Abstract
Objective To examine longitudinal reciprocal relationships between marijuana use and psychiatric disorders, and identify the role of HIV in a sample (N = 340) of youth perinatally infected with HIV (PHIV+) and youth perinatally exposed but uninfected with HIV (PHIV−) (60.6% PHIV+; 9–16 years at baseline; 51% female). Methods Cross-lagged structural equation modeling was used to examine longitudinal associations between changes in marijuana use and changes in any behavioral, mood, and anxiety disorders at three time points across adolescence. Results Marijuana use predicted behavioral and mood disorders in youth, regardless of HIV status. Behavioral and mood disorders predicted marijuana use for PHIV− youth; behavioral disorders predicted marijuana use for PHIV+ youth. Anxiety disorders and marijuana use were not associated for either group. Conclusions For PHIV+ and PHIV− youth, interventions that target early marijuana use may reduce later psychiatric disorders. Similarly, treatment for early behavioral disorders may prevent subsequent marijuana use.
Keywords: adolescent HIV, longitudinal, marijuana use, perinatal HIV, psychiatric disorders
Youth in the United States with perinatal HIV infection (PHIV+) are at high risk for psychiatric disorders (Mellins et al., 2009; Mellins & Malee, 2013). In addition, as they age through adolescence, PHIV+ youth increasingly experiment with marijuana similar to their noninfected peers (Alperen et al., 2014; Elkington, Bauermeister, Santamaria, Dolezal, & Mellins, 2015). Recent studies have documented the significant impact of marijuana use on the developing adolescent brain, including reduced neuronal connectivity and volume of specific brain structures (Volkow, Baler, Compton, & Weiss, 2014). Furthermore, studies in adolescent community and treatment samples have demonstrated a robust association between marijuana use and psychiatric disorders (Armstrong & Costello, 2002; Rey, Martin, & Krabman, 2004). These comorbidities have been associated with a more serious course of mental illness, poorer treatment response (Kessler, 2004), and poorer behavioral health outcomes, including sexual risk behavior and nonadherence to treatment for chronic health conditions (Elkington et al., 2008; Hicks et al., 2007).
Negative behavioral health outcomes during a developmental period of normative increased risk behavior are of particular concern in PHIV+ youth, who are coping with a chronic, sexually transmittable health condition that itself has neurological effects (Mellins & Malee, 2013; Tassiopoulos et al., 2013). As pediatric HIV in the United States becomes an adolescent and young adult epidemic, understanding the developmental course of co-occurring marijuana use and psychiatric disorders will have important implications not only for psychiatric and substance use treatment, but also for long-term HIV management and reduction of HIV transmission.
PHIV+ youth are at increased risk for marijuana use and psychiatric disorders owing to individual, family, and contextual risk factors—for example, residing in impoverished inner-city communities; exposure to trauma, violence, or parental illness or death; parental psychiatric or substance use (Havens & Mellins, 2008; Lee, Lester, & Rotheram-Borus, 2002). However, the influence of HIV infection on the association between psychiatric disorders and marijuana use remains largely unexamined. Many US PHIV+ youth experienced early years of less advanced antiretroviral treatment, and poorly controlled HIV infection (Gonzalez-Scarano & Martin-Garcia, 2005) that may have affected CNS function, including the subcortical white matter and frontostriatal systems involved in regulation of mood and behavior (Sharer, 2005). Thus, PHIV+ youth with a history of viremia may be at increased risk for mental health problems and experience greater impact of marijuana use.
Existing studies of PHIV+ youth focus on younger adolescents, who have relatively low rates of marijuana use (Alperen et al., 2014; Elkington, Bauermeister, Brackis-Cott, Dolezal, & Mellins, 2009; Elkington et al., 2015) and examine either a cross-sectional association between substance use and psychiatric disorders (Kapetanovic et al., 2011; Mellins et al., 2009; Williams et al., 2010) or development of each problem separately over time (Alperen et al., 2014; Gadow et al., 2012; Mellins et al., 2012). Yet, marijuana use and psychiatric disorders may be related in three important ways: marijuana use may lead to psychiatric disorders (Griffith-Lendering, Huijbregts, Mooijaart, Vollebergh, & Swaab, 2011; Patton et al., 2002), psychiatric disorders may lead to marijuana use (Brook, Brook, Zhang, Cohen, & Whiteman, 2002; O'Neil, Conner, & Kendall, 2011), or a third shared underlying variable may moderate or mediate the association (Fergusson, Boden, & Horwood, 2011).
To our knowledge, no published studies have examined the longitudinal and reciprocal relationship between marijuana use and psychiatric disorders in PHIV+ youth. Use of longitudinal data enables us to examine the association between changes in marijuana use and psychiatric disorders. Moreover, a comparison group of perinatally HIV-exposed but uninfected (PHIV−) youth with similar sociodemographic characteristics (e.g., age, HIV+ mother, poverty, race/ethnicity, neighborhoods of residence) offers a unique opportunity to examine the role of HIV.
Using data from a longitudinal study examining mental health and behavioral health outcomes in New York City (NYC) PHIV+ and PHIV− youth, we examine the reciprocal relationship between marijuana use and psychiatric disorders over time. Beyond the expected cross-sectional associations between psychiatric disorders and marijuana use documented in the literature, hypotheses include (1a) increases in marijuana use will predict onset of psychiatric disorders; (1b) these associations will be stronger for PHIV+ youth than for PHIV− youth; (2a) the onset of psychiatric disorders will predict increased marijuana use; and (2b) these associations will be stronger for PHIV+ youth than for PHIV− youth.
Methods
Participants and Procedures
Project CASAH (Child and Adolescent Self Awareness and Health; CASAH-1) participants were recruited between 2003 and 2008 from four NYC medical centers providing primary and tertiary care to HIV-affected families to complete two interviews approximately 18 months apart. Participants included youth and his/her primary caregiver with the following inclusion criteria: (1) youth aged 9–16 years with perinatal exposure to HIV (confirmed by medical providers and charts), (2) cognitive capacity to complete interviews, (3) English- or Spanish-speaking, and (4) caregiver with legal ability to sign permission for child participation.
Of 443 eligible participants at baseline (BL), 17% refused contact or could not be contacted by the study coordinators. Of the 367 caregiver–youth dyads approached, 340 were enrolled at BL (77% of eligible families; 206 PHIV+ and 134 PHIV− youth), and 82% (166 PHIV+ and 114 PHIV−) were retained at the first follow-up (FU1).
Although not initially planned, additional funding was secured to continue to follow the cohort (CASAH-2) for three additional interviews (FU2, FU3, FU4); for CASAH-2, 84% of CASAH-1 youth (179 PHIV+ and 105 PHIV−) were re-recruited. For the current analyses, we used data from BL, FU1, and FU2 interviews. The median time interval between the BL and FU1 was approximately 1.5 years (Myears =1.65, SD = 0.45) and the mean time interval between FU1 and FU2 interviews was 3 years (Myears = 3.06, SD = 1.42). There were minimal but statistically significant differences by HIV status in years between assessments between BL and FU1 (MPHIV− = 1.09, SD = 0.42, MPHIV+ = 1.28, SD = 0.63; t = −3.08, p = .005), and FU1 and FU2 (MPHIV− = 2.56, SD = 1.15, MPHIV+ = 3.39, SD = 1.48; t = −5.02, p < .001). HIV status and age at each follow-up were included as covariates.
Data sources included caregiver and youth interviews and medical chart data on viral load and CD4 counts. Caregivers and youth were interviewed separately in English or Spanish at the family’s home, their medical clinic, or study research offices. Institutional review board approval was obtained from all study sites and the principal investigator’s home institution. Caregivers provided written informed consent for themselves and permission for youth who were <18 years of age; youth provided written informed assent if <18 years and consent if ≥18 years. Monetary reimbursement for time and travel was provided.
Measures
Youth Characteristics
Youth HIV status was determined by youth enrollment in HIV primary care clinics and verified by clinicians. Youth demographics assessed by self-report included age, gender, and race/ethnicity.
Caregiver Characteristics
Caregiver HIV status was assessed by self-report questions about HIV tests and results (HIV infected vs. uninfected/untested). Self-reported demographics included caregiver age, gender, relationship to youth (birth or nonbirth parent), and household income. Household income was calculated in ranges (e.g., 1 = $5,000 or less; 5 = $20,000–25,000; 13 = More than $150,000).
Psychiatric Disorder
Presence (yes/no) of youth current psychiatric disorder was assessed using the Diagnostic Interview Schedule for Children-IV (DISC-IV) (Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000), a well-validated diagnostic instrument that can be administered by trained lay interviewers to assess the most common DSM disorders (American Psychiatric Association, 1994). Youth were interviewed about presence or absence of symptoms in the past year, based on diagnostic categories. The most common diagnostic statistical manual (DSM)-IV adolescent disorders were examined: (a) any behavioral disorder (attention-deficit/hyperactivity disorder, oppositional defiant disorder, conduct disorder); (b) any mood disorder (major depressive disorder, dysthymia, bipolar disorder); and (c) any anxiety disorder (social anxiety disorder, separation anxiety disorder, specific phobia, agoraphobia, panic disorder, generalized anxiety disorder, obsessive-compulsive disorder).
Marijuana Use
Youth marijuana use also was assessed using the DISC-IV, documenting how often youth reported using marijuana in the past year on a 5-point Likert-type scale: 4 = daily or almost every day, 3 = 3–4 days/week, 2 = 1–2 days/week, 1 = less than that, 0 = no use.
Youth report of marijuana use is used, as caregivers often have minimal knowledge of adolescent substance use (Williams, McDermitt, Betrand & Davis, 2003), particularly as youth age (youth’s age at FU2 was 17 [M = 17.2; SD = 2.74]). To be consistent with our use of youth-only report for marijuana use, we also use youth-only report for psychiatric diagnoses. Several studies have demonstrated the validity of using youth-only report to determine psychiatric diagnoses (Jensen et al., 1999; Ko, Wasserman, McReynolds, & Katz, 2004).
Statistical Analysis
First, BL sample characteristics and prevalence of psychiatric disorders and frequency of marijuana use across time points were examined, comparing differences by HIV status using t-tests and chi-square tests as appropriate (Table I). As PHIV+ youth were approximately 1 year older than PHIV− youth at FU2, we adjusted for age using analysis of variance when examining group differences in frequency of marijuana use at FU2. Second, cross-lagged structural equation models (SEM) were used to examine longitudinal associations between changes in marijuana use and changes in psychiatric disorders at three time points: BL (Mage = 12.58 years, SD = 2.25, range =9–16 years); FU1 (Mage = 14.01 years, SD = 2.35, range = 10–21 years); and FU2 (Mage = 17.40 years, SD = 2.79, range = 13–24 years).
Table I.
Sample Characteristics by HIV Status Among a Sample of Perinatally Exposed Youth (n = 340)
| Characteristics | PHIV+(n = 206) |
PHIV−(n = 134) |
t-test/χ2 | ||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Gender | |||||
| Male | 101 | 49.0 | 65 | 48.5 | 0.01 |
| Female | 105 | 51.0 | 69 | 51.5 | |
| Agea | 12.7 | (2.16) | 12.4 | (2.37) | −1.23 |
| Race ethnicity | |||||
| Black | 119 | 57.8 | 66 | 49.3 | 0.68 |
| Hispanic | 62 | 30.1 | 43 | 32.1 | |
| Otherb | 25 | 12.1 | 25 | 18.6 | |
| Caregiver HIV+ | 65 | 31.4 | 92 | 68.7 | 43.96** |
| Caregiver is birth parent | 75 | 36.2 | 94 | 70.2 | 36.09** |
| Caregiver employed | 59 | 30.1 | 27 | 20.9 | o2.91 |
| Household incomea,c | 5.8 | (2.88) | 5.0 | (2.49) | −2.44* |
| HIV characteristics | |||||
| CD4 counta | 605.67 | (318.4) | |||
| Viral loadd | 3.50 | (0.84) | |||
| ART | 133 | 68.7 | |||
| Any marijuana usee | |||||
| Baseline | 9 | 4.37 | 11 | 8.21 | 0.57 |
| FU1 | 16 | 7.77 | 11 | 9.65 | 0.00 |
| FU2f | 65 | 36.31 | 26 | 24.76 | 0.04 |
| Behavioral disorderse | |||||
| Baseline | 13 | 6.31 | 10 | 7.46 | 0.08 |
| FU1 | 12 | 7.27 | 9 | 7.89 | 0.04 |
| FU2 | 16 | 8.94 | 8 | 7.62 | 0.15 |
| Mood disorderse | |||||
| Baseline | 7 | 3.40 | 3 | 2.24 | 1.23 |
| FU1 | 10 | 6.06 | 6 | 5.26 | 0.08 |
| FU2 | 12 | 6.97 | 8 | 7.62 | 0.08 |
| Anxiety disorderse | |||||
| Baseline | 63 | 30.58 | 43 | 32.09 | 0.09 |
| FU1 | 35 | 21.21 | 25 | 21.93 | 0.02 |
| FU2 | 32 | 17.88 | 21 | 20.00 | 0.20 |
*p ≤ .05; **p ≤ .01.
aMean (SD).
bOther race/ethnicity category: White non-Hispanic, Caribbean English, mixed race, other non-Hispanic.
cHousehold income assessed using a 12-point scale; each point represents a $5,000 increase such that 1 = <$5,000; 2 = $5,001–$10,000; 3 = 10,001–$15,000, etc.
dlog10 mean.
eOwing to missing data, percent values are not generated based on the total for each group.
fAnalysis of variance F test controlling for age.
SEM models identified (1) autoregressive paths: relationships within marijuana use and psychiatric disorders from early to late adolescence (e.g., does early marijuana use predict later marijuana use?); and (2) cross-lagged paths: the degree to which, after accounting for earlier psychiatric disorders, changes (increase/decrease) in marijuana use predict changes (onset/remission) in later psychiatric disorders. The reciprocal nature of this model also permitted testing of the degree to which earlier changes in psychiatric disorders predict later changes in marijuana use (Kenny, 1979). For example, cross-lagged models ask whether, after accounting for frequency of marijuana use at BL, increases in marijuana use between BL and FU1 predict onset of psychiatric disorders between FU1 and FU2. The model used four cross-lagged structural paths: (1) BL marijuana use predicting onset of FU1 psychiatric disorder, (2) BL psychiatric disorder predicting changes in FU1 marijuana use, (3) changes in marijuana use between BL to FU1 predicting onset of FU2 psychiatric disorder, and (4) onset of FU2 psychiatric disorder predicting changes in marijuana use. This model was run for marijuana use with behavioral, mood, and anxiety disorders separately. Nested model comparisons identify paths that significantly account for variance in later constructs, identifying potentially causal paths.
Gender, race/ethnicity, and age were included at each time point as covariates. Analyses were conducted in M-plus (Muthén & Muthén, 1998–2010). All models were specified using maximum likelihood (ML) estimation with categorical variables specified as indicated. For each model, HIV status was examined to identify whether cross-lagged and autoregressive relationships were the same for PHIV+ and PHIV− youth using the multiple group functionality within M-plus. Unless otherwise indicated, standardized coefficients are presented.
Missing Data Analysis
Missing data were considered using ML under the assumption that data were missing at random (MAR), which permits “missingness” in data to be a function of measured covariates and outcomes. Although MAR cannot be tested, ML is robust to minor violations of this assumption. ML integrates all possible values of missing data and gives more weight to values that are more likely to occur. This approach uses all available data to identify the most likely value for missing data (Little & Rubin, 1989).
Results
Sample Characteristics
Table I presents sample BL characteristics and prevalence of marijuana use and psychiatric disorders of both PHIV+ and PHIV− youth. (For illustrative purposes, Table I includes prevalence of any past year marijuana use while SEM analyses use frequency of marijuana use.) There were no significant differences by youth HIV status in age, gender, or race/ethnicity. Families of PHIV+ youth reported slightly higher average annual income, yet the average across both groups was under the NYC poverty line for a family of four. Significantly fewer PHIV+ youth were living with a birth parent (36% vs. 70%; χ2 = 36.091, p ≤ .001), and thus, fewer PHIV+ youth were living with an HIV+ caregiver (31% vs. 69%; χ2 = 43.962, p ≤ .001), as 100% of birth mothers were PHIV+. The majority of PHIV+ youths (68.7%) were on antiretroviral therapy (ART), and yet, 65% had a viral load >400 copies/ml. At BL, 70% of PHIV+ youth had been told their HIV diagnosis; by FU1, 81% and by FU2, 96% knew their status.
There were no significant differences in prevalence of any past year marijuana use between PHIV+ and PHIV− youth at any time point, and prevalence of any past year marijuana use increased significantly over time for both groups (χ2 = 63.071, p < .001). By FU2, 36.31% of PHIV+ and 24.76% of PHIV− youth reported smoking marijuana within the past year.
Overall prevalence of behavioral disorders remained stable from BL (6.3% PHIV+ and 7.5% PHIV− youth) to FU2 (8.94% PHIV+ and 7.62% PHIV− youth), with no significant changes across time for either group (χ2 = 0.359, p = .400). Mood disorders were less common, and prevalence did not change significantly over time for either group (χ2 = 0.592, p = .569): PHIV+ (BL = 3.40%, FU2 =6.97%) and PHIV− (BL = 2.24%, FU2 = 7.62%). Rates of anxiety disorders decreased for both groups; however, this was not significant (χ2 = 1.689, p = .127). There were no differences in prevalence of psychiatric disorders by HIV status at any time point.
Cross-Sectional Associations
Frequency of marijuana use was associated with having a behavioral disorder at BL (r = .428; p = .003), FU1 (r = .512, p = .001), and FU2 (r = .710, p < .0001) and with having a mood disorder at BL (r = .255, p = .001), FU1 (r = .614, p < .0001), and FU2 (r = .607, p < .0001). Frequency of marijuana use was not significantly associated with having an anxiety disorder at BL (r = .098, p = .495), FU1 (r = .184, p = .238), or FU2 (r = .125, p = .351). Owing to the lack of cross-sectional relationships between anxiety disorders and marijuana use, cross-lagged models for anxiety disorders are not presented. Correlations presented here are polychoric owing to categorical nature of variables.
Cross-Lagged Structural Models
Before addressing reciprocal relationships between marijuana use and psychiatric disorders, we examined autoregressive paths between constructs. For each category of disorder (behavioral, mood, and anxiety), having a psychiatric disorder at BL predicted having that disorder at FU1, and having a disorder at FU1 predicted having that disorder at FU2. Similarly, earlier frequency of marijuana use predicted later use. For behavioral disorders, relationships between earlier disorders and later disorders were the same for PHIV+ and PHIV− youth. Mood disorders, however, were more stable from BL to FU1 for PHIV− youth (bBL-FU1 = 0.462) than for PHIV+ youth (bBL-FU1 =0.065, Δχ2(1) = 11.193, p = .001). Similarly, there was a stronger relationship from BL to FU1 between earlier frequency of marijuana use and later use for PHIV− youth (bBL-FU1 = 0.843) than for PHIV+ youth (bBL-FU1 = 0.417, Δχ2(1) = 11.193, p = .001).
For all SEM models, overall fit for the entire sample to determine whether separate models are needed for PHIV+ and PHIV− youth is described first. Then the relationship between frequency of marijuana use predicting onset of specific psychiatric disorders over time (Hypothesis 1) and, finally, the relationships between psychiatric disorders predicting marijuana use over time (Hypothesis 2) are described.
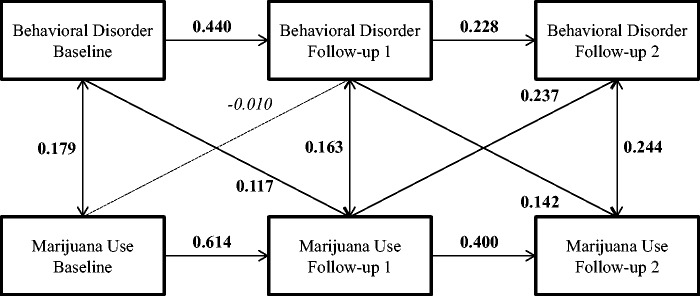
Marijuana Use and Behavioral Disorders
Because there were no group differences in the relationship between behavioral disorders and marijuana use (Δχ2 = 3.359, Δdf = 4, p = .499), the best-fitting cross-lagged paths included both PHIV+ and PHIV− adolescents (Figure 1). The cross-lagged model fit the data well (comparative fit index (CFI) = 0.981, tucker Lewis index (TLI) = 0.940). Marijuana use at BL did not predict onset of behavioral disorder between BL and FU1 (bBL-FU1 = −0.010, Δχ2 = 0.016, Δdf = 1, p = .899, 95% CI = −0.046, 0.034), but increased marijuana use from BL to FU1 predicted onset of behavioral disorder between FU1 and FU2 (bFU1-FU2 = 0.237, Δχ2 = 5.692, Δdf = 1, p = .017, R2 =6.75%). Having a behavioral disorder at BL predicted increased marijuana use from BL to FU1 (bBL-FU1 = 0.117, Δχ2 = 11.548, Δdf = 1, p < .001, R2 =5.52 %), and developing a behavioral disorder between BL and FU1 predicted increased marijuana use from FU1 to FU2 (bFU1-FU2 = 0.142, Δχ2 = 4.100, Δdf = 1, p = .043, R2 = 4.66%).
Figure 1.
Cross-lagged associations between any behavioral disorder and marijuana use. Note. Coefficients in bold are significant; coefficients in italics are not significantly different from zero (i.e., nonsignificant).
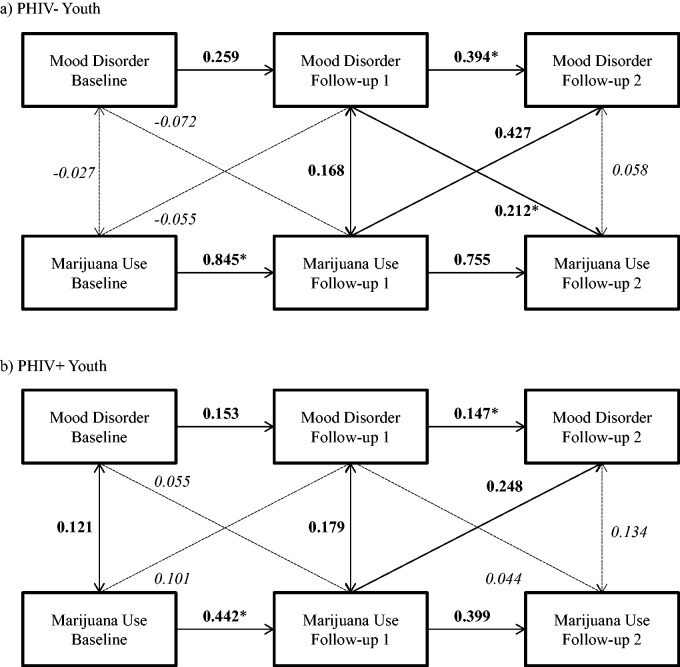
Marijuana Use and Mood Disorders
The best-fitting model was a multiple group model by HIV status, indicating that the relationship between mood disorders and marijuana use differed between PHIV+ and PHIV− youth (Δχ2 = 10.394, Δdf = 4, p = .0342). Therefore, cross-lagged paths were independently estimated by HIV status; the multiple-group cross-lagged model fit the data well (CFI = 0.961, TLI = 0.929) (Figure 2). Initial frequency of marijuana use at BL did not predict onset of a mood disorder at FU1 for PHIV− youth (bBL-FU1 = −0.055, Δχ2 = 0.692, Δdf = 1, p = .405) or for PHIV+ youth (bBL-FU1 = 0.101, Δχ2 = 0.481, Δdf = 1, p = .488). Increase in marijuana use from BL to FU1 predicted onset of a mood disorder between FU1 and FU2 for both PHIV− youth (bFU1-FU2 = 0.427, Δχ2 = 7.855, Δdf = 1, p = .005, R2 = 10.25%) and PHIV+ youth (bFU1-FU2 = 0.248, Δχ2 = 6.961, Δdf = 1, p = .008, R2 = 8.07%); this relationship was not significantly greater for PHIV− than for PHIV+ youth (Δχ2 = 0.912, Δdf = 1, p = .340). Having a mood disorder at BL was unrelated to frequency of marijuana use at FU1 for either PHIV− youth (bBL-FU1 = −0.072, Δχ2 = 0.547, Δdf = 1, p = .459) or PHIV+ youth (bBL-FU1 = 0.055, Δχ2 = 1.706, Δdf = 1, p = .192). For PHIV− youth, developing a mood disorder between BL and FU1 predicted increased marijuana use from FU1 to FU2 (bFU1-FU2 = 0.212, Δχ2 = 6.961, Δdf = 1, p = .008, R2 = 5.35%); this relationship was not significant for PHIV+ youth (bFU1-FU2 = −0.044, Δχ2 = 1.929, Δdf = 1, p = .165).
Figure 2.
Cross-lagged associations between any mood disorder and marijuana use. Note. Coefficients in bold are significant. *Denotes coefficients are significantly different by HIV status. Coefficients in italics are not significantly different from zero.
Discussion
This study is the first to examine the relationships between marijuana use and psychiatric disorders across adolescence in a sample of PHIV+ and PHIV− youth. Almost all prior studies of PHIV+ and PHIV− youth examining the link between substance use and psychiatric disorders use cross-sectional designs that preclude statements about predictive relationships or temporal priority, which are important in developing interventions. The main findings suggest that, as both PHIV+ and PHIV− youth age, increases in marijuana use predict onset of behavioral and mood disorders. The role of psychiatric disorders in predicting marijuana use differs by HIV status.
Cross-Sectional Associations
For both PHIV+ and PHIV− youth, prevalence of marijuana use more than tripled from BL to FU2, whereas prevalence of behavioral, mood, and anxiety disorders did not significantly change. Consistent with the adolescence literature, using marijuana was correlated with having a behavioral or mood disorder at each time point (Armstrong & Costello, 2002; O'Neil et al., 2011), with no differences by HIV status. Contrary to the study hypothesis, there were no correlations between marijuana use and anxiety disorders at any time point. This may be owing to the heterogeneous construct of “any anxiety disorder” in this study, which comprised specific phobia, social anxiety disorder, agoraphobia, panic disorder, generalized anxiety disorder, and obsessive-compulsive disorder, and the relationship may differ by type of anxiety disorder, warranting further investigation.
Longitudinal Relationships of Marijuana Use and Psychiatric Disorders
The presence of marijuana use at an earlier time point predicted later use for both PHIV+ and PHIV− youth; the same pattern was seen for psychiatric disorders overall. However, the degree to which earlier marijuana use is associated with later use and earlier mood disorder is associated with later mood disorder was greater for PHIV− youth. This may be owing to greater access to treatment and care and overall monitoring of PHIV+ youth (Mellins et al., 2009; Mellins & Malee, 2013) in contrast to PHIV− youth, who are typically not engaged in care systems (Gadow et al., 2012; Mellins et al., 2009).
The main goal of these analyses was to examine longitudinal, cross-lagged relationships to determine whether there were reciprocal relationships between marijuana use and psychiatric disorders over time or whether only one predicted the other, and to examine the role of HIV infection.
Marijuana Use Predicting Psychiatric Disorders
Partial support was found for the hypothesis that marijuana use would predict psychiatric disorders, but there were no HIV status differences. Specifically, although BL marijuana use by youth did not predict later onset of any psychiatric disorders examined, as the sample aged (at FU1) marijuana use predicted later behavioral and mood disorders (at FU2). This is consistent with previous studies of early adolescence (Brook et al., 2002; Patton et al., 2002) and suggests that shorter-term marijuana use by younger adolescents may not have the impact of longer-term use on psychiatric disorders seen in older adolescents (Griffith-Lendering et al., 2011). As youth age, increases in marijuana use may play a more critical role in development of later psychiatric disorders (i.e., by FU2) (Patton et al., 2002).
Psychiatric Disorders Predicting Marijuana Use
The longitudinal association between specific psychiatric disorder and marijuana use varied with disorder.
Behavioral Health Disorders. Findings supported our hypothesis that behavioral disorders predict marijuana use consistently across adolescence for both PHIV+ and PHIV− youth, consistent with a large adolescence literature (e.g., Alperen et al., 2014; Brook et al., 2002; Griffith-Lendering et al., 2011). Reasons may include self-medication of behavioral disorder symptoms (e.g., hyperactivity, feeling keyed-up) (Griffith-Lendering et al., 2011); alienation from protective systems (e.g., school, prosocial peers); and affiliation with deviant peer groups in which substance use may be the norm.
Mood Disorders. A smaller literature documents that mood disorders, particularly major depressive disorder, predict marijuana use (O'Neil et al., 2011). This association was found only for PHIV− youth once they were older: mood disorders at FU1 only predicted later marijuana use (i.e., at FU2), perhaps because more PHIV+ youth are receiving mental health treatment (Mellins et al., 2009; Mellins & Malee, 2013). Untreated mood disorders in PHIV− youth may result in marijuana use to self-medicate symptoms or may place significant strain on key protective mechanisms (e.g., parental monitoring, parent–child attachment, or peer relationships), thus increasing youths’ risk of substance use as they age. Alternatively, a third underlying variable may explain this association. A greater proportion of PHIV+ youth had a caregiver who was HIV+ and potentially ill. Caregiver illness may directly impact youth mental health and indirectly influence marijuana use by an ill caregivers' compromised ability to monitor adolescent behaviors. In either case, PHIV− youth should be targeted for psychiatric intervention while also providing psychosocial support for HIV+ caregivers as necessary.
Limitations
This study has several limitations. Participants were recruited from HIV primary care clinics, and this convenience sample may not reflect the larger population of PHIV+ and PHIV− adolescents, particularly youth living outside of NYC or PHIV+ youth not enrolled in HIV care clinics. Related, our findings do not take into account treatment services that might have been provided. Despite examining reciprocal relationships between marijuana use and psychiatric disorders, attributions about causality of these relationships must be made with caution, as the analyses are not free from potential confounds or underlying third variables. Analyses are based on frequency of marijuana use, not prevalence of marijuana use disorder (which was low); the association between marijuana use disorder and psychiatric disorders may be different and requires further examination as the sample ages. Only youth report of marijuana use and psychiatric disorders was used. While youth-only report of psychiatric diagnoses is valid (Ko et al., 2004), particularly for substance use (Williams et al., 2003), youth may under- or overreport or not recognize symptoms, particularly those of behavioral disorders such as ADHD (Salbach-Andrae, Klinkowski, Lenz, & Lehmkuhl, 2009). Chart data on psychiatric disorders, medications, and treatment that might have validated participant reports were not available to us. Finally, although retention rates were high and the analytic approach accounted for missing data based on earlier measured levels of marijuana use, psychiatric disorders, gender, race/ethnicity, age, or HIV status (Muthén & Muthén, 1998–2010), participants who missed interviews might be more likely to have developed disorders or to have used marijuana owing to factors not included in the statistical models.
Future Research and Clinical Intervention
Despite these limitations, these findings have implications for research and clinical practice. As both PHIV+ and PHIV− youth age, increases in marijuana use predict onset of behavioral and mood disorders. Further research is required to identify potential causal mechanisms and distinguish the influence of biological/neurotoxic effects of marijuana use from its psychosocial ramifications. Neuroimaging studies have described adolescence as a period of significant brain development, particularly increased myelinization in brain areas involved in emotional processing (Volkow et al., 2014). Research establishing a link between the biological effects of marijuana use on the developing brain and subsequent mental health outcomes would further elucidate how marijuana use and psychiatric disorders are associated. This research is relevant for the aging US perinatally HIV-infected population for whom the long-term CNS impact of HIV may compound the effect of marijuana use on psychiatric disorders.
For both PHIV+ and PHIV− youth, marijuana use appears to be a consistent risk factor for future psychiatric disorders. Therefore, prevention and treatment of marijuana use among younger youth may reduce development of later psychiatric disorders. Furthermore, marijuana use prevention efforts delivered in nontraditional treatment settings such as schools or community-based organizations may be more successful in reaching PHIV− youth, who may be disconnected from traditional health care or substance use treatment systems.
Behavioral disorders are a consistent predictor of marijuana use across adolescence, irrespective of HIV status. Mechanisms for this association may be direct (i.e., self-medication of symptoms) as well as indirect through increased likelihood of negative psychosocial outcomes that are in turn associated with marijuana use (e.g., school dropout, delinquent activity, and negative peer groups). Understanding which outcomes confer the greatest risk may direct efforts for reducing onset of marijuana use. Moreover, effective treatment for early behavioral disorders may prevent or mitigate risk of subsequent marijuana use.
Conclusions
Examining relationships between marijuana use and psychiatric disorders across adolescence in a sample of PHIV+ and PHIV− youth, this study found minimal impact of HIV infection, and, where HIV differences were found, PHIV− youth seem to be at greater risk. As youth age out of adolescence, they typically lose sources of clinical and psychosocial support, and this may be more likely for PHIV− youth who often are not as connected to regular health care, mental health care, or other support services as their PHIV+ counterparts. As a result, their psychiatric and psychosocial needs—and associated negative outcomes—may increase greatly as they move into early adulthood. The challenge for the field is to find these youth as they age to deliver targeted interventions and re-engage them in service systems. That said, although PHIV+ youth may be retained in support systems owing to their HIV clinical needs and thus “do better,” they must not be ignored from intervention given the significant ramifications of marijuana use and psychiatric disorders, such as unprotected sex and poor medical adherence.
Funding
This research was supported by several grants from the National Institute of Mental Health (R01MH63636, PI: C.A.M.; P30MH43520; PI: R.H.R.). Dr. K.S.E.’s effort was supported by a Career Development Award from the National Institute of Mental Health (K01MH089832, PI).
Conflicts of interest: None declared.
References
- Alperen J., Brummel S., Tassiopoulos K., Mellins C. A., Kacanek D., Smith R., Seage G. R., Moscicki A. B. (2014). Prevalence of and risk factors for substance use among perinatally Human Immunodeficiency Virus-infected and perinatally exposed but uninfected youth. Journal of Adolescent Health , 54, 341–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association. (1994). Diagnostic and Statistical Manual of Mental Disorders (4th ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- Armstrong T. D., Costello E. J. (2002). Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. Journal of Consulting and Clinical Psychology , 70, 1224–1239. [DOI] [PubMed] [Google Scholar]
- Brook D. W., Brook J. S., Zhang C., Cohen P., Whiteman M. (2002). Cannabis and anxiety: A critical review of the evidence. Archives of General Psychiatry , 59, 1039–1048. [DOI] [PubMed] [Google Scholar]
- Elkington K. S., Bauermeister J. A., Brackis-Cott E., Dolezal C., Mellins C. A. (2009). Substance use and sexual risk behaviors in perinatally Human Immunodeficiency Virus-exposed youth: Roles of caregivers, peers and HIV status. Journal of Adolescent Health , 45, 133–141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elkington K. S., Bauermeister J. A., Santamaria E. K., Dolezal C., Mellins C. A. (2015). Substance use and the development of sexual risk behaviors in youth with perinatal HIV infection. Journal of Pediatric Psychology , 40, 442–454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elkington K. S., Teplin L. A., Mericle A. A., Welty L. J., Romero E. G., Abram K. M. (2008). HIV/sexually transmitted infection risk behaviors in delinquent youth with psychiatric disorders: A longitudinal study. Journal of the American Academy of Child and Adolescent Psychiatry , 47, 901–911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fergusson D. M., Boden J. M., Horwood L. J. (2011). Structural models of the comorbidity of internalizing disorders and substance use disorders in a longitudinal birth cohort. Social Psychiatry and Psychiatric Epidemiology , 46, 933–942. [DOI] [PubMed] [Google Scholar]
- Gadow K. D., Angelidou K., Chernoff M., Williams P. L., Heston J., Hodge J., Nachman S. (2012). Longitudinal study of emerging mental health concerns in youth perinatally infected with HIV and peer comparisons. Journal of Developmental Behavioral Pediatrics , 33, 456–468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez-Scarano F., Martin-Garcia J. (2005). The neuropathogenesis of AIDS. Nature Reviews Immunology , 5, 69–81. [DOI] [PubMed] [Google Scholar]
- Griffith-Lendering M. F., Huijbregts S. C., Mooijaart A., Vollebergh W. A., Swaab H. (2011). Cannabis use and development of externalizing and internalizing behaviour problems in early adolescence: A TRAILS study. Drug and Alcohol Dependence , 116, 11–17. [DOI] [PubMed] [Google Scholar]
- Havens J. F., Mellins C. A. (2008). Psychiatric aspects of HIV/AIDS in childhood and adolescence. In Rutter M., Taylor E. (Eds.), Child and adolescent psychiatry (5th ed., pp. 945–955). Oxford, UK: Blackwell. [Google Scholar]
- Hicks P. L., Mulvey K. P., Chander G., Fleishman J. A., Josephs J. S., Korthuis P. T., Hellinger J., Gaist P., Gebo K. A.; HIV Research Network. (2007). The impact of illicit drug use and substance abuse treatment on adherence to HAART. AIDS Care , 19, 1134–1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen P. S., Rubio-Stipec M., Canino G. J., Bird H. R., Dulcan M. K., Schwab-Stone M. E., Lahey B. B. (1999). Parent and child contributions to diagnosis of mental disorder: Are both informants always necessary? Journal of the American Academy of Child and Adolescent Psychiatry , 38, 1569–1579. [DOI] [PubMed] [Google Scholar]
- Kapetanovic S., Wiegand R., Dominguez K., Blumberg D., Bohannon B., Wheeling J., Rutstein R.; LEGACY Consortium. (2011). Associations of medically documented psychiatric diagnoses and risky health behaviors in highly active antiretroviral therapy-experienced perinatally HIV-infected youth. AIDS Patient Care and STDs , 25, 493–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny D. A. (1979). Cross-lagged panel correlation: Practice and promise. Journal of Applied Psychology , 64, 372–379. [Google Scholar]
- Kessler R. (2004). The epidemiology of dual diagnosis. Biological Psychiatry , 56, 730–737. [DOI] [PubMed] [Google Scholar]
- Ko S. J., Wasserman G. A., McReynolds L. S., Katz L. (2004). Contribution of parent report to voice DISC-IV diagnosis among incarcerated youths. Journal of the American Academy of Child and Adolescent Psychiatry , 43, 868–877. [DOI] [PubMed] [Google Scholar]
- Lee M. B., Lester P., Rotheram-Borus M. J. (2002). The relationship between adjustment of mothers with HIV and their adolescent daughters. Clinical Child Psychology and Psychiatry , 7, 71–84. [Google Scholar]
- Little R. J. A., Rubin D. B. (1989). The analysis of social science data with missing values. Sociological Methods and Research , 18, 292–326. [Google Scholar]
- Mellins C. A., Brackis-Cott E., Leu C. S., Elkington K. S., Dolezal C., Wiznia A., McKay M. M., Bamji M., Abrams E. J. (2009). Rates and types of psychiatric disorders in perinatally human immunodeficiency virus-infected youth and seroreverters. Journal of Child Psychology and Psychiatry , 50, 1131–1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellins C. A., Elkington K. S., Leu C. S., Santamaria E. K., Dolezal C., Wiznia A., Bamji M., McKay M. M., Abrams E. J. (2012). Prevalence and change in psychiatric disorders among perinatally HIV-infected and HIV-exposed youth. AIDS Care , 24, 953–962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mellins C. A., Malee K. A. (2013). Understanding the mental health of youth living with perinatal HIV infection: Lessons learned and current challenges. Journal of the International AIDS Society , 16, 18593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L. K., Muthén B. O. (1998–2010). Mplus user’s guide (6th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- O'Neil K. A., Conner B. T., Kendall P. C. (2011). Internalizing disorders and substance use disorders in youth: Comorbidity, risk, temporal order, and implications for intervention. Clinical Psychology Review , 31, 104–112. [DOI] [PubMed] [Google Scholar]
- Patton G. C., Coffey C., Carlin J. B., Degenhardt L., Lynskey M., Hall W. (2002). Cannabis use and mental health in young people: Cohort study. British Medical Journal , 325, 1195–1198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rey J. M., Martin A., Krabman P. (2004). Is the party over? Cannabis and juvenile psychiatric disorder: The past 10 years. Journal of the American Academy of Child and Adolescent Psychiatry, 43, 1194–1205. [DOI] [PubMed] [Google Scholar]
- Salbach-Andrae H., Klinkowski N., Lenz K., Lehmkuhl U. (2009). Agreement between youth-reported and parent-reported psychopathology in a referred sample. European Child and Adolescent Psychiatry, 18(3), 136–143. [DOI] [PubMed] [Google Scholar]
- Shaffer D., Fisher P., Lucas C. P., Dulcan M. K., Schwab-Stone M. E. (2000). NIMH diagnostic interview schedule for children version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry , 39, 28–38. [DOI] [PubMed] [Google Scholar]
- Sharer L. R. (2005). Neuropathological aspects of HIV-1 infection in children. In Gendelman H. E., Grant I., Everall I. P., Lipton S. A., Swindells S. (Eds.), The neurology of AIDS (pp. 875–906). Oxford: Oxford University Press. [Google Scholar]
- Tassiopoulos K., Moscicki A. B., Mellins C., Kacanek D., Malee K., Allison S., Hazra R., Siberry G. K., Smith R., Paul M., Van Dyke R. B., Seage G. R. (2013). Sexual risk behavior among youth with perinatal HIV infection in the United States: Predictors and implications for intervention development. Clinical Infectious Diseases , 56, 283–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Volkow N. D., Baler R. D., Compton W. M., Weiss S. R. B. (2014). Adverse health effects of marijuana use. New England Journal of Medicine , 370, 2219–2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams P. L., Leister E., Chernoff M., Nachman S., Morse E., Di Poalo V., Gadow K. D. (2010). Substance use and its association with psychiatric symptoms in perinatally HIV-infected and HIV-affected adolescents. AIDS and Behavior , 14, 1072–1082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams R. J., McDermitt D. R., Bertrand L. D., Davis R. M. (2003). Parental awareness of adolescent substance use. Addictive Behaviors , 28, 803–809. [DOI] [PubMed] [Google Scholar]