Abstract
Smoking in combination with other behavioral risk factors is known to have a negative influence on health, and individuals who smoke typically engage in multiple risk behaviors. However, little is known about the clustering of risk behaviors among smokers of varying race/ethnicity. The purpose of this study was to examine patterns of cancer risk behaviors and to identify predictors of multiple risk behaviors in a racially/ethnically diverse sample of individuals seeking smoking cessation treatment. Overweight/obesity, at-risk alcohol consumption, and insufficient physical activity were measured in 424 smokers (African American, n = 144; Latino, n = 141; Caucasian, n = 139). Results indicated that 90% of participants reported behavioral cancer risk factors in addition to smoking. Approximately 70% of participants were overweight or obese, 48% engaged in at-risk drinking, and 27% were insufficiently physically active. Univariate analyses indicated that race/ethnicity, p < .001, smoking level, p = .03, and marital status, p = .04, were significant predictors of multiple risk behaviors, although only race/ethnicity remained a significant predictor, p < .001, when gender, smoking level, age, education, household income, marital status, and health insurance status were included in a multivariate model. Multivariate analysis indicated that the odds of engaging in multiple risk behaviors were significantly higher among Latinos, OR = 2.85, and African Americans, OR = 1.86, than Caucasians. Our findings highlight the need for research aimed at identifiying determinants of racial/ethnic differences in multiple risk behaviors, and indicate the importance of developing culturally sensitive interventions that target multiple risk behaviors.
Keywords: Tobacco, Alcohol, Obesity, Physical Activity
Introduction
Recent research has indicated that approximately 40% of all deaths in the United States are related to tobacco use, poor nutrition/obesity, physical inactivity, and alcohol consumption.1 Further, each of these behavioral factors has been independently linked with cancer risk and mortality.2–5 The presence of multiple risk factors has been shown to have an additive or synergistic negative influence on health,6–7 and research suggests that individuals frequently engage in more than one risk behavior concurrently.8–9 The clustering of risk behaviors may be particularly important because certain combinations of risk behaviors can increase risk for the development of specific diseases, such as in the synergistic effects of concurrent tobacco and alcohol use on the development of head and neck cancers.6,10
There is abundant evidence that several racial/ethnic minority groups are at increased risk for the development of tobacco-related cancers and cancer mortality.11–12 A biopsychosocial model has been proposed in which racial/ethnic differences in nutrition, obesity prevalence, and alcohol consumption are hypothesized to contribute to current health disparities among smokers.13 Although studies have reported racial/ethnic differences in individual behavioral factors including diet, obesity rates, physical activity (PA), and alcohol consumption,14–17 little is known about racial/ethnic differences in the clustering of risk behaviors.18 Studies of the patterns and predictors of multiple risk behaviors across racial/ethnic groups are needed to better understand health disparities and to more optimally direct cancer prevention efforts towards at-risk groups.
Individuals who smoke are more likely to engage in multiple risk behaviors than those who do not smoke,19–20 and the vast majority of individuals who smoke also engage in one or more additional risk behaviors.21–22 Smokers are more likely to drink heavily, to be physically inactive, and to eat less healthfully than non-smokers.19,23–27 Some research suggests that the higher prevalence of health risk behaviors among those who smoke may be due, in part, to poorer health knowledge relative to individuals who do not smoke.27–28
Although behavioral risk factors are more prevalent among individuals who smoke, little is known about the predictors of multiple risk behaviors within this population. Initial studies have indicated that greater daily smoking rate, greater age, less education, and male gender may predict engaging in multiple risk behaviors among individuals who smoke.21–22,24,26 Less education, lower income, and single marital status are associated with multiple risk behaviors in the general population, whereas the evidence for gender and age as predictors in the general population has been equivocal.8–9,18–19,22,29,30 Further, very little is known about racial/ethnic differences in the prevalence or predictors of multiple risk behaviors within the general population or among smokers.
Researchers have recently emphasized the need for evidence-based interventions that address multiple health risk behaviors.31–32 Initiation of smoking cessation treatment may provide a unique opportunity to access and treat individuals who are engaging in multiple risk behaviors and are thus at higher risk for the development of cancer. Knowledge of the patterns of multiple risk behaviors within racially/ethnically diverse populations seeking smoking cessation treatment may be utilized to develop multiple behavior change interventions that specifically target the most prevalent combinations of risk behaviors in an efficient and culturally sensitive manner.
The purpose of the present study was 1) to identify the patterns and prevalence of multiple cancer risk behaviors within a sample of individuals seeking smoking cessation treatment, 2) to determine whether the risk of engaging in multiple behavioral risk factors differed by race/ethnicity, and 3) to identify other demographic and social characteristics that are predictive of engaging in multiple risk behaviors. Gender, smoking level, age, education, income, marital status, and health insurance status were examined as predictors of the number of cancer risk factors based on findings from previous research and their potential contribution to racial/ethnic differences in risk behavior.
Materials and Methods
Data for the current study were collected as part of a longitudinal cohort study designed to examine racial/ethnic differences in the process of smoking cessation among African American, Latino, and Caucasian smokers. In the larger study, participants were followed from one week prior to their quit date through 26 weeks after their quit date. All participants received smoking cessation treatment that included nicotine patch therapy, self-help materials, and counseling. Participants were compensated for their participation with $20 gift cards at each of the first five study visits and $40 gift cards at each of the last two study visits (i.e., $180 for all study visits).
Participants
Individuals were eligible to participate if they were ≥ 21 years of age, smoked at least five cigarettes per day during the previous year, were motivated to quit within 30 days, possessed a home address and a functioning home telephone number, and were able to understand English at a sixth-grade literacy level. Individuals were excluded from the study if they reported regular use of tobacco products other than cigarettes, used bupropion or nicotine replacement products other than the nicotine patches supplied by the study, had another household member enrolled in the study, participated in a smoking cessation program during the previous 90 days, or reported that the nicotine patch was medically contraindicated.
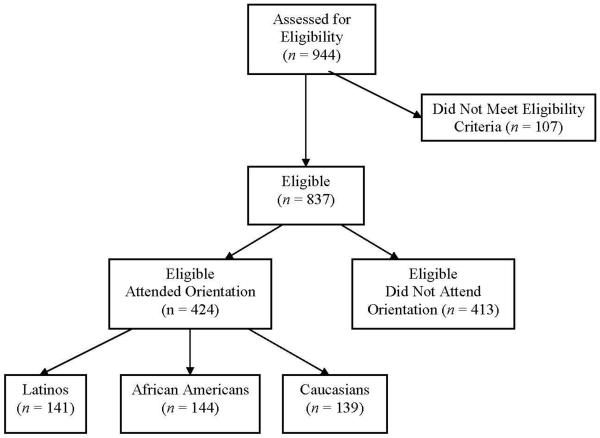
A total of 944 individuals were screened for eligibility. Of those screened, 837 individuals (88.7%) were eligible to participate in the study. However, 413 (49.3%) of the eligible individuals did not attend the initial visit and were therefore not enrolled in the study. Eligible individuals who enrolled in the study were of greater age, (41.22 vs. 37.12), F(1, 914) = 28.60, p < .001, smoked more cigarettes per day (21.11 vs. 18.36), F(1, 914) = 15.75, p < .001, reported more years of smoking, (21.55 vs. 18.28), F(1, 912) = 19.06, p < .001, and completed more years of education (12.90 vs. 12.58), F(1, 865) = 5.65, p = .02, than eligible individuals who did not enroll in the study. Further, the racial/ethnic distribution of participants differed significantly between eligible individuals who enrolled and those who did not enroll, χ2(3) = 48.26, p < .001. Among those enrolled in the study, 33.2% were Latino, 34.0% were African American, and 32.8% were Caucasian. Comparatively, the racial/ethnic distribution of those who did not enroll in the study was 47.3% Latino, 31.1% African American, 17.6% Caucasian, and 4.0% other. No differences between the groups were found in the distributions of gender, marital status, or income. Participant recruitment and flow are depicted in Figure 1.
Figure 1.
Flow of participants through the study protocol.
Measures
The Demographic Information Questionnaire was composed of 18 items that inquired about characteristics including age, gender, race/ethnicity, education, health insurance, and family income.
Overweight/Obesity Status was determined based on height and weight measurements, which were converted to body mass index (BMI; kg/m2). Participants with a BMI ≥ 25 were considered overweight/obese.
The Tobacco History questionnaire inquired about years of smoking and daily smoking rate. Participants who smoked < 20 cigarettes per day were considered light/moderate smokers and those who smoked ≥ 20 cigarettes per day were considered heavy smokers.
The Patient Health Questionnaire (PHQ) – Alcohol Abuse/Dependence Scale is a self-report questionnaire used to indicate probable abuse or dependence on alcohol.33 The first item inquires about whether the participant ever consumes alcohol, and any positive response on the subsequent items suggests probable alcohol abuse or dependence. The self-report version of the PHQ Alcohol/Abuse Dependence Scale has a sensitivity of 62%, a specificity of 97%, and an overall accuracy of 95% for detecting diagnoses of Alcohol Abuse or Dependence.33 Further, a kappa coefficient of .60 has been reported for the measure, suggesting moderate to substantial agreement between the alcohol/abuse dependence diagnoses suggested by the questionnaire and the diagnoses indicated by mental health professionals.33
The Alcohol Quantity and Frequency Questionnaire is a self-report measure of average alcohol consumption on each day of the week over the last 30 days.34 Average daily alcohol consumption was summed to determine average weekly alcohol consumption. In addition, the measure inquires about the number of binge drinking episodes (i.e., five or more drinks on one occasion) during the past three months.
At-Risk Drinking35 was confirmed if any of the following criteria were met: 1) participant was male and consumed an average of > 14 drinks per week, 2) participant was female and consumed an average of > seven drinks per week, 3) any individual who consumed ≥ five drinks on at least one occasion during the previous three months, or 4) any participant with probable alcohol abuse or dependence as indicated by the PHQ Alcohol Abuse/Dependence Scale.
The International Physical Activity Questionnaire – Short Format (IPAQ) is a seven-item self-report questionnaire that was used to measure the amount of time spent in moderate activity, vigorous activity, and walking during the past seven days.36 Weekly minutes spent engaging in each type of activity were multiplied by the corresponding metabolic equivalent (MET) value, and MET minutes were summed to arrive at the total weekly MET minutes spent in PA. PA categories (low, moderate, high) were assigned based on total weekly MET minutes, the number of days per week engaged in PA, and the amount of time spent in each type of PA.37 Individuals were considered insufficiently active if they were categorized as having low activity during the previous week. The IPAQ short format has demonstrated good test-retest reliability (pooled Spearman reliability coefficient = .75), and reliability estimates did not differ substantially whether the “last seven days” or the “usual week” were used as the reference period.36
Procedure
The present study was approved by the Institutional Review Board of the University of Texas M.D. Anderson Cancer Center. Informed consent was obtained from all participants. All questionnaire and anthropometric data were collected prior to the quit date of the larger smoking cessation study.
Analytic Plan
The present study focused on three cancer risk factors in addition to smoking: Overweight/obesity, insufficient physical activity, and at-risk drinking. Descriptive statistics were utilized to determine the prevalence of each risk behavior, and to identify the frequencies of all combinations of risk behaviors. Chi-Square analysis and Analysis of Variance (ANOVA) were utilized to determine whether there were differences in the total number of risk factors or the frequencies of individual and multiple risk factors between racial/ethnic and gender groups. Ordinal logistic regression (OLR) analysis was used to examine the relationships between race/ethnicity, gender, level of smoking, age, education, household income, marital status, health insurance status, and the total number of cancer risk factors in addition to smoking (i.e., 0, 1, 2, or 3). Each predictor variable was tested for significance as a univariate predictor of the total number of risk behaviors, and all variables were tested together in a multivariate model. Univariate and multivariate OLR analyses were also conducted using an individual income variable (i.e., household income/household members). The individual income variable produced the same results as the household income variable and will therefore not be discussed further. Two-way interactions between race/ethnicity and each of the other study variables were tested using OLR analyses as well.
OLR analysis was selected because the dependent variable (i.e., total number of cancer risk factors) was a sequence of ordered categories (i.e., 0, 1, 2, 3), and this approach permits the quantification of the odds of having a greater number of risk factors.38 Specifically, the probability of being in a higher category rather than a lower category is determined by dichotomizing the dependent variable at each successively higher increment of the dependent variable (i.e., 0 vs. 1, 2, 3; 0, 1 vs. 2, 3; and 0, 1, 2 vs. 3 additional risk factors). An overall proportional odds ratio is subsequently produced that summarizes the odds ratios generated with each set of dichotomized categories of the dependent variable.
When using OLR analysis, it is assumed that the odds ratios produced with each dichotomy of the dependent variable are homogenous (i.e., the proportional odds assumption). Therefore, the overall proportional odds ratio is assumed to be independent of the specific cut-point used to dichotomize the dependent variable in the analysis. Thus, if the proportional odds assumption is valid, the odds of being in the higher category rather than in the lower category are the same, regardless of how the “higher” versus “lower” outcome categories are delineated. For example, a proportional odds ratio of 2.00 for males would be interpreted to mean that males are twice as likely to have a higher versus lower number of cancer risk factors than females, regardless of where the cut-point is located. In the current study, the proportional odds assumption was verified with a test of parallel lines for each analysis (SPSS version 15.0). With the exception of marital status in the univariate analyses only (p = .02), no violations of the proportional odds assumption were identified in the univariate or multivariate analyses (all p's > .18).
Results
Participant Characteristics
A total of 424 individuals participated in the study. Approximately 34% of the participants were African American (n = 144), 33.2% were Latino (n = 141), and 32.8% were Caucasian (n = 139). Participants differed significantly by racial/ethnic group on a variety of demographic, socioeconomic, and other variables (see Table 1).
Table 1.
Participant characteristics by race/ethnicity.
| n | Latinos (n = 141) | African Americans (n = 144) | Caucasians (n = 139) | Total Sample (N = 424) | p | |
|---|---|---|---|---|---|---|
| Age, years | 424 | 36.0 (±10.2) | 44.8 (±9.8) | 42.9 (±11.6) | 41.2 (±11.2) | <.001a |
| Gender (% female) | 424 | 44.7 | 59.7 | 56.1 | 53.5 | .03b |
| Marital Status (% single) | 420 | 51.1 | 75.5 | 68.8 | 65.2 | <.001b |
| Years of Education | 420 | 12.5 (±2.1) | 12.8 (±1.6) | 13.3 (±2.2) | 12.9 (±2.0) | .004a |
| Members of Household | 419 | 3.4 (±1.8) | 2.5 (±1.7) | 2.4 (±1.6) | 2.8 (±1.8) | <.001a |
| Annual Household Income (median) | 375 | $30,000–39,000 | $10,000–19,999 | $30,000–39,000 | $20,000–29,000 | .001b |
| Health Insurance (% none) | 419 | 46.8 | 35.0 | 36.5 | 39.4 | <.001b |
| Body Mass Index | 424 | 31.2 (±7.1) | 30.2 (±7.6) | 27.9 (±7.7) | 29.8 (±7.6) | .001a |
| Heavy Smoking (%) | 424 | 63.1 | 63.2 | 80.6 | 68.9 | .001b |
| Drinks per Week | 416 | 12.1 (±16.6) | 6.7 (±11.9) | 5.0 (±9.5) | 8.0 (±13.4) | <.001a |
| PHQ Alcohol Abuse/Dependence (%) | 421 | 28.6 | 17.6 | 17.3 | 21.1 | .03b |
| Binge Drinking (past 3 mos.; %) | 413 | 56.8 | 37.0 | 35.3 | 43.1 | <.001b |
| Binge Drinking Episodes (past 3 mos.) | 413 | 6.3 (±16.9) | 1.92 (±8.0) | 1.67 (±4.3) | 3.31 (±11.3) | .001a |
p-value based on ANOVA test for differences between racial/ethnic groups.
p-value based on Chi-square test for differences between racial/ethnic groups.
Risk Factor Prevalence
Participants reported an average of 1.44 (±.77) cancer risk factors in addition to smoking. Approximately 70.3% of participants were overweight or obese, 48.4% were at-risk drinkers, and 27.2% were insufficiently active. Only 10.3% of participants reported smoking as their sole risk factor, while 42.1% reported one additional risk factor, 40.7% reported two additional risk factors, and 6.9% reported all three additional risk factors. The three most prevalent combinations of risk factors among participants in the sample were smoking in combination with overweight/obesity (28.3%), overweight/obesity and at-risk drinking (25.7%), and at-risk drinking (12.7%).
Racial/Ethnic Differences in Risk Factor Prevalence
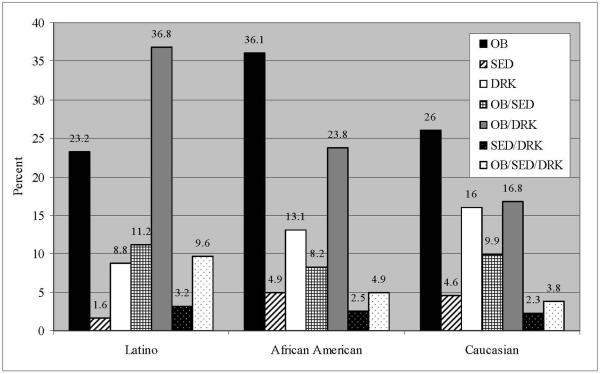
The total number of cancer risk factors differed significantly by race/ethnicity, F(2, 375) = 12.46, p < .001, such that Latinos reported the greatest number of risk factors in addition to smoking, followed by African Americans, and Caucasians (1.68 vs. 1.44 vs. 1.21). The prevalence of overweight/obesity, χ2(2) = 22.42, p < .001, and at-risk drinking, χ2(2) = 14.11, p = .001, differed significantly by race/ethnicity, such that Latinos had the highest rates of overweight/obesity and at-risk drinking, followed by African Americans, and Caucasians (see Figure 2). No differences were found between racial/ethnic groups in the prevalence of insufficient physical activity. The distribution of the total number of risk factors differed significantly by race/ethnicity, χ2(6) = 29.15, p < .001. Latinos had the highest percentage of participants with all three additional risk factors, while Caucasians had the highest percentage of individuals who reported no additional risk factors (see Figure 3). The combinations of risk factors also differed significantly by race/ethnicity, χ2(14) = 40.19, p < .001. Specifically, smoking and overweight/obesity was the most prevalent combination of risk factors among African Americans and Caucasians, while smoking, obesity, and at-risk drinking was the most prevalent combination among Latinos (see Figure 4).
Figure 2.
Percent of participants with each individual risk factor by race/ethnicity.
Figure 3.
The prevalence of having zero to three risk factors in addition to smoking by race/ethnicity.
Figure 4.
The prevalence of each combination of risk factors by race/ethnicity.
Note: OB = Overweight/Obese; SED = Insufficient Physical Activity; DRK = At-Risk Drinking.
Gender Differences in Risk Factor Prevalence
Males and females differed significantly in the prevalence of each individual risk factor. Males had higher rates of overweight/obesity (75.1% vs. 66.1%), χ2(1) = 4.13, p = .04, and at-risk drinking (57.1% vs. 41.0%), χ2(1) = 10.63, p = .001, than females, while higher rates of insufficient physical activity were found among females than males (31.7% vs. 22.1%), χ2(1) = 4.53, p = .03. The prevalence of all combinations of risk factors also differed significantly by gender, χ2(7) = 14.84, p = .04. Among males, the most prevalent combinations of risk factors were smoking in combination with overweight/obesity and at-risk drinking (32.6%), overweight/obesity (28.0%), and at-risk drinking (13.1%). Among females, the most prevalent combinations of risk factors were smoking in combination with overweight/obesity (28.6%), overweight/obesity and at-risk drinking (19.7%), overweight/obesity and insufficient physical activity (12.3%), and at-risk drinking (12.3%). Neither the average number of cancer risk factors nor the distribution of the total number of risk factors (i.e., zero, one, two, or three) differed significantly by gender.
Univariate Analyses
Univariate OLR analysis revealed that race/ethnicity was a significant predictor of engaging in multiple risk behaviors, χ2(2) = 24.90, p < .001. Latino and African American race/ethnicity were each associated with greater odds of engaging in multiple risk behaviors relative to Caucasians (see Table 2). Smoking level, χ2(1) = 4.76, p = .03, and marital status, χ2(1) = 4.16, p = .04, were also significantly associated with engaging in multiple risk behaviors. Light to moderate smoking (< 20 cigarettes per day) was associated with significantly greater odds of engaging in multiple risk behaviors relative to participants who were heavier smokers (≥ 20 cigarettes per day). Additionally, single marital status was associated with significantly lower odds of having multiple risk factors relative to participants who were married or living with a significant other. Gender, age, education, annual household income, and health insurance status were not significantly associated with engaging in multiple risk behaviors.
Table 2.
Univariate and multivariate predictors of the number of cancer risk factors in addition to smoking (i.e., 0, 1, 2, or 3 additional risk factors).
| Univariate | Multivariate | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| n | Odds Ratio (95% CI) | p | n | Adjusted Odds Ratio (95% CI) | p | |
| Race/Ethnicity | ||||||
| Latinos | 125 | 3.33 (2.06, 5.37) | <.001 | 107 | 2.85 (1.66, 4.89) | <.001 |
| African Americans | 122 | 1.75 (1.10, 2.80) | .02 | 112 | 1.86 (1.11, 3.13) | .02 |
| Caucasians | 131 | 1.00 | - | 114 | 1.00 | - |
| Gender | ||||||
| Male | 175 | 1.37 (.94, 2.00) | .11 | 156 | 1.34 (.87, 2.05) | .18 |
| Female | 203 | 1.00 | - | 177 | 1.00 | - |
| Smoking Level | ||||||
| Light/Moderate (< 20/day) | 116 | 1.59 (1.05, 2.40) | .03 | 103 | 1.32 (.82, 2.11) | .25 |
| Heavy (≥ 20/day) | 262 | 1.00 | - | 230 | 1.00 | - |
| Age | ||||||
| 21–35 years | 121 | 1.42 (.90, 2.25) | .13 | 103 | 1.25 (.73, 2.15) | .42 |
| 36–45 years | 120 | 1.16 (.74, 1.84) | .52 | 106 | 1.11 (.67, 1.84) | .68 |
| ≥ 46 years | 137 | 1.00 | - | 124 | 1.00 | - |
| Education | ||||||
| ≤ High School | 155 | 1.09 (.74, 1.60) | .66 | 134 | .86 (.56, 1.33) | .51 |
| ≥ Some College | 220 | 1.00 | - | 199 | 1.00 | - |
| Annual Household Income | ||||||
| < $10,000 | 93 | .76 (.45, 1.27) | .30 | 93 | 1.12 (.56, 2.33) | .76 |
| $10,000 – $39,999 | 129 | .98 (.61, 1.57) | .93 | 128 | 1.04 (.60, 1.79) | .90 |
| ≥ $40,000 | 112 | 1.00 | - | 112 | 1.00 | - |
| Marital Status | ||||||
| Single, Divorced, Separated, Widowed | 242 | .66 (.44, .98) | .04 | 217 | .68 (.42, 1.09) | .11 |
| Married, Living with Sig. Other | 133 | 1.00 | - | 116 | 1.00 | - |
| Health Insurance Status | ||||||
| None | 152 | .97 (.64, 1.48) | .90 | 131 | 1.00 (.59, 1.68) | .99 |
| Medicare/Medicaid/Medical Assistance | 68 | .83 (49, 1.42) | .50 | 59 | 1.09 (.56, 2.12) | .81 |
| Private/Group Insurance | 154 | 1.00 | - | 143 | 1.00 | - |
Note: The last group within each category served as the reference group. Bolded outcomes indicate p-values < .05.
Multivariate Analysis
A multivariate model was tested in which all variables were included (i.e., race/ethnicity, gender, smoking level, age, education, household income, marital status, health insurance status). Results indicated that only race/ethnicity remained a significant predictor of engaging in multiple risk behaviors, χ2(2) = 14.96, p < .001. Latino and African American race/ethnicity were associated with greater odds of engaging in multiple risk behaviors relative to Caucasians (see Table 2). Gender, smoking level, age, education, annual family income, marital status, and health insurance status were not significantly associated with engaging in multiple risk behaviors. All two-way interactions between race/ethnicity and each study variable were additionally tested using OLR, and no significant two-way interactions were found.
Discussion
Engaging in multiple risk behaviors is normative among individuals who smoke. Consistent with the findings of previous research,21–22 90% of participants in the current study had at least one cancer risk factor in addition to smoking. Males were more likely to be overweight/obese and at-risk drinkers, while females were more likely to be insufficiently active. Importantly, Latino and African American race/ethnicity were associated with engaging in a greater number of risk behaviors. Latino ethnicity, in particular, was associated with the greatest odds of engaging in multiple risk behaviors. Few studies have focused on risk behaviors among Latinos, thus the present findings provide important initial information about risk factors in one group of Latino smokers. Understanding the cancer risk behaviors of Latinos is critically important to the public health of the nation, as Latinos are the fastest growing and largest minority group in the United States.39
The patterns and prevalence of risk factors were found to differ by race/ethnicity. Latinos had the highest rates of overweight/obesity and at-risk drinking, followed by African Americans, and Caucasians. This is consistent with previous findings indicating that Latinos consume more alcohol per drinking occasion and engage in more frequent binge drinking than other racial/ethnic groups.14,17 Similarly, the prevalence rates of overweight/obesity are reported to be elevated among Mexican Americans and African Americans relative to Caucasians.16 Although some research has indicated that Latinos and African Americans may engage in less physical activity than Caucasians,15 no racial/ethnic differences were found in the prevalence of insufficient physical activity in the current study. Given the higher prevalence of overweight/obesity and at-risk drinking among Latinos, it is not surprising that Latinos also had the highest proportion of individuals engaging in two or three additional risk factors concurrently. The most frequent combination of risk factors among Caucasians and African Americans was smoking and overweight/obesity, while the most frequent combination of risk factors among Latinos was smoking, overweight/obesity, and at-risk drinking. Although findings indicate that racial/ethnic groups vary in the prevalence of behavioral risk factors, overweight/obesity and at-risk drinking were common behavioral risk factors among smokers of all racial/ethnic groups.
Previous research has indicated that PA level, alcohol consumption, and body weight may influence smoking cessation outcomes. Specifically, alcohol consumption is associated with relapse following smoking cessation,40 while PA is associated with successful smoking cessation.41 Continuously abstinent individuals may expect to gain an average of 13 pounds one year post-cessation,42 and more than 10 percent of individuals gain at least 29 pounds.43 Latinos and African Americans, in particular, are at risk of excessive postcessation weight gain.44–45 Postcessation weight gain may exacerbate obesity-related health problems among individuals who are already overweight or obese. Thus, it is plausible that intervening to address multiple cancer risk factors during treatment could improve smoking cessation rates and minimize the health consequences associated with alcohol use and postcessation changes in energy balance.
The present study has several strengths and limitations. The racially/ethnically diverse sample provided an opportunity to obtain valuable information about the health behaviors of African American, Latino, and Caucasian smokers. Unfortunately, the findings do not explain the underlying reasons for racial/ethnic differences in risk behavior. Research has indicated that acculturation may influence health behavior among Latinos.17 In addition, socioeconomic status,46 cultural environment,47 access to medical care,48–49 biological and genetic factors,50–51 and neighborhood characteristics52–54 may also influence health behavior and disease risk. For example, research has indicated that neighborhoods composed primarily of racial/ethnic minorities are less likely to support walking for PA, and also contain higher densities of alcohol advertisements, tobacco advertisements, and fast food restaurants than predominantly Caucasian neighborhoods.52–54 Thus, neighborhood and other factors likely contribute to an explanation of the higher prevalence of risk behaviors among Latinos and African Americans.
Several issues related to the generalizability of the findings should be considered. Given the high proportion of Mexican Americans residing in the Houston area, our results may not be generalizable to Latinos of other ethnic backgrounds (e.g., Puerto Rican, Cuban). Further, nearly half of individuals who were eligible to participate did not attend the initial visit and were therefore not enrolled in the study. However, it is important to note that enrollment rates in the present study were consistent with or slightly better than enrollment rates in other smoking cessation studies.55–56 Individuals who participated in the study were of greater age, had more education, smoked more heavily, and reported more years of smoking than individuals who were eligible but did not participate. These characteristics are indicative of individuals who are more motivated to quit smoking due to a longer smoking history, heavier smoking, and greater education. It is also noteworthy that a higher proportion of eligible Latinos than other racial/ethnic groups did not attend the initial orientation session. Finally, the inclusion of solely smokers within the context of a smoking cessation study may be considered a limitation, although the presence of additional risk factors among individuals who smoke may compound risk for tobacco-related cancers. Overall, the results should be interpreted with caution until they are replicated within additional populations in other studies.
It is important to note the limitations of the self-report measures of alcohol consumption and PA that were utilized in the study. It is possible that participants underestimated their alcohol consumption due to poor recall or social desirability. However, this does not seem likely given the research indicating that self-reports of alcohol consumption are generally accurate.34 Recent evidence suggests that the IPAQ may overestimate PA levels,57 which may help to explain the higher than expected prevalence of active participants. Alternatively, it is possible that the participants had physically demanding jobs relative to participants of higher socioeconomic status in other studies. Findings related to PA in the present study should be interpreted cautiously until they can be replicated with other measures of PA.
The results of the current study highlight the need for interventions focused on multiple risk behaviors in smokers. Although some studies have successfully targeted multiple risk behaviors within specific populations including weight-concerned female smokers56 and those with diabetes or cardiovascular disease,31 the findings of our study suggest that the majority of individuals who enroll in smoking cessation interventions also appear to be in need of such interventions. Thus, it may be efficient to include treatment components that address common co-occurring risk factors (e.g., overweight/obesity, at-risk drinking) within existing smoking cessation interventions, although the optimal timing of the treatment components (i.e., sequential vs. concurrent) remains to be determined.31 Interventions may also incorporate treatment components that are tailored to the specific needs of the individual, which may be identified through an initial assessment of current risk factors as well as motivation for change with regard to each risk factor. Differing lifestyles, traditions, and beliefs between cultures are likely to influence the likelihood of involvement in risk behaviors, and thus interventions must address such behaviors in a culturally sensitive fashion. Ultimately, it is hoped that effective multiple behavior change interventions will reduce disparities in cancer risk factors, and contribute to the elimination of cancer.
Acknowledgements
This research was supported by grants R01-DA014818 awarded by the National Institute on Drug Abuse, R25T-CA57730 awarded by the National Cancer Institute, and K01-DP000086 awarded by the National Center for Chronic Disease Prevention and Health Promotion.
References
- 1.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004 Mar 10;291(10):1238–45. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 2.Calle EE, Rodriguez C, Walker-Thurmond K, Thun MJ. Overweight, obesity, and mortality from cancer in a prospectively studied cohort of U.S. adults. N Engl J Med. 2003 Apr 24;348(17):1625–38. doi: 10.1056/NEJMoa021423. [DOI] [PubMed] [Google Scholar]
- 3.Lee I. Physical activity and cancer prevention – Data from epidemiologic studies. Med Sci Sports Exerc. 2003 Nov;35(11):1823–7. doi: 10.1249/01.MSS.0000093620.27893.23. [DOI] [PubMed] [Google Scholar]
- 4.Levitz JS, Bradley TP, Golden AL. Overview of smoking and all cancers. Med Clin North Am. 2004 Nov;88(6):1655–75. doi: 10.1016/j.mcna.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 5.Poschl G, Seitz HK. Alcohol and cancer. Alcohol Alcohol. 2004 May-Jun;39(3):155–65. doi: 10.1093/alcalc/agh057. [DOI] [PubMed] [Google Scholar]
- 6.Blot WJ, McLaughlin JK, Winn DM, Austin DF, Greenberg RS, Preston-Martin S, et al. Smoking and drinking in relation to oral and pharyngeal cancer. Cancer Res. 1988 Jun 1;48(11):3282–7. [PubMed] [Google Scholar]
- 7.Xu WH, Zhang XL, Gao YT, Xiang YB, Gao LF, Zheng W, et al. Joint effect of cigarette smoking and alcohol consumption on mortality. Prev Med. 2007 Oct;45(4):313–9. doi: 10.1016/j.ypmed.2007.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fine LJ, Philogene S, Gramling R, Coups EJ, Sinha S. Prevalence of multiple chronic disease risk factors: 2001 National Health Interview Survey. Am J Prev Med. 2004 Aug;27(Suppl 2):18–24. doi: 10.1016/j.amepre.2004.04.017. [DOI] [PubMed] [Google Scholar]
- 9.Pronk NP, Anderson LH, Crain L, Martinson BC, O'Connor PJ, Sherwood NE, et al. Meeting recommendations for multiple healthy lifestyle factors: Prevalence, clustering, and predictors among adolescent, adult, and senior health plan members. Am J Prev Med. 2004 Aug;27(Suppl 2):25–33. doi: 10.1016/j.amepre.2004.04.022. [DOI] [PubMed] [Google Scholar]
- 10.Lewin F, Norell SE, Johansson H, Gustavsson P, Wennerberg J, Biorklund A, et al. Smoking tobacco, oral snuff, and alcohol in the etiology of squamous cell carcinoma of the head and neck. Cancer. 1998 Apr 1;82(7):1367–75. doi: 10.1002/(sici)1097-0142(19980401)82:7<1367::aid-cncr21>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 11.Berger M, Lund MJ, Brawley OW. Racial disparities in lung cancer. Curr Probl Cancer. 2007 May-Jun;31(3):202–10. doi: 10.1016/j.currproblcancer.2007.02.002. [DOI] [PubMed] [Google Scholar]
- 12.Fagan P, Moolchan ET, Lawrence D, Fernander A, Ponder PK. Identifying health disparities across the tobacco continuum. Addiction. 2007 Oct;102(Suppl 2):5–29. doi: 10.1111/j.1360-0443.2007.01952.x. [DOI] [PubMed] [Google Scholar]
- 13.Fernander AF, Shavers VL, Hammons GJ. A biopsychosocial approach to examining tobacco-related health disparities among racially classified social groups. Addiction. 2007 Oct;102(Suppl 2):43–57. doi: 10.1111/j.1360-0443.2007.01954.x. [DOI] [PubMed] [Google Scholar]
- 14.Dawson DA. Beyond black, white, and Hispanic: Race, ethnic origin and drinking patterns in the United States. J Subst Abuse. 1998;10(4):321–39. doi: 10.1016/s0899-3289(99)00009-7. [DOI] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention (CDC) Prevalence of fruit and vegetable consumption and physical activity by race/ethnicity – United States, 2005. Morb Mortal Wkly Rep. 2007 Apr 6;56(13):301–4. [PubMed] [Google Scholar]
- 16.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006 Apr 5;295(13):1549–55. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 17.Otero-Sabogal R, Sabogal F, Perez-Stable EJ, Hiatt RA. Dietary practices, alcohol consumption, and smoking behavior: Ethnic, sex, and acculturation differences. J Natl Cancer Inst Monogr. 1995;18:73–82. [PubMed] [Google Scholar]
- 18.Berrigan D, Dodd K, Troiano RP, Krebs-Smith SM, Barbash RB. Patterns of health behavior in U.S. adults. Prev Med. 2003 May;36(5):615–23. doi: 10.1016/s0091-7435(02)00067-1. [DOI] [PubMed] [Google Scholar]
- 19.Burke V, Milligan RAK, Beilin LJ, Dunbar D, Spencer M, Balde E, et al. Clustering of health-related behaviors among 18-year-old Australians. Prev Med. 1997 Sep-Oct;26(5 Pt 1):724–33. doi: 10.1006/pmed.1997.0198. [DOI] [PubMed] [Google Scholar]
- 20.Laaksonen M, Luoto R, Helakorpi S, Uutela A. Associations between health-related behaviors: A 7-year follow-up of adults. Prev Med. 2002 Feb;34(2):162–70. doi: 10.1006/pmed.2001.0965. [DOI] [PubMed] [Google Scholar]
- 21.Chiolero A, Wietlisbach V, Ruffieux C, Paccaud F, Cornuz J. Clustering of risk behaviors with cigarette consumption: a population-based survey. Prev Med. 2006 May;42(5):348–53. doi: 10.1016/j.ypmed.2006.01.011. [DOI] [PubMed] [Google Scholar]
- 22.Emmons KM, Marcus BH, Linnan L, Rossi JS, Abrams DB. Mechanisms in multiple risk factor interventions: Smoking, physical activity, and dietary fat, intake among manufacturing workers. Prev Med. 1994 Jul;23(4):481–9. doi: 10.1006/pmed.1994.1066. [DOI] [PubMed] [Google Scholar]
- 23.Kvaavik E, Meyer HE, Tverdal A. Food habits, physical activity and body mass index in relation to smoking status in 40–42 year old Norwegian women and men. Prev Med. 2004 Jan;38(1):1–5. doi: 10.1016/j.ypmed.2003.09.020. [DOI] [PubMed] [Google Scholar]
- 24.Ma J, Betts NM, Hampl JS. Clustering of lifestyle behaviors: The relationship between cigarette smoking, alcohol consumption, and dietary intake. Am J Health Promot. 2000 Nov-Dec;15(2):107–17. doi: 10.4278/0890-1171-15.2.107. [DOI] [PubMed] [Google Scholar]
- 25.Revicki D, Sobal J, DeForge B. Smoking status and the practice of other unhealthy behaviors. Fam Med. 1991 Jul;23(5):361–4. [PubMed] [Google Scholar]
- 26.Thornton A, Lee P, Fry J. Differences between smokers, ex-smokers, passive smokers, and non-smokers. J Clin Epidemiol. 1994 Oct;47(10):1143–62. doi: 10.1016/0895-4356(94)90101-5. [DOI] [PubMed] [Google Scholar]
- 27.Woodward M, Bolton-Smith C, Tunstall-Pedoe H. Deficient health knowledge, diet, and other lifestyles in smokers: Is a multifactorial approach required? Prev Med. 1994 May;23(3):354–61. doi: 10.1006/pmed.1994.1049. [DOI] [PubMed] [Google Scholar]
- 28.Castro FG, Newcomb MD, McCreary C, Baezconde-Garbanati L. Cigarette smokers do more than just smoke cigarettes. Health Psychol. 1989;8(1):107–29. doi: 10.1037//0278-6133.8.1.107. [DOI] [PubMed] [Google Scholar]
- 29.Poortinga W. The prevalence and clustering of four major lifestyle risk factors in an English adult population. Prev Med. 2007 Feb;44(2):124–8. doi: 10.1016/j.ypmed.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 30.Schuit AJ, van Loon AJM, Tijhuis M, Ocke MC. Clustering of lifestyle risk factors in a general adult population. Prev Med. 2002 Sep;35(3):219–24. doi: 10.1006/pmed.2002.1064. [DOI] [PubMed] [Google Scholar]
- 31.Goldstein MG, Whitlock EP, DePue J. Multiple behavioral risk factor interventions in primary care: Summary of research evidence. Am J Prev Med. 2004 Aug;27(Suppl 2):61–79. doi: 10.1016/j.amepre.2004.04.023. [DOI] [PubMed] [Google Scholar]
- 32.Pronk NP, Peek CJ, Goldstein MG. Addressing multiple behavioral risk factors in primary care: A synthesis of current knowledge and stakeholder dialogue sessions. Am J Prev Med. 2004 Aug;27(Suppl 2):4–17. doi: 10.1016/j.amepre.2004.04.024. [DOI] [PubMed] [Google Scholar]
- 33.Spitzer RL, Kroenke K, Williams JBW. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. JAMA. 1999 Nov 10;282(18):1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 34.Sobell LC, Sobell MB. Alcohol consumption measures. In: Allen JP, Wilson VB, editors. Assessing alcohol problems: A guide for clinicians and researchers. 2nd ed. U.S. Department of Health and Human Services, National Institute on Alcohol Abuse and Alcoholism; Bethesda: 2003. pp. 75–99. NIH Publication No. 03-3745. [Google Scholar]
- 35.U.S. Department of Health and Human Services (USDHHS) Helping patients who drink too much: A clinician's guide. 2007 May; NIH Publication No. 07-3769.
- 36.Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, et al. International Physical Activity Questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003 Aug;35(8):1381–95. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- 37.Guidelines for data processing and analysis of the International Physical Activity Questionnaire (IPAQ) – November 2005. [cited 2007 Oct 17]. Available from: http://www.ipaq.ki.se/ipaq.htm.
- 38.Scott SC, Goldberg MS, Mayo NE. Statistical assessment of ordinal outcomes in comparative studies. J Clin Epidemiol. 1997 Jan;50(1):45–55. doi: 10.1016/s0895-4356(96)00312-5. [DOI] [PubMed] [Google Scholar]
- 39.U.S. Census Bureau Nation's population one-third minority. 2006 May 10; [cited 2007 Oct 24]. Available from: http://www.census.gov/PressRelease/www/releases/archives/population/006808.html.
- 40.McClure JB, Wetter DW, de Moor C, Cinciripini PM, Gritz ER. The relation between alcohol consumption and smoking abstinence: Results from the Working Well Trial. Addict Behav. 2002 May-Jun;27(3):367–79. doi: 10.1016/s0306-4603(01)00177-0. [DOI] [PubMed] [Google Scholar]
- 41.Nagaya T, Yoshida H, Takahashi H, Kawai M. Cigarette smoking weakens exercise habits in healthy men. Nicotine Tob Res. 2007 Oct;9(10):1027–32. doi: 10.1080/14622200701591575. [DOI] [PubMed] [Google Scholar]
- 42.Klesges RC, Winders SE, Meyers AW, Eck LH, Ward KD, Hultquist CM, et al. How much weight gain occurs following smoking cessation? A comparison of weight gain using both continuous and point prevalence abstinence. J Consult Clin Psychol. 1997 Apr;65(2):286–91. doi: 10.1037//0022-006x.65.2.286. [DOI] [PubMed] [Google Scholar]
- 43.Williamson DF, Madans J, Anda RF, Kleinman JC, Giovino GA, Byers T. Smoking cessation and severity of weight gain in a national cohort. N Engl J Med. 1991 Mar 14;324(11):739–45. doi: 10.1056/NEJM199103143241106. [DOI] [PubMed] [Google Scholar]
- 44.Burke JP, Hazuda HP, Stern MP. Rising trend in obesity in Mexican Americans and non-Hispanic whites: Is it due to cigarette smoking cessation? Int J Obes Relat Metab Disord. 2000 Dec;24(12):1689–94. doi: 10.1038/sj.ijo.0801439. [DOI] [PubMed] [Google Scholar]
- 45.Filozof C, Fernandez Pinilla MC, Fernandez-Cruz A. Smoking cessation and weight gain. Obes Rev. 2004 May;5(2):95–103. doi: 10.1111/j.1467-789X.2004.00131.x. [DOI] [PubMed] [Google Scholar]
- 46.Adler NA, Ostrove JM. Socioeconomic status and health: what we know and what we don't. Ann N Y Acad Sci. 1999;986:3–15. doi: 10.1111/j.1749-6632.1999.tb08101.x. [DOI] [PubMed] [Google Scholar]
- 47.Kumanyika SA, Whitt-Glover MC, Gary TL, Prewitt E, Odoms-Young AM, Banks-Wallace J, et al. Expanding the obesity research paradigm to reach African American communities. Prev Chronic Dis. 2007 Oct;4(4):1–22. [PMC free article] [PubMed] [Google Scholar]
- 48.Sambamoorthi U, McAlpine DD. Racial, ethnic, socioeconomic, and access disparities in the use of preventive services among women. Prev Med. 2003 Nov;37(5):475–84. doi: 10.1016/s0091-7435(03)00172-5. [DOI] [PubMed] [Google Scholar]
- 49.Wisdom JP, Berlin M, Lapidus JA. Relating health policy to women's health outcomes. Soc Sci Med. 2005 Oct;61(8):1776–84. doi: 10.1016/j.socscimed.2005.03.030. [DOI] [PubMed] [Google Scholar]
- 50.Fernandez JR, Allison DB. Understanding racial differences in obesity and metabolic syndrome traits. Nutr Rev. 2003 Sep;61(9):316–9. doi: 10.1301/nr.2003.sept.316-319. [DOI] [PubMed] [Google Scholar]
- 51.Lemieux S. Genetic susceptibility to visceral obesity and related clinical implications. Int J Obes Relat Metab Disord. 1997 Oct;21(10):831–8. doi: 10.1038/sj.ijo.0800488. [DOI] [PubMed] [Google Scholar]
- 52.Block JP, Scribner RA, DeSalvo KB. Fast food, race/ethnicity, and income: A geographic analysis. Am J Prev Med. 2004 Oct;27(3):211–17. doi: 10.1016/j.amepre.2004.06.007. [DOI] [PubMed] [Google Scholar]
- 53.Hackbarth DP, Silvestri B, Cosper W. Tobacco and alcohol billboards in 50 Chicago neighborhoods: Market segmentation to sell dangerous products to the poor. J Public Health Policy. 1995;16(2):213–30. [PubMed] [Google Scholar]
- 54.Kelly CM, Schootman M, Baker EA, Barnidge EK, Lemes A. The association of sidewalk walkability and physical disorder with area-level race and poverty. J Epidemiol Community Health. 2007 Nov;61(11):978–83. doi: 10.1136/jech.2006.054775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.McCarthy DE, Piasecki TM, Lawrence DL, Jorenby DE, Shiffman S, Fiore MC, et al. A randomized controlled trial of bupropion SR and individual smoking cessation counseling. Nicotine Tob Res. 2008 Apr;10(4):717–729. doi: 10.1080/14622200801968343. [DOI] [PubMed] [Google Scholar]
- 56.Spring B, Doran N, Pagoto S, Schneider K, Pingitore R, Hedeker D. Randomized trial for behavioral smoking and weight control treatment: Effect of concurrent versus sequential intervention. J Consult Clin Psychol. 2004 Oct;72(5):785–796. doi: 10.1037/0022-006X.72.5.785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fogelholm M, Malmberg J, Suni J, Santtila M, Kyrolainen H, Mantysaari M, et al. International Physical Activity Questionnaire: Validity against fitness. Med Sci Sports Exerc. 2006 Apr;38(4):753–60. doi: 10.1249/01.mss.0000194075.16960.20. [DOI] [PubMed] [Google Scholar]