Highlights
-
•
We report a patient treated successfully via endovascular surgery within 24 h after intravenous thrombolysis using recombinant tissue plasminogen activator for acute cervical internal carotid artery occlusion.
-
•
Emergency carotid artery stenting for the acute internal carotid artery occlusion may be considered a safe procedure in preventing early stroke recurrence in selected patients.
-
•
When trying to perform emergency carotid artery stenting within 24 h after intravenous recombinant tissue plasminogen activator administration, several issues require attention, such as the decisions regarding the type of stent and embolic protection device, the selection of antiplatelet therapy and the methods of preventing hyper perfusion syndrome.
-
•
We administered aspirin and clopidogrel for the prevention of subacute thrombosis, and we used dexmedetomidine for preventing hyperperfusion syndrome, so that we also obtained a good result.
Abbreviations: IV, intravenous; rt-PA, recombinant tissue plasminogen activator; ICA, internal carotid artery; MCA, middle cerebral artery; HPS, hyperperfusion syndrome; CAS, carotid artery stenting; MRI, magnetic resonance imaging; MRA, magnetic resonance angiography; CCA, common carotid artery; PTA, percutaneous transluminal angioplasty; TICI, thrombolysis in cerebral infarction; SPECT, single photon emission tomography; EPD, embolic protection device
Keywords: Recombinant tissue plasminogen activator, Penumbra System, Emergency carotid artery stenting, Hyperperfusion syndrome, Subacute, Thrombosis, Dexmedetomidine
Abstract
Introduction
We report a patient treated successfully via endovascular surgery within 24 h after intravenous thrombolysis using recombinant tissue plasminogen activator for acute cervical internal carotid artery occlusion.
Presentation of case
A 68-year-old man was admitted to our hospital. Neurological examination revealed severe left-sided motor weakness. Magnetic resonance imaging showed no cerebral infarction, but magnetic resonance angiography revealed complete occlusion of the right internal carotid artery. Systemic intravenous injection of recombinant tissue plasminogen activator was performed within 4 h after the onset. But, magnetic resonance angiography still revealed complete occlusion. Revascularization of the right cervical internal carotid artery was performed via endovascular surgery. The occluded artery was successfully recanalized using the Penumbra System® and stent placement at the origin of the internal carotid artery. Immediately after surgery, dual antiplatelet therapy (aspirin and clopidogrel) was initiated, and then cilostazol was added on the following day. Carotid ultrasonography and three-dimensional computed tomographic angiography at 14 days revealed no further obstruction to flow.
Discussion
When trying to perform emergency carotid artery stenting within 24 h after intravenous recombinant tissue plasminogen activator administration, several issues require attention, such as the decisions regarding the type of stent and embolic protection device, the selection of antiplatelet therapy and the methods of preventing hyperperfusion syndrome.
Conclusion
Emergency carotid artery stenting for the acute internal carotid artery occlusion may be considered a safe procedure in preventing early stroke recurrence in selected patients.
1. Introduction
Generally, in patients with acute ischemic strokes, intravenous (IV) thrombolysis with recombinant tissue plasminogen activator (rt-PA) is employed to recanalize thrombosed intracranial vessels (such as the internal carotid artery (ICA) and the middle cerebral artery (MCA) and its branches) within 4.5 h [1], [2], [3]. In addition, various reports have been published that a combination of IV thrombolysis and early carotid revascularization via endovascular technique might be a more effective secondary stroke prevention strategy. On the other hand, during the first 24 h after IV rt-PA administration, the risk of intracranial hemorrhage associated with early reperfusion might be increased because of hyperperfusion syndrome (HPS) and the use of anticoagulant drugs or antiplatelet agents [3], [4], [5], [6], [7]. Here, we present a case of acute ICA occlusion treated successfully by use of the Penumbra System® and carotid artery stenting (CAS) within 24 h after IV thrombolysis using rt-PA.
2. Case report
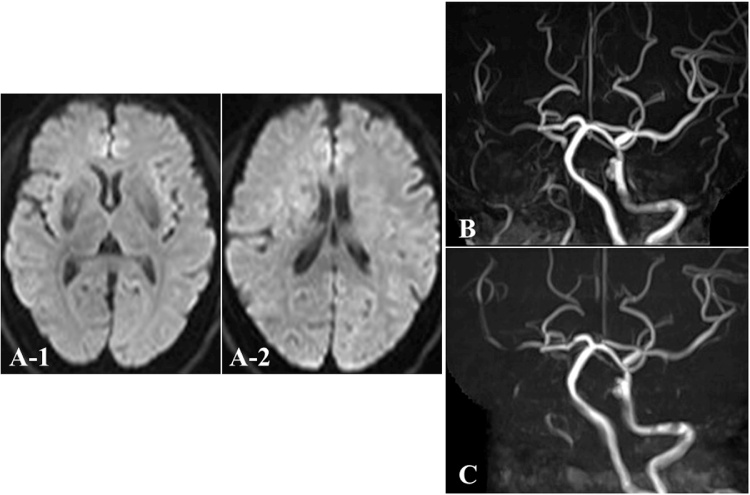
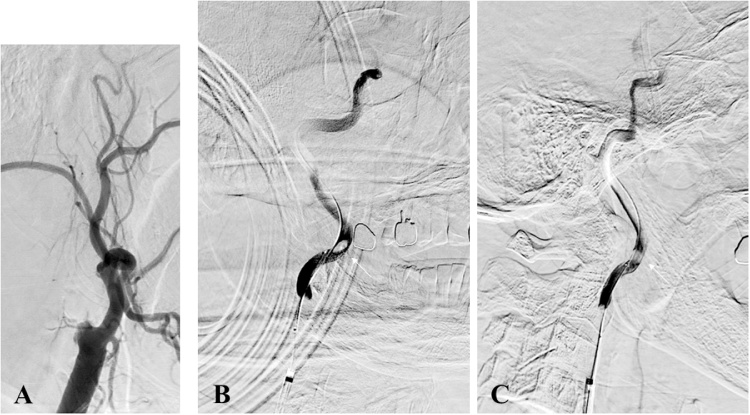
A 68-year-old man with a history of hypertension, hyperlipidemia and diabetes mellitus was admitted to our hospital. Neurological examination on admission revealed disturbance of consciousness and severe left-sided motor weakness (16 on the National Institutes of Health Stroke Scale). Blood biochemistry findings revealed no evidence of inflammation or coagulation system abnormalities. Electrocardiography indicated a sinus rhythm at 70 beats/min. Diffusion-weighted magnetic resonance imaging (MRI) showed no acute cerebral infarction (Fig. 1A), but magnetic resonance angiography (MRA) revealed occlusion of the right ICA (Fig. 1B). We made a diagnosis of acute cerebral ischemia, then a systemic IV injection of rt-PA was performed 4 h after onset. However, neurological symptoms did not improve for 1 h. In addition, repeated MRA (Fig. 1C) and cerebral angiography still revealed complete occlusion of the right cervical ICA at its origin (Fig. 2A). As collateral blood flow from the contralateral anterior and posterior circulation was poor, revascularization of the right cervical ICA was performed using an endovascular technique.
Fig. 1.
Magnetic resonance imaging (MRI) and MR angiography (MRA) findings. (A, B) MRI/diffusion-weighted imaging (DWI) at the time of initial presentation shows no acute cerebral infarction, but MRA reveals complete occlusion of the right internal carotid artery (ICA). (C) After intravenous injection of recombinant tissue plasminogen activator (rt-PA), cervical MRA demonstrates that the right ICA is still occluded.
Fig. 2.
(A) Preoperative right common carotid angiography (CAG) revealing complete occlusion of the right internal carotid artery (ICA) at the origin; (B, C) Right internal carotid angiography (ICAG) from Excelsior SL-10® demonstrating obvious floating clot (white arrow) in the cervical ICA (B: anteroposterior view; C: lateral view).
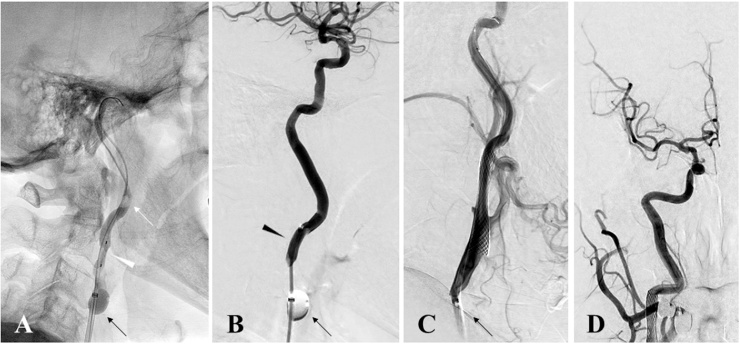
We performed all procedures under local anesthesia. An OPTIMO balloon-tipped guiding catheter (Tokai Medical Products, Kasugai, Japan) was inserted into the right femoral artery and advanced until the tip reached the right common carotid artery (CCA). After blockage of the proximal blood flow in the right CCA, an Excelsior SL-10® Microcatheter (Stryker Neurovascular, Fremont, CA, USA) was inserted to the right ICA segment distal to the occlusion area. Imaging study performed from the Excelsior SL-10® Microcatheter demonstrated obvious floating clot in the cervical right ICA (Fig. 2B and C). Transluminal balloon angioplasty was performed with a 3.0-mm Gateway® Monorail™ percutaneous transluminal angioplasty (PTA) Balloon Catheter (Stryker Neurovascular) for the occluded area within the ICA (Fig. 3A) and a Penumbra aspiration catheter 5MAX™ ACE (Penumbra, Alameda, CA, USA) was passed distal to the position. Then, we performed a direct aspiration of the floating clot using this Penumbra aspiration catheter (Fig. 3B). After recanalization of the right ICA, a GuardWire® Temporary Occlusion & Aspiration System (Medtronic, Minneapolis, MN, USA) was passed through the stenotic portion into the distal right ICA. Transluminal balloon angioplasty was performed with a 3.5-mm Sterling PTA balloon catheter (Boston Scientific, Natick, MA, USA). Next, a 10 × 24-mm Carotid Wallstent Monorail® (Boston Scientific) was deployed (Fig. 3C), and post-dilatation was performed using a 4.5-mm Sterling PTA balloon catheter (Boston Scientific). Subsequent angiography confirmed successful recanalization of the right ICA (thrombolysis in cerebral infarction (TICI) grade 3) at 7 h post-onset (Fig. 3D).
Fig. 3.
Intraoperative angiography; (A) OPTIMO (black arrow) is placed at the right common carotid artery (CCA). Balloons placed in the CCA are inflated; then a transluminal balloon angioplasty was performed with a 3.0-mm Gateway™ PTA balloon catheter (white arrowhead) for the occluded area of the internal carotid artery (ICA). (B) Penumbra aspiration catheter, 5 MAX™ ACE (black arrowhead), is passed distal to the position, allowing suctioning of the floating clot (white arrow) using this aspiration system. (C) A carotid wall stent was deployed and revascularization was recognized. (D) Postoperative angiography confirmed successful recanalization of the right ICA (thrombolysis in cerebral infarction (TICI) grade 3).
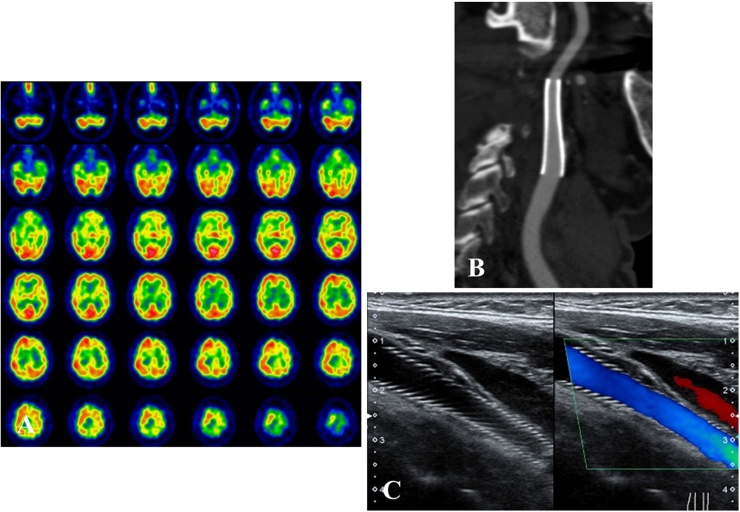
Immediately after these procedures, we started treatment with dual-agent antiplatelet therapy (aspirin 100 mg/day and clopidogrel 75 mg/day) and cilostazol 200 mg/day was added on the following day. The patient was restless with neurological abnormalities, and 123I IMP-single photon emission tomography (SPECT) (Fig. 4A) and INVOS-3100 revealed hyperperfusion in the territory of the right ICA. Strict control of blood pressure under dexmedetomidine anesthesia allowed effective prevention of HPS. Carotid ultrasonography and three-dimensional computed tomographic angiography at 14 days (Fig. 4B and C) revealed no further obstruction to flow, and the patient was discharged 3 weeks after surgery with mild left motor weakness.
Fig. 4.
Single photon emission computed tomography (SPECT), three-dimensional computed tomographic angiography (3D-CTA) and carotid ultrasonography. (A) PAO-SPECT (1 day after endovascular surgery) reveals increased cerebral blood flow in the right cerebral hemisphere. (B, C) 3D-CTA (B) and carotid ultrasonography (C) shows sufficient patency 14 days postoperatively.
3. Discussion
In patients with acute cerebral infarction due to severe stenosis or occlusion of the ICA, IV rt-PA alone has been reported to be less effective, and its morbidity and mortality are higher than conventional therapy [8], [9]. In addition, acute ischemic stroke associated with cervical carotid occlusion at the origin is relatively rare, so its management has not been studied extensively, and therapeutic approaches, in particular how to choose of antiplatelet agents within 24 h after IV rt-PA, remain unclear. A combination of IV thrombolysis using rt-PA and early carotid revascularization by endovascular surgery might result in more effective secondary stroke prevention. Several publications and studies have proposed that recanalization via aggressive endovascular treatment of acute cervical ICA occlusion at the origin may be successful with high rates of favorable outcomes [7], [10]. However, at least in the first 24 h after IV rt-PA administration, the risk of intracranial hemorrhage associated with early reperfusion of ischemic brain tissue might be increased [11], [12].
When trying to perform emergency CAS within 24 h after IV rt-PA administration, several issues require attention, such as the decisions regarding the type of stent and embolic protection device (EPD), the selection of antiplatelet therapy and the methods of preventing HPS. At first, with respect to emergency CAS, the selection of type of stent and EPD is very important [3], [6]. In the present case, although we were unable to evaluate the nature of the carotid plaques because of the need for emergency treatment, we strongly suspected that the plaque was vulnerable because of the sudden onset of symptoms. Because an open-cell stent often elicits embolic complications due to plaque protrusion, we selected a self-expandable closed-cell stent, and we were careful to avoid over-dilating the lesion. In addition, we also blocked the blood flow in the proximal CCA only when doing PTA and advancing the balloon-design EPD through the stenotic lesion to prevent scattering of the carotid plaque.
The second important point is the choice of perioperative antiplatelet agents. Antithrombotic therapy becomes required after the CAS enforcement. Generally, the double antiplatelet regimen is highly recommended before and after CAS in order to prevent subacute stent occlusion [3], [6]. However, it is a generally accepted principle that the administration of any anticoagulant drugs within 24 h after IV rt-PA therapy is contraindicated because of the risk of bleeding complications [2]. Furthermore, in the case of an emergency CAS procedure, the administration of several antiplatelet agents is particularly dangerous from the perspective of HPS [11], [12], [13], [14]. On the other hand, Fabrizio et al. and Inoue et al. demonstrated dual antiplatelet therapy, for example, the combination of aspirin (100 mg/day) and clopidogrel (75 mg/day) begun during the emergency CAS procedure within 24 h after IV rt-PA therapy over the 6 weeks after stent placement, resulting in good outcomes without serious hemorrhagic complications [15], [16]. Therefore, in our case, we administered aspirin and clopidogrel in the doses mentioned above for the prevention of subacute thrombosis, and we also obtained a good result.
Finally, the risk of intracranial hemorrhage due to hyperperfusion is potentially high in patients with acute stroke receiving emergency CAS because anticoagulation and antiplatelet medications must be administered during or after the procedure [16], [17]. However, the development of HPS may be avoided by strict blood pressure control [16], [17], [18]. Dexmedetomidine is a central alpha2 adrenoceptor agonist. Recently, this drug was shown to be a safe and acceptable sedative agent for patients requiring sedation after brain surgery including preventing hyperperfusion syndrome after carotid endarterectomy [16], [18]. In fact, although anticoagulation and antiplatelet therapy were added immediately after the CAS procedure in our case, careful control of blood pressure under dexmedetomidine anesthesia enabled effective management of the resulting HPS and there was no intracranial hemorrhage.
This present case suggests that early treatment with CAS for acute ischemic stroke due to ICA occlusion at the origin may be considered a safe and feasible alternative modality to carotid endarterectomy in selected patients at high risk of stroke recurrence, even if within 24 h after IV rt-PA administration.
4. Conclusion
We have described a case of cervical ICA occlusion treated successfully with the Penumbra System® and emergency CAS within 24 h after injection of rt-PA thrombolysis. If we can make the appropriate perioperative management, emergency CAS for the acute ICA occlusion at the origin may be considered a safe procedure in preventing early stroke recurrence in selected patients.
Conflict of interest
None of the authors have any commercial or financial involvement in connection with this study that represents or appears to represent any conflicts of interest.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Ethical approval
None.
Consent
Written informed consent was obtained from the patient’s family for publication of this case report and any accompanying images. A copy of the written consent is available for review by Editor-in-Chief of this journal on request.
Author contributions
All authors in this manuscript contributed to the interpretation of data, and drafting and writing of this manuscript. AI is first and corresponding author of this paper. He and SF performed the operation, conceived and designed the study and drafted the manuscript. AI, SF, SO, SN, HT, KK, KO, HI, SO, HM and SI were engaged in patient’s care in his hospital coarse including surgery under the supervision of KK and BO. All the authors read and approved the final manuscript.
Guarantor
Kanehisa Kohno, MD, PhD.
Acknowledgements
The authors would like to express their gratitude to Isao Kawamata, Atsushi Kyoshita, Shinichi Utsunomiya, Shotaro Kubo and Yosuke Orikawa, Department of Neurological Center, Ehime Prefectural Central Hospital, Japan for their helpful information regarding radiological image acquisition.
References
- 1.Del Zoppo G.J., Saver J.L., Jauch E.C., Adams H.P., Jr., American Heart Association Stroke Council Expansion of the time window for treatment of acute ischemic stroke with intravenous tissue plasminogen activator: a science advisory from the American Heart Association/American Stroke Association. Stroke. 2009;40:2945–2948. doi: 10.1161/STROKEAHA.109.192535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hacke W., Kaste M., Bluhmki E., Brozman M., Dávalos A., Guidetti D. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N. Engl. J. Med. 2008;359:1317–1329. doi: 10.1056/NEJMoa0804656. [DOI] [PubMed] [Google Scholar]
- 3.Bazan H.A., Zea N., Jennings B., Smith T.A., Vidal G., Sternbergh W.C., 3rd Urgent carotid intervention is safe after thrombolysis for minor to moderate acute ischemic stroke. J. Vasc. Surg. 2015;62:1529–1538. doi: 10.1016/j.jvs.2015.07.082. [DOI] [PubMed] [Google Scholar]
- 4.Wechsler L.R. Intravenous thrombolytic therapy for acute ischemic stroke. N. Engl. J. Med. 2011;364:2138–2146. doi: 10.1056/NEJMct1007370. [DOI] [PubMed] [Google Scholar]
- 5.Naylor A.R. Thrombolysis and expedited carotid revascularization. J. Cardiovasc. Surg. (Torino) 2015;56:159–164. [PubMed] [Google Scholar]
- 6.Koraen-Smith L., Troëng T., Björck M., Kragsterman B., Wahlgren C.M., Swedish Vascular Registry and the Riks-Stroke Collaboration Urgent carotid surgery and stenting may be safe after systemic thrombolysis for stroke. Stroke. 2014;45:776–780. doi: 10.1161/STROKEAHA.113.003763. [DOI] [PubMed] [Google Scholar]
- 7.Ratanaprasatporn L., Grossberg J.A., Spader H.S., Jayaraman M.V. Endovascular treatment of acute carotid occlusion. Clin. Neurol. Neurosurg. 2013;115:2521–2523. doi: 10.1016/j.clineuro.2013.10.008. [DOI] [PubMed] [Google Scholar]
- 8.Rha J.H., Saver J.L. The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke. 2007;38:967–973. doi: 10.1161/01.STR.0000258112.14918.24. [DOI] [PubMed] [Google Scholar]
- 9.Kimura K., Iguchi Y., Shibazaki K., Aoki J., Uemura J. Early recanalization rate of major occluded brain arteries after intravenous tissue plasminogen activator therapy using serial magnetic resonance angiography studies. Eur. Neurol. 2009;62:287–292. doi: 10.1159/000235753. [DOI] [PubMed] [Google Scholar]
- 10.Rahme R., Abruzzo T.A., Ringer A.J. Acute ischemic stroke in the setting of cervical carotid occlusion: a proposed management strategy. World Neurosurg. 2011;76:60–65. doi: 10.1016/j.wneu.2011.08.016. [DOI] [PubMed] [Google Scholar]
- 11.Ning M., Furie K.L., Koroshetz W.J., Lee H., Barron M., Lederer M. Association between tPA therapy and raised early matrix metalloproteinase-9 in acute stroke. Neurology. 2006;66:1550–1555. doi: 10.1212/01.wnl.0000216133.98416.b4. [DOI] [PubMed] [Google Scholar]
- 12.Wang Y.F., Tsirka S.E., Strickland S., Stieg P.E., Soriano S.G., Lipton S.A. Tissue plasminogen activator (tPA) increases neuronal damage after focal cerebral ischemia in wild-type and tPA-deficient mice. Nat. Med. 1998;4:228–231. doi: 10.1038/nm0298-228. [DOI] [PubMed] [Google Scholar]
- 13.Imai K., Mori T., Izumoto H., Watanabe M., Majima K. Emergency carotid artery stent placement in patients with acute ischemic stroke. AJNR Am. J. Neuroradiol. 2005;26:1249–1258. [PMC free article] [PubMed] [Google Scholar]
- 14.Zaidat O.O., Alexander M.J., Suarez J.I., Tarr R.W., Selman W.R., Enterline D.S. Early carotid artery stenting and angioplasty in patients with acute ischemic stroke. Neurosurgery. 2004;55:1237–1242. doi: 10.1227/01.neu.0000143164.66698.c9. [DOI] [PubMed] [Google Scholar]
- 15.Sallustio F., Koch G., Rocco A., Rossi C., Pampana E., Gandini R. Safety of early carotid artery stenting after systemic thrombolysis: a single center experience. Stroke Res. Treat. 2012;10:1155–1159. doi: 10.1155/2012/904575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Inoue A., Tagawa M., Nishikawa M., Kumon Y., Watanabe H., Ohnishi T. Emergency carotid artery stenting within 24 hours after intravenous thrombolysis for acute ischemic stroke: a case report. No Shinkei Geka. 2013;41:609–617. [PubMed] [Google Scholar]
- 17.Papanagiotou P., Roth C., Walter S., Behnke S., Grunwald I.Q., Viera J. Carotid artery stenting in acute stroke. J. Am. Coll. Cardiol. 2011;58:2363–2369. doi: 10.1016/j.jacc.2011.08.044. [DOI] [PubMed] [Google Scholar]
- 18.Suehiro S., Kohno K., Inoue A., Yamashita D., Tei N., Matsushige T. Two cases of cervical carotid artery stenosis with high risk post-operative hyperperfusion treated with dexmedetomidine after carotid endarterectomy. No Shinkei Geka. 2010;38:731–738. [PubMed] [Google Scholar]