Abstract
Introduction:
Peritonitis is one of the most common problems in general surgery practice with high mortality rate. One of the reasons for high mortality is that peritonitis affects the general condition and leads to complications causing multiple organ failure, renal failure, sepsis, and postoperative ventilatory support. Early prognostic evaluation of patients with peritonitis is desirable to select high-risk patients for intensive management and also to provide a reliable objective classification of severity and operative risk.
Patients and Methods:
Fifty cases with diagnosis of peritonitis coming to Government Medical College, Amritsar, were studied. Stratification of these patients was done according to Mannheim peritonitis index (MPI), and their outcome was examined.
Results:
Mortality steadily increases with increase in MPI score. For patients with a score <21, the mortality rate was 0%; for score 21–27, it was 27.28%; and for score >27, it was 100% (P < 0.001). For patients with a score <21, the morbidity rate was 13.33%; for score 21-27, it was 65.71%; and for score >27, it was 100% (P < 0.001). Duration of pain >24 h, organ failure on admission, female sex, and feculent exudate were found to be independently significant factors in predicting the mortality among the study population. For a score of 27, the sensitivity was 66.67%, specificity was 100%, and positive predictive value for mortality is 100% at an accuracy of 94%.
Conclusion:
This study proves that MPI scoring system is a simple and effective tool for assessing the morbidity and mortality in patients with peritonitis.
KEYWORDS: Mannheim peritonitis index, morbidity, mortality, organ failure, peritonitis
INTRODUCTION
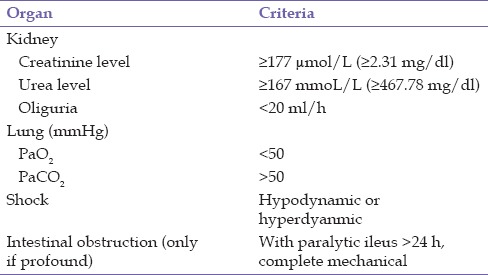
Peritonitis denotes inflammation of the peritoneum from any cause. It may be regarded as the localized equivalent of the systemic inflammatory response seen after any trigger of inflammation,[1,2] which recently has been described as systemic inflammatory response syndrome.[3] The complex nature of surgical infections, the multifaceted aspects of treatment, and the complexity of Intensive Care Unit (ICU) support makes evaluation of new diagnostic and therapeutic advances in this field very difficult. Many scoring systems have been tried to predict death in peritonitis. Mannheim peritonitis index (MPI) is a scoring system used in peritonitis which is simple and cost-effective. MPI was originally derived from data collected from 1253 patients with peritonitis treated between 1963 and 1979 and was developed by discriminant analysis of 17 possible risk factors, by Wacha, 8 of these were of prognostic relevance and was currently employed widely for predicting mortality from peritonitis.[4] The information is collected at the time of admission and first laparotomy [Tables 1 and 2].[4]
Table 1.
Mannheim peritonitis index
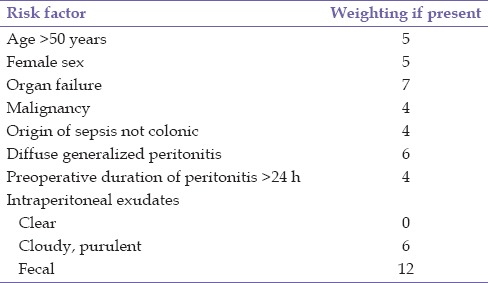
Table 2.
Organ failure
PATIENTS AND METHODS
The study was done in fifty patients with peritonitis who presented at Government Medical College, Amritsar, and were operated after taking informed consent. Patients with associated vascular, neurogenic injuries were excluded from the study. Patients were scored from the data available preoperatively and operative findings according to MPI. Patients were followed up for the final outcome, and results were analyzed with the score of MPI.
RESULTS
In this study, majority of patients belonged to age group of 21-50 years. The youngest patient was 8-year-old female, whereas to oldest was a 65-year-old male. There were 82% male patients and 18% female patients with the male to female ratio being 4.6:1 [Figure 1].
Figure 1.
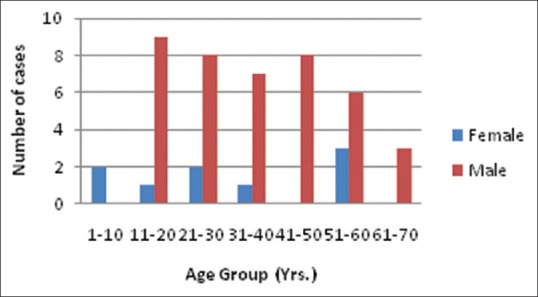
Age and sex incidence
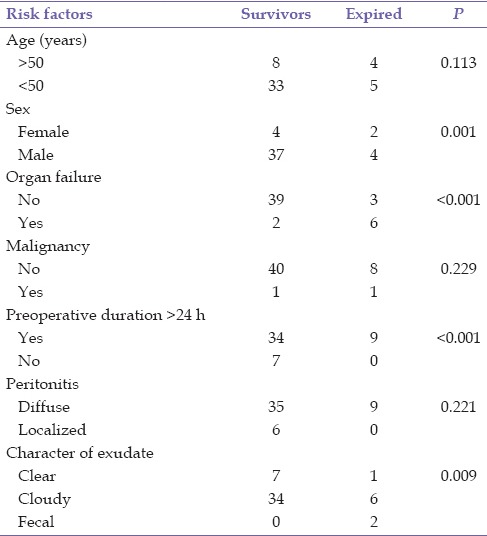
It was found that the mortality rate is 13.16% for patients <50 years and 33.33% for patients more than 50 years. It was further found that mortality for female patients was 55.56%, and for male patients, it was 9.76%. In patients with localized peritonitis, there was no mortality as compared to diffuse peritonitis which had mortality of 20.45%.
Majority of the patients presented to hospital after 24 h (86%), and most commonly during 48-72 h (44%). The mortality of patients was highest (66%) who were presented to hospital after 72 h, and it was 33% who were presented between 48 and 72 h. There was no mortality for patients who presented within 48 h.
The mortality of patients who had clear, cloudy, and fecal character of exudates was 12.5%, 15%, and 100%, respectively. For patients with no malignancy, mortality was 16.67% as compared to patients having malignancy, mortality was 50%. Patients’ having no organ failure preoperatively, mortality was 7.14% as compared to patients having organ failure, mortality was 75% [Table 3].
Table 3.
Summary of risk factors of Mannheim peritonitis index and mortality
The study showed that mortality steadily increases with increase in MPI score showing statistically significant results [P < 0.001, Figure 2].
Figure 2.
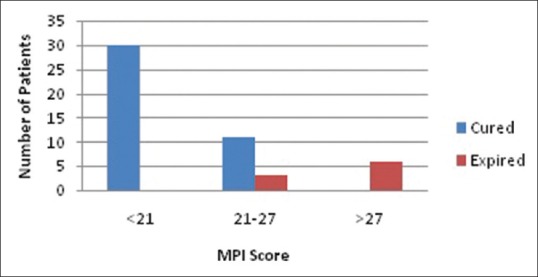
Mortality and Mannheim peritonitis index score
Various postoperative complications seen in the study group were wound sepsis, wound dehiscence, acute renal failure, pneumonitis, acute respiratory distress syndrome, and shock. The study also showed that morbidity steadily increases with MPI score [P < 0.001, Figure 3].
Figure 3.
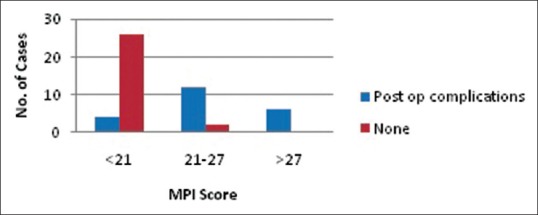
Morbidity and Mannheim peritonitis index score
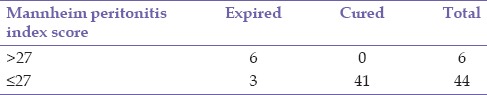
For a score of 27, the sensitivity was 66.67%, specificity was 100%, and positive predictive value for mortality is 100% at an accuracy of 94% [P < 0.001, Table 4].
Table 4.
Sensitivity and specificity of Mannheim peritonitis index score 27
DISCUSSION
Peritonitis, inflammation of serosal membrane lining the abdominal cavity and abdominal viscera, is associated with high mortality rate.[5] Peritonitis remains a hot spot for the surgeons despite advancements in surgical technique and intensive care treatment. Various factors such as age, sex, duration, site of perforation, extent of peritonitis, and delay in surgical intervention are associated with morbidity and mortality.
Bacteria and digestive enzymes act on the peritoneal serosal surface lead to enzymatic digestion and necrosis and an outpouring of serum protein and electrolytes from the blood to the cavity. There is formation of exudate rich in granulocytes, which may be diffuse or confined to an abscess. Systemically, there is paralysis of the bowel, hemoconcentration occurs, and alterations of the cardiac output due to the shift of fluids and later acidosis. Intrapulmonary shunting, hypo- or hypercapnia, hypoxemia, progressive azotemia, acute tubular necrosis, weight loss by protein consumption, fall of body temperature, loss of heat production, and exhaustion are other complications that may lead to the death of the patient, if the process is not interrupted.
A successful outcome depends on early surgical intervention, source control, and exclusive intraoperative peritoneal lavage. It may also depend on exact recognition of the seriousness of the disease, an accurate assessment, and classification of the patient's risks.[6] Despite the surgical treatment and sophisticated ICUs, last generation antibiotics and a better understanding of pathophysiology of peritonitis mortality rate are still very high, i.e., 10–20% even in good institutions.[7] Early prognostic evaluation is necessary to select high-risk patients for more aggressive therapeutic procedures such as radical debridement, lavage systems, open management, and planned reoperations.
Classification of the severity of disease means the definition of groups by risk, and it is of confirmed value in both controlled and uncontrolled clinical trials. An accurate risk index classification is only method to settle a standard of comparison between groups of patient and different treatment methods which would allow further prospective adequate comparative study. MPI is a simple and effective tool in predicting outcome in cases of peritonitis. The MPI has a definite score for an individual, which has a good accuracy. It uses clinical parameters and predicts of the individual prognosis of patients with peritonitis.
MPI can be used to define risk groups as well as predict outcome in patients with peritonitis, as indicated by various studies. Wach et al. showed patients who obtained <21 points and more than 29 points, mortality rate was 6% and 50%, respectively.[4] Notash et al. showed mortality at score of above 21 and 29 of 60% and 100%, whereas Függer et al. showed below 21, no mortality; between 21 and 29, mortality was 29%; and more than 29, it was 100%.[8,9] Studies showed mortality among patients who obtained <21 points varied between 0% and 2.3%, in the 21–29-point group between 3.85% and 60%, and in patients with score of >29 – between 15% and 100%.[9,10,11,12,13] Billing's meta-analysis showed the following mean mortality rates in the groups with <21 points, between 21 and 29 points, and above 29 points: 2.3% (0–11%), 22.5% (10.6–50%), and 59.1% (41–87%), respectively.[14] Other studies have also shown statistically significant relation of morbidity and mortality with increasing MPI score.[15,16,17,18,19,20,21,22] Many studies used different cutoff points for better prediction of mortality. Yoshiko and Masayuki showed patients with MPI score of 26 or less have mortality of 3.8%, whereas score of 26 or more had mortality of 41%.[15] Bosscha et al. showed 100% mortality above MPI of 27.[16] Such difference in cutoff values might be due to different demographics and therapeutic options offered to patients at different institutions. In our study, score of 27 showed the sensitivity, specificity, and positive predictive value at 66.67%, 100%, and 100%, respectively, at an accuracy of 94%. In our study showed mortality rate with score <21, 21-27, and >27 was 0%, 27.28%, and 100%, respectively. Similarly, morbidity rate for patients with a score <21, 21-27, and >27 was 13.33%, 65.71%, and 100%, respectively. The predictions resulting from MPI were reliable, indicating stratification of risk groups can be done by probability intervals.
Correia et al. study showed that age >50 years out of a total of 79.3% death was seen in 85.2% and survival in 67.6% and P = 0.04, thus showing that age >50 years is a significant risk factor.[6] In our study, patients <50 years, mortality rate is 13.16%, and for patients more than 50 years, the mortality rate is 33.33% although it did not reach statistically significant values (P = 0.113).
Wittmann showed in his study, a high mortality rate (50%) when the diagnosis of peritonitis was made after 48 h.[23] The observed high frequency of patients with preoperative peritonitis duration longer than 24 h (65.5%) was correlated with high death rate. Our study also showed similar results with mortality of patients who presented between 48 and 72 h was 33% and >72 h was 66% as compared to no mortality who presented within 24 and 48 h (P < 0.001).
A study by Basnet and Sharma, out of the fifty patients included in the study, 21 (42%) were female and 29 (58%) were male. About 24.1% of the males and 19% of females requiring relaparotomy expired in the study, making female sex not a bad prognosticator in their study (P = 0.100).[24] Although our study showed female sex, a significant risk factor for mortality. Mortality for female patients was 55.56% as compared to male patients having mortality of 9.76% (P = 0.001).
The study by Notash et al. had mortality 17.5% mostly due to organ failure and septicemia.[8] Our study also showed organ failure, a significant risk factor as patients having organ failure had mortality of 75% as compared to no organ failure having mortality of 7.14% (P < 0.001). Another study concluded that with age more than 50 years, late presentation, diffuse peritonitis, purulent exudate, noncolonic pathology, and organic failure associated with high MPI score and more mortality.[25]
This study proves that MPI scoring system is a simple and effective tool for assessing the morbidity and mortality in patients with peritonitis with statistically significant results. Duration of pain >24 h, organ failure on admission, female sex, and feculent exudate were found to be independently significant factors in predicting the mortality.
CONCLUSION
Increasing score of MPI predicts poor prognosis. It is associated with increased morbidity and mortality. Such patients should be monitored closely with close attention to be given to support the vital systems. To conclude, MPI is a simple and reliable tool in predicting the outcome in cases of peritonitis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Goris RJ, te Boekhorst TP, Nuytinck JK, Gimbrère JS. Multiple-organ failure. Generalized autodestructive inflammation? Arch Surg. 1985;120:1109–15. doi: 10.1001/archsurg.1985.01390340007001. [DOI] [PubMed] [Google Scholar]
- 2.Marshall J, Sweeney D. Microbial infection and the septic response in critical surgical illness. Sepsis, not infection, determines outcome. Arch Surg. 1990;125:17–22. doi: 10.1001/archsurg.1990.01410130019002. [DOI] [PubMed] [Google Scholar]
- 3.Bone RG. Sepsis, SIRS and MODS: The New Definition. Proceedings of Sepsis/SIRS; 21-22 February, 1995; Washington, DC. [Google Scholar]
- 4.Linder MM, Wacha H, Feldmann U, Wesch G, Streifensand RA, Gundlach E. [The Mannheim peritonitis index. An instrument for the intraoperative prognosis of peritonitis] Chirurg. 1987;58(2):84–92. [German] [PubMed] [Google Scholar]
- 5.Seiler CA, Brügger L, Forssmann U, Baer HU, Büchler MW. Conservative surgical treatment of diffuse peritonitis. Surgery. 2000;127:178–84. doi: 10.1067/msy.2000.101583. [DOI] [PubMed] [Google Scholar]
- 6.Correia MM, Thuler LC, Velasco E, Vidal EM, Schanaider A. Prediction of death using the Mannheim peritonitis index in oncologic patients. Rev Bras Cancerologia. 2001;47:63–8. [Google Scholar]
- 7.Weigelt JA. Empiric treatment options in the management of complicated intra-abdominal infections. Cleve Clin J Med. 2007;74(Suppl 4):S29–37. doi: 10.3949/ccjm.74.suppl_4.s29. [DOI] [PubMed] [Google Scholar]
- 8.Notash AY, Salimi J, Rahimian H, Fesharaki Ms, Abbasi A. Evaluation of Mannheim peritonitis index and multiple organ failure score in patients with peritonitis. Indian J Gastroenterol. 2005;24:197–200. [PubMed] [Google Scholar]
- 9.Függer R, Rogy M, Herbst F, Schemper M, Schulz F. Validation study of the Mannheim peritonitis index. Chirurg. 1988;59:598–601. [PubMed] [Google Scholar]
- 10.Batra P, Gupta D, Batra R, Kothari R, Deshmukh PR. Mannheim peritonitis index as an evaluative tool in predicting mortality in patients of perforation peritonitis. CIBTech J Surg. 2013;2:30–6. [Google Scholar]
- 11.Chandrashekar N, Prabhakar GN, Gurukiran CS, Shivakumarappa GM, Naveen HM. Study of prognostic factors in perforative peritonitis. J Evol Med Dent Sci. 2013;2:5568–74. [Google Scholar]
- 12.Ermolov AS, Bagdat’ev VE, Chudotvortseva EV, Rozhnov AV. Evaluation of the Mannheim peritonitis index. Vestn Khir Im I I Grek. 1996;155:22–3. [PubMed] [Google Scholar]
- 13.Qureshi AM, Zafar A, Saeed K, Quddus A. Predictive power of Mannheim peritonitis index. J Coll Physicians Surg Pak. 2005;15:693–6. [PubMed] [Google Scholar]
- 14.Billing A, Fröhlich D, Schildberg FW. Prediction of outcome using the Mannheim peritonitis index in 2003 patients. Peritonitis study group. Br J Surg. 1994;81:209–13. doi: 10.1002/bjs.1800810217. [DOI] [PubMed] [Google Scholar]
- 15.Yoshiko K, Masayuki N. Study of Mannheim peritonitis index to predict outcome of patients with peritonitis. Jpn J Gastroenterol Surg. 2004;37:7–13. [Google Scholar]
- 16.Bosscha K, Reijnders K, Hulstaert PF, Algra A, van der Werken C. Prognostic scoring systems to predict outcome in peritonitis and intra-abdominal sepsis. Br J Surg. 1997;84:1532–4. [PubMed] [Google Scholar]
- 17.Demmel N, Muth G, Maag K, Osterholzer G. Prognostic scores in peritonitis: The Mannheim peritonitis index or APACHE II? Langenbecks Arch Chir. 1994;379:347–52. doi: 10.1007/BF00191581. [DOI] [PubMed] [Google Scholar]
- 18.Gedik E, Girgin S, Taçyildiz IH, Akgün Y. Risk factors affecting morbidity in typhoid enteric perforation. Langenbecks Arch Surg. 2008;393:973–7. doi: 10.1007/s00423-007-0244-8. [DOI] [PubMed] [Google Scholar]
- 19.Mulari K, Leppäniemi A. Severe secondary peritonitis following gastrointestinal tract perforation. Scand J Surg. 2004;93:204–8. doi: 10.1177/145749690409300306. [DOI] [PubMed] [Google Scholar]
- 20.Kologlu M, Elker D, Altun H, Sayek I. Validation of MPI and PIA II in two different groups of patients with secondary peritonitis. Hepatogastroenterology. 2001;48:147–51. [PubMed] [Google Scholar]
- 21.Liverani A, Correnti SF, Paganelli MT, Antonini G, Mercati U. Mannhein index in the prognosis and treatment of acute peritonitis. Minerva Chir. 1998;53:385–9. [PubMed] [Google Scholar]
- 22.Rogy M, Függer R, Schemper M, Koss G, Schulz F. The value of 2 distinct prognosis scores in patients with peritonitis. The Mannheim peritonitis index versus the Apache II score. Chirurg. 1990;61:297–300. [PubMed] [Google Scholar]
- 23.Wittman DH. Intra-abdominal Infections: Pathophysiology and Treatment. New York: Marcel Dekker; 1991. pp. 48–51. [Google Scholar]
- 24.Basnet RB, Sharma VK. Evaluation of predictive power of Mannheim peritonitis index. Postgrad Med J NAMS. 2010;10:10–3. [Google Scholar]
- 25.Chaudhari ND, Nakum A, Mahida H. Mannheim's peritonitis index validation study in the Indian set-up. Int J Sci Res. 2014;3:1808–11. [Google Scholar]


