Abstract
Introduction
Myiasis, parasitic infestation of the body by fly larvae, caused by the Cordylobia rodhaini is very rare with only fourteen cases published since 1970. We present a rare case of myiasis mimicking a breast abscess.
Presentation of case
A 17-year-old female presented with a nodular ulcerative lesion in her left breast 14 days following a trip to Ghana. She had been initially unsuccessfully treated with the antibiotic flucloxacillin following a misdiagnosis of a breast abscess. Following application of Vaseline to the breast wound, covering the wound for 2 h and gentle manipulation the larvae was removed successfully and the patient made a good recovery.
Discussion
Presenting as an inflammatory papule with central opening oozing serosanguinous fluid myiasis secondary to C. rodhaini can easily be mistaken for a breast abscess, often avoiding detection by unsuspecting surgeons on initial assessment. In turn ineffective antibiotic treatment is often prescribed leading to further disease progression and associated morbidity.
Conclusion
Myiasis secondary to C. rodhaini is a rare but important differential surgeons should consider in women presenting with an inflammatory breast lesion with a recent history of foreign travel to ensure timely diagnosis and treatment. Ultrasound imaging can be useful in confirming diagnosis and avoiding treatment delays.
Keywords: Cordylobia rodhaini, Myiasis, Breast abscess, Fly larvae
1. Introduction
Myiasis refers to the parasitic infestation of a mammal’s body by fly larvae which feed on its tissue. Cordylobia is a fly belonging to the Calliphoridae family of which there are three species. C. rodhaini was initially named “Lund’s fly”, after the surname of Captain Lund who witnessed the first recorded patient affected by myiasis due to C. rodhaini and himself had a larva extracted from his arm in Congo [1]. Originating in Sub-Saharan Africa and most prevalent in rain-forest regions its usual hosts are small mammals, in particular rodents and small antelopes, though humans can also become infested [2]. Myiasis caused by the larvae of C. rodhaini is very rare with only 14 cases reported in published literature [1], [2], [3], [4], [5], [6], [7], [8], [9], [10]. We present a case of Cordylobia rodhaini myasis acquired in Ghana mimicking a breast abscess.
2. Presentation of case
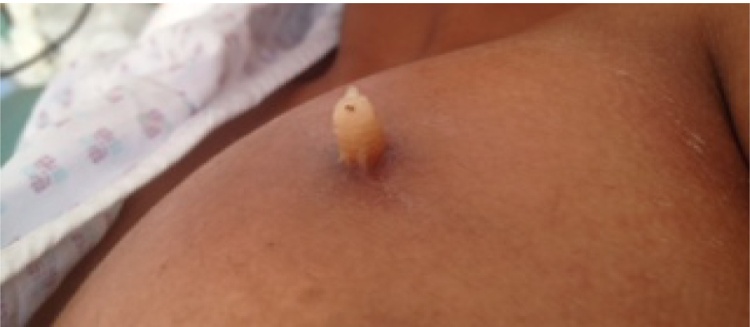
A 17 year old female presented with a nodular ulcerative lesion in her left breast initially treated with antibiotic (Flucloxacillin 500 mg four times daily) upon a diagnosis of breast abscess. The patient returned from a voyage in Ghana fourteen days before attending our Emergency department and seventeen days before she was seen in our breast clinic. Following application of Vaseline to the breast wound, covering the wound for 2 h and gentle manipulation the larvae was removed (see Fig. 1, Fig. 2) successfully and the patient made a good recovery.
Fig. 1.
Myiasis left breast: larvae leaving wound.
Fig. 2.
Cordylobia rodhaini larvae.
3. Discussion
C. rodhaini commences its 28 day life cycle with the female fly depositing her eggs on dry sand, or in the case of human infestation on clothing with their eggs hatching in approximately 3 days [1], [2]. Once activated by body warmth the larvae penetrate the skin and over the next 15 days they can reach length on 1.5 cm at maturity and emerge from the skin spontaneously. Throughout this process they induce initially a red papule which becomes a furuncular swelling on the skin giving rise to the term ‘furuncular myiasis’ [2]. The adult fly emerges in 23–26 days and the life cycle resumes. Larvae breath and release their serosanguinous fluid faeces through an opening at the centre of the lesion which is associated with increasing pain for the host until the larvae emerges. Epidemiologically, myiasis secondary to C. rodhaini is most common in those with recent travel to central and sub-Saharan Africa: Cameroon [2], [4], Kenya [3], Ethiopia [1], [2], [6], [9], Uganda [2], [10] and Ghana [8]. The number of body lesions on an infested host is variable ranging from one to fifteen [2], and in one extreme case a patient was found to be infested with 150 larvae at multiple body sites [1]. Systemic symptoms are less common but can manifest as fever or lymphadenopathy [1], [6]. Haematological and immunological investigation can reveal a neutrophilic leucocytosis associated with increased IgA [1]. Use of ultrasound (US) in the emergency department has been shown to be useful in detection of cutaneous myiasis demonstrating spontaneous movement immediately beneath the skin [11], [12]. Other US findings include fusiform hyperechoic mass surrounded by a hypoechoic halo and in an observational study of 25 cases US was shown to prevent misdiagnosis and treatment delays [13], [14]. Mammographic appearances of cutaneous myiasis include indistinct masses associated with pairs of microcalcifications [13]. As previously mentioned, mature larvae may emerge from the skin spontaneously [6], for this reason sometimes no treatment is necessary. In order to force the larvae to emerge some authors applied petrolatum [7], [8]. In our patient, evacuation of the larvae was achieved by applying Vaseline over the opening and a sealing the dressing for 2 h. After removing the dressing with gentle manual pressure at the edge of the lesion the larva was removed. If conservative management fails then surgical management can be pursued to mechanically remove the larvae. Potential longer lasting complications include hyperpigmentation which may persist on the skin of the affected area for several months [6].
4. Conclusion
Presenting as an inflammatory papule with central opening oozing serosanguinous fluid myiasis secondary to C. rodhaini can easily be mistaken for a breast abscess, often avoiding detection by unsuspecting surgeons on initial assessment. Myiasis secondary to C. rodhaini is a rare but important differential surgeons should consider in women presenting with an inflammatory breast lesion with a recent history of foreign travel to ensure timely diagnosis and appropriate treatment. Ultrasound imaging can be useful in confirming diagnosis and avoiding treatment delays.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Veronica Grassi: involved in study concept, data analysis and writing the paper.
James W. Butterworth: involved in study design, data collection, data analysis and writing the paper.
Layloma Latiffi: involved in study concept, data collection and writing the paper.
Conflicts of interest
None.
Guarantor
Miss Grassi (Consultant Breast Surgeon).
Source of funding
No funding provided/recieved.
Ethical approval
NA.
Acknowledgment
My sincerest thanks to the library staff who facilitated a broad literature search for this article through use of their resources.
References
- 1.Pampiglione S., Schiavon S., Candiani G., Fioravanti M.L. Clinical and parasitological observations on a case of disseminated furuncular myiasis caused by Cordylobia rodhaini in a man in Ethiopia. Parassitologia. 1991;33:159–167. (Article in Italian) [PubMed] [Google Scholar]
- 2.Veraldi Stefano, Serini Stefano Maria, Süss Luciano. Three cases of cutaneous myiasis caused by Cordylobia rodhaini. J. Infect. Dev. Countries. 2014;8:249–251. doi: 10.3855/jidc.3825. [DOI] [PubMed] [Google Scholar]; Kremer M., Lenys J., Basset M., Rombourg H., Molet B. Deux cas de myiase à Cordylobia rhodaini contracteé au Cameroun et diagnosticeé en Alsace. Bull. Soc. Pathol. Exot. 1970;63:592–596. [PubMed] [Google Scholar]
- 3.Scholten T.H., Hicks R.J. Myiasis by Cordylobia rodhaini contracted in Africa and diagnosed in Canada. Can. J. Public Health. 1973;64:488–489. [PubMed] [Google Scholar]
- 4.Hori E., Yamaguchi K., Wada Y., Yamamura H., Kano R., Shinonaga S., Fujino N. Three human cases of myiasis caused by larvae of Cordylobia (Calliphoridae) in Cameroon and Côte d’Ivoire, West Africa. Jpn. J. Med. Zool. 1984;35:87–90. [Google Scholar]
- 5.Hubsch H.M., Kalvelage H., Bercher M. Fliegenlarvenbefall der haut (Cutane Myiasis) durch Cordylobia rodhaini. Akt. Dermatol. 1989;15:243–245. [Google Scholar]
- 6.Pampiglione S., Schiavon S., Fioravanti M.L. Extensive furuncular myiasis due to Cordylobia rodhaini larvae. Br. J. Dermatol. 1992;126:418–419. doi: 10.1111/j.1365-2133.1992.tb00698.x. [DOI] [PubMed] [Google Scholar]
- 7.Geary M.J., Hudson B.J., Russell R.C., Hardy A. Exotic myiasis with Lund’s fly (Cordylobia rodhaini) Med. J. Aust. 1999;171:654–655. doi: 10.5694/j.1326-5377.1999.tb123838.x. [DOI] [PubMed] [Google Scholar]
- 8.Tamir J., Haik J., Schwartz E. Myiasis with Lund’s fly (Cordylobia rodhaini) in travelers. J. Travel Med. 2003;10:293–295. doi: 10.2310/7060.2003.2732. [DOI] [PubMed] [Google Scholar]
- 9.Hannam P., Khairnar K., Downey J., Povis J., Ralevski F., Pillai D.R. Cutaneous myiasis in traveler returning from Ethiopia. Emerg. Infect. Dis. 2011;17:2385–2386. doi: 10.3201/eid1712.111062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pezzi M., Cultrera R., Chicca M., Leis M. Furuncular myiasis caused by cordylobia rodhaini (Diptera: Calliphoridae): a case report and a literature review. J. Med. Entomol. 2015;52:151–155. doi: 10.1093/jme/tju027. [DOI] [PubMed] [Google Scholar]
- 11.Hannam P., Khairnar K., Downey J., Powis J., Ralevski F., Pillai D.R. Cutaneous myiasis in traveler returning from Ethiopia. Emerg. Infect. Dis. 2011;17:2385–2386. doi: 10.3201/eid1712.111062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schechter E., Lazar J., Nix M.E., Mallon W.K., Moore C.L. Identification of subcutaneous myiasis using bedside emergency physician performed ultrasound. J. Emerg. Med. 2011;40:1–3. doi: 10.1016/j.jemermed.2007.11.095. [DOI] [PubMed] [Google Scholar]
- 13.De Barros N., D'Avila M.S., de Pace Bauab S., Issa F.K., Freitas F.J., Kim S.J. Cutaneous myiasis of the breast: mammographic and us features-report of five cases. Radiology. 2001;218:517–520. doi: 10.1148/radiology.218.2.r01fe16517. [DOI] [PubMed] [Google Scholar]
- 14.Quintanilla-Cedillo M.R., León-Ureña H., Contreras-Ruiz J., Arenas R. The value of Doppler ultrasound in diagnosis in 25 cases of furunculoid myiasis. Int. J. Dermatol. 2005;44:34–37. doi: 10.1111/j.1365-4632.2004.02471.x. [DOI] [PubMed] [Google Scholar]