Abstract
Objective
Critical to the success of any intervention study is successful recruitment. The aim of this paper was to examine the recruitment process of a randomized controlled trial evaluating an intervention conducted with family child care home providers. Specifically, the recruitment challenges, the efforts employed to address the challenges, and their impact on participant recruitment are discussed.
Methods
The study’s original recruitment protocol was employed during waves 1 and 2 (out of 5). However, recruitment tracking showed a failure to meet enrollment targets, particularly in wave 2. Low enrollment prompted an all-day retreat to discuss potential revisions and enhancements to recruitment strategies. Four strategies to enhance the recruitment protocol emerged from the retreat: improving recruitment materials to enhance communication, increasing engagement with community partners, addressing provider concerns about participation and study burden, and facilitating parent engagement.
Results
The study successfully recruited 166 family child care home providers across the 5 waves. There was a significant impact on the recruitment of waves 3–5 versus waves 1–2 using the enhanced recruitment protocol. There was a dramatic increase in those who “consented” (43% vs. 60%, respectively) and a corresponding decrease in the percent of “interested and eligible” who then “failed to consent” (57% vs. 40%, respectively).
Conclusion
Results of these enhanced recruitment strategies demonstrate the many lessons learned about successful recruitment of a difficult-to-reach population, family child care homes; specifically, the importance of building relationships, communicating clearly, and identifying key motivators.
Keywords: Recruitment strategies, Family child care homes, Randomized controlled trial
1. Introduction
Child care is increasingly recognized as important setting for childhood obesity prevention efforts [1], [2]. These programs serve a large proportion of young children [3] who are still forming habits around eating and physical activity [4], [5]. While there have been some recent child care-based intervention studies, additional research is needed [6], [7], [8].
Critical to the success of any intervention study is recruitment of an adequate sample to ensure sufficient power to detect intervention impact. Unfortunately, recruitment receives little attention in the literature. Although the Consolidated Standards of Reporting Trials (CONSORT) Statement [9] has helped improve consistency in reporting of recruitment and retention [10], recruitment protocols details and lessons learned remain sparse [11].
Child care-based obesity intervention studies encounter multiple recruitment challenges, such as the need to recruit participants at multiple levels and to account for clustering. Primary outcomes are typically child-level variables (e.g., weight, diet, physical activity); therefore, parents must agree to participate and provide consent for children’s participation. However, the child care program provides the study setting — where data are collected and where the intervention is delivered. Hence, the program and center-level staff (e.g., director, teachers) must also consent to participate. The unit of randomization for these studies is often the child care program, thus necessitating the use of a cluster-randomized design, which in turn increases the required sample size.
Child care-based studies, particularly those testing prevention-focused interventions, should create recruitment messages that motivate child care programs and parents to join research studies. Weight-focused messages may be ineffective because weight is not recognized as an issue by the parent or child care provider compared to more acute health conditions [12], especially if the child is not yet obese but just at risk for obesity. Lack of motivation plagues many prevention studies, and results in low response to recruitment efforts (20–25%) [13].
Lastly, child care-based studies must consider the specific type of child care program being targeted. Child care programs vary greatly in number of children enrolled, quality of care, provider characteristics and program type (e.g., centers, Head Start, family homes). Most child care studies to date have targeted centers or Head Start programs. Family child care homes are generally much smaller in scale, with individuals caring for children in their homes. These businesses are less stable, thus potentially increasing the likelihood of losing homes due to closing. The clusters of children within these homes are small, generally less than 7 children. Homes often have lower fees and may enroll children from a diverse economic background whose parents may feel even less able to take on the burden of study participation. These unique characteristics can exacerbate recruitment challenges.
The current literature offers little in terms of specific strategies to address the recruitment challenges that accompany research in child care settings, particularly family child care homes. This paper addresses this gap by describing efforts used to recruit participants for the prevention intervention study, Keys to Healthy Family Child Care Homes. In this paper, we discuss recruitment efforts employed, challenges encountered during recruitment, enhancements made to recruitment, and the impact of those enhancements.
2. Methods
2.1. Keys study overview
The Keys to Healthy Family Child Care Homes study (Keys study) is a two-arm, cluster-randomized controlled trial evaluating the efficacy of a 9-month intervention designed to encourage healthy diet and physical activity habits in young children. Family child care home providers (FCCHs) are randomly assigned (1:1) into either the intervention or control arm. The intervention arm is delivered over nine months in three modules (each lasting 3 months), including “Healthy You,” “Healthy Home,” and “Healthy Business.” Participants assigned to the control arm receive an enhanced version of the Healthy Business module, also delivered over nine months. Specific study details are published elsewhere [14]. Primary outcomes are children’s physical activity and diet quality while at the FCCH. Additionally, children’s BMI, providers’ physical activity and diet quality, and provider’s FCCH practices around nutrition and physical activity are assessed as secondary outcomes. The study was approved by the Institutional Review Boards at the University of North Carolina at Chapel Hill and Duke University Medical Center.
2.2. Original recruitment protocol
The original power calculation [14] suggested a sample of 150 FCCHs and 450 children. To meet this goal, the original recruitment plan proposed recruiting in five waves, with each wave enrolling approximately 30 FCCHs and 90 children (on average, 3 children per FCCH). Recruitment efforts were planned across multiple counties in central North Carolina, each wave targeting a specific geographical area. Priority was given to counties with lower income and higher child obesity rates. At the outset of each wave, a recruitment pool of FCCHs was identified from the NC Division of Child Development website [15], a publically available online database of licensed child care facilities in NC. To be eligible for participation, FFCH providers had to have at the very minimum two children currently enrolled between the ages of 18 months and 4 years, serve at least one meal and one snack to children, be open year round, and have been in business for two years with no plans to close in the coming year.
The original recruitment protocol began by emailing information about the study to a diverse group of local community partners (e.g., child care partnerships, health department, child care resource and referral agencies) with strong ties to local child care programs. The goal of this initial contact was to inform these partners about the study and garner their support. The next step in recruitment was to mail and email all potential FCCHs in the designated sample areas an invitation and information flyer inviting them to participate. Invitations were followed by a phone call from study staff. During these phone calls, study staff described the study in detail, including the intervention and control programs (topics addressed, time required, potential for continuing education credits), the process of randomization (i.e., potential assignment to control condition), required measures, and incentives ($75 after baseline assessments, $125 after follow-up assessments, and up to 28 contact hours (or 2.8 continuing education units) for participating in the intervention. Interested providers were then screened for eligibility. FCCHs who were both “interested and eligible” moved to the “eligible and interested” list. For those FCCHs who were not interested, effort was made to understand the reasons for disinterest. Commonly reported reasons included: lack of time, currently taking classes toward a degree, wary of having strangers in their home, and concern that parents would not be interested. FCCHs that were unable to be contact were classified as “unscreened.”
Interested and eligible FCCH providers were then mailed a “welcome packet” containing an introductory letter with an overview about the study, a demographics survey, a health survey, and a consent form for them to sign and return. The packet also included “information packets” for parents, including an introductory letter about the study geared toward parents, a demographics survey, and a consent form for child participation, which the provider distributed to the parents. About one week later, staff followed up with a phone call in case the provider had any questions about the study or the completed information packets. If at least 3 parents agreed to take part, the provider was asked to mail back all materials using the provided postage paid envelope.
Once the necessary consent information was received, the FCCH was considered to be “consented” and efforts were made to schedule a 2-day, in-home measurement visit. This measurement visit had to be completed and all measures collected before the FCCH was considered eligible for randomization. Randomization occurred once the enrollment target for the wave was complete.
A tracking database was created in order to monitor completion of this multi-step recruitment protocol and movement of providers toward randomization. All potential FCCHs identified from the targeted counties were listed in this database. The database was used to record the date that mail and email invitations were distributed, date of interest and screening call, number of attempts required to complete this call, date that welcome packet was mailed, completion of consent (or failure to obtain sufficient parent consent), and date of measurement visit. In addition, a participant call log and screener were created for every potential FCCH participant to capture more detail regarding the interest and screening call. The call log captured each call attempt, including date and time, outcome of call, and any relevant notes. The screener then captured initial interest and compliance with eligibility criteria. From this tracking information we were able calculate the number of FCCHs who were contacted from the pool of possible providers, and determine the number who were interested in the study and eligible for participation.
2.3. Recruitment problems identified
This original recruitment protocol was used for waves 1 and 2 (April 2013 through December 2013). Wave 1 targeted counties in the immediate area surrounding the two university sponsors and met the recruitment goal of 30 FCHHs and 90 children. However, wave 2 targeted counties further away and resulted in the recruitment of only 18 homes and 52 children - only 60% of the original recruitment goal. Low enrollment prompted the study team to regroup and closely examine recruitment procedures. Adding to this problem was the need to re-examine power calculations to adjust for lower than projected retention of child participants observed during wave 1 follow-up. Based on our previous work in child care and the pilot study, projected loss to follow-up was 20%; however, the actual observed loss to follow-up for wave 1 was 47%. Hence, retained clusters were approximately two children per home instead of three. The short duration of the pilot (only 6 weeks instead of 36 weeks) likely limited the opportunity for child turnover during the pilot and masked the true rates of turnover in FCCHs. Reasons for this higher loss observed during the initial waves of the study included change in parent’s employment status, loss of employment, or, most commonly, change in child care arrangements (e.g., moving to neighbor-care or moving children into center-based care). Because of this retention issue, a new power calculation was conducted which increased the enrollment target from 150 to 165 FCCH providers which further added to our recruitment challenge.
2.4. Enhanced recruitment protocol
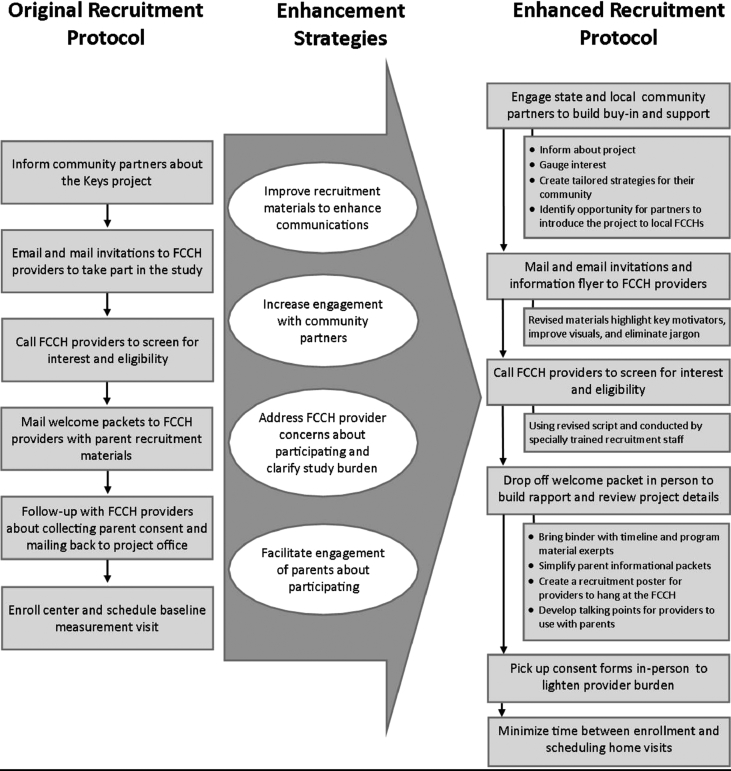
Investigators and critical personnel attended an all-day retreat to discuss potential revisions and enhancements to recruitment strategies. After a careful review of existing strategies and feedback from recruitment, measurement, and intervention staff members, the group identified several strategies to enhance recruitment efforts. These strategies generally fell within one of four categories, including: (1) improving recruitment materials to enhance communication (e.g., identify key motivating messages for each target of recruitment – community, FCCH provider, parent; and eliminate use of jargon), (2) increasing engagement with community partners, (3) addressing provider concerns about participating and study burden, and (4) facilitating engagement of parents. Fig. 1 illustrates the impact of these enhanced recruitment strategies on the recruitment protocol and details of these enhancements are described below.
-
1.
Improved Recruitment Materials: Close scrutiny was given to all recruitment materials, including materials used with community stakeholders, FCCH providers, and parents. Although care was taken in the development of the original materials, their use in waves 1 and 2 identified materials and components which needed improvement. For example, it was critical that messages better addressed key motivators and perceived barriers for each of the groups being targeted (providers and parents). Additionally, materials were edited to simplify language, remove jargon, reduce reading level, and improve understanding. Specific enhancements are described below.
-
2.
Increased Engagement with Community Partners: Gaining endorsement from local community partners was important for enhancing perceptions of the study’s legitimacy and importance among FCCH providers. Recruitment for wave 1 included moderate community engagement efforts, but no additional effort was undertaken in wave 2. The lack of local endorsement was particularly problematic as recruitment efforts moved further away from the universities where the project and study team were housed. To address these issues, we worked with state-level contacts, with whom we had long-standing partnerships, to get introductions to local community partners. A slideshow presentation and 1-page flyer about the study were created to help inform the state partners about the study. In addition, state-level partners were provided a template for an email introduction of the study to their local contacts that emphasized their endorsement of the study and the potential community benefits of participation. In addition, contacts were made with a large variety of local community organizations that interact with and support FCCH providers (e.g., Smart Start, Child Care Resource & Referral, CACFP sponsoring organizations). The project manager followed up with these local community organizations to arrange a call or in-person meeting with all professionals within that organization who regularly engaged with FCCH providers to provide educational programs, trainings, problem-solving, and career support. These individual had established relationships with FCCH providers and were trusted sources of information. That call/meeting was used to introduce the study (using the slideshow presentation and 1-page flyer described above), gauge the community’s interest, and discuss strategies for engaging local FCCH providers. These individuals helped develop tailored strategies for engaging their local FCCH providers and how they and their organization could help “introduce” the study and give their “seal of approval”. The study staff offered a variety of templates to facilitate these efforts (e.g., email, newsletter announcement) and offered study staff to attend any in-person meetings attended by FCCHs providers (e.g., scheduled trainings).
-
3.
Address Provider Concerns about Participation: Feedback from those “not interested” in waves 1 and 2 revealed that providers were often quite apprehensive about participating in a research study. They were concerned about the time required, confused about requirements, did not want to take part in measures, and worried about how collected information might be used. The mail and email invitations and information flyer were revised to make sure that key benefits from participation were highlighted (e.g., potential to earn contact hours), to emphasize that the study team was not associated with any accrediting bodies, and helpful topics being addressed in both the intervention and control programs were emphasized. Recruitment scripts were re-written to improve the order in which study components were presented and to simplify and clarify what to expect if they participated. A rigorous training protocol was adopted for all recruitment staff that included multiple rounds of practice and feedback prior to a “certification.” To help build rapport, welcome packets were delivered in person (instead of by mail). During this in-person delivery visit, recruitment staff brought a binder of materials with a visual of the study timeline (to clarify expectations around study participation), showed excerpts from program materials (to illustrate the professional quality of the program), reviewed consent forms and surveys, discussed how to present the study to parents, and answered any questions the provider had. Additionally, the welcome packets were streamlined and made to be more visually appealing. The cover page was also reworked to provide a simple study description as well as brief step-by-step instructions for how to get their FCCH enrolled.
-
4.
Facilitate Parent Engagement: Although research staff was prepared to help FCCH providers with parent recruitment, most providers were hesitant to allow direct contact with parents. To help initiate these parent conversations, FCCH providers were given a study poster to display in their home, a handout of talking points, and a parent Frequently Asked Questions (FAQ). These elements helped guide providers’ conversations with parents about what would happen during measurement (in particular, wearing the accelerometer) and the intervention period. These materials helped providers feel more comfortable explaining the study and answering questions from parents. We also revised and simplified the material in the parent information packets, based on the concerns expressed in waves 1 and 2 that lengthy packets made the study appear too cumbersome. The packet materials used in waves 1 and 2 did represent an improvement over those used in the pilot (e.g., incorporated project logo and branding, highlighted incentives, improved messaging); however, challenges noted in waves 1 and 2 demonstrated that additional modifications were needed. Unnecessary material was deleted (e.g., welcome letter from the investigators) and information about study overview, measures, and next step instructions were condensed into a single cover page.
Fig. 1.
Enhanced strategies implemented in response to initial recruitment problems. The left column represents the original sequence of recruitment events, the middle arrow describes the challenges, and the right column shows the enhanced recruitment procedures.
2.5. Evaluation of recruitment success
Success of recruitment methods could be compared using data from the tracking database. The recruitment “pool” represents all potential FCCH providers licensed within the counties being targeted during a given wave. “Screened” represents all FCCH providers who completed the phone call that screened for interest and eligibility. Based on these calls, providers were categorized as “not interested”, “not eligible”, or “interested and eligible.” The screening procedure first assessed interest, then eligibility but for only those interested. Once deemed “eligible and interested,” welcome packets were delivered. At this point, some providers lost interest or failed to get parent buy-in and consent; these were labeled as “failed to consent” with “consented” being those FCCH providers who agreed to participate, met inclusion criteria (including parent consents, and signed the consent document). Once consented, measurement visits were scheduled; if successfully completed, the FCCH along with the index children, were classified as “consented and measured” and were eligible for randomization into the study.
3. Results
In total, the study has successfully recruited 166 FCCH providers and 496 children. All providers are female, and, on average, 49.7 years of age. A vast majority are African American (79%) and most either overweight or obese (BMI≥ 25, 89%). Incomes are relatively modest, with 75% of providers reporting a household income below $50,000 (median income for this area). Education levels of providers are primarily a high school diploma or general education development (GED) (24.7%) or an Associate’s degree (49.5%). Most of the enrolled FCCH programs (68%) have received a high quality rating (4- or 5-stars) based on North Carolina 5-star Quality Rating Indicator. Table 1 provides a detailed description of providers’ characteristics, with slight fluctuations in participant characteristics observed across waves. T-tests comparing the characteristics of participants recruited in waves 1–2 to those in waves 3–5 revealed that there were no significant differences in any of these demographic variables (p values ranged from 0.16 to 0.82). The slight differences seen between waves are most likely attributable to the counties where recruitment took place (e.g., wave 3 targeted more rural counties), rather than to a preferential recruitment of FCCH providers with higher incomes or education levels.
Table 1.
Characteristics of FCCH providers by wave.
| FCCH providers |
Wave 1 n = 30 |
Wave 2 n = 18 |
Wave 3 n = 27 |
Wave 4 n = 50 |
Wave 5 n = 41 |
Total n = 166 |
|---|---|---|---|---|---|---|
| Female | 30 (100%) | 18 (100%) | 27 (100%) | 50 (100%) | 41 (100%) | 166 (100%) |
| Age (years) | 47.37 | 50.56 | 50.04 | 50.56 | 48.34 | 49.33 |
| Racial category | ||||||
| Asian | 0 (0%) | 0 (0%) | 1 (3.7%) | 1 (2.0%) | 0 (0%) | 2 (1.2%) |
| Native Hawaiian or Pacific Islander | 0 (0%) | 1 (5.6%) | 0 (0%) | 0 (0%) | 0 (0%) | 1 (0.6%) |
| Black or African American | 24 (80.0%) | 14 (77.8%) | 21 (77.8%) | 35 (70.0%) | 29 (70.7%) | 123 (74.1%) |
| White | 4 (13.3%) | 3 (16.6%) | 5 (18.5%) | 10 (20.0%) | 8 (19.5%) | 30 (18.1%) |
| More than one race | 2 (6.7%) | 0 (0%) | 0 (0%) | 4 (8.0%) | 4 (9.8%) | 10 (6.0%) |
| Ethnic category | ||||||
| Hispanic or Latino | 1 (3.3%) | 1 (5.6%) | 1 (3.7%) | 2 (4.0%) | 3 (7.3%) | 8 (4.8%) |
| Not Hispanic or Latino | 29 (96.7%) | 17 (94.4%) | 26 (96.3%) | 48 (96.0%) | 38 (92.7%) | 158 (95.2%) |
| Income | ||||||
| Less than $25,000 | 7 (23.3%) | 4 (22.2%) | 5 (18.5%) | 8 (16.0%) | 14 (34.1%) | 39 (23.5%) |
| $25,000–$50,000 | 13 (43.3%) | 10 (55.6%) | 14 (51.9%) | 30 (60.0%) | 20 (48.8%) | 86 (51.8%) |
| Greater than $50,000 | 8 (26.7%) | 4 (22.2%) | 8 (29.6%) | 10 (20.0%) | 6 (14.6%) | 36 (21.7%) |
| Missing (unreported) | 2 | 0 | 0 | 2 | 1 | 5 |
| Education | ||||||
| High school diploma or GED | 2 (6.7%) | 7 (38.9%) | 7 (25.9%) | 15 (30.0%) | 9 (22.0%) | 41 (24.7%) |
| Associate’s degree or 60 h college credit | 15 (50.0%) | 6 (33.3%) | 20 (74.1%) | 20 (40.0%) | 21 (51.2%) | 82 (49.4%) |
| Bachelor’s degree | 11 (36.6%) | 5 (27.8%) | 0 (0%) | 12 (24.0%) | 10 (24.4%) | 37 (22.3%) |
| Master’s degree | 2 (6.7%) | 0 (0%) | 0 (0%) | 2 (4.0%) | 1 (2.4%) | 5 (3.0%) |
| Missing (unreported) | 1 | 1 | ||||
| Degree in early childhood education or childhood development | ||||||
| Yes | 15 (50.0%) | 7 (38.9%) | 16 (59.3%) | 19 (38.0%) | 21 (51.2%) | 78 (47.0%) |
| BMI (kg/m2, average) | 33.63 | 33.74 | 33.82 | 32.56 | 33.32 | 33.28 |
| Normal weight (BMI<25) | 2 (6.7%) | 2 (11.1%) | 2 (7.4%) | 8 (16.0%) | 3 (7.3%) | 17 (10.2%) |
| Overweight (BMI 25–29) | 6 (20.0%) | 4 (22.2%) | 9 (33.3%) | 13 (26.0%) | 8 (19.5%) | 40 (24.1%) |
| Obese (BMI > 30) | 22 (73.3%) | 12 (66.7%) | 16 (59.3%) | 29 (58.0%) | 30 (73.2%) | 109 (65.7%) |
| Star ratinga | ||||||
| 1 or 2 stars | 0 (0%) | 1 (5.6%) | 3 (11.1%) | 3 (6.0%) | 6 (14.6%) | 13 (7.8%) |
| 3 stars | 7 (23.3%) | 7 (38.9%) | 7 (25.9%) | 15 (30.0%) | 4 (9.8%) | 40 (24.1%) |
| 4 stars | 15 (50.0%) | 3 (16.6%) | 12 (44.5%) | 19 (38.0%) | 19 (46.3%) | 68 (41.0%) |
| 5 stars | 8 (26.7%) | 7 (38.9%) | 5 (18.5%) | 13 (26.0%) | 12 (29.3%) | 45 (27.1%) |
| Accepts CACFPbsubsidy | ||||||
| Yes | 30 (100%) | 16 (88.9%) | 25 (92.6%) | 45 (90.0%) | 35 (85.4%) | 151 (91.0%) |
Star Rating is a North Carolina indicator of child care quality that rates all child care programs on a scale of 1–5 stars.
CACFP = the Child and Adult Care Food Program, a federal program that provides reimbursement for meals provided to low income children.
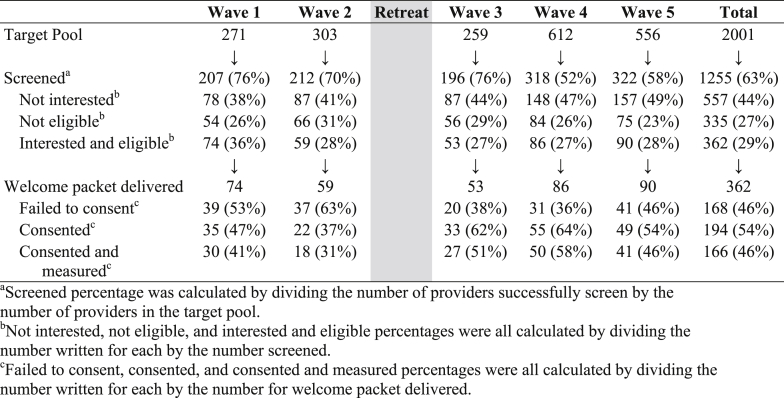
Recruitment tracking across the five waves (Table 2) illustrates the impact of changes to the recruitment protocol on advancing the potential FCCH participants successfully through the multi-step recruitment process. During each wave, roughly 200–300 providers were screened. Waves 4 and 5 had the largest number of providers screened (318 and 322, respectively). The decrease in percent screened during these later waves is the result of the larger target pools employed (roughly double the size of target pools in earlier waves). The percentage of potential participants who opted out during screening, indicating “not interested,” increased between waves 1–2 and waves 3–5 (39% vs. 47%, respectively). This increase in “not interested” could be seen as negative feedback to the revised protocol; however, it may also reflect improved explanations of study procedures and requirements allowing us to secure a more committed participant from the outset. Eliminating not interested providers earlier in the recruitment process allows us to better direct our efforts toward providers who may actually enroll and remain through randomization.
Table 2.
Tracking of recruitment steps by wave.
Those screened as “interested and eligible” ranged from 27 to 36%, with an average of 29% across all waves. All of those screened as “interested and eligible” received a welcome packet. For this step in the recruitment process, there was a measurable increase in those who “consented” (43% vs. 60%, respectively) and a corresponding decrease in the percent of “interested and eligible” who then “failed to consent” (57% vs. 40%, respectively). Again, these shifts appear to demonstrate the positive impacts of the recruitment protocol changes. FCCH providers had a clearer understanding of the study, a chance to meet a member of the staff in-person (associating the study with a friendly face), support for eliciting parent participation, and reduced burden for returning consents. The conversion from “interested and eligible” to “consented” was slightly lower in wave 5 due to the preset cap on enrollment of 165 FCCHs, which limited our ability to complete the recruitment process with all eligible and interested providers. Once we reached the maximum recruitment target, it was necessary to close recruitment.
Based on data collected in the screener, a majority of the participants, 105 (63%), learned about the study through the mailed invitation. This recognition of the mailed invitation was present across all waves. Professional referral was noted by 35 providers (21%) as a way they learned about the study, particularly in later waves when there was increased engagement with community partners. The emailed invitation, provider referral, and website appeared to be less effective strategies for reaching this population of FCCH providers.
4. Discussion
To our knowledge, this is the first paper to provide a detailed description of recruitment efforts for an intervention study set in family child care homes. Even through FCCHs are a unique organizational setting, the lessons learned offer several strategies that can potentially enhance overall recruitment efforts in child care-based studies. The original recruitment plan for Keys was based on years of experience recruiting child care centers and/or parents into prevention trials and our formative and pilot studies [14]. When implemented, the biggest challenges encountered centered around providers’, and to a lesser degree parents’, mistrust, apprehension, and lack of interest in being in a research study. It is not unexpected to encounter challenges during recruitment, even with careful planning. Cruz and colleagues used lessons learned from recruitment in Pathways [16] to plan their Head Start-based obesity prevention study [17]. Despite a recruitment plan that incorporated strategies directed at multiple audiences (Head Start centers, children, parents), challenges were noted including confusion about eligibility, failure to get consent, history of distrust and low enrollment. We used a full-day retreat of the investigative team to critically evaluate the original recruitment protocol and identify changes needed to enhance those efforts. Modifications included improving recruitment materials, increasing engagement with community partners, addressing provider concerns about participation, and facilitating parent engagement. Common among these changes were the importance of building relationships, communicating clearly, and identifying key motivators.
The enhanced recruitment protocol invested more time in building relationships that could help access FCCHs and engage providers and parents. We looked for opportunities for facilitated introductions whenever possible using local community connections. Once connected, we moved to solidify the connection, establish good rapport, and build enthusiasm and support for the study. FCCH providers were pivotal in the study – they were participants as well as gatekeepers to parent and child participants. These providers are a challenging population to engage, but having the support and endorsement of local community partners increased provider receptivity to the study because they first learned about it from someone they knew and trusted. “Relationships” was a reoccurring theme in recruitment strategies proposed by Schoeppe and colleagues following their literature review of recruitment papers from studies with children and Delphi study with researchers [18]. Among the 16 effective recruitment strategies identified, they noted the importance of (1) having support from key stakeholders or project champions and (2) investing time in developing relationships with study partners.
Building good relationships is particularly important when working in FCCHs, as this population is often skeptical and unfamiliar with research. Generally, their only experience with someone coming into the home to assess their practices is associated with licensure, which can be very stressful. Part of the relationship building was introducing providers to research – what it meant to be in a research study, what they would be asked to do, and how their confidentiality would be maintained. Even once this relationship was established with providers, they were often unwilling to allow study staff into their home to recruit parents directly. While direct recruitment of parents is often preferred and seen as more effective [17], [18], it was important to remain flexible with FCCH providers around this issue so as not to damage our relationship. The time we invested with FCCH providers became even more important as we needed to get them excited about the study and provide the information and tools necessary to engage their families for study participation.
The enhanced recruitment protocol also paid closer attention to clear and effective communication, a theme that occurs often in studies of recruitment [18], [19]. In the literature, effective communication requires identifying the most appropriate communication channels (e.g., posters, flyers, direct mail, email, phone, in-person) and key messages (e.g., study purpose, requirements, benefits) [18], [19]. For each step in the recruitment process, we examined the communication channels employed, key messages conveyed, and language and terminology used. The enhanced protocols called for use of a wider variety of communication channels that could appeal to different learning styles. In-person delivery of the welcome packet and provision of visuals around key study details (e.g., timeline, sample program materials) assisted providers in understanding just what would be required of them. These approaches helped ensure that the numerous details about study participation were clearly conveyed so that participants could make an informed choice before enrolling. Messages delivered were also revisited to make sure that they were clear, simple, and focused on the most important details. We also found it important to watch for potential hidden meanings that certain words may have. For example, “activity monitors” was originally used to refer to accelerometers, but we learned that “monitor” created thoughts of “surveillance” which seemed intrusive. Hence, revised materials replaced “activity monitor” with “step counter.”
Enhancing the effectiveness of our communication in the revised protocol also required examining key motivators for participation, another common theme that arises in recruitment studies [17], [18]. To identify key recruitment motivators for each of our targeted audiences (i.e., community partners, FCCH providers, and parents) required that we interact with and get to know each of these groups. While enthusiasm and incentives are important, we learned that key motivators for our study needed to speak to shared interests and goals and how we might work together to identify win-win opportunities. For example, community partners were often local affiliates of state-level organizations working with child care (e.g., Smart Start Partnership, food program sponsors). The mission of these organizations often includes improving the quality of child care or the health or nutrition of children. Key motivating messages for these community partners thus focused on how our study, and its intervention, could support their own goals and contribute resources toward their agencies’ mission.
Identifying key motivators for FCCH providers was more difficult given our limited experience with this type of provider. Like other child care providers we had worked with, we knew there was a strong motivation to provide good care for children to put them on a path for success. However, we learned that our messages also needed to address FCCH providers’ unique challenges. For example, these providers have little “extra” time; they often have no additional staff support; they manage multiple responsibilities (e.g., providing child care, running a business); and they deal with a lot of turnover and unpredictability in child enrollment (and hence financial instability). Revised messages, therefore, focused on how the intervention had been tailored for FCCH providers – delivering much of the intervention in-home and on their schedule, helping them fulfill licensing requirements for contact hours/continuing education, and, not least, including a component that addressed good business practices.
This sub-study of recruitment methods offers many lessons regarding keys to successful recruitment for a difficult-to-reach population; however, it is not without limitations. The major limitation is the quasi-experimental evaluation of different recruitment protocols. Conclusions drawn about the impact of the enhanced strategies represent a comparison across waves rather than within waves. These waves often targeted different geographical areas, which may have also impacted some of the differences in recruitment success that were observed. Given these differences across waves, future analyses will control for wave. Another limitation is our inability to rigorously test whether some strategies were more fruitful than others. Later waves employed all of the enhanced strategies, which represented the most promising and feasible ideas generated by the collective research team. Finally, we did not attempt to assess recruitment costs; therefore, a cost comparison across waves is not possible.
Although not tracked explicitly, the enhanced methods did cost more. Enhanced strategies required an additional investment of staff time to revise recruitment materials (e.g., agendas, talking points, slideshows and handouts for community partners; mail and email invitations, flyers, posters, parent talking points for providers; informational packets for parents; and all consent materials) so that messages were clear, simple, effective, and visually appealing. The new protocol also required more staff and/or staff time to implement. Mileage was another large expense because we added an additional trip to each FCCH. For use in subsequent studies, feasibility and cost of dropping off and picking up recruitment materials should be considered. However, ineffective recruitment efforts are costly because they may result in premature participant drop-out and extra time to keep a participant in the study when they are less enthusiastic at study entry.
5. Conclusions
This sub-study of recruitment reinforces many issues expressed by other researchers especially in recruiting hard-to-reach populations. As noted by Schoeppe and colleagues [18], successful strategies include building trusting relationships, finding champions (or connectors), augmenting enrollment procedures, minimizing participant burden, and working within a well-connected research team. Researchers interested in conducting studies that involve family child care home providers should (1) carefully plan and articulate their recruitment protocol, (2) engage trusted partners early in the process, (3) develop strategies within the recruitment protocol that create trust and connectedness between the FCCH provider and the study, (4) conduct the process with a participant-centered mindset, and (5) include sufficient resources for recruitment. These approaches are necessary to implement a successful recruitment process with the potential for launching and sustaining a successful intervention study within the community.
Acknowledgements
We would like to thank the following people who contributed to the recruitment for the Keys project:
Megan Peters, Colleen Lynd, Julie King, Kamaria Mason, Linda Shipman, Tiffany Glasscock, Cathy Horner, Charlotte Zuber, Ashely McGee, Charmee Mehta, Alex Lang, Charlotte Stoute, Kahliah Gordon, Charmaine Bell-Grantham, Riley Craven, Hannah Heidenreich, Daniela Canasi, Joy Long, Sakinah Omar, our Community Advisory Group of local family child care home providers, and all of the providers and the children who participated in the project.
This research was funded by the National Heart, Lung, And Blood Institute of the National Institutes of Health under Award Number R01HL108390. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The sponsor played no role in the study design; collection, analysis, or interpretation of the data; writing of the article; or decision to publish this article.
References
- 1.Birch L.L., Ventura A.K. Preventing childhood obesity: what works? Int. J. Obes. 2005;2009(33):S74–S81. doi: 10.1038/ijo.2009.22. [DOI] [PubMed] [Google Scholar]
- 2.Larson N., Ward D.S., Neelon S.B., Story M. What role can child-care settings play in obesity prevention? A review of the evidence and call for research efforts. J. Am. Diet. Assoc. 2011;111:1343–1362. doi: 10.1016/j.jada.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 3.Laughlin Lynda. Who’s Minding the Kids? Child Care Arrangements: Spring 2011. Current Population Reports. U.S. Census Bureau, Washington, DC. 2013:70–135. [Google Scholar]
- 4.Story M., Kaphingst K.M., French S. Vol. 16. The David and Lucile Packard Foundation; 2006. pp. 143–168. (The Role of Child Care Settings in Obesity Prevention. The Future of Children/Center for the Future of Children). [DOI] [PubMed] [Google Scholar]
- 5.Monasta L., Batty G.D., Cattaneo A. Vol. 11. 2010. pp. 695–708. (Early-life Determinants of Overweight and Obesity: a Review of Systematic Reviews). [DOI] [PubMed] [Google Scholar]
- 6.Zhou Y., Emerson J., Levine R., Kihlberg C., Hull P. Vol. 28. 2014. pp. 92–103. (Childhood Obesity Prevention Interventions in Childcare Settings: Systematic Review of Randomized and Nonrandomized Controlled Trials). [DOI] [PubMed] [Google Scholar]
- 7.Mikkelsen M., Husby S., Skov L., Perez-Cueto F. 2014. A Systematic Review of Types of Healthy Eating Interventions in Preschools; p. 13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ward D.S., Vaughn A., McWilliams C., Hales D. Vol. 42. 2010. Interventions for Increasing Physical Activity at Child Care; pp. 526–534. [DOI] [PubMed] [Google Scholar]
- 9.Begg Colin, Cho Mildred, Eastwood Susan, Horton Richard, Moher David, Olkin Ingram, Pitkin Roy, Rennie Drummond, Schulz Kenneth F., Simel David, Stroup Donna F. Improving the quality of reporting of randomized controlled trials: the CONSORT statement. JAMA. 1996;276:637–639. doi: 10.1001/jama.276.8.637. [DOI] [PubMed] [Google Scholar]
- 10.Turner L., Shamseer L., Altman D.G., Schulz K.F., Moher D. Does use of the CONSORT Statement impact the completeness of reporting of randomised controlled trials published in medical journals? A Cochrane review. Syst. Rev. 2012;1:60. doi: 10.1186/2046-4053-1-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Toerien M., Brookes S., Mecalfe C. 2009. A Review of Reporting of Participant Recruitment and Retention in RCTs in Six Major Journals; p. 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Senturia Y., McNiff M., Baker D. Vol. 19. 1998. pp. 544–554. (Successful Techniques for Retention of Study Participants in an Inner-city Population). [DOI] [PubMed] [Google Scholar]
- 13.Spoth R., Redmond C. Vol. 9. 1994. pp. 353–370. (Effective Recruitment of Parents into Family-focused Prevention Research: a Comparison of Two Strategies). [DOI] [PubMed] [Google Scholar]
- 14.Østbye T., Mann C., Vaughn A. Vol. 40. 2015. pp. 81–89. (The Keys to Healthy Family Child Care Homes Intervention: Study Design and Rationale). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.North Carolina Division of Child Development. Child Care Facility Search Site. http://ncchildcaresearch.dhhs.state.nc.us/search.asp. accessed, 2013.
- 16.Gittelsohn J., Davis S., Steckler A. Vol. 37. 2003. pp. S107–S112. (Pathways: Lessons Learned and Future Directions for School Based Interventions Among American Indians). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cruz T., Davis S., FitzGerald C., Canaca G., Keane P. Vol. 35. 2014. pp. 135–149. (Engagement, Recruitment, and Retention in a Trans-community, Randomized Controlled Trails for the Prevention of Obesity in Rural American Indian and Hispanic Children). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schoeppe S., Oliver M., Badland H., Burke M., Duncan M. Vol. 21. 2014. pp. 794–803. (Recruitment and Retention of Children in Behavioral Health Risk Factor Studies: REACH Strategies). [DOI] [PubMed] [Google Scholar]
- 19.Tiwari T., Casciello A., Gansky S. 2014. Recruitment for Health Disparities Preventive Intervention Trials: the Early Childhood Caries Collaborating Centers; p. 11. [DOI] [PMC free article] [PubMed] [Google Scholar]