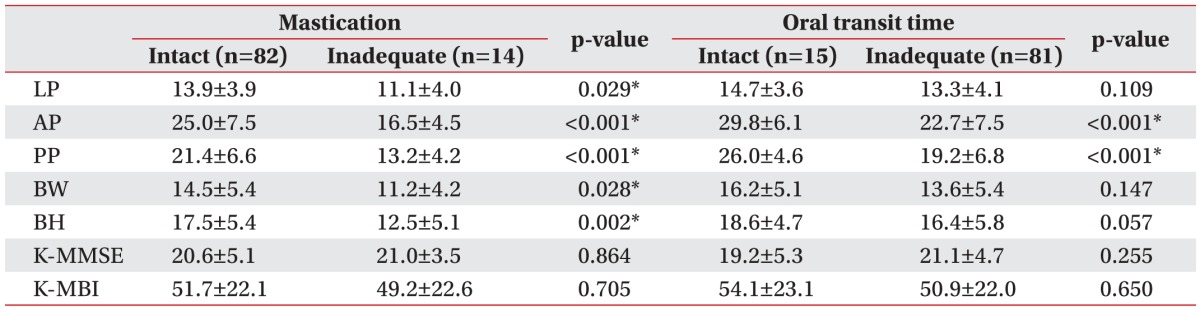
Values are presented as mean±standard deviation.
LP, lip pressure; AP, anterior hard palate-to-tongue pressure; PP, posterior hard palate-to-tongue pressure; BW, buccal-to-tongue pressure on the weak side; BH, buccal-to-tongue pressure on the healthy side; K-MMSE, the Korean version of Mini-Mental State Examination; K-MBI, the Korean version of Modified Barthel Index.
*p<0.05, Mann–Whitney U test.
Oral transit time
Like other dysphagia scales, AP and PP were significantly correlated with OTT in our study. This correlation was negative, indicating that increased pressure was associated with shorter OTT. According to the VDS, patients were divided into two groups depending on OTT (<1.5 seconds vs. ≥1.5 seconds). The average maximum AP and PP values in the normal OTT group were significantly higher than those in the delayed OTT group (AP, p<0.001; PP, p<0.001). There was no significant correlation between K-MMSE scores and OTT (Table 3).
Premature bolus loss
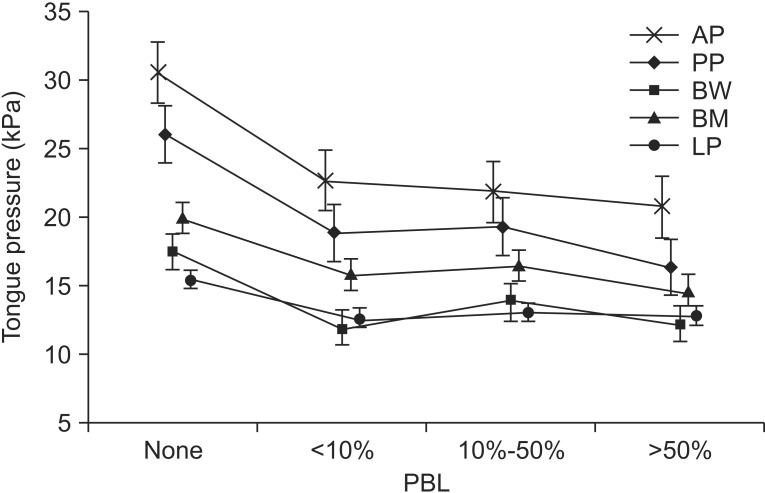
When we divided the patients into groups according to the presence of PBL, tongue pressure was associated with PBL (AP, p<0.001; PP, p<0.001; BW, p=0.001; BH, p=0.002; LP, p=0.006) (Table 4), as was the case with the other oral-phase dysphagia scales. The VDS classifies the amount of premature bolus loss into four levels. We compared these levels with tongue pressure, and the linear correlation between PBL and tongue pressure was tested with the Jonckheere–Terpstra rank correlation test. We found that a larger amount of PBL was associated with a lower maximal tongue pressure (AP, p<0.001; PP, p<0.001; BW, p=0.011; BH, p=0.008; LP, p=0.033) (Fig. 2).
Table 4. The relationships of LP, tongue pressure, and functional outcome with premature bolus loss and tongue-topalate contact (unit, kPa).
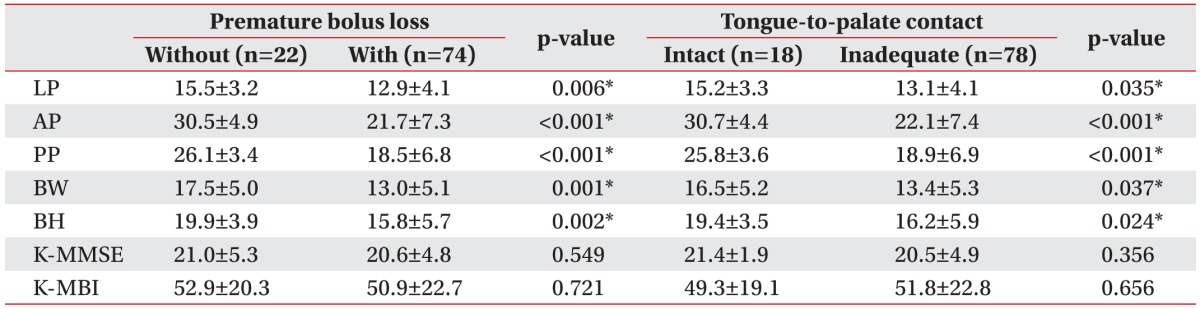
Values are presented as mean±standard deviation.
LP, lip pressure; AP, anterior hard palate-to-tongue pressure; PP, posterior hard palate-to-tongue pressure; BW, buccal-to-tongue pressure on the weak side; BH, buccal-to-tongue pressure on the healthy side; K-MMSE, the Korean version of Mini-Mental State Examination; K-MBI, the Korean version of Modified Barthel Index.
*p<0.05, Mann–Whitney U test.
Fig. 2. Correlation between premature bolus loss (PBL) and mean tongue pressure. A larger amount of PBL was associated with a lower maximal tongue pressure (Jonckheere– Terpstra rank correlation test, p<0.05). AP, anterior hard palate-to-tongue pressure; PP, posterior hard palate-to-tongue pressure; BW, buccal-to-tongue pressure on the weak side; BH, buccal-to-tongue pressure on the healthy side; LP, lip closure pressure.
Tongue-to-palate contact
Like PBL, TP was correlated with all five parameters (AP, p<0.001; PP, p<0.001; BW, p=0.037; BH, p=0.024; LP, p=0.035) (Table 4).
DISCUSSION
Previous studies have revealed that tongue pressure is a good predictor of the presence of oral-phase swallowing impairment, especially for BF, mastication, and oral clearance [8,20].
Robbins et al. [21] reported that an 8-week lingual resistance exercise program showed promising results with respect to preventing dysphagia due to sarcopenia and serving as a treatment strategy for patients with lingual weakness and swallowing disorders. Their results suggest that increasing tongue pressure with lingual exercises could be helpful in improving oral dysphagia.
We found that AP and PP were related to all phases of oral swallowing. This indicates that forward and backward tongue movements, such as tongue protrusion and retraction, were more important factors in oral-phase swallowing than lateral tongue movements. Only PBL, TP, and mastication were correlated with buccal-to-tongue pressure on both sides.
In the present study, LC was not related to the degree of LP, but it was significantly associated with AP and PP. In stroke patients, inadequate LC is frequently found in patients with facial palsy. Hagg and Anniko [22], who studied the association between LP and swallowing capacity, found that LP did not differ according to whether or not facial palsy was present. However, LP was significantly lower in stroke patients than in healthy subjects. These factors may indicate that LC has no relation with LP.
Tongue movement is also an important factor in holding the bolus. While drinking a liquid substance, the posterior oral cavity is sealed by tongue–palate contact during the oral preparatory stage when the bolus is held in the oral cavity [23]. Clark et al. [8] measured tongue strength with the IOPI and found that holding and manipulating the bolus were most strongly correlated with subjective measures of tongue strength. Like this previous study, we also found that PBL was related to all five parameters.
To the best of our knowledge, this is the first published study that examined the relationship between tongue pressure and functional outcomes. The K-MMSE and K-MBI results showed no significant differences in each oral phase between the intact and inadequate groups. Moon et al. [24] studied the cognition factors affecting oral-phase dysphagia in stroke patients. In contrast to our study, they found that inadequate LC and PBL were associated with low K-MMSE scores. However, we found no correlation between K-MMSE scores and any phase of oral dysphagia. Unlike the previous study, we included dementia patients who could follow our simple steps in order. Thus, their inclusion criteria differed from our criteria.
This study has several limitations. First, the evaluation of mastication, TP and amount of PBL may vary from physician to physician. Although two experienced rehabilitation physicians interpreted the VFSS, the results were subjective. Kim et al. [25] also demonstrated that VDS showed a lower rate of inter-rater agreement in the oral-phase parameters. Second, there was no healthy control group. Third, the timing of the study varied, as each patient had a different onset time depending on when the patient was referred to our rehabilitation center. Finally, the possible correlation between the location of the brain lesion and tongue pressure was not considered in this study. In cases of medullary infarction, with involvement of the hypoglossal nerve, ipsilateral tongue deviation and tongue movement disorder may be observed. Further study is needed to evaluate these limitations.
In summary, the findings of this study demonstrate the relationship of tongue weakness, as measured by tongue pressure, with oral-phase dysphagia in post-stroke patients. This suggests that patients with tongue-movement weakness during oral swallowing are at high risk for oral-phase dysphagia. However, the ways in which tongue weakness affects oral-phase swallowing remain unclear. Thus, further study is needed to precisely determine the relationship between tongue pressure and the oral-phase swallowing function.
Appendix 1
Videofluoroscopic dysphagia scale [15]
Footnotes
CONFLICT OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
- 1.Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005;36:2756–2763. doi: 10.1161/01.STR.0000190056.76543.eb. [DOI] [PubMed] [Google Scholar]
- 2.Smithard DG, O'Neill PA, Parks C, Morris J. Complications and outcome after acute stroke. Does dysphagia matter? Stroke. 1996;27:1200–1204. doi: 10.1161/01.str.27.7.1200. [DOI] [PubMed] [Google Scholar]
- 3.Dodds WJ, Stewart ET, Logemann JA. Physiology and radiology of the normal oral and pharyngeal phases of swallowing. AJR Am J Roentgenol. 1990;154:953–963. doi: 10.2214/ajr.154.5.2108569. [DOI] [PubMed] [Google Scholar]
- 4.Daniels SK, Brailey K, Foundas AL. Lingual discoordination and dysphagia following acute stroke: analyses of lesion localization. Dysphagia. 1999;14:85–92. doi: 10.1007/PL00009592. [DOI] [PubMed] [Google Scholar]
- 5.Logemann JA. Evaluation and treatment of swallowing disorders. 2nd ed. Austin: Pro-Ed; 1998. [Google Scholar]
- 6.Konaka K, Kondo J, Hirota N, Tamine K, Hori K, Ono T, et al. Relationship between tongue pressure and dysphagia in stroke patients. Eur Neurol. 2010;64:101–107. doi: 10.1159/000315140. [DOI] [PubMed] [Google Scholar]
- 7.Ku DN, Ma PP, McConnel FM, Cerenko D. A kinematic study of the oropharyngeal swallowing of a liquid. Ann Biomed Eng. 1990;18:655–669. doi: 10.1007/BF02368453. [DOI] [PubMed] [Google Scholar]
- 8.Clark HM, Henson PA, Barber WD, Stierwalt JA, Sherrill M. Relationships among subjective and objective measures of tongue strength and oral phase swallowing impairments. Am J Speech Lang Pathol. 2003;12:40–50. doi: 10.1044/1058-0360(2003/051). [DOI] [PubMed] [Google Scholar]
- 9.Horner J, Massey EW. Silent aspiration following stroke. Neurology. 1988;38:317–319. doi: 10.1212/wnl.38.2.317. [DOI] [PubMed] [Google Scholar]
- 10.Roth EJ. Medical complications encountered in stroke rehabilitation. Phys Med Rehabil Clin North Am. 1991;2:563–577. [Google Scholar]
- 11.DePippo KL, Holas MA, Reding MJ, Mandel FS, Lesser ML. Dysphagia therapy following stroke: a controlled trial. Neurology. 1994;44:1655–1660. doi: 10.1212/wnl.44.9.1655. [DOI] [PubMed] [Google Scholar]
- 12.Falsetti P, Acciai C, Palilla R, Bosi M, Carpinteri F, Zingarelli A, et al. Oropharyngeal dysphagia after stroke: incidence, diagnosis, and clinical predictors in patients admitted to a neurorehabilitation unit. J Stroke Cerebrovasc Dis. 2009;18:329–335. doi: 10.1016/j.jstrokecerebrovasdis.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 13.Han TR, Paik NJ, Park JW. Quantifying swallowing function after stroke: a functional dysphagia scale based on videofluoroscopic studies. Arch Phys Med Rehabil. 2001;82:677–682. doi: 10.1053/apmr.2001.21939. [DOI] [PubMed] [Google Scholar]
- 14.Logemann JA. Manual for the videofluorographic study of swallowing. 2nd ed. Austin: Pro-Ed; 1993. [Google Scholar]
- 15.Han TR, Paik NJ, Park JW, Kwon BS. The prediction of persistent dysphagia beyond six months after stroke. Dysphagia. 2008;23:59–64. doi: 10.1007/s00455-007-9097-0. [DOI] [PubMed] [Google Scholar]
- 16.Robbins J, Levine R, Wood J, Roecker EB, Luschei E. Age effects on lingual pressure generation as a risk factor for dysphagia. J Gerontol A Biol Sci Med Sci. 1995;50:M257–M262. doi: 10.1093/gerona/50a.5.m257. [DOI] [PubMed] [Google Scholar]
- 17.Park JS, You SJ, Kim JY, Yeo SG, Lee JH. Differences in orofacial muscle strength according to age and sex in East Asian healthy adults. Am J Phys Med Rehabil. 2015;94:677–686. doi: 10.1097/PHM.0000000000000230. [DOI] [PubMed] [Google Scholar]
- 18.Shah S, Vanclay F, Cooper B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol. 1989;42:703–709. doi: 10.1016/0895-4356(89)90065-6. [DOI] [PubMed] [Google Scholar]
- 19.Kang Y, Na DL, Hahn S. A validity study on the Korean Mini-Mental State Examination (K-MMSE) in dementia patients. J Korean Neurol Assoc. 1997;15:300–308. [Google Scholar]
- 20.Pouderoux P, Kahrilas PJ. Deglutitive tongue force modulation by volition, volume, and viscosity in humans. Gastroenterology. 1995;108:1418–1426. doi: 10.1016/0016-5085(95)90690-8. [DOI] [PubMed] [Google Scholar]
- 21.Robbins J, Gangnon RE, Theis SM, Kays SA, Hewitt AL, Hind JA. The effects of lingual exercise on swallowing in older adults. J Am Geriatr Soc. 2005;53:1483–1489. doi: 10.1111/j.1532-5415.2005.53467.x. [DOI] [PubMed] [Google Scholar]
- 22.Hagg M, Anniko M. Influence of lip force on swallowing capacity in stroke patients and in healthy subjects. Acta Otolaryngol. 2010;130:1204–1208. doi: 10.3109/00016481003745550. [DOI] [PubMed] [Google Scholar]
- 23.Matsuo K, Palmer JB. Anatomy and physiology of feeding and swallowing: normal and abnormal. Phys Med Rehabil Clin N Am. 2008;19:691–707. doi: 10.1016/j.pmr.2008.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moon HI, Pyun SB, Kwon HK. Correlation between location of brain lesion and cognitive function and findings of videofluoroscopic swallowing study. Ann Rehabil Med. 2012;36:347–355. doi: 10.5535/arm.2012.36.3.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim DH, Choi KH, Kim HM, Koo JH, Kim BR, Kim TW, et al. Inter-rater reliability of videofluoroscopic dysphagia scale. Ann Rehabil Med. 2012;36:791–796. doi: 10.5535/arm.2012.36.6.791. [DOI] [PMC free article] [PubMed] [Google Scholar]