George as a child. Who would have known then the impact he would make on the world of the science of obesity?
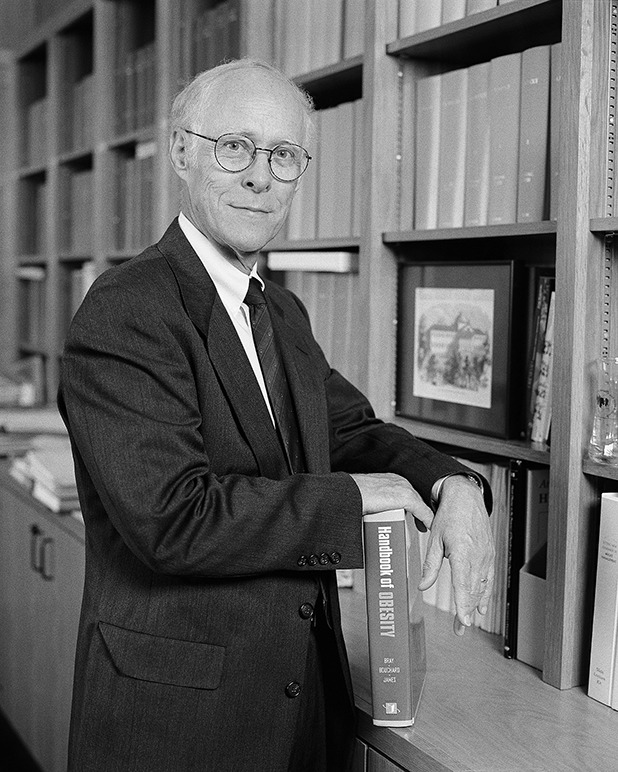
George at the end of his tenure as executive director of Pennington Biomedical Research Center.
As Mitzi watches, George receives a commemorative plaque from Dr. Claude Bouchard (executive director after George) during a 20th anniversary celebration event for Pennington Biomedical Research Center.
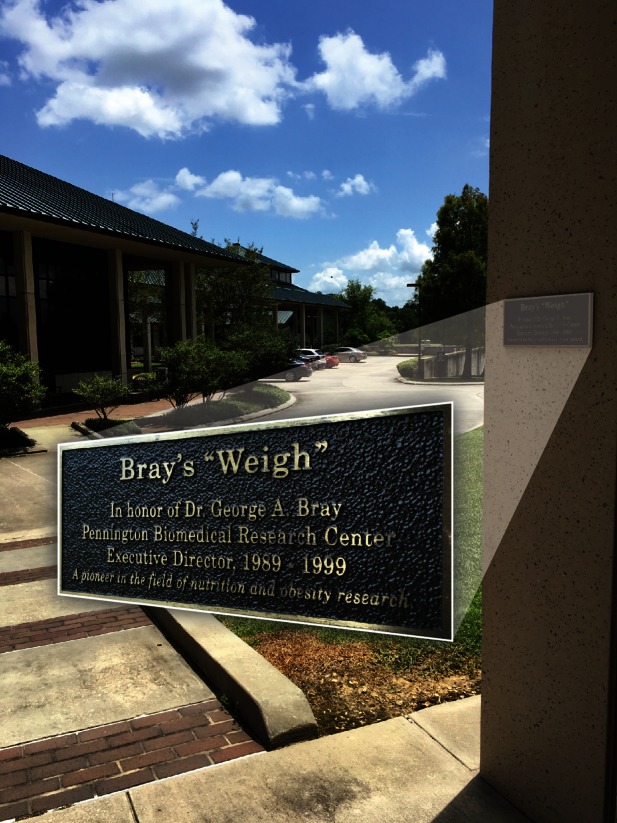
In gratitude and acknowledgment for his work and contributions, and for always doing things the “George Bray way,” Pennington Biomedical named the walkway between the basic and clinical research buildings Bray’s “Weigh” in his honor on the occasion of his retirement from the center on 10 December 2014.
Formative Years: Intimations of What Is to Come
George A. Bray was born 25 July 1931 in Winnetka, IL, during the peak of the Depression. He was the first child of George August and Mary H. Bray. His only sibling, Mary Elizabeth (Betsy) Bray, died secondary to rheumatic heart disease. Influenced by his mother, George developed a natural interest in education at a young age, even though one of his teachers at Hubbard Woods School in Winnetka reported that 11-year-old “George is doing good average work in all subjects” (1). Despite this inauspicious assessment, high school marked the emergence of a lifelong interest in and aptitude for science. This is clearly evidenced by his own writing in 1949 in an application for a national college scholarship program when he wrote: “Ever since I took my first science course in high school, I’ve been interested in the infinite possibilities of science.” When it came time to choose a college, George’s choice between Harvard and Brown University was based on the desire to attend one for college and the other for medical school. Choosing Brown University for undergraduate school was to have lifelong implications, as it was at the freshman mixer at Brown that he met his current wife, Mitzi. However, the budding romance was interrupted during their sophomore year; they would not meet again until their 25th class reunion in 1978. They have been virtually inseparable since. They married in 1982 and have shared a lifetime of traveling the world together, seeing places only known to Ripley of “believe it or not” fame. George has truly shared his science with the world.
College gave George his first taste of research, measuring the optical rotation of synthetic organic compounds. He furthered his interest in summer jobs at G.D. Searle in Skokie, IL. He graduated summa cum laude from Brown University in 1953, and 4 years later received his M.D. from Harvard Medical School magna cum laude. His internship on the Osler service of the Johns Hopkins Hospital exposed him to the precepts of Sir William Osler (1849–1919) and stirred George’s continuing interest in the history of medicine. Osler had mused that “no bubble is so iridescent or floats longer than that blown by the successful teacher.” Osler was prescient about his own role in the launch of young George when he said that “the good physician treats the disease; the great physician treats the patient who has the disease.” This concept was carried forth with great commitment by George. George has had a lifetime interest in history. His series of articles on the history of obesity, originally published in Obesity Research, has recently been published as a single volume (2). Following his internship at Johns Hopkins Hospital, he entered the U.S. Public Health Service and spent 2 years at the National Institutes of Health (NIH) investigating renal physiology. It was here that he published his article on “Bray’s Solution,” a cocktail for determining radioactivity in aqueous solutions (3). This is one of his most highly cited articles and merited a “Classics” review by the Institute of Scientific Information.
The NIH years not only solidified a choice to pursue a research career but also led to his marriage to Martha Bardenhagen (1933–2005), a nurse he met during his year as an intern at Johns Hopkins Hospital. George completed a medical residency at the Strong Memorial Hospital of the University of Rochester in Rochester, NY, and then began an endocrine fellowship in Rochester. This period was marked by the birth of George Hamilton Bray (1961–1990), the first of George and Martha’s four children (Thomas Luther, Susan Bardenhagen, and Nancy Sylvester Bray).
George’s research training continued with work in thyroid hormone and the sympathetic nervous system in a 1-year fellowship in London, U.K., with Dr. Rosalind V. Pitt-Rivers, the discoverer of T3 (triiodothyronine). A second postdoctoral fellowship in thyroid research followed with Dr. Edwin Bennett Astwood at the New England Medical Center in Boston, MA. It was Astwood who fatefully set George on his quest to understand the biologic underpinnings of obesity. As George described, the time with Astwood was when his “directional sails were set and obesity was the compass heading.”
The First 25 Scholarly Years (1964–1989)
George began an academic career as an assistant professor of medicine at Tufts University School of Medicine and as assistant physician at New England Medical Center Hospitals in Boston. The Zucker fatty rat had just been identified in 1963, and Astwood had the only other stock other than the ones in the Zucker laboratory. In addition to his thyroid studies, George began his initial experimental work in obesity by comparing these animals with other models of obesity, including animals with hypothalamic injury and animals with a form of obesity experimentally induced by the feeding of a very high-fat diet. One of the defining aspects of his approach to research has been to proceed simultaneously on both basic and clinical research fronts. So, in many ways he did “translational” research before it became fashionable! For his clinical work in this period, he studied patients who became obese due to hypothalamic disease (4) and patients who became obese because of the inheritance of the Prader-Willi syndrome (5).
In a move to Harbor-UCLA Medical Center in Torrance, CA, George was accompanied by post-doctoral fellow David York, PhD, who had also been a research fellow with George in Boston in 1969. David and George continued to collaborate over the years, including exchanging sabbaticals. David was the first scientist George recruited to the Pennington Center in 1989. They enjoyed a long personal friendship, and their extensive collaboration produced many discoveries at the bench and in rodent models. Most notably, their animal studies led to the publication of “Hypothalamic and Genetic Obesity in Experimental Animals: An Autonomic and Endocrine Hypothesis” (6), which was then followed by numerous experiments that supported this hypothesis. During their time together at the Pennington Center, they showed the essential role of glucocorticoids in the development of obesity, did much to aid our understanding of the systems—both central and peripheral—that regulate the intake of dietary fat, and enhanced our knowledge of the metabolic and endocrine differences between animals susceptible and resistant to obesity. Dr. David York was the leader of basic science research at Pennington for 13 years and was a key contributor to the success of that effort.
George’s research during this period also had a clinical component. He had developed an interest in overfeeding based on the work of Dr. Ethan Sims. In anticipation of conducting an overfeeding study, he used himself as an experimental model, going from 165 to 190 lbs. As with all overfeeding studies, at the end of the experiment his weight slid back down to 165 lbs. and remains there today.
In this period, George fostered and organized the nascent field and can be considered a father of obesity research. He chaired the organizing committee for the 1973 Fogarty Center International Conference on Obesity, held in Bethesda, MD, and this set the stage for the 1st International Congress on Obesity (ICO) that was held at the Royal College of Physicians in London in 1974. He was a key organizer of that very successful, and first of many, IOC, with over 500 attendees said to represent over 30 countries. It was a conference that launched the careers of two other young scientists, John Blundell and Barbara Hansen. The Association for the Study of Obesity (of the U.K.) was established out of those meetings. Alan Howard and George became the founding editors of the first (1977) scientific journal devoted to obesity, the International Journal of Obesity, which was established as a quarterly journal. It was an important event sharing the year 1977 with two other events, the 2nd IOC and the 2nd Fogarty Center International Conference on Obesity, both held in Washington, D.C. In 1982 George and others, including Marcie Greenwood and Wayne Calloway, who chaired and organized the NIH-sponsored workshop to explore “The Obesities,” gathered many of the early leaders in the U.S. in the field of obesity research to try to sort out whether obesity was one or many diseases. At that meeting at Vassar College in Poughkeepsie, NY, George chaired the organizing committee that was to develop a plan to establish what became the North American Association for the Study of Obesity (NAASO, now called The Obesity Society). Barbara Hansen became the first president of NAASO, and George later became its fifth president. That effort also led to the establishment of the official International Association for the Study of Obesity (IASO) that was formulated at a meeting in Brighton, England, representing about a dozen countries with commitments to obesity research (of which George later was to serve as a president). The first meeting was held in Israel. He served 4 years on the Advisory Council of the National Institute of Diabetes and Digestive and Kidney Diseases, 4 years on the Board of Regents of the American College of Physicians, and 1 year as president of the American Society for Clinical Nutrition.
Building an Obesity Research Center and Continuing Scholarship (1989–2015)
In 1989, George became the executive director of the nascent Pennington Biomedical Research Center at Louisiana State University in Baton Rouge, LA. During his 10 years as its director, it rose to become an internationally recognized nutrition research center with a strong focus on obesity research and energy metabolism. As executive director, he oversaw the growth of the facility from 25 employees and a million dollar budget to a flourishing research enterprise with over 70 scientists, 350 employees, and an annual budget of nearly $20 million. Today, Pennington Biomedical has grown into a research enterprise with an annual operating budget of over $62 million per year! George recruited key scientists such as York, who became the first head of basic research, leading the Experimental Obesity Research Program, and he chose Donna Ryan to lead the center’s first clinical research team. George and his growing team also attracted key institutional grants. Although his chief responsibility during this period was developing the programs at Pennington Biomedical, he maintained a basic science laboratory and led clinical research projects. Those basic and clinical activities continued beyond his tenure as an administrator, when he joined the faculty ranks in 2001 as a Boyd Professor, Louisiana State University’s highest academic rank.
With unparalleled resources to support basic science and clinical research, George led research teams at Pennington Biomedical that have had a major influence on modern assumptions about the biology of obesity. The first major study in this category was the Dietary Approaches to Stop Hypertension, or DASH, study. Pennington Biomedical and four other nutrition research leading centers initiated a feeding study that tested dietary patterns for effects on blood pressure. Given the hypothesis that magnesium, calcium, potassium, and fiber would have salutatory effects on blood pressure, the study tested increasing consumption of fruits and vegetables and low-fat dairy products as sources of these factors. It produced clinically significant reductions of blood pressure in men and women of all ethnic groups (9). Because the dietary pattern translates into an easily understood public health message, the DASH diet has been considered one of the best diets in America and is recommended by most national guidelines.
The power of modest weight loss to produce health improvement is a major contribution to field of clinical treatment in obesity. That one does not need to fully normalize body weight has huge implications for clinical care in obesity. George has been a leader in developing and executing the two landmark clinical studies in testing the effect of weight loss achieved through lifestyle intervention. He was the leader of the Pennington Biomedical clinical site in the Diabetes Prevention Program (DPP), which began in 1996 and continues as the Diabetes Prevention Program Outcome Study (DPPOS). After the first 3.2 years of DPP, the lifestyle intervention reduced the conversion rate from impaired glucose tolerance to type 2 diabetes by 58% and a metformin treatment group had a reduced conversion rate of 31% (10). The 10-year outcome data (11) confirmed the durability of the initial intervention in reducing the long-term risk of developing diabetes.
The other landmark study of lifestyle intervention benefitting from George’s contribution and his tenure at Pennington Biomedical is the Look AHEAD (Action for Health in Diabetes) trial. This study recruited over 5,000 people with overweight or obesity and diabetes and randomly assigned them to a diabetes support condition or an intensive lifestyle intervention (ILI). At the end of the first year the average weight loss was 8.6% for those in the ILI condition compared with 0.9% loss in the support condition (12). At 4 years, some weight had been regained (14), and the study was continued in observation beyond the 4 years of active intervention. Although the study did not show a difference at 10.5 years in the primary end point (a composite of cardiovascular events) between the groups (15), the study is notable for documenting the benefits of modest weight loss. For those in ILI, there were long-term improvements in cardiovascular risk factors, glycemia, diabetes medication use, and even conversion to normoglycemia (12–15). Further, the study showed modest weight loss with lifestyle intervention produced improvements in symptoms of obstructive sleep apnea (16), hepatic steatosis (17), quality-of-life measures (18), depression (19), decline in mobility associated with aging (20), urinary incontinence (21,22), sexual function (23,24), and cost of medical care (25).
There has long been great scientific and popular interest in macronutrient approaches to dieting that might magically produce and sustain weight loss. In collaboration with Frank Sacks, MD, from the Harvard School for Public Health, George designed and executed the Preventing Obesity Using Novel Dietary Strategies (POUNDS LOST) study. This study assessed macronutrient content of the diet on the background of a uniform program of behavior modification and exercise. This study used an ingenious 2 × 2 factorial design to compare 20% vs. 40% fat and 15% vs. 25% protein. Thus the study had the ability to compare four levels of carbohydrate content (35%, 45%, 55%, and 65%). This well-executed study (811 subjects with a 2-year completion rate of 80%) clearly shows that calories count and that the macronutrient composition of the diet does not have a measurable effect on the rate or quantity of weight lost (26). In contrast, adherence to the dietary program was central to predicting weight loss (27).
Pennington Biomedical’s unsurpassed metabolic study and clinical research facilities and U.S. Department of Agriculture funding enabled George to pursue his curiosity and interest in factors that influence risk for obesity. On the basis of his early interest in animal models that became obese on a high-fat diet, he developed studies asking how people adapt, or fail to adapt, to eating a high-fat diet. He showed that the rate of adaptation to a high-fat diet was much slower than for a high-carbohydrate diet (28). More important, for the public health perspective, was that the rate of adapting to a high-fat diet could be increased with exercise (29).
George’s early interest in overfeeding, which spurred his personal experimentation, returned and he executed a study comparing three groups of individuals who were overfed at a level 40% above maintenance requirements for 8 weeks with diets varying in protein content (5%, 15%, or 25%). The subjects eating the low-protein diet gained significantly less weight than the subjects consuming the 15% or 25% protein diets, but the quantity of fat deposited, as determined by dual-energy X-ray absorptiometry, was identical. Subjects eating the low-protein diet did not increase their resting energy expenditure or body protein stores and the extra calories were stored as fat. Those eating the 15% and 25% protein diets increased their resting energy expenditure and stored more protein but less fat. These findings suggest that higher-protein diets are associated with less fat storage and that low-protein diets will not spare protein but will enhance energy storage as fat (30).
During his decade as executive director at Pennington Biomedical, George laid the foundation for the center’s growth trajectory and it became world renown. After stepping down from the executive director post in 1999, he remained an active Pennington Biomedical faculty member, continuing to make many seminal contributions to the field of nutrition research, particularly to the area of obesity. In 2014, he formally retired from Pennington Biomedical and Louisiana State University bestowed upon him the rank of Professor Emeritus.
Show Me the Boy and I Will Show You the Man
That early teacher may have been wrong in stating that the 11-year-old George was “average,” but the teacher did recognize George’s interest and aptitude for “all subjects.” Indeed, the remarkable attribute of George’s scientific career is its breadth. His work bridges molecule to man to populations. George self-identifies (1) four major themes that continue to guide his interests, as follows:
A metabolic and endocrine hypothesis of obesity (6) that later became known as MONA LISA, which stands for Most Obesities knowN Are Low In Sympathetic Activity (31)
The concept that prevention of obesity, similar to the prevention of dental caries, might come from the surreptitious manipulation of environmental factors—the FLUORIDE (For Lowering Universal Obesity Rates Implement ideas that Don't demand Effort) hypothesis for the prevention of obesity (32)
Changes in the content of sucrose and fructose in the food supply as potential environmental drivers of obesity and its complications (33)
These self-described interests, some of which remain hypothetical and demand further study, speak to George’s broad and comprehensive knowledge of body weight regulation and its dysregulation and enable him to creatively explore discovery from bench to bedside to populations.
Certainly no man is merely his curriculum vitae. George’s finest qualities are not listed in that document, though it does reflect those qualities—perseverance, civility, industry, optimism, curiosity, and creativity. His success is not based solely on his scientific acumen but also on his social skills and ability to mentor and to promote the careers of his collaborators. A cadre of mentees (Donna Ryan, David York, Steven Smith, Ken Fujioka, Frank Greenway, Richard Atkinson, and Jennifer Lovejoy, among others) have established successful independent careers. Long-time collaborators such as Barbara Hansen, Richard Bergman, and Frank Sacks are not just colleagues but friends.
In his free time, George loves adventure travel (to most of the countries of the world), theater (for which he has a scholarly and intense appreciation), and his large and growing family (between his children and Mitzi’s five children, Timothy, Bradley, Clinton, Sally, and William, together they currently have 16 grandchildren). These enriching aspects of his life create qualities that are more than his singular scientific abilities. This multidimensional aspect of his character is what made him capable of shaping the field of obesity inquiry. Throughout his career he has been an advocate for patients and an early explorer of the biology that underlies their struggle with excess body weight and its consequences. His impact on the field is measurable in leading to the current understanding that obesity is a disease to be taken seriously.
One of the major characteristics of George is his calming effect on others and his clear direction of the science. While guiding the research at Pennington, it was well known that the study was best conducted “George’s way!” Interestingly, it also became apparent that George took the same path every day from his office to the basic and administrative buildings at Pennington Biomedical. Thus, the path became known as “George’s way,” and on his retirement, and due to his work in a lifetime of obesity, there was a play on words, and the path is now dedicated to George with a permanent plaque distinguishing it as Bray’s “Weigh.” As you can see, the boy in George has not changed, but he changed obesity forever.
References
- 1.Bray GA. Why obesity? Annu Rev Nutr 2015;35:1–31 [DOI] [PubMed] [Google Scholar]
- 2.Bray GA. The Battle of the Bulge. Pittsburgh, PA, Dorrance Publishing, 2007 [Google Scholar]
- 3.Bray GA. A simple efficient liquid scintillator for counting aqueous solutions in a liquid scintillation counter. Anal Biochem 1960;1:279–285 [Google Scholar]
- 4.Bray GA, Gallagher TF Jr. Manifestations of hypothalamic obesity in man: a comprehensive investigation of eight patients and a review of the literature. Medicine (Baltimore) 1975;54:301–330 [DOI] [PubMed] [Google Scholar]
- 5.Bray GA, Dahms WT, Swerdloff RS, Fiser RH, Atkinson RL, Carrel RE. The Prader-Willi syndrome: a study of 40 patients and a review of the literature. Medicine (Baltimore) 1983;62:59–80 [PubMed] [Google Scholar]
- 6.Bray GA, York DA. Hypothalamic and genetic obesity in experimental animals: an autonomic and endocrine hypothesis. Physiol Rev 1979;59:719–809 [DOI] [PubMed] [Google Scholar]
- 7.Nishizawa Y, Bray GA. Ventromedial hypothalamic lesions and the mobilization of fatty acids. J Clin Invest 1978;61:714–721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.York DA, Bray GA. Dependence of hypothalamic obesity on insulin, the pituitary and the adrenal gland. Endocrinology 1972;90:885–894 [DOI] [PubMed] [Google Scholar]
- 9.Appel LJ, Moore TJ, Obarzanek E, et al.; DASH Collaborative Research Group . A clinical trial of the effects of dietary patterns on blood pressure. N Engl J Med 1997;336:1117–1124 [DOI] [PubMed] [Google Scholar]
- 10.Knowler WC, Barrett-Connor E, Fowler SE, et al.; Diabetes Prevention Program Research Group . Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Diabetes Prevention Program Research Group, Knowler WC, Fowler SE, Hamman RF, et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet 2009;374:1677–1686 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Pi-Sunyer X, Blackburn G, Brancati FL, et al.; Look AHEAD Research Group . Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the Look AHEAD trial. Diabetes Care 2007;30:1374–1383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wing RR; Look AHEAD Research Group . Long-term effects of a lifestyle intervention on weight and cardiovascular risk factors in individuals with type 2 diabetes mellitus: four-year results of the Look AHEAD trial. Arch Intern Med 2010;170:1566–1575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wing RR, Bolin P, Brancati FL, et al.; Look AHEAD Research Group . Cardiovascular effects of intensive lifestyle intervention in type 2 diabetes. N Engl J Med 2013;369:145–154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gregg EW, Chen H, Wagenknecht LE, et al.; Look AHEAD Research Group . Association of an intensive lifestyle intervention with remission of type 2 diabetes. JAMA 2012;308:2489–2496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kuna ST, Reboussin DM, Borradaile KE, et al.; Sleep AHEAD Research Group of the Look AHEAD Research Group . Long-term effect of weight loss on obstructive sleep apnea severity in obese patients with type 2 diabetes. Sleep 2013;36:641–649A [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lazo M, Solga SF, Horska A, et al.; Fatty Liver Subgroup of the Look AHEAD Research Group . Effect of a 12-month intensive lifestyle intervention on hepatic steatosis in adults with type 2 diabetes. Diabetes Care 2010;33:2156–2163 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williamson D, Rejeski J, Lang W, et al.; Look AHEAD Research Group . Impact of a weight management program on health-related quality of life in overweight adults with type 2 diabetes. Arch Intern Med 2009;169:163–171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Faulconbridge LF, Wadden TA, Rubin RR, et al.; Look AHEAD Research Group . One-year changes in symptoms of depression and weight in overweight/obese individuals with type 2 diabetes in the Look AHEAD study. Obesity (Silver Spring) 2012;20:783–793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rejeski WJ, Ip EH, Bertoni AG, et al.; Look AHEAD Research Group . Lifestyle change and mobility in obese adults with type 2 diabetes. N Engl J Med 2012;366:1209–1217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Phelan S, Kanaya AM, Subak LL, et al.; Look AHEAD Research Group . Weight loss prevents urinary incontinence in women with type 2 diabetes: results from the Look AHEAD trial. J Urol 2012;187:939–944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Breyer BN, Phelan S, Hogan PE, et al.; Look AHEAD Research Group . Intensive lifestyle intervention reduces urinary incontinence in overweight/obese men with type 2 diabetes: results from the Look AHEAD trial. J Urol 2014;192:144–149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wing RR, Rosen RC, Fava JL, et al. Effects of weight loss intervention on erectile function in older men with type 2 diabetes in the Look AHEAD trial. J Sex Med 2010;7:156–165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wing RR, Bond DS, Gendrano IN 3rd, et al.; Sexual Dysfunction Subgroup of the Look AHEAD Research Group . Effect of intensive lifestyle intervention on sexual dysfunction in women with type 2 diabetes: results from an ancillary Look AHEAD study. Diabetes Care 2013;36:2937–2944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Espeland MA, Glick HA, Bertoni A, et al.; Look AHEAD Research Group . Impact of an intensive lifestyle intervention on use and cost of medical services among overweight and obese adults with type 2 diabetes: the Action for Health in Diabetes. Diabetes Care 2014;37:2548–2556 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sacks FM, Bray GA, Carey VJ, et al. Comparison of weight-loss diets with different compositions of fat, protein, and carbohydrates. N Engl J Med 2009;360:859–873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Williamson DA, Anton SD, Han H, et al. Adherence is a multi-dimensional construct in the POUNDS LOST trial. J Behav Med 2010;33:35–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Smith SR, de Jonge L, Zachwieja JJ, et al. Fat and carbohydrate balances during adaptation to a high-fat. Am J Clin Nutr 2000;71:450–457 [DOI] [PubMed] [Google Scholar]
- 29.Smith SR, de Jonge L, Zachwieja JJ, et al. Concurrent physical activity increases fat oxidation during the shift to a high-fat diet. Am J Clin Nutr 2000;72:131–138 [DOI] [PubMed] [Google Scholar]
- 30.Bray GA, Smith SR, de Jonge L, et al. Effect of dietary protein content on weight gain, energy expenditure, and body composition during overeating: a randomized controlled trial. JAMA 2012;307:47–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bray GA. Obesity, a disorder of nutrient partitioning: the MONA LISA hypothesis. J Nutr 1991;121:1146–1162 [DOI] [PubMed] [Google Scholar]
- 32.Bray GA. The FLUORIDE hypothesis and DIOBESITY: how to prevent diabetes by preventing obesity. In Progress in Obesity Research: 9. Medeiros-Neto G, Halpern A, Bouchard EC, Eds. London, John Libbey, 2003, p. 26–28 [Google Scholar]
- 33.Bray GA, Popkin BM. Dietary sugar and body weight: have we reached a crisis in the epidemic of obesity and diabetes? Health be damned! Pour on the sugar. Diabetes Care 2014;37:950–956 [DOI] [PMC free article] [PubMed] [Google Scholar]