Abstract
We present the cases of two patients with bioprosthetic aortic valves who developed an allergy to alpha-gal. Each had premature degeneration of their bioprosthesis and demonstrated rapidly increasing transvalvular gradients after development of their allergy. Each underwent successful replacement with a mechanical aortic valve within 1–2 years of symptom onset.
Allergy to mammalian meat is increasingly prevalent around the world.1 Patients develop anaphylactic reactions after eating beef, pork, or lamb. Commins and colleagues were among the first to report on mammalian meat allergy to galactose-alpha-1,3-galactose (alpha-gal).1 The alpha-gal oligosaccharide is a blood group structure evolutionarily conserved in most non-primate mammalian species. While ingestion of this antigen is harmless, inoculation by the lone star tick (Amblyomma americanum) induces both an IgG1 and IgE response, and is thought to be the inciting event.2 As bioprosthetic valves and heparin are bovine or porcine-derived products, alpha-gal allergy may be a significant factor in valve surgery. Two patients at our institution were found to have a history of tick bites, elevated alpha-gal IgE titers, and development of mammalian meat allergy within the last two years. They presented with heart failure symptoms and evaluation demonstrated rapid degeneration of their bioprosthetic aortic valves.
PATIENT PROFILE
Case 1
A 39-year-old male with a history of IV drug abuse and endocarditis required aortic valve replacement (AVR) in 2004. He received a 23 mm Mosaic porcine bioprosthetic valve (Medtronic, Minneapolis, MN, USA) and through 2011 remained healthy and asymptomatic. In 2012, he developed urticaria six hours after eating steak, followed by similar episodes. In 2014, he developed progressive shortness of breath and an echocardiogram demonstrated severe aortic insufficiency and prosthetic valve deterioration (Fig. 1). His IgE level was found to be 485 IU/mL (reference range 10–180 IU/mL) with an alpha-gal specific IgE level >100 kU/L (reference range <0.35 kU/L), consistent with alpha-gal allergy. He underwent uncomplicated reoperative AVR with a 21 mm mechanical aortic valve (On-X, Austin, TX). Intraoperatively there was no evidence of endocarditis and his prosthetic valve leaflets were mostly destroyed. He was transitioned to warfarin using Bivalirudin and discharged to home.
Figure 1.
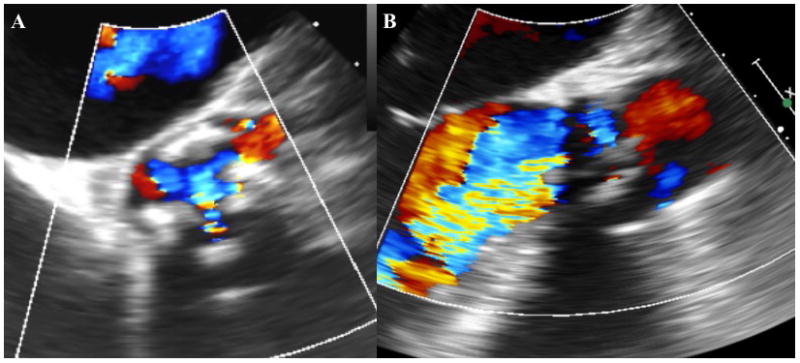
Case #1 transesophageal echocardiogram demonstrating severe aortic stenosis on short-axis view (A) and insufficiency on long-axis view (B).
Case 2
A 49-year-old male with a bicuspid aortic valve and severe stenosis had an AVR in 2009 with a 23 mm Magna Ease bovine pericardial aortic valve (Edwards Lifesciences, Irvine, CA, USA). In follow-up, he was noted to have an elevated mean gradient that was stable through the end of 2013 and ranged from 31 mmHg to 35 mmHg. In April 2014, he experienced chest pain and urticaria four hours after eating a hamburger. Throughout the year, recurrent anaphylactic reactions associated with meat consumption required several visits to the emergency department. Finally, an allergist completed diagnostic blood work that demonstrated an alpha-gal titer of 1.48 kU/L (reference range <0.35 kU/L). Avoiding red meat relieved his symptoms. However, within six months of symptom onset his mean transvalvular gradient increased from 35 mmHg to 69 mmHg. Four months later in 2015, he was admitted for chest pain and shortness of breath. He had a mean gradient of 82 mmHg causing demand ischemia. He underwent reoperation with a 21 mm mechanical valve (St. Jude, St. Paul, MN, USA) where the bioprosthesis demonstrated advanced calcific degeneration (Fig. 2). His postoperative course was uncomplicated and he was transitioned to Coumadin using Fondaparinux. He was discharged to home and is currently doing well.
Figure 2.
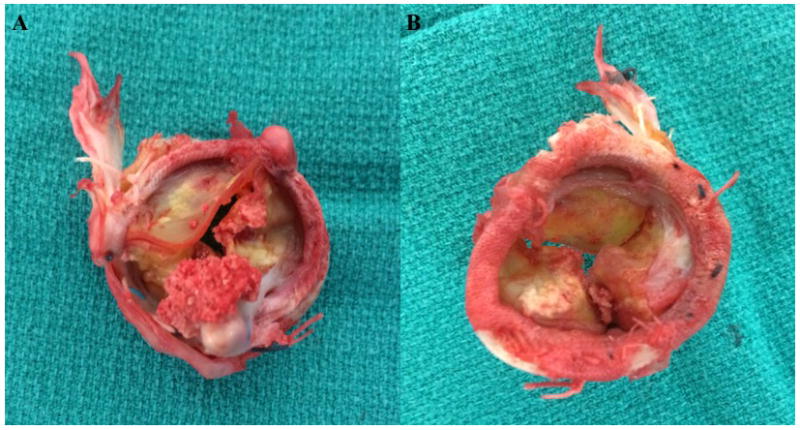
Case #2 gross specimen of calcified bioprosthetic aortic valve from superior (A) and inferior (B) views.
Institutional Review Board approval was not required according to institutional policy regarding case reports including two patients.
DISCUSSION
The experience of alpha-gal allergy in the context of bioprosthetic valves is extremely limited. In 2011, Fournier and colleagues reported a case of recurrent mitral valve vegetation requiring four tissue valve replacements.3 Post-mortem examination demonstrated eosinophilic infiltration of the valve and progressively increasing IgE levels, including to pork, although alpha-gal IgE was never tested. Most recently, three patients with known alpha-gal IgE titers experienced perioperative anaphylactic reactions after implantation of bioprosthetic valves.4 All three patients recovered well after appropriate treatment.
Prior work evaluating the immunologic activity against bioprosthetic valves demonstrated that the deposition of IgM and IgG immunoglobulins may trigger calcification. Konokci and colleagues demonstrated that the alpha-gal epitope is contained within the connective tissue of bioprosthetic valves.5 They postulated that a specific IgM-mediated response is mounted against alpha-gal after the bioprosthetic valve is implanted. This causes opsonization, macrophage recruitment, and ultimately valve degeneration. We hypothesize that the alpha-gal allergy may work through this pathway to cause early degeneration of bioprosthetic valves and further research is required to investigate these possible changes.
In patients with known alpha-gal sensitization, special considerations should be considered for valve replacement. Our patients may have developed accelerated valve degeneration after sensitization to alpha-gal. They required bioprosthetic valve replacement 10 and 6 years after implantation, and within 1–2 years of allergy development. While the exact durability of bioprosthetic valves in this population is unknown, mechanical valves may be preferred as they lack alpha-gal antigens. An additional consideration is the use of heparin. To date, no studies have defined the risk of heparin administration in this patient population. Our immunologists believe the risk for cross-reactivity is low. It is reasonable to use heparin for anticoagulation on cardiopulmonary bypass, as the alternatives are less desirable. Postoperatively, excellent alternatives exist and heparin can easily be avoided while bridging to oral anticoagulation.
CONCLUSION
To our knowledge, these are the first cases of premature bioprosthetic valve degeneration possibly associated with an alpha-gal allergy. We theorize that the IgE-mediated response to alpha-gal seen in these two patients is an accelerated version of the typical IgG/IgM-mediated process of alpha-gal targeted bioprosthesis calcification and degeneration. Special considerations may be considered for monitoring patients with bioprosthetic aortic valves who develop alpha-gal allergy. AVR with a mechanical valve is a reasonable consideration in patients with alpha-gal sensitivity.
Acknowledgments
Grant sponsor: National Institutes of Health; Grant number: T32 HL07849
Footnotes
Conflict of interest: The authors acknowledge no conflict of interest in the submission.
References
- 1.Commins SP, Satinover SM, Hosen J, et al. Delayed anaphylaxis, angioedema, or urticaria after consumption of red meat in patients with ige antibodies specific for galactose-alpha-1,3-galactose. J Allergy Clin Immunol. 2009;123:426–433. doi: 10.1016/j.jaci.2008.10.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Commins SP, James HR, Kelly LA, et al. The relevance of tick bites to the production of IgE antibodies to the mammalian oligosaccharide galactose-alpha-1,3-galactose. J Allergy Clin Immunol. 2011;127:1286–1293. doi: 10.1016/j.jaci.2011.02.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fournier PE, Thuny F, Grisoli D, et al. A deadly aversion to pork. Lancet. 2011;377:1542. doi: 10.1016/S0140-6736(11)60021-4. [DOI] [PubMed] [Google Scholar]
- 4.Mozzicato SM, Tripathi A, Posthumus JB, et al. Porcine or bovine valve replacement in 3 patients with IgE antibodies to the mammalian oligosaccharide galactose-alpha-1,3-galactose. J Allergy Clin Immunol Pract. 2014;2:637–638. doi: 10.1016/j.jaip.2014.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Konakci KZ, Bohle B, Blumer R, et al. Alpha-gal on bioprostheses: Xenograft immune response in cardiac surgery. Eur J Clin Invest. 2005;35:17–23. doi: 10.1111/j.1365-2362.2005.01441.x. [DOI] [PubMed] [Google Scholar]


