Abstract
Rates of exclusive breastfeeding are slowly increasing, but remain suboptimal globally despite the health and economic benefits. This study estimates the costs of not breastfeeding across seven countries in Southeast Asia and presents a cost-benefit analysis of a modeled comprehensive breastfeeding strategy in Viet Nam, based on a large programme. There have been very few such studies previously for low- and middle-income countries. The estimates used published data on disease prevalence and breastfeeding patterns for the seven countries, supplemented by information on healthcare costs from representative institutions. Modelling of costs of not breastfeeding used estimated effects obtained from systematic reviews and meta-analyses. Modelling of cost-benefit for Viet Nam used programme data on costs combined with effects from a large-scale cluster randomized breastfeeding promotion intervention with controls. This study found that over 12 400 preventable child and maternal deaths per year in the seven countries could be attributed to inadequate breastfeeding. The economic benefits associated with potential improvements in cognition alone, through higher IQ and earnings, total $1.6 billion annually. The loss exceeds 0.5% of Gross National Income in the country with the lowest exclusive breastfeeding rate (Thailand). The potential savings in health care treatment costs ($0.3 billion annually) from reducing the incidence of diarrhoea and pneumonia could help offset the cost of breastfeeding promotion. Based on the data available and authors’ assumptions, investing in a national breastfeeding promotion strategy in Viet Nam could result in preventing 200 child deaths per year and generate monetary benefits of US$2.39 for every US$1, or a 139% return on investment. These encouraging results suggest that there are feasible and affordable opportunities to accelerate progress towards achieving the Global Nutrition Target for exclusive breastfeeding by 2025.
Keywords: Breastfeeding, nutrition, maternal newborn, and child health, Southeast Asia, economic evaluation, costing, cost benefit analysis
Key Messages
Inadequate breastfeeding results in substantial human loss and monetary costs for families and governments in Southeast Asia.
Every year, over 12 400 child and maternal deaths can be attributed to inadequate breastfeeding in the seven Southeast Asian countries. Breastfeeding can prevent 50% of child deaths due to diarrhoea and pneumonia and 10% of deaths due to breast cancer.
Savings in health care treatment costs from reductions in pneumonia and diarrhoea from increased breastfeeding could help offset the additional cost of breastfeeding promotion.
The potential improvements in cognition alone, through higher IQ and earnings, could amount to as much as 0.5% of Gross National Income globally.
Based on findings from a programme implemented in 15 of 63 provinces and municipalities, a modeled breastfeeding promotion strategy at national scale in Viet Nam could yield a benefit-cost ratio of $2.39:1 or a return on investment of 139%.
Introduction
Despite the crucial benefits that breastfeeding provides, we have failed to create an environment whereby optimal breastfeeding is the social norm, and thus rates remain well below coverage targets set by the World Health Organization (Editorial 2014). Optimal breastfeeding for children includes early initiation of breastfeeding within 1 h of birth, exclusive breastfeeding up to 6 months, and continued breastfeeding to 2 years and beyond, accompanied with nutritionally adequate and safe complementary foods (UNICEF 2011). Moreover, breastfeeding is a child’s right. The United Nations Convention on Rights of the Child states that governments have the responsibility ‘to ensure that all segments of society, in particular parents and children, are informed, have access to education and are supported in the use of basic knowledge of child health and nutrition, the advantages of breastfeeding, hygiene and environmental sanitation and the prevention of accidents’ (United Nations 1989).
Between 1995 and 2010, the proportion of infants 0–5 months exclusively breastfed across low- and middle-income countries rose slightly from 33 to 39% overall. The greatest gains were achieved in Africa, while rates in Asia only rose by three percentage points to 41%. The gradual increase is positive, but the differences among countries, and within countries, are substantial. East Asia and the Pacific (excluding China) was the only UNICEF region that experienced a decline over the 15-year period—the exclusive breastfeeding rate decreased from 31 to 29% (Cai et al. 2012).
Breastfeeding rates, however, tend to decline as national income rises, although some countries have succeeded in reversing that trend (Victora et al. 2016). Breastfeeding to 6 months (even if not exclusive) confers important cognitive benefits. The cognitive losses associated with not being breastfed to 6 months are estimated globally as 0.49% of world Gross National Income (Rollins et al. 2016) National policy can make a difference: breastfeeding rates increased by 1% per year, or twice as fast as the global average, in countries with pro-breastfeeding social policies (Rollins et al. 2016).
In addition to a set of interventions to protect, promote, and support breastfeeding, the WHO and UNICEF global strategy for infant and young child feeding (IYCF) includes pro-breastfeeding policy initiatives that have gained traction globally in recent decades (WHO and UNICEF 2003). First, the International Code of Marketing of Breast-milk Substitutes (BMS) adopted in 1981 aims to protect against the consequences of unethical promotion of BMS by the baby food industry (UNICEF and WHO 1981). The Code and subsequent relevant World Health Assembly (WHA) resolutions prohibit the advertisement or promotion of these products to the general public or through the health care system. By 2015, only 43 of 192 countries have national regulations covering all of the provisions of the international Code, while a further 48 have national measures covering most of the provisions of the Code (UNICEF 2015). Code implementation is recommended by the Committee on the Rights of the Child and is part of nutrition relevant legislation under the Scaling Up Nutrition movement.
Second, the International Labour Office (ILO) Protection Convention 2000 number 183 entitles women to a minimum of 14 weeks of paid maternity leave, and recommends extending the paid leave to a minimum of 18 weeks (International Labour Office 2014). Maternity leave policies are widespread globally with only a few exceptions, but the level of entitlements, length of leave, and spousal benefit entitlement, and source of pay (social security or employer) vary by country. Employed mothers are entitled to one or two paid breastfeeding breaks per working day, although actual practice differs. Notably, maternity and parental leave policies do not cover women working in the informal sector or in family businesses, or those who are self-employed. Third, the Baby-friendly Hospital Initiative (BFHI) was launched by UNICEF and WHO in 1991 to encourage health facilities to institutionalize the WHO Ten Steps to Successful Breastfeeding (WHO and UNICEF 2009). Over 20 000 hospitals in 156 countries were certified as baby-friendly at some point since inception, although it is likely many no longer meet the criteria. Many countries are currently incorporating the WHO Ten Steps to Successful Breastfeeding requirements into their regular hospital standards and accreditation process, rather than a separate process in an effort to reduce cost and increase breastfeeding coverage. These policy actions can be complemented by breastfeeding counselling and support for individual mothers, and by social marketing campaigns that promote breastfeeding behaviours and help shift social norms.
Previous studies (Bertran et al. 2001; Bartick and Reinhold 2010; Bartick et al. 2013; Pokhrel et al. 2014) have shown that inadequate breastfeeding is associated with significant human and economic costs. We use the term inadequate here to describe limited breastfeeding according to various indicators, some of which correspond to less than ‘optimal’ breastfeeding as defined by WHO and UNICEF (UNICEF 2013). In the USA, it was estimated that 911 child lives and $13 billion could be saved if 90% of mothers could breastfeed exclusively for 6 months instead of the current rate of 12.3% (Bartick and Reinhold 2010). Breastfeeding for <2 years over a woman’s lifetime is estimated to result in 4981 maternal breast cancer deaths and US$17.4 billion in annual costs related to premature death (Bartick et al. 2013). Betran et al. (2001) estimated that exclusive breastfeeding to 3 months could prevent 52 000 deaths in Latin America. In the UK, Pohkrel et al. found that:
Supporting mothers who are exclusively breastfeeding at 1 week to continue breast feeding until 4 months can be expected to reduce the incidence of three childhood infectious diseases and save at least £11 million annually, and doubling the proportion of mothers currently breastfeeding for 7–18 months in their lifetime is likely to reduce the incidence of maternal breast cancer and save at least £31 million annually. (Pokhrel et al. 2014)
There were no estimates of the cost of not breastfeeding in Southeast Asia published. Given the expected large economic costs associated with inadequate breastfeeding however, a cost-benefit analysis is an appropriate method to use to analyse the priority of breastfeeding promotion among health and other government priorities. A cost-benefit approach values the benefits of a health programme in terms of monetary units (e.g. health cost savings, economic productivity benefits) in order to facilitate direct comparison with costs (Drummond et al. 2005). Cost-effectiveness analysis, on the other hand, is appropriate when the primary outcomes are expressed in health terms (e.g. reduced mortality, reduced time lived with disability or impaired health). The benefit-cost ratio (BCR) is used to measure the economic returns from each dollar invested in the intervention (Drummond et al. 2005). No evaluations were found on cost-benefit or cost-effectiveness analyses of breastfeeding promotion interventions for a low- or middle-income country since 2000 in the peer-reviewed literature in English (although Rajkumar et al. 2012 provide a cost-benefit analysis of breastfeeding promotion in Ethiopia, in a World Bank publication). Only one other country study was located since 1990 (Horton et al. 1996).
Our study, therefore, aims to fill a gap in the literature by estimating the cost of suboptimal breastfeeding in seven countries in the Southeast Asia region and the cost-benefit associated with a modeled comprehensive breastfeeding strategy at national-scale in one country, Viet Nam, using effectiveness results from a large-scale operational programme.
Context in Southeast Asia
Southeast Asia is a region of fast economic growth and, in countries such as Thailand, women’s labour market participation rates are amongst the highest in the world. Given the above-mentioned decline in breastfeeding rates in the region, this study concentrated on seven countries in Southeast Asia: one low-income country, Cambodia; five lower-middle-income countries, Indonesia, Laos, Myanmar, Timor-Leste and Viet Nam; and one upper-middle-income country, Thailand (World Bank 2015).
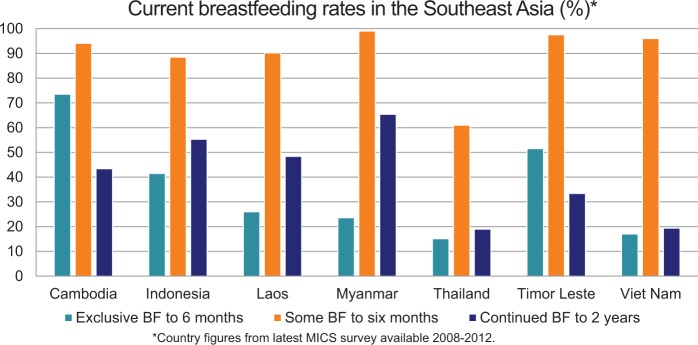
The rates of exclusive breastfeeding up to 6 months in this group of countries range from 15.1 to 17.0% in Thailand and Viet Nam, respectively up to 73.5% in Cambodia (Figure 1). Higher exclusive and any breastfeeding rates in this region are more common in smaller, lower income countries (General Statistical Office 2011; National Institute of Statistics et al. 2011; UNICEF 2011; National Statistical Office et al. 2013). Most infants in the region do; however, receive some breastmilk during the first 6 months. The percentages of infants receiving some breast-milk range between 88.5% in Indonesia and 97.5% in Timor-Leste, except for Thailand at 61% (Statistics Indonesia et al. 2013).
Figure 1.
Breastfeeding rates (%) in the seven study countries in the Southeast Asia region.
The baby food industry has increased marketing of BMS for children under 2 years of age, particularly in emerging economies, where potential markets have grown due to increases in disposable incomes and the large child populations (Rollins et al. 2016). Yet, only five out of the seven countries have legislated the Code of Marketing of BMS to some degree, either partially or fully. The lack of enforcement mechanisms and resources is a common gap that limits the effectiveness of the laws. Thailand and Timor-Leste have only drafted legislation but not yet fully enacted it into law (Table 1). Viet Nam and Myanmar have recently updated national codes to align with the latest WHA resolutions.
Table 1.
Summary of breastfeeding policy implementation at country-level
| Maternity leave |
WHO code on marketing of BMS |
BFHI |
||||
|---|---|---|---|---|---|---|
| Country | No. of weeks | Source of pay | Legislation status | Year | Implementation progress | |
| Cambodia | 13 | At 50% paid by employer | Partial: sub-decree No. 133 prohibits advertising of BMS without government approval; however not enforced | 2005 partial | 29% of hospitals were ever-certified as Baby-friendly; however follow-up has not been done | |
| Indonesia | 13 | At 100% paid by employer; 1.5 months prior to delivery, 1.5 months after | Partial: Government Regulation No. 69 on Food Labeling and Advertisement covers for >1 year; No. 33 on exclusive Breastfeeding only covers <6 months. Some district level monitoring and enforcement, no national system. | 1999; 2012 | 5% of hospitals and maternity facilities reported ever-certified Baby-friendly, but no certification process currently in place | |
| Laos | 13 | At 100% paid by social security | Partial: Agreement on Infant and Child Food Products Control released; but weak on enforcement | 2007 | <5% hospitals accredited up to 1999; Baby-friendly process accreditation process found to be burdensome. | |
| Myanmar | 14; 26 for civil service | At 70% paid by social security for 6 weeks prior to delivery plus for 8 weeks after delivery at 120%; | Full: National Code on Infant Food endorsed, but not currently enforced | 2014 | 76% of hospitals and maternity facilities reported as Baby-friendly. Health system in need of strengthening; BFHI principles should be institutionalized. | |
| Thailand | 13 | At 100% paid by employer for 45 days plus 45 days at 50% paid by social security | Voluntary: Code is in process of being drafted: activities, which would violate Code, are widespread | None | Approximately 20% of hospitals were accredited as Baby-friendly in most recent 3-year round. 78% reported ever-certified. | |
| Timor-Leste | 12 | At 67% paid by employer until social security fund created. | Voluntary: BMS Code is drafted. Inadequate mechanisms for enforcement. | None | 33% of hospitals were internally assessed and reported as Baby-friendly, but not formally accredited. | |
| Viet Nam | 26 | 100% paid by social security | Partial: Advertisement Law bans advertising for children <2 and complementary food for infants <6 months. Decree No. 100 regulates trading and using BMS for children <2. | 2012; 2014 | 9% of Baby-friendly hospitals ever-certified. BFHI 10 Steps are mandatory for all public and private hospitals since 2014. | |
Source: WHO and UNICEF (2009), WHO: Revised (2013), International Labour Office (2014), Labbok (2012).
The percentage of hospitals in the region ever-certified as Baby-Friendly ranged from an estimated 5% in Laos to 75% of hospitals and maternity facilities in Myanmar (WHO and UNICEF 2009; Labbok 2012). Myanmar did not undertake this programme. The duration of legislated maternity leave in this group of countries ranges between 12 and 14 weeks in duration. The exception is Viet Nam, which has recently implemented 6 months (26 weeks) of paid maternity leave (International Labour Office 2014). Less than 6 months of maternity leave creates significant barriers for working mothers to sustain exclusive breastfeeding until infants are 6 months of age. Indonesia and Myanmar both require that 6 weeks of maternity leave be taken before delivery, thereby limiting further support for breastfeeding. Maternity leave is funded entirely by social security in Viet Nam and Laos, as recommended by ILO, in contrast to the partial or sole funding required by employers in other countries.
Most of the countries have not implemented a national comprehensive strategy to support and promote breastfeeding—Viet Nam is an exception. Between 2010 and 2014, the Alive & Thrive breastfeeding promotion programme was implemented in 15 of 63 provinces and municipalities (Nguyen et al. 2014). The programme required US$1.2m in start-up costs and US$4.64m in recurrent costs for 1-year of implementation, policy development, monitoring, mass media campaigns and social franchising of IYCF counselling. The programme covered 599 013 women between January 2012 and September 2014 through social franchising of IYCF counselling from the third trimester of pregnancy until children reached 2 years of age. The mean number of visits in the last 6 months was 1.7 and 1.3 for mothers with children under 6 and 6–23 months, respectively. The breastfeeding-counselling package was estimated to cost ∼US$1.5 per visit. It was envisaged that up to 15 counselling sessions per mother and child pairing would be required per birth, but actual usage was ∼5.8 visits per mother from birth of child until 2 years of age (Alive & Thrive 2013).
At the same time the government scaled extension of maternity leave from 4 to 6 months across the whole country. In early 2013, the new Advertisement Law banning the marketing of BMS for young children <2 years of age and complementary foods for infants <6 months came into effect. In the same year, Viet Nam institutionalized the WHO 10 Steps for Successful Breastfeeding into the overall standards and accreditation systems for all public and private hospitals with costs covered by health system and hospital budgets.
The control and intervention areas had baseline rates of exclusive breastfeeding similar to the national average of 17.0% (General Statistics Office 2011). The breastfeeding initiatives’ evaluation suggests that the targeted breastfeeding strategy and underlying trends raised the rate of exclusive breastfeeding in infants 0–5 months from 18.9 to 57.8% from baseline to end line in the intervention sites as compared a change from 17.8 to 28.9% in the control sites. This suggests a difference-in-difference estimated change of 28.3% over the 5-year period (Rawat et al. 2015). Although exclusive breastfeeding rates improved, there was no change in the rate of continued breastfeeding to 2 years. For further details of the evaluation design (a randomized, geographically clustered, difference-in-difference methodology, comparing 20 intervention communes to 20 similar controls, in 4 provinces) see Menon et al. (2013).
Methods
This study analysed both the costs of not breastfeeding in seven countries in Southeast Asia and the cost-benefit of a modeled national breastfeeding promotion strategy in Viet Nam.
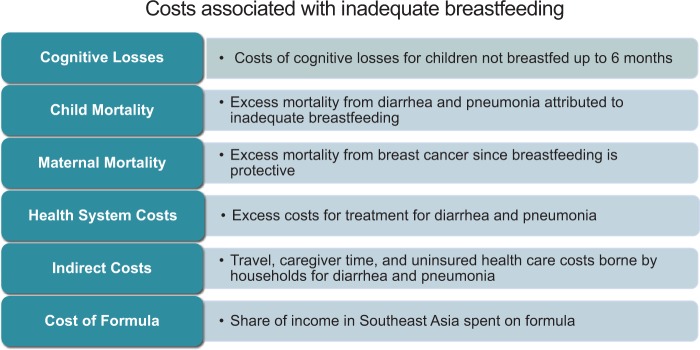
Costs of not breastfeeding
We estimate six components of the costs of inadequate breastfeeding (see Figure 2) relative to counterfactual scenarios of optimal breastfeeding. The human costs of inadequate breastfeeding include premature mortality both for children under the age of 2 as well as mothers. Economic costs include reduced cognition, health system treatment costs for selected illnesses in children under the age of 2 (diarrhoea and pneumonia), and the costs of BMS. In addition, we estimate indirect costs borne by families seeking treatment for their child’s illness in one country, Indonesia that could have been averted by optimal breastfeeding.
Figure 2.
Components of framework for costing analysis of not breastfeeding.
The costs are relative to the counterfactual scenario where 100% of children receive some breastmilk up to the age of 6 months (cognition costs). 100% of children are exclusively breastfed to age 6 months and then continue to receive some breastmilk to age 2 years (child mortality and health treatment costs), and 90% of women breastfeed cumulatively for 2 years over their lifetime (maternal mortality). This counterfactual is consistent with WHO breastfeeding recommendations (allowing for the fact that not all women have children), but we note that the highest national rate for exclusive breastfeeding to 6 months 2008–12 was only 85% (UNICEF 2015).
The costing analyses included cost components from the government and societal viewpoints, which measures cost to health system, households and society, for a 1-year timeframe, but is not exhaustive in capturing all possible social costs. Breastfeeding rates and disease prevalence and incidence data were calculated from the latest Demographic Health Survey (DHS) and Multiple-Indicator Cluster Surveys (MICS) for Indonesia (Statistics Indonesia et al. 2013), Myanmar (Ministry of National Planning and Economic Development and Ministry of Health Myanmar 2011), Thailand (National Statistical Office et al. 2013) and Viet Nam (General Statistical Office 2011). Population data for children’s age groups were retrieved from UNICEF statistics (UNICEF 2015).
The estimation of cognitive losses attributed to inadequate breastfeeding assumes that some breastfeeding up to 6 months of age is associated with an increase in IQ of 2.6 points (0.17 SDs) as compared with no breastfeeding (Victora et al. 2015). This rate is based on the nine studies, which controlled for maternal IQ, from a systematic review, which identified 16 studies, of which 14 were from high-income countries. A one SD increase in IQ is in turn associated with an increase in labour earnings of 16% in low- and middle-income countries (Hanushek and Woessmann 2008) and labour earnings constitute half of national income on average.
Inadequate breastfeeding is one of the largest contributors to the global burden of childhood disease due to the higher relative risk of frequency of infection and mortality from diarrhoea and pneumonia (Lopez and Murray 1998; Das et al. 2014). Exclusive breastfeeding to 6 months substantially reduces the risk of mortality from diarrhoea and respiratory disease, compared with predominant, partial and no breastfeeding, and continued breastfeeding to 2 years of age reduces the risk compared with no breastfeeding. In order to estimate the projected child mortality attributable to inadequate breastfeeding behaviours, published relative risks by either the diarrhoea or pneumonia infection pathway (Black et al. 2008) were multiplied by the percentage of households in each breastfeeding behaviour category (from DHS and MICS), and then multiplied by the total mortality for each disease for the corresponding age group from WHO Global Health Observatory data (World Health Organization 2013). This method was applied for each of the neonatal, under 6 months, and 6–23 months’ age groups separately.
The health system costs for the treatment of cases of diarrhoea and pneumonia in children under the age of 2 attributed to inadequate breastfeeding were calculated using a similar methodology as for mortality. The incidence of illness calculated was multiplied by percentages for health-seeking behaviour by type of facility (from DHS and MICS data) to determine the number of annual cases treated in each type of facility. Since data on health seeking behaviour for the treatment of diarrhoea were not available for Myanmar, Thailand and Viet Nam, regional averages or the best proxy available in published literature were used for those countries (Lamberti et al. 2012; Aung et al. 2013). The estimate of the number of cases treated in each type of facility was then multiplied by treatment unit costs estimates.
The economic cost analysis used unit costs data collected between 2013 and 2015 since centralized national data sources on costs were not available in these countries. Unit cost data for inpatient and outpatient treatment for children with diarrhoea and pneumonia in both under 6 months and 6–23 month age groups were collected through consultations with government agencies, health facilities and non-governmental organization sources. Specific unit costs were from Pracharak Referral Hospital and Pak Kret Community Hospital in Thailand; Yangon Children’s Hospital, a rural health centre and Population Service International clinics in Myanmar; and Da Nang Hospital in Viet Nam. For Indonesia, the authors (AS and PP) conducted an in-depth survey of health facilities including one health post, one primary health centre, one public hospital and one private hospital, and used DHS data to weight the costs in order to generate an average for inpatient and outpatient costs weighted by usage pattern. All costs for these four countries were reported in 2015 US dollars. Similar data were drawn from previous studies on the cost of malnutrition in Cambodia (Council for Agriculture and Rural Development et al. 2013) Laos PDR (Bagriansky and Voladet 2013) and Timor-Leste (Bagriansky 2014).
Breastfeeding also has protective benefits for mothers—it reduces the maternal risk of breast cancer (Victora et al. 2016). The method used for estimating the mortality of breast cancer attributed with no breastfeeding follows the approach of Pokhrel et al. (2014) in the UK, which is based on the fact that lifetime duration of breastfeeding reduces the relative risk of morbidity from breast cancer and assumes that the effect on mortality is the same magnitude. Pokhrel et al. (2014) use an effect size based on a large collaborative reanalysis from 47 studies in 30 countries. Data on breast cancer mortality by country come from GLOBOCAN 2012 data (International Agency for Research on Cancer 2012).
The costs of BMS purchased by families of children aged under the age of 2 months is estimated as a proportion of household income and as a proportion of GDP per capita. Data on the cost of economy brands of infant formula were collected from local markets in Indonesia, Myanmar, Thailand and Viet Nam and paired with aggregate market size information from a Euromonitor study commissioned by the WHO (Rollins et al. 2016). Data on national GDP were retrieved from the World Bank Open Data (World Bank 2014) and data on earnings was obtained from the International Labour Office statistics (ILO 2015).
Last, the authors (A.S. and P.P.) conducted a survey of patient families, in Indonesia only, in order to estimate indirect costs. A total of 200 accompanying family members of children-seeking care for diarrhoea or pneumonia, 50 from each of four different types of health facilities, were surveyed about the amount of indirect costs incurred for transportation costs, travel time, uninsured medical costs and caregiver time.
Cost-benefit analysis for Viet Nam
Having analysed costs, a cost-benefit analysis was undertaken for one country, Viet Nam, comparing the estimates of benefits of improved breastfeeding with the costs of the implementation of a modeled comprehensive breastfeeding promotion strategy at national-scale. This was undertaken using a prevalence-based methodology that compared the recurrent costs of a programme to promote breastfeeding with the annual losses, which could potentially be averted by the intervention. A limitation of prevalence-based studies is that they assume a steady state, which applies to breastfeeding rates in this study. This approach, however, is simpler to implement than incidence-based methods, which have their own limitations such as strong assumptions regarding the rate of growth of wages several decades in the future and the social rate of discount.
The monetary benefits included the estimated cognitive losses averted and reduced health system treatment costs. Although we also acknowledge the human benefits related to averted child and maternal deaths attributed to increased breastfeeding, we do not take the step of attributing an economic value to the loss of life because this method is somewhat controversial [see e.g. Zweifel et al. (2009)]. Neither do we include cost savings from reducing BMS purchases, which would be partially offset by increased maternal food consumption. In addition, indirect costs borne by families are not included in this analysis since we do not have these data for Viet Nam.
The costs of a comprehensive, national breastfeeding programme were extrapolated from the Alive & Thrive initiative’s 5-year programme implemented in 15 of 63 provinces and municipalities in Viet Nam (Alive & Thrive 2013). The programme model included monitoring and policy development, mass communications and interpersonal counselling of women on IYCF. The calculation of the recurrent costs of breastfeeding promotion rely on programme cost estimates. These do not necessarily capture all social costs, e.g. if market prices do not reflect opportunity costs of all resources. The evaluation of this programme estimated its effect on increasing exclusive breastfeeding rates and other indicators compared with control provinces (Nguyen et al. 2014).
We assumed that the costs of programme implementation in the 15 provinces could be extrapolated to the national scale (63 provinces), and that maintaining the programme would also generate the same effectiveness in increasing both partial and exclusive breastfeeding rates to 6 months. We also included the cost estimates of extending maternity leave from 4 to 6 months, event though this occurred in all provinces across the country (Viet Nam Social Insurance 2012). We assumed no change in continued breastfeeding rates to 2 years, since this was not observed in the 15-province intervention.
Results
Costs of not breastfeeding
We present the results for the estimates of the six cost components here, in the same sequence as in Figure 2. The key driver for the cost of ‘cognitive’ losses is the percentage of babies under 6 months that are neither partially nor exclusively breastfed. As a result, the cost of lower cognitive scores ranged from 0.03% of GNI in Timor-Leste where 97.5% of infants under 6 months of age receive some breastmilk to 0.54% of GNI in Thailand where only 61% of infants do so (see Table 2). The combined total of estimated losses due to lower cognition is ∼US$1.63 billion per year across the seven countries. The majority of losses occurred in the more populous countries but most of all US$1.34 billion for Indonesia (Table 2).
Table 2.
Summary annual cognitive and health system costs of inadequate breastfeeding
| Country | Cognitive losses (US$m) | Cognitive loss (% GNI) | Health expenditure costs (US$m) | Average cost per episode per child treated for diarrhoea (US$) | Average cost episode treated for pneumonia (US$) |
|---|---|---|---|---|---|
| Cambodia | 10.70 | 0.08 | 1.86 | 9.40 | 5.30 |
| Indonesia | 1343.70 | 0.16 | 256.42 | 22.50 | 19.70 |
| Laos | 11.40 | 0.14 | 0.55 | 15.00 | 19.20 |
| Myanmar | n/a | 0 | 3.38 | 4.80 | 3.30 |
| Thailand | 192.60 | 0.54 | 7.65 | 15.30 | 17.50 |
| Timor-Leste | 1.40 | 0.03 | 0.33 | 16.00 | 15.60 |
| Viet Nam | 70.40 | 0.06 | 23.36 | 13.10 | 13.20 |
| Total | 1630.20 | 293.55 |
In terms of ‘infant and child mortality’, there were an estimated 10 718 annual deaths of children under the age of 2 from diarrhoea and acute respiratory infection (ARI), a proxy for pneumonia, attributable to inadequate breastfeeding in the seven countries in the study (Table 4). ARI accounts for ∼70% of child deaths attributed to inadequate breastfeeding (n = 7529) and 52% of deaths in children under the age of 2 are in the first 6 months (n = 5570). Indonesia alone accounted for nearly half of the region’s attributable deaths (n = 5377) followed by countries with relatively high mortality rates such as Viet Nam (n = 2011) and Myanmar (n = 1636). Cambodia, Laos and Timor-Leste also had high mortality rates, but a low absolute burden due to smaller population sizes.
Table 4.
Summary of child mortality attributed to inadequate breastfeeding by country, disease and age group
| Cambodia |
Indonesia |
Laos |
Myanmar |
Thailand |
Timor-Leste |
Vietnam |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Diarrhoea | ARI | Diarrhoea | ARI | Diarrhoea | ARI | Diarrhoea | ARI | Diarrhoea | ARI | Diarrhoea | ARI | Diarrhoea | ARI | |
| <1 m | 6 | 71 | 52 | 1083 | 25 | 178 | 27 | 336 | 0 | 90 | 2 | 14 | 0 | 666 |
| 1–5 m | 51 | 88 | 480 | 1211 | 73 | 95 | 205 | 288 | 19 | 42 | 10 | 22 | 274 | 162 |
| 6–23 m | 113 | 199 | 747 | 1804 | 179 | 244 | 298 | 482 | 36 | 75 | 18 | 44 | 574 | 335 |
| Subtotal | 170 | 358 | 1279 | 4098 | 277 | 517 | 530 | 1106 | 55 | 207 | 30 | 80 | 848 | 1163 |
| Country total | 528 | 5377 | 794 | 1636 | 262 | 110 | 2011 | |||||||
| Regional total | 10 718 | |||||||||||||
The ‘maternal mortality’ losses are due to breast cancer, which kills ∼33 164 women annually in the seven countries in this study. It is estimated that current breastfeeding rates help prevent 1749 deaths per year from breast cancer, and there is potential to avert another 1706 annual deaths if 90% of mothers breastfeed for 2 years (Table 3). Countries with low breastfeeding rates—specifically Thailand (n = 406) and Viet Nam (n = 371)—had a disproportionately high mortality from the disease.
Table 3.
Summary of annual breastfeeding rates and maternal mortality attributed to inadequate breastfeeding by country
| Country | EBF 0-5 months (%)a | Continued BF to 2 years (%)b | Number of maternal deaths averted by current BF rates | Additional maternal deaths avertible if 90% of women BF for 2 years |
|---|---|---|---|---|
| Cambodia | 73.5 | 50.40 | 29 | 31 |
| Indonesia | 41.50 | 55.30 | 1279 | 803 |
| Laos | 40.4 | 40.00 | 12 | 11 |
| Myanmar | 24.09 | 62.28 | 216 | 81 |
| Thailand | 15.11 | 18.18 | 109 | 406 |
| Timor-Leste | 51.5 | 63.70 | 2 | 3 |
| Viet Nam | 24.03 | 21.80 | 102 | 371 |
| TOTAL | 1749 | 1706 |
aLatest DHS and MICS survey in each country.
The key drivers for ‘health treatment costs’ for the treatment of children under the age of 2 with diarrhoea or pneumonia attributed to inadequate breastfeeding are the disease prevalence, the proportion of children that seek care in health facilities, and the health facility treatment fees. Costing data collected from several countries produced rough estimates for average unit costs of inpatient and outpatient treatment of diarrhoea and pneumonia. Unit costs for treatment vary by level of care, between countries and between public and private facilities. The average costs per child treated in Myanmar (US$4.8 for diarrhoea and US$3.3 for pneumonia) and Cambodia (US$9.4 for diarrhoea and US$5.3 for pneumonia) were noticeably lower than in the other five countries, which were mostly in the US$13–15 range for diarrhoea and US$14–19 range for pneumonia. Indonesia had the highest costs per child at US$22.5 for diarrhoea and US$19.7 for pneumonia in part due to higher costs in the private healthcare system. Predictably, due to the population size, Indonesia had the highest absolute health system treatment cost (Table 2). The overall health system costs attributed to inadequate breastfeeding in the seven countries was US$293.5 million.
In addition to the health system costs, families incur ‘indirect health costs’ associated with seeking treatment for children with diarrhoea and pneumonia. For 88 024 children in Timor Leste, Bagriansky (2014) estimated a total annual cost of US$357 251 for travel time to health facilities and child care for families. From a survey of 200 mothers in Bandung City, West Java, Indonesia, the authors’ survey (A.S. and P.P.) estimated the average indirect costs borne by families with children seeking treatment per episode treated—some children may be treated more than once in a year. Estimates ranged from US$0.81 for diarrhoea, US$2.02 for ARI and US$2.71 for children suffering from both at a health post. The indirect cost was twice as high for treatment at primary health centres, which are generally further away, ten times as high at public hospitals and thirty times as high at private hospitals. Indirect costs added another 25% to the treatment costs, which is consistent with similar estimates for Timor Leste (Bagriansky 2014).
The ‘cost of formula’ for infants is significant for average working families in low- and middle-income countries, and unaffordable for households in the lowest wealth quintiles. The surveyed unit cost per 400 g can of an economy brand of infant formula from markets in the seven study countries ranges from US$2.53 in Indonesia to US$13.22 for the equivalent size in Myanmar. Based on 54 cans (400 g) of formula being consumed if infants up to 6 months exclusively received formula (ENN et al. 2004), the cost of consumption of infant formula (no breastfeeding) represents an estimated 13.8% of mean nominal monthly earnings of employees in Indonesia, 20.5% in Thailand and 47% in Viet Nam.
Countries with rapidly growing economies have the highest sales of infant and child formula in this region—a reflection of families having increases in disposable incomes. A study by Euromonitor (Rollins et al. 2016), reported that the value of milk annual formula sales nationally for children under the age of 3 was estimated at US$2400m in Indonesia, US$800m in Thailand and US$1,100m in Viet Nam in 2014. For Myanmar, the authors estimated the total value of sales of infant formula for children under the age of 2 to be ∼US$182 million per year. These national costs of formula represent the equivalent of between 0.22% GNI in Thailand to 0.7% GNI in Viet Nam. Although we present these data, we note that the entire cost of BMS is not saved by breastfeeding since mothers need to consume additional food to account for the additional caloric requirements. Exclusively breastfeeding mothers should increase their intake by ∼500 kcal per day in the first 6 months (FAO 2001).
Cost-benefit analysis for Viet Nam
We estimate that the cost of the national strategy extrapolated from annual recurrent costs of the Alive & Thrive programme plus the costs to Social Security of improved maternity leave benefits would be US$30.13 million per year (see Table 5). The primary monetary benefits in the form of health systems savings due to reduced treatment of child illnesses and cognitive losses averted totaled US$72.14 million. Overall, this scenario would generate human benefits of 200 child deaths averted and a BCR of $2.39 for every $1 invested, or a 139% return on investment. Since no improvement in continued breastfeeding to 2 years occurred, there were no benefits in terms of reduced maternal mortality from breast cancer.
Table 5.
Summary of cost-benefit analysis of a modeled national breastfeeding strategy in Viet Nam
| Intervention costs | Annual recurrent cost (US$m) |
|---|---|
| Policy and M&E | 0.60 |
| Furniture | 2.54 |
| Mass communications | 2.40 |
| IYCF counselling for all mothers of children 0–23 months | 12.09 |
| Extension of maternity leave from 4 to 6 months | 12.50 |
| Total | 30.13 |
| Benefits | Annual monetary benefit (US$m) |
| Cognitive losses averted | 70.40 |
| Health system treatment savings | 1.74 |
| Total | 72.14 |
| BCR | =72.14/30.13 =2.39 |
| Return on investment | 139% |
| Child deaths averted | 200 |
Discussion
Our study finds that the costs of inadequate breastfeeding in a group of low- and middle-income countries are substantial but differ from estimates in the US and UK (Bartick and Reinhold, 2010; Bartick et al. 2013; Pokhrel et al. 2014). Differences are likely due to disparities in breast cancer and childhood disease prevalence and factors related to wealth between settings. We included cognitive losses in the analysis for Southeast Asia, whereas others have not.
The estimated cost of a national-scale breastfeeding strategy cost of US$30.13 million in Viet Nam is much lower than the recent estimates by the World Breastfeeding Costing initiative (WBCi), a global costing analysis. The WBCi included costs for policy development, monitoring, legislating and implementing the international code, training of health workers, for media promotion, community outreach and mother support, implementation of BFHI and maternity entitlement for women below the poverty line. The WBCi estimates of US$121.1 million for a comprehensive strategy in Viet Nam, or US$52.9 million without the maternity stipends for women below the poverty line, may be overestimated (Holla-Bhar et al. 2015). BFHI accreditation and maternity stipends for low-income women might increase breastfeeding rates still further, but were not included in our studies’ cost-benefit analysis because these interventions were not part of Alive & Thrive’s programme in Viet Nam.
The BCR we identify is lower than those estimated elsewhere for reducing stunting and for micronutrient interventions. Hoddinott et al. (2013) showed that the BCR for the reduction of stunting prevalence ranged from US$4 to US$53 per dollar invested across 18 countries. For micronutrient interventions, the BCR similarly ranged from US$8 to US$46 (surveyed in Horton and Levin Forthcoming 2016). Interventions involving behaviour change may have somewhat lower BCR than those for interventions involving a commodity such as vaccines or micronutrient supplementation or fortification. The BCR we obtain is also lower than that estimated for breastfeeding promotion in Ethiopia (Rajkumar et al. 2012) in part this is because the Ethiopian study includes a monetary value for lives saved, which we do not. Our estimate may also be conservative since we included the costs of extending maternity leave to 6 months, which took place across the country, and we did not include potential benefits from potential reduced household spending on infant formula or indirect costs.
Overall, our findings on the BCR of breastfeeding promotion in Viet Nam likely still support the Copenhagen Consensus conclusion that the SDGs focused on reducing malnutrition reducing newborn mortality were among the best value for money goals (Kydland et al. 2014). The encouraging results from a comprehensive breastfeeding strategy in Viet Nam suggest that there are feasible and affordable opportunities to accelerate progress towards achieving the Sustainable Development Goal indicator and the World Health Assembly’s Global Nutrition Target on exclusive breastfeeding by 2025.
Our estimates have some limitations. They should be updated with new DHS and MICS datasets to be released for Viet Nam and Myanmar. We have used effect sizes (on IQ, wages, child mortality and morbidity and maternal mortality) derived from systematic reviews and meta-analyses from a range of countries not just in Southeast Asia. Cost estimates could be strengthened with more comprehensive surveys of health care costs at various levels of care. Notably, none of the countries had the capacity to provide national data on health care treatment costs. We have relied on programme costs as measured by the government, and not attempted to estimate the full social cost of the intervention. We have not attempted to monetize the value of child lives lost, and we were not able to obtain data on indirect costs of health care treatment for Viet Nam. We also did not undertake a sensitivity analysis: our estimates are particularly sensitive to the effectiveness of the breastfeeding promotion intervention.
Conclusion
The health and economic consequences of inadequate breastfeeding are substantial, not only for children and their families but also for governments and the economy. This study found that up to 50% of child deaths from diarrhoea and pneumonia and 10% of breast cancer deaths are due to inadequate breastfeeding—over 12 400 preventable child and maternal deaths annually in seven countries in the Southeast Asia region. The savings in health care treatment costs from pneumonia and diarrhoea can help offset the additional cost of breastfeeding promotion strategies. Increased breastfeeding will reduce household indirect costs for treatment of childhood diseases. It should be noted that improvements in cognition alone, through higher IQ and earnings, potentially amount to as much as 0.5% of Gross National Income in countries with the lowest breastfeeding rates below 6 months.
Based on the data available and educated assumptions, this study estimated, conservatively, that investing in a national breastfeeding promotion strategy in Viet Nam could result in saving over 200 child lives annually and generate monetary benefits of US$2.39 for every US$1, or a 139% return on investment. The effect of the strategy may vary from country to country based on determinants of breastfeeding and other factors including prevalence and mortality rate of childhood illnesses, strength of health system, level of BMS industry penetration and the nutrition policy context. Countries with lower rates of exclusive breastfeeding are likely to have a greater BCR. The Alive & Thrive programme success in Viet Nam suggests that interventions need to occur at all levels—national policy, mass communications, in the workplace and in one-on-one counselling of mothers in the community and health facilities.
Acknowledgements
The authors would like to acknowledge FHI 360 and UNICEF as well as the individuals within the governments of Myanmar, Thailand and Indonesia and INGOs for their support in helping to collect data and in understanding the policy context for the study. We are grateful to Jack Bagriansky for sharing methodologies from previous studies in the region. This study also benefited from data made available by the DHS Programme for Indonesia and UNICEF MICS for Myanmar, Thailand and Viet Nam.
Funding
This research was conducted by Alive & Thrive, an initiative funded by the Bill & Melinda Gates Foundation and by the governments of Canada and Ireland.
Conflict of interest statement. None declared.
References
- Alive & Thrive. 2013. Viet Nam Costing Study: Implementation Expenditure and Costs. Hanoi: Alive & Thrive. [Google Scholar]
- Aung T, McFarland W, Khin HS, Montagu D. 2013. Incidence of pediatric diarrhea and public-private preferences for treatment in rural Myanmar: a randomized cluster survey. Journal of Tropical Pediatrics 59: 10–6. [DOI] [PubMed] [Google Scholar]
- Bagriansky J. 2014. The Economic Consequences of Malnutrition in Timor-Leste. Dili, Timor-Leste: UNICEF. [Google Scholar]
- Bagriansky J., Voladet 2013. The Economic Consequences of Malnutrition in Lao PDR: A Damage Assessment Report. Vientiane, Lao PDR: UNICEF; http://www.smeru.or.id/report/other/cpsp/Paper,%20Abstact,%20CV/0201_saykham%20voladet%20-%20paper.pdf. [Google Scholar]
- Bartick M, Reinhold A. 2010. The burden of suboptimal breastfeeding in the United States: a pediatric cost analysis. Pediatrics 125: 1048–56. [DOI] [PubMed] [Google Scholar]
- Bartick MC, Stuebe AM, Schwarz EB. et al. 2013. Cost analysis of maternal disease associated with suboptimal breastfeeding. Obstetrics and Gynecology 122: 111–9. [DOI] [PubMed] [Google Scholar]
- Betran AP, De Onis M, Lauer JA. et al. 2001. Ecological study of effect of breastfeeding on infant mortality in Latin America. BMJ (Clinical research ed.), 323: 303–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Black R, Allen L, Bhutta Z. et al. 2008. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet 371: 243–60. [DOI] [PubMed] [Google Scholar]
- Cai X, Wardlaw T, Brown DW. 2012. Global trends in exclusive breastfeeding. International Breastfeeding Journal 7: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Council for Agriculture and Rural Development, UNICEF & World Food Programme. 2013. The Economic Consequences of Malnutrition in Cambodia: A Damage Assessment Report. Phnom Penh, Cambodia: http://www.wfp.org/sites/default/files/Report%20on%20Economic%20Consequences%20of%20Malnutrition%20in%20Cambodia.pdf.
- Drummond MF, Sculpher MJ, Torrance GW, O’Brien BJ, Stoddart GL. 2005. Methods for the Economic Evaluation of Health Care Programme. 3rd edn Oxford: Oxford University Press. [Google Scholar]
- Das JK, Salam RA, Bhutta ZA. 2014. Global burden of childhood diarrhea and interventions. Current Opinion in Infectious Diseases 27: 451–8. [DOI] [PubMed] [Google Scholar]
- Editorial. 2014. Indonesia’s breastfeeding challenge is echoed the world over. Bulletin of the World Health Organization 92: 234–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ENN, IBFAN, Terre des hommes et al. 2004. Infant Feeding in Emergencies. http://www.unhcr.org/45f6cc4e2.pdf.
- FAO. 2001. Energy Requirements of Lactation. ftp://ftp.fao.org/docrep/fao/007/y5686e/y5686e00.pdf, accessed 15 July 2015.
- General Statistical Office. 2011. Viet Nam Multiple Indicator Cluster Survey 2011, Final Report. Hanoi, Viet Nam. http://www.childinfo.org/files/MICS4_Vietnam_FinalReport_2011_Eng.pdf.
- Hanushek E, Woessmann L. 2008. The role of cognitive skills in economic development. Journal of Economic Literature 46: 607–68. [Google Scholar]
- Hoddinott J, Alderman H, Behrman JR, Haddad L, Horton S. 2013. The economic rationale for investing in stunting reduction. Maternal and Child Nutrition 9: 69–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holla-Bhar R, Iellamo A, Gupta A, Smith JP, Dadhich JP. 2015. Investing in breastfeeding - the world breastfeeding costing initiative. International Breastfeeding Journal 10: 8–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horton S, Levin C. Forthcoming, 2016. Cost-effectiveness of interventions for reproductive, maternal, newborn and child health. In Black R, Laxminarayan R, Temmerman M, Walker N. Disease Control Priorities (3rd edition): Volume 2, Reproductive, Maternal, Newborn and Child Health. Washington DC: World Bank.
- ILO. 2015. ILOSTAT Database. http://www.ilo.org/ilostat/faces/home/statisticaldata?_afrLoop=39430847112133#%40%3F_afrLoop%3D39430847112133%26_adf.ctrl-state%3Dbakdhzsnf_4, accessed 2 May 2015.
- International Agency for Research on Cancer. 2012. Estimated cancer incidence, prevalence and mortality worldwide in 2012. http://globocan.iarc.fr/Pages/online.aspx, accessed June 2015.
- International Labour Office 2014. Maternity and paternity at work: law and practice across the world. Geneva: http://www.ilo.org/wcmsp5/groups/public/—dgreports/—dcomm/—publ/documents/publication/wcms_242615.pdf.
- Kydland F, Sotkey N, Schelling T. 2014. Smart development goals. http://www.copenhagenconsensus.com//sites/default/files/outcomedocument_bw.pdf, accessed 2 May 2015.
- Labbok MH. 2012. Global baby-friendly hospital initiative monitoring data: update and discussion. Breastfeeding Medicine 7: 210–22. [DOI] [PubMed] [Google Scholar]
- Lamberti L, Fischer Walker C, Black R. 2012. Systematic review of diarrhea duration and severity in children and adults in low- and middle-income countries. BMC Public Health 12: 276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez AD, Murray CJL. 1998. The global burden of disease, 1990-2020. Nature Medicine 4: 1241.. [DOI] [PubMed] [Google Scholar]
- Menon P, Rawat R, Ruel M. 2013. Bringing rigor to evaluations of large-scale programs to improve infant and young child feeding and nutrition: the evaluation designs for the Alive & Thrive initiative. Food and Nutrition Bulletin 34(3 Suppl), S195–211. [DOI] [PubMed] [Google Scholar]
- Ministry of National Planning and Economic Development and Ministry of Health Myanmar. 2011. Myanmar Multiple Indicator Cluster Survey 2009 - 2010 Final Report. Nay Pyi Taw, Myanmar. Ministry of National Planning and Economic Development and Ministry of Health, Myanmar.
- National Institute of Statistics, Directorate General for Health & ICF Macro. 2011. Cambodia Demographic and Health Survey 2010 Phnom Penh, Cambodia and Calverton, Maryland, USA: National Institute of Statistics, Directorate General for Health, and ICF Macro. http://dhsprogram.com/pubs/pdf/FR249/FR249.pdf.
- National Statistical Office, United Nations Children’s Fund, Ministry of Public Health et al. 2013. Thailand Multiple Indicator Cluster Survey 2012. Bangkok, Thailand: National Statistical Office. http://www.unicef.org/thailand/57-05-011-MICS_EN.pdf.
- Nguyen PH, Kim SS, Keithly SC. et al. 2014. Incorporating elements of social franchising in government health services improves the quality of infant and young child feeding counselling services at commune health centres in Vietnam. Health Policy and Planning 29: 1008–20. [DOI] [PubMed] [Google Scholar]
- Pokhrel S, Quigley MA, Fox-Rushby J. et al. 2014. Potential economic impacts from improving breastfeeding rates in the UK. Archives of Disease in Childhood 0: 1–7. [DOI] [PubMed] [Google Scholar]
- Rajkumar A, Gaukler C, Tilahun J. 2012. Combating Malnutrition in Ethiopia: An Evidence-Based Approach for Sustained Results. Africa Human Development Series. World Bank: World Bank. [Google Scholar]
- Rawat R, Nguyen P, Kim S. et al. 2015. Incorporating Social Franchising (SF) Principles in Government Health Services Improves Breastfeeding (BF) Practices in Vietnam. The FASEB Journal 29: no. 1 Supplement 584.29. [Google Scholar]
- Rollins N, Bhandari N, Hajeebhoy N. et al. 2016. Breastfeeding in the 21st Century: why invest, and what will it take to improve breastfeeding practices. Lancet 287: 491–504. [DOI] [PubMed] [Google Scholar]
- Statistics Indonesia, National Population and Family Planning Board, Ministry of Health Indonesia & MEASURE DHS. 2013. DHS Final Report: Indonesia http://www.dhsprogram.com/publications/publication-FR275-DHS-Final-Reports.cfm#sthash.Wd9Kvl3X.dpuf.
- UNICEF. 2015. Statistic and Monitoring. http://www.unicef.org/statistics/index_countrystats.html, accessed 2 May 2015.
- UNICEF. 2013. Breastfeeding on the worldwide agenda: findings from a landscape analysis on political commitment for programmes to protect, promote and support breastfeeding. New York: UNICEF http://www.unicef.org/eapro/breastfeeding_on_worldwide_agenda.pdf
- UNICEF. 2011. Infant and Young Child Feeding: Programming Guide: http://www.unicef.org/nutrition/files/Final_IYCF_programming_guide_2011.pdf.
- UNICEF and WHO. 1981. International Code of Marketing of Breast-milk Substitutes. International Code of Marketing of Breast-milk Substitutes.
- United Nations. 1989. Convention on the rights of the child.
- Victora C, Bahl R, Barros A. et al. 2016. Breastfeeding in the 21st Century: epidemiology, mechanisms and lifelong effect. Lancet 287: 475–90. [DOI] [PubMed] [Google Scholar]
- Victora CG, Horta BL, de Mola CL. et al. 2015. Association between breastfeeding and intelligence, educational attainment, and income at 30 years of age: a prospective birth cohort study from Brazil. The Lancet Global Health 3: 199–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Viet Nam Social Insurance. 2012. Social Insurance Fund with the Extension of Maternity Leave for Female Employee to Six Months. Hanoi: Government of Viet Nam. [Google Scholar]
- WHO and UNICEF. 2009. Baby-friendly Hospital Initiative: Revised, Updated and Expanded for Integrated Care. Section 1: Background and Implementation. Geneva: WHO. http://whqlibdoc.who.int/publications/2009/9789241594967_eng.pdf?ua=1. [PubMed]
- WHO and UNICEF. 2003. Global Strategy for Infant and Young Child Feeding: http://www.who.int/nutrition/publications/gs_infant_feeding_text_eng.pdf. [PubMed]
- World Bank. 2015. Country and lending groups. http://data.worldbank.org/about/country-and-lending-groups#Low_income, accessed 15 July 2015.
- World Bank. 2014. World Bank Open Data. http://data.worldbank.org/, accessed 10 April 2014.
- World Health Organization. 2013. Global Health Observatory Data Repository. http://apps.who.int/gho/data/?theme=main, accessed 10 April 2015.
- Zweifel P, Breyer F, Kifmann M. 2009. Health Economics. 2nd Edition. Berlin Heidelberg: Springer-Verlag.