Abstract
Strategic priority setting and implementation of strategies to reduce maternal mortality are key to the post Millennium Development Goal (MDG) 2015 agenda. This article highlights the feasibility and the advantages of using a systematized tacit knowledge approach, using data from maternal health program personnel, to identify local challenges to implementing policies and programs to inform the post MDG era. Communities of practice, conceived as groups of people sharing professional interests, experiences and knowledge, were formed with diverse health personnel implementing maternal health programs in Mexico and Nicaragua. Participants attended several workshops and developed different online activities aiming to strengthen their capacities to acquire, analyze, adapt and apply research results and to systematize their experience and knowledge of the actual implementation of these programs. Concept mapping, a general method designed to organize and depict the ideas of a group on a particular topic, was used to manage, discuss and systematize their tacit knowledge about implementation problems of the programs they work in. Using a special online concept mapping platform, participants prioritized implementation problems by sorting them in conceptual clusters and rating their importance and feasibility of solution. Two hundred and thirty-one participants from three communities of practice in each country registered on the online concept mapping platform and 200 people satisfactorily completed the sorting and rating activities. Participants further discussed these results to prioritize the implementation problems of maternal health programs. Our main finding was a great similarity between the Mexican and the Nicaraguan general results highlighting the importance and the feasibility of solution of implementation problems related to the quality of healthcare. The use of rigorously organized tacit knowledge of health personnel proved to be a feasible and useful tool for prioritization to inform implementation priorities in the post MDG agenda.
Keywords: : Communities of practice, implementation research, low- and middle-income countries, quality, maternal health services, maternal mortality, tacit knowledge
Key Messages
The use of rigorously organized tacit knowledge of health personnel proves to be a powerful tool for prioritization in maternal health programs.
We report on an innovative approach to using tacit knowledge from health personnel on the front lines of care to develop priorities for quality improvement activities or implementation research.
It is pertinent and useful to use health personnel’s tacit knowledge to set post MDG agendas at the local level.
According to this tacit knowledge and its support on scientific literature, improving the quality of care in maternal health programs should be in the first place to guide post MDG agendas.
Introduction
Maternal mortality remains a priority global health concern, and health programs addressing it face great expectations to achieve stated health and policy goals. Despite a number of policies and programs targeting Millennium Development Goal (MDG) 5 (to reduce maternal mortality by 75% between 1990 and 2015), only a few countries will reach this goal. Two years before 2015, the global average reduction only reached 45% (United Nations 2014). In 2013, the maternal mortality ratio in developing regions (230 maternal deaths per 100 000 live births) was 14 times higher than that of developed regions (United Nations 2014). Even though important progress has been made in almost all regions, many countries, among them Mexico and Nicaragua, will not meet MDG5. Failure to achieve desired results has been explained as failure of implementation, particularly in developing countries (Peters et al. 2013).
In low- and middle-income countries (LMICs), although the design of policies and programs is increasingly based on available scientific evidence, it is not yet very common to find evidence-based decision making about the implementation of public health interventions (González-Block et al. 2008; 2011). The implementation of maternal health programs encompasses an array of real-world actors and processes involving health personnel, the adequate use of resources and the delivery of services, at the right time and for properly identified health needs. Thus, successful implementation of evidence-based interventions requires both organizational decisions at different levels to adopt an intervention and its actual implementation or everyday functioning, all of which will determine failure or success (González Block et al. 2011).
The need to develop reasonable and equitable priority setting mechanisms concerning maternal health is highly recognized (Shiffman 2007). Priority setting becomes particularly important in contexts where resources are limited. Different approaches to priority setting, mainly economical, have been advanced (Nair et al. 2014; Stefanini 1999). Notwithstanding these elements, the kind of evidence to be considered in public health should include not only the different perspectives of scientific research but also other factors such as the knowledge and views of the diverse stakeholders participating in maternal health programs (Nair et al. 2014; Panisset et al. 2012).
This article uses data from an Alliance for Health Policy and Systems Research (AHPSR)/World Health Organization-funded project that tested a capacity strengthening model for maternal health personnel in two LMICs: Mexico and Nicaragua. The project goal was based on existing evidence and aimed to strengthen health personnel’s capacity to use research results and to understand the core focus and characteristics of implementation research to guide evidence-based decision making in maternal health programs (González-Block et al. 2011; Rouvier et al. 2013).
Existing maternal health programs in Mexico and Nicaragua promote scientifically proven interventions; therefore, the capacity-building model of this project was initially oriented towards the utilization of implementation research (IR), the branch of health systems research dedicated to study the way any health intervention is made available to the public, answering how and why scientifically proven interventions fail or succeed in reaching their goals (Peters et al. 2013). Moreover, as Peters et al. (2013 p. 9) state, ‘implementation research is often at its most useful where implementers have played a part in the identification, design and conduct phases of the research undertaken’, combining the objective of strengthening maternal health programs’ personnel to use and apply scientific evidence with this characteristic of IR, the project worked on the systematization of the knowledge and perspectives of the people actually working in them. Because the actual implementation of policies and programs in local settings is always related to contextual factors, we considered the role of tacit knowledge as an important element that can offer important information on how national policies and programs developed to achieve the MDGs are implemented and function locally.
We considered the tacit knowledge of the people working in the implementation of maternal health programs as a potentially useful approach to identify and prioritize implementation challenges that need to be addressed. Tacit knowledge has been defined as a kind of knowledge that every human being has a relation to his or her everyday practice of a task or profession (Business Dictionary 2014; Polanyi 1966). Tacit knowledge is always linked to a particular individual, making it hard to formalize and communicate (Nonaka 1994). It includes two dimensions: (1) a technical element that has been described as the know how related to certain skills in a particular context and (b) a cognitive element that ‘refers to the individual’s images of reality and visions for the future, that is to say, what is and what ought to be’ (Nonaka 1994, p. 16). Other authors also note that it is usually shared through informal channels, and that to be transferred, it requires close or extensive personal contact and trust (Ambrosini and Bowman 2001; Kothari et al. 2011; Landry et al. 2006; McAdam et al. 2011). Finally, to assure its best utilization, tacit knowledge needs to be socialized and systematized.
The purpose of this article is to assess the feasibility of using the tacit knowledge methodology to prioritize challenges to implementation of current maternal health programs and inform the post MDG agenda in LMICs.
Methods
In this project, we implemented a participative approach by creating six communities of practice (CoPs). CoPs function as interactive interfaces in which researchers and practitioners can meet, motivated by common interests while they also foster their members’ development both personally and professionally (Bertone et al. 2013, Best et al. 2007; Wenger 1998). The CoPs were formed in three states of Mexico and three departments of Nicaragua and selected using three basic criteria: (1) relatively high (above national averages) rates of maternal mortality; (2) similar human development indexes and (3) presence of health authorities willing to participate in the project. The project included the states of Hidalgo, Morelos and Veracruz in Mexico and the departments of Chontales, Jinotega and Matagalpa in Nicaragua. The CoPs were formed during May to June 2013 following a call for participation launched by the health authorities in each state or department. Participants included managers of maternal health programs and personnel in contact with patients and other healthcare providers or administrators (Table 1). Participation in these CoPs was voluntary. In agreement with the corresponding health authorities, a person with expertise in information and communication technologies was named as a facilitator to organize each CoP and serve as link with the research team. We sought to engage the CoPs in a priority-setting process based on their tacit knowledge of implementation challenges, face-to-face workshops and a participatory online forum for the concept mapping exercise. These activities were held from July to December 2013.
Table 1.
Socio-demographic composition of CoP members from Mexico and Nicaragua with useful answers in Concept Mapping activities
| Variables | Mexico |
Nicaragua |
Total |
|||
|---|---|---|---|---|---|---|
| Total | % | Total | % | Total | % | |
| Sex | ||||||
| Male | 26 | 32.1 | 37 | 31.09 | 63 | 31.5 |
| Female | 55 | 67.9 | 82 | 68.91 | 137 | 68.5 |
| Age | ||||||
| <30 | 13 | 16.05 | 52 | 43.7 | 65 | 32.5 |
| 31–50 | 63 | 77.78 | 58 | 48.74 | 121 | 60.5 |
| >50 | 5 | 6.17 | 9 | 7.56 | 14 | 7 |
| Educationa | ||||||
| Below University | 9 | 11.11 | 41 | 34.45 | 50 | 25 |
| University/nursing/physician | 51 | 62.96 | 62 | 52.1 | 113 | 56.5 |
| Postgraduate | 21 | 25.92 | 16 | 13.44 | 37 | 18.5 |
| Nurse | 26 | 32.09 | 50 | 42.02 | 76 | 38 |
| Profession | ||||||
| Physician | 38 | 46.91 | 21 | 17.65 | 59 | 29.5 |
| Manager | 6 | 7.41 | 19 | 15.97 | 25 | 12.5 |
| Other | 11 | 13.58 | 29 | 24.37 | 40 | 20 |
| Place of work | ||||||
| Primary care | 53 | 65.43 | 77 | 64.71 | 130 | 65 |
| Hospitals | 17 | 20.99 | 23 | 19.33 | 40 | 20 |
| Administration | 11 | 13.58 | 19 | 15.97 | 30 | 15 |
| Total | 81 | 40.5 | 119 | 59.5 | 200 | 100 |
* Note In Mexico and Nicaragua physicians have a university level degree, while nurses may or may not have it.
Concept mapping was our main tool to extract and systematize what we defined as the ‘raw’ tacit knowledge of each CoP about the implementation challenges of various maternal health programs. Concept mapping is a general methodology that helps to organize and graphically present the ideas of a group of people about a subject of common interest (Trochim 1989). All participants gave informed consent to participate in concept mapping, and the whole process was performed in the six CoPs of the two countries. The first workshop was based in the following protocol:
A brief didactic presentation on health systems, implementation and implementation research.
The concept mapping initial brainstorming session to answer the focus question: What are the main problems of the state or departmental health system that represent an obstacle to reach the expected results of maternal health programs?
Participants were organized in groups of 6–10 people and asked to individually write 5–15 answers to the focus question based on their own personal experience.
Individual answers to the question were recorded on cards.
After discussion, each group eliminated duplicated or redundant answers.
Using this material and a content analysis approach, the research team collated and synthesized answers from all CoPs eliminating duplicates and redundancies across groups and reducing the list to 98 statements (Hsieh and Shannon 2005). During a second workshop, participants were trained on the use of the Concept Systems Global platform, an online tool, to perform the rest of the concept mapping activities online (Concept Systems Global 2014). The research team uploaded the 98 statements to the platform, and the research team leader formatted the platform according to the specific objectives of the project.
Each CoP member was next asked to perform five tasks on the online platform:
Register on the platform creating their own usernames and passwords.
Provide basic anonymous sociodemographic information (country, state or department, age, gender, education and main responsibilities in the maternal health programs).
Sort the 98 statements in conceptual clusters (minimum of 5 and a maximum of 20) and name them according to their own criteria to finally save their personal sorting results.
Rate each statement according to its importance using a Likert scale in which 1 equals ‘not important’ and 5 equals ‘of vital importance’.
Rate the feasibility of solving the problem referred in each statement on a similar Likert scale in which 1 equals ‘cannot be solved’ and 5 equals ‘it’s already being solved’.
Facilitators of the CoPs were responsible for the follow-up with each member to assure timely and accurate participation. The research team reviewed and confirmed the validity of each member’s information.
Using the statements and the results of the online sorting exercise, we generated clusters or conceptual groups using multidimensional scaling and a correlation matrix embedded in the platform, then weighted each cluster using the priority and feasibility data provided by CoP members. The cluster or conceptual group names were discussed with the CoPs in order to make sure that they accurately represented the main ideas of the statements gathered in each cluster. We next tested varying numbers of clusters (8, 10 and 12 clusters in a map) and presented the options to the CoPs for discussion. Consensus was reached that 10 cluster maps were the best.
We next used the average values of the importance and feasibility of solution rating scores for each statement to generate a correlation to identify the importance–feasibility relationship at the statement level. Starting with the discussion on the clusters, the selection of the particular problems to be addressed through implementation research was made by each CoP after discussing on the problems combining the highest scores for both criteria (importance and feasibility). We thus finished with cluster-level and statement-level average ratings of importance and feasibility, as well as a measure of joint importance and feasibility.
A thorough analysis of the concept mapping results was made during a 40-h workshop and an additional training on evidence-based decision making in public health and implementation research with 25 leaders of the different CoPs. By the end of the week, each CoP had started developing an implementation research protocol focused on a priority implementation problem to be discussed and finalized with the participation of all of its members. The analysis of the concept maps also served as basis for the selection of problems upon which a more local action would be undertaken after the elaboration of small intervention protocols.
Results
From the 298 participants in the brainstorming activities in both countries, 231 members of the six CoPs registered in the CSG platform and 200 people satisfactorily completed them (Table 1).
Our main finding was the similarity between the Mexican and the Nicaraguan general results as they appeared in their corresponding concept maps, particularly concerning both the importance and the feasibility of solution rating of two clusters: one containing the statements related to the quality of healthcare and another one gathering statements about the lack of financial resources. This led to consider the global concept maps of the two countries organizing the 98 ideas in 10 conceptual groups or clusters.
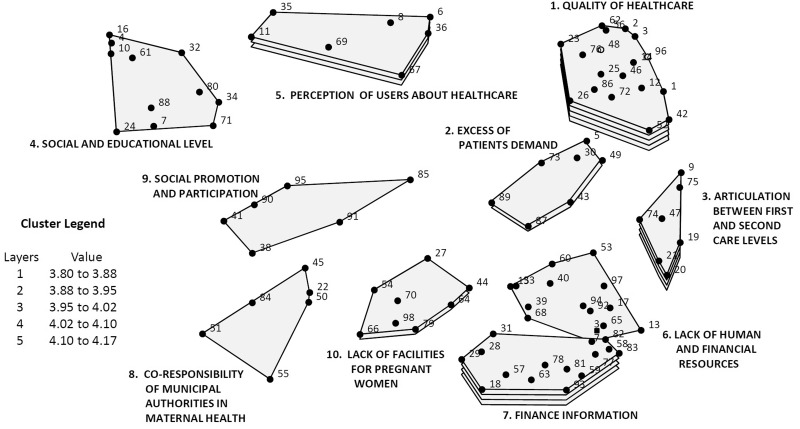
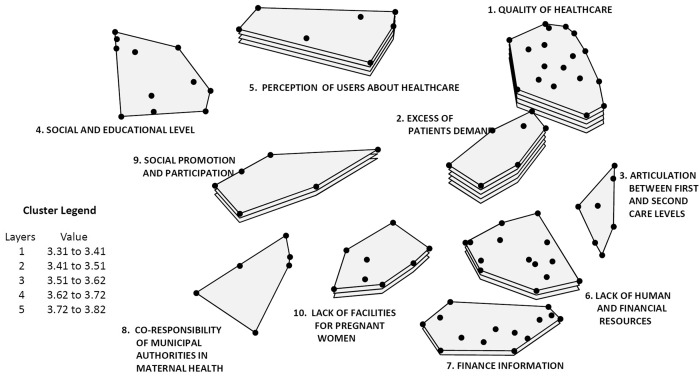
Figures 1 and 2 present the maps including the relevance of each cluster according to the average of its rating for importance (Figure 1) and feasibility of solution (Figure 2). The points in each cluster represent each one of the 98 problems identified by the CoPs, with their corresponding numbers, according to the random order given to them by the platform. The number of layers of each cluster represents the average rating: five layers represent the highest rating of the ideas, whereas only one layer is accorded to sets of ideas with the lowest rating average.
Figure 1.
Concept map of systematized tactic knowledge on maternal health programs implementation problems. Averaging rating (importance), Mexico and Nicaragua
Figure 2.
Concept map of systematized tactic knowledge on maternal health programs implementation problems. Averaging rating (feasibility), Mexico and Nicaragua
Cluster 1 ‘quality of healthcare’ in Figure 1 has five layers, showing the highest importance rating average, and it includes the largest number of statements (18 points), all of which describe different problems related to the quality of care. Two other clusters with four layers follow: Cluster 3 and Cluster 7. Including only two layers, Clusters 2 and 10 have average ratings between 3.88 and 3.95 while the average rating of the other three clusters with only one layer is below 3.88.
Concerning the feasibility of solution of the implementation problems, Figure 2 shows two clusters with high rating averages and, therefore, five layers: Cluster 1 ‘quality of healthcare’ and Cluster 3 ‘excess of patients demand’. The following cluster in feasibility of solution average rating is Cluster 5 with four layers, whereas three clusters show intermediate averages of feasibility rating: Clusters 6, 9 and 10. Instead, the rating of Cluster 7 corresponds to very difficult to resolve problems. Finally, the clusters that are the most difficult to resolve are 3 and 8.
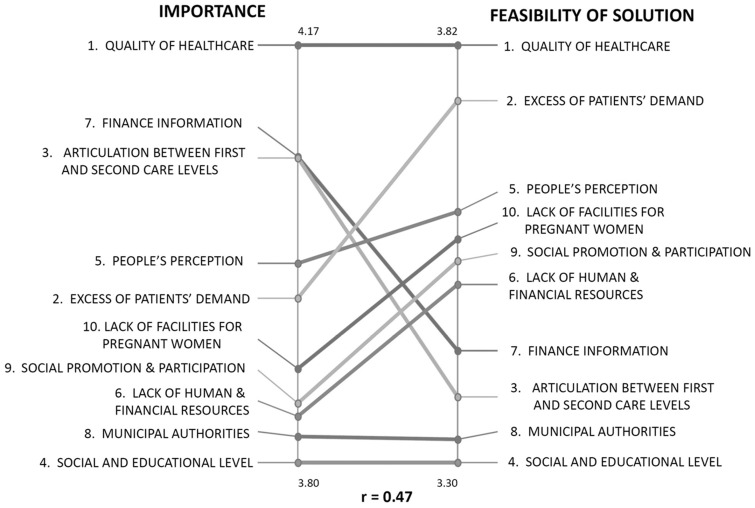
Figure 3 depicts the correlation of importance and feasibility ratings of each of the 10 clusters. This figure compares the average value of the two ratings of the statements included in each cluster. Some clusters were rated similarly—quality high on both, importance and feasibility, municipal authorities and social/educational level low on both—whereas others received different ratings for the two criteria.
Figure 3.
Correlation between average ratings of the 10 clusters of implementation problems of maternal health programs by Mexican and Nicaraguan CoPs
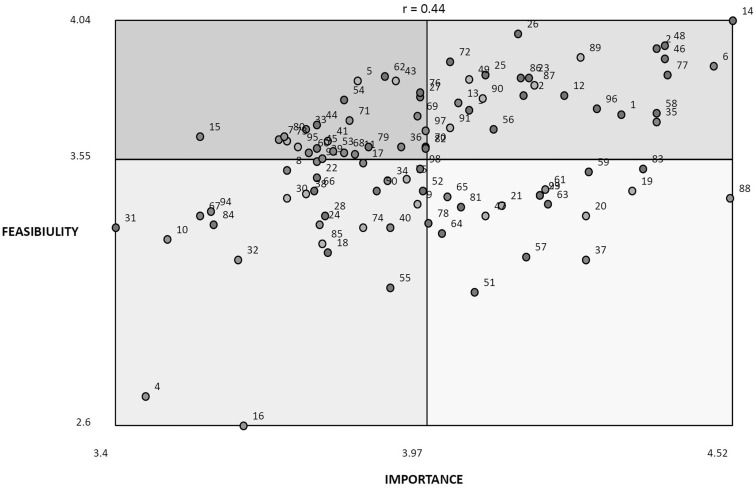
In addition to classifying the importance and feasibility rating of all clusters, we also classified individual statements according the highest average ratings for importance and feasibility of solution (Figure 4). The statements (problems) falling in Square I of Figure 4 combine the lowest rating for importance and feasibility of solution. Square II gathers those problems with a higher rating average for feasibility of solution, but a low rating concerning importance. Square III includes problems with a high importance average rating but low feasibility of solution. Finally, Square IV or Go Zone gathers those problems with the highest average ratings for importance and feasibility of solution. Logically, this is the priority zone where decision makers and researchers should look for the development of their proposals. The most important finding is that 15 out of 25 problems in Square IV focus on quality issues. Although the clusters correlation permitted to give a general orientation towards quality of health care, the position of each statement in Figure 4 permitted to focus, in particular, on implementation problems.
Figure 4.
Strategic zones of average ratings of implementation problems of maternal health programs by Mexican and Nicaraguan CoPs
Table 2 also shows that out of 25 statements in the Go Zone, 15 are part of Cluster 1 ‘quality of healthcare’, whereas the other 10 are distributed among five other clusters.
Table 2.
Individual statements that rated high on importance and feasibility, Mexican and Nicaraguan CoPs
| Statement Number | Statements rated high on both importance and feasibility Green Go Zone | Included in Cluster |
|---|---|---|
| 1 | Consultations for risk pregnancies are established in distant dates and even after the delivery date | Quality of care |
| 2 | Deficient valuation of pregnant women by the personnel who receives them (physicians and nurses) | Quality of care |
| 3 | Negative attitude during care of personnel towards pregnant women | Quality of care |
| 6 | Pregnant women and their families fail to make a timely detection of alarm signs | People’s perception |
| 12 | Bad reception of pregnant women in emergency cases by surveillance personnel in health units | Quality of care |
| 13 | Problems with the distribution of delivery care inputs | Lack of resources |
| 14 | Deficient quality of care during pregnancy, delivery and postpartum | Quality of care |
| 23 | High rate of refusal of care for pregnant women in health units | Quality of care |
| 25 | Lack of follow-up of postpartum by health care personnel | Quality of care |
| 26 | Lack of compliance to Official Norms and Practice Guides | Quality of care |
| 35 | Pregnant women fail to attend to antenatal control | People’s perception |
| 42 | Long waiting time for pregnant women’s care in health units | Quality of care |
| 46 | Inadequate follow-up of obstetric complications | Quality of care |
| 48 | Inadequate identification of obstetric risk by health personnel | Quality of care |
| 49 | Lack of follow-up and evaluation of maternal health care processes | Excess of demand |
| 56 | Lack of human attitudes in health personnel responsible for pregnant women’s care | Quality of care |
| 58 | Obstetric emergency and general care equipment is in bad conditions | Finance information |
| 72 | Limited follow-up of pregnant women in the first level of care | Quality of care |
| 77 | Lack of drugs for normal and emergency obstetric care | Finance information |
| 86 | Lack of follow-up in pregnant women’s care to guarantee an integral care | Quality of care |
| 87 | Human resources for health are badly trained during their studies | Excess of demand |
| 89 | Health personnel lacks training | Excess of demand |
| 90 | Sexual education programs for adolescents are not implemented | Social promotion |
| 91 | Community personnel linked with maternal health programs lacks training | Social promotion |
| 96 | Negligence on the part of health personnel | Quality of care |
Elaborated from the CSG platform analysis of statements.
After analyzing their own systematized tacit knowledge, the leaders of each CoP focused on the priority clusters and individual statements rated highly on both importance and feasibility of their state or department and decided upon the implementation problems they would choose either to develop a small local intervention protocol or a larger implementation research protocol. The first aimed at improving the implementation of local issues with high and relatively simple feasibility of solution concerning such things as prenatal control, obstetric risk identification, health professionals training, post-natal follow-up and the referral system. In the cases of problems demanding a deeper consideration and study, implementation research protocols were designed.
For the implementation research protocols, in Mexico, the CoP Hidalgo chose statements 2 (‘deficient valuation of pregnant women by the personnel who receives them -physicians and nurses’) and 14 (‘deficient quality of care during pregnancy, delivery and postpartum’). The choice of the CoP from Morelos was statement number 6 (‘pregnant women and their families fail to make a timely detection of alarm signs’), also in the Go Zone of both countries. In the case of Veracruz, the CoP also selected statement 14, but did not link it to any other one. In Nicaragua, also finding a relevant relationship between statements 14 and 26 (‘lack of compliance to official norms and practice guides’), the cops of Chontales and Jinotega resolved to address the quality of care vis-à-vis the Health Ministry’s norm on prenatal care (Ministerio de Salud 2008). Finally, the CoP of Matagalpa focused on statement number 48 (‘inadequate identification of obstetric risk by health personnel’) to work on an IR protocol.
Discussion
We report on an innovative approach to using tacit knowledge from health personnel on the front lines of care to develop priorities for quality improvement activities or implementation research. Our Communities of Practice and concept mapping approach was feasible and acceptable to participants. Tacit knowledge is supported by what we know from the literature. It is feasible and valuable to use tacit knowledge to prioritize problems in the implementation of maternal health programs that can eventually inform the post-MDG agenda at the local level. We are aware that tacit knowledge might leave certain issues aside, as could be the case of unsafe abortion, HIV and other stigmatized issues. So, even though we found it useful, we recognize that the tacit knowledge approach needs to be complemented by other methods. Our key finding is that deficiencies in the quality of maternal health care emerged as a priority issue based on the systemized tacit knowledge of participating healthcare personnel in both Mexico and Nicaragua. There was clear agreement on the high importance of problems related to the quality of care and on the high feasibility of addressing such problems. When compared with the other nine conceptual groups, the quality of care cluster, not only combines the highest rating for importance and feasibility of solution but also gathers the largest number of statements (18 points). Finally, 15 out of 25 individual statements describing implementation problems with the highest rating average for both criteria are quality of care problems.
CoPs in both countries identified factors determining deficient quality of care in public healthcare facilities that include pregnancy, childbirth and post-partum (Yemile Ordaz-Martínez et al. 2010). They considered human resources problems such as the lack of them or their deficient training, particularly in first-level health facilities (McIntosh et al. 2012). The absence of the humane sensibility among health personnel was also identified, as was the inaccurate assessment of obstetric risk, from which stems a deficient follow-up. Due to problems in timely admission, pregnant women are forced to look for care elsewhere and many complications derive from the delays originated in bad reference and counter-reference (Collado-Peña and Sánchez-Bringas 2012; Lassi et al. 2014). Another aspect of the quality of healthcare that was recognized was the refusal of obstetric healthcare that women sometimes suffer in public facilities. These practices highlight the bad quality of care and the violation of the right to receive healthcare (Pérez-Castro y Vázquez et al. 2012). CoPs also recognized a persistent lack of drugs and other inputs, which specially hinders the adequate care of obstetric emergencies (Rouvier et al. 2011). Finally, different problems limit the proper follow-up of post-natal care, a period during which many obstetric complications might arise causing maternal deaths (Pérez-Castro y Vázquez et al. 2012).
The organization and delivery of maternal health services must be able to address unpredictable events and high-risk situations (DuPree et al. 2009; Institute of Medicine 2001). One tool to foster best practices, monitor and improve quality in direct clinical encounters is the World Health Organization Childbirth Checklist Programme (World Health Organization 2013). But there is also a need to interventions to improve quality at the health system level (Huntington et al. 2012). Strategies for improving the quality of maternal health care in LMICs, such as educational programs for women, capacity strengthening programs for health professionals, integration of services, use of clinical practice guidelines, provider incentives and other related to the support of local opinion leaders have been identified (Althabe et al. 2008).
Notwithstanding the important progress made during the past decades in public hospitals of Mexico and Nicaragua, both countries still face a long agenda to reach good quality standards in maternal healthcare programs, particularly in rural areas (Barber et al. 2007). The prioritization made by the CoPs is based on the experience of people directly responsible of the administration or the health care provided by maternal healthcare programs. And it is not a matter of mere coincidence that they recognize bad quality of public healthcare services. The results of their systematized tacit knowledge find substantial support in a large spectrum of scientific evidence and represent a feasible approach that can inform priority setting in the post MDG era (Nair et al. 2014).
Conclusions
The problems that were identified and prioritized based on the tacit knowledge of health system actors are supported by scientific literature. We therefore consider tacit knowledge is a feasible and potentially valuable approach to inform the post MDG agenda at the local level. Tacit knowledge, as it is initially externalized by the health personnel, can be considered as some kind of ‘raw’ material that has to be managed using scientifically sound methods. There is certainly not one single way to do this. Nevertheless, it is essential to assure its systematization. The experience presented here was essentially based on concept mapping combining face-to-face and virtual exchanges among participants. No doubt researchers and health workers can find other ways to make the best use of the latters’ tacit knowledge.
Improving the quality of care in maternal health programs becomes the sine qua non strategy to assure universal and effective coverage and stands in the first place to guide the post MDG agendas. Based on this new perspective, strategic planning should aim to work on building the necessary capacities of the health system and the health personnel in care provision and its management.
Acknowledgements
This article is based on the results of the project ‘Strengthening capacities to demand, access and apply implementation research to scale-up maternal health programs for underserved populations in Mexico and Nicaragua’, which is financed by the Alliance for Health Policy and Systems Research/World Health Organization (SPHQ14-APW-2064). Dr. Octavio Gómez-Dantés read the final draft and contributed important commentaries.
Conflict of interest statement. None declared.
References
- Althabe F, Bergel E, Cafferata ML. et al. 2008. Strategies for improving the quality of health care in maternal and child health in low- and middle-income countries: an overview of systematic reviews. Paediatric and Perinatal Epidemiology 22 (Suppl. 1): 42–60. [DOI] [PubMed] [Google Scholar]
- Ambrosini V, Bowman C. September 2001. Tacit Knowledge: some suggestions for operationalization. Journal of Management Studies 38: [Google Scholar]
- Barber SL, Bertozzi SM, Gertler PJ. 2007. Variations in prenatal care quality for the rural poor in Mexico. Health Affairs 26: w310–23. doi:10.1377/hlthaff.26.3.w310 [DOI] [PubMed] [Google Scholar]
- Bertone MP, Meessen B, Clarysse G. et al. 2013. Assessing communities of practice in health policy: a conceptual framework as a first step towards empirical research. Health Research Policy and Systems 11: 39 http://www.health-policy-systems.com/content/11/1/39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Best A, Clark P, Scott JL, Trochim W. 2007. Chapter 7. What we know In: Greater Than the Sum: Systems Thinking in Tobacco Control. Tobacco Control Monograph Series. Monograph Eighteen. National Cancer Institute. U.S. Department of health and Human Services. Bethesda, MD: National Institutes of Health; http://dccps.cancer.gov/TCRB/monographs/18/m18_complete.pdf [Google Scholar]
- Business Dictionary. 2014. Tacit knowledge definition. http://www.businessdictionary.com/definition/tacit-knowledge.html, accessed 8 December 2014.
- Collado-Peña S, Sánchez-Bringas Á. 2012. Referencia y contrarreferencia o multi-rechazo hospitalario? Un abordaje cualitativo. Revista CONAMED 17: S23–31. [Google Scholar]
- Concept Systems Global. 2014. Online platform. http://www.conceptsystemsglobal.com/, accessed 8 December 2014.
- DuPree E, O’Neill L, Anderson RM. 2009. Achieving a safety culture in obstetrics. Mount Sinai Journal of Medicine 76: 529–38. [DOI] [PubMed] [Google Scholar]
- González-Block MA, Mercado FJ, Ochoa H, Rivera H, Idrovo AJ. 2008. Utilización de la investigación por gestores de salud en México: diagnóstico de la capacidad y propuestas de fortalecimiento. Salud Pública de México/ 50. [PubMed] [Google Scholar]
- González-Block MA, Rouvier M, Becerril V, Sesia P. 2011. Mapping of health system functions to strengthen priority programs. The case of maternal health in Mexico. BMC Public Health 11: 164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huntington D, Banzon E, Dy Recidoro Z. 2012. A systems approach to improving maternal health in the Philippines. Bull World Health Organ 90: 104–10. doi:10.2471/BLT.11.092825 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh HF, Shannon SE. 2005. Three approaches to qualitative content analysis. Qualitative Health Research 15: 1277–88. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. 2001. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, D.C: National Academy Press. [PubMed] [Google Scholar]
- Kothari A, Bickford J, Edwards N, Dobbins MJ, Meyer M. 2011. Uncovering Tacit Knowledge: a pilot study to broaden the concept of knowledge in knowledge translation. BMC Health Services Research 11: 198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landry R, Amara N, Pablos-Mendes A, Shademani R, Gold I. 2006. The knowledge-value chain: a conceptual framework for knowledge translation in health. Bulletin of the World Health Organization 84: 597–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lassi Z, Das J, Salam R, Bhutta Z. 2014. Evidence from community level inputs to improve quality of care for maternal and newborn health: interventions and findings. Reproductive Health 11 Suppl: 2S2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McAdam R, Mason B, McCrory J. 2007. Exploring the dichotomies within the tacit knowledge literature: towards a process of tacit knowing in organizations. Journal of Knowledge and Management 11: 43–59. [Google Scholar]
- McIntosh B, Cookson G, Sandall J. 2012. A call to arms: the efficient use of the maternity workforce. British Journal of Midwifery 20: 122–7. [Google Scholar]
- Ministerio de Salud. 2008. Normativa 011 Normas y protocolos para la atención prenatal, parto, recién nacido/a y puerperio de bajo riesgo. Ministerio de Salud. Dirección General de Servicios de Salud. Nicaragua: http://apps.who.int/medicinedocs/documents/s18992es/s18992es.pdf [Google Scholar]
- Nair M, Yoshida S, Lambrechts T. et al. 2014. Facilitators and barriers to quality of care in maternal, newborn and child health: a global situational analysis through metareview. BMJ Open 4: e004749. doi:10.1136/bmjopen-2013-004749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nonaka I. 1994. A dynamic theory of organizational knowledge creation. Organization Science 5: 14–37. [Google Scholar]
- Panisset U, Pérez Koehlmoos T, Hamdi Alkhatib A. et al. 2012. Implementation research evidence uptake and use for policy-making. Health Research Policy and Systems 10: 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez-Castro y Vázquez JA, Castillo-Vázquez C, Domínguez-de la Peña M. et al. 2012. Análisis de 129 casos de mortalidad materna 2011 en la CONAMED. Revista CONAMED 17: S32–6. [Google Scholar]
- Peters D, Tran N, Adam T. 2013. Implementation Research in Health. A practical guide. Alliance for Health Policy and Systems Research. Geneva: World Health Organization. [Google Scholar]
- Polanyi M. 1966. The Tacit Dimension. Chicago: University of Chicago Press. [Google Scholar]
- Rouvier M, González-Block MA, Becerril-Montekio V. et al. 2011. Problem mapping by state and federal actors for maternal health attention. Salud Pública de México 53: 48–56. [DOI] [PubMed] [Google Scholar]
- Rouvier M, González-Block MA, Sesia P, Becerril-Montekio V. 2013. Problems of the health system in Mexican states with high incidence of maternal mortality. Salud Pública de México 55: 185–92. [DOI] [PubMed] [Google Scholar]
- Shiffman J. 2007. Generating political priority for maternal mortality reduction in 5 developing countries. American Journal of Public Health 97: 796–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stefanini A. 1999. Ethics in health care priority-setting: a north–south double standard? Tropical Medicine and International Health 4: 709–12. [DOI] [PubMed] [Google Scholar]
- Trochim WMK. 1989. An introduction to concept mapping for planning and evaluation. Evaluation and Program Planning 12: 1–16. [Google Scholar]
- United Nations. 2014. The Millennium Development Goals Report 2014. New York: United Nations; http://www.un.org/millenniumgoals/2014%20MDG%20report/MDG%202014%20English%20web.pdf [Google Scholar]
- Wenger E. 1998. Communities of practice: learning, meaning, and identity. Cambridge, UK: Cambridge University Press. [Google Scholar]
- World Health Organization. 2013. Safe Childbirth Checklist Programme. An overview. Geneva: World Health Organization. [Google Scholar]
- Yemile Ordaz-Martínez K, Rangel R, Hernández-Girón C. 2010. Factores de riesgo asociados con mortalidad materna en el estado de Morelos, México. Ginecologia y Obstetricia de Mexico 78: 357–64. [PubMed] [Google Scholar]