Abstract
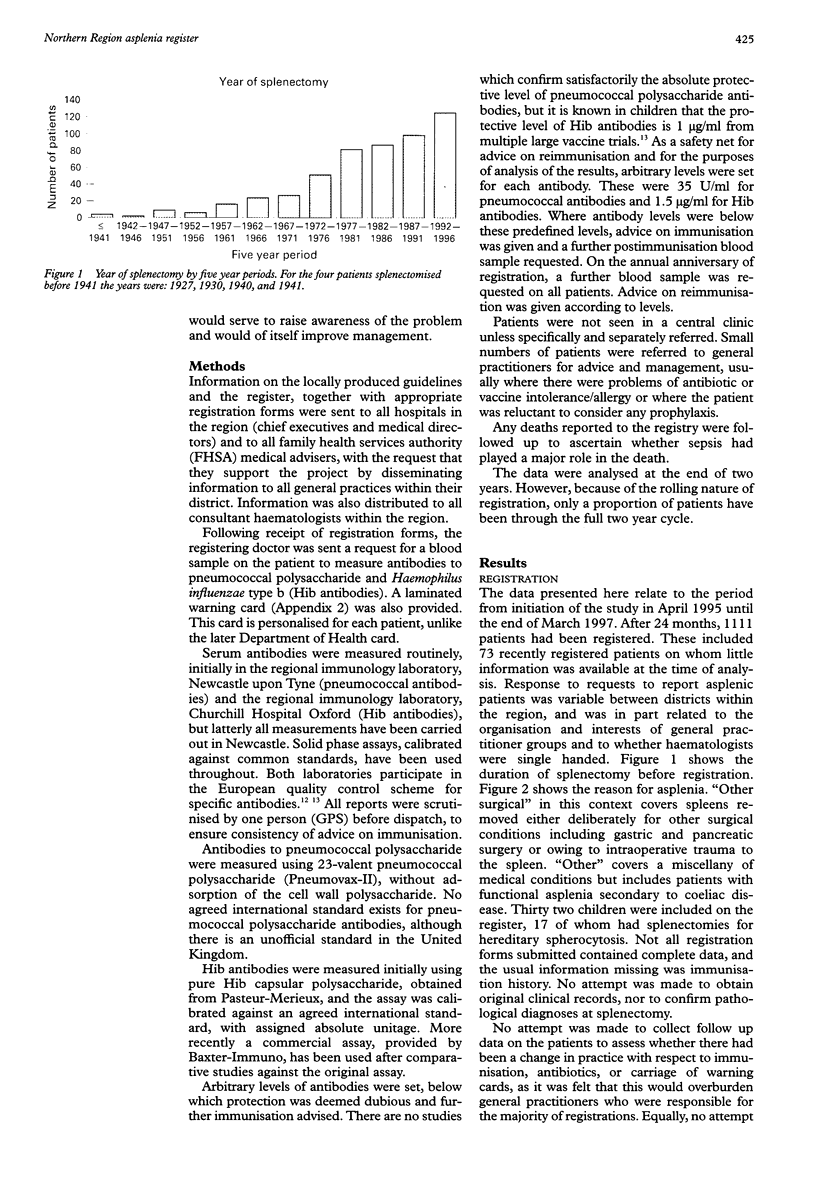
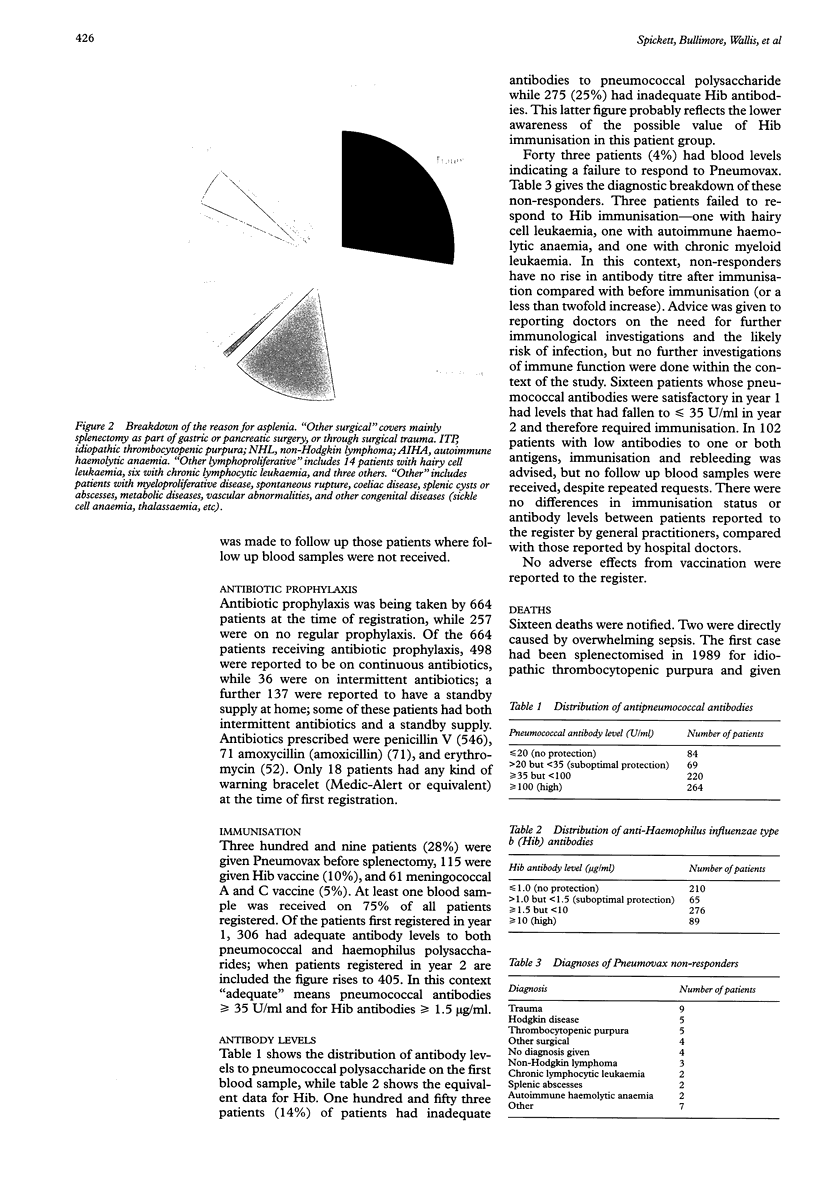
OBJECTIVES: To assess the feasibility of setting up a register of patients with asplenia within a defined geographical area; to ensure that guidelines on best practice were implemented; to obtain information on antibody levels to pneumococcal capsular polysaccharides and Haemophilus influenzae type b capsular polysaccharide, before and after immunisation and annually thereafter; to raise awareness of risks among clinicians and to offer advice on management. DESIGN: Prospective recruitment using multiple sources of recruitment. Annual follow up reminders sent from Registration Centre. SUBJECTS: Population of (old, pre-1995) Northern Health Region: approximately 3.1 million. MAIN OUTCOME MEASURES: Data were obtained on reasons for asplenia, duration of asplenia, use of prophylactic antibiotics, Medic-Alert bracelets, immunisations, antibody levels, death. RESULTS: The register was initiated at the beginning of April 1995 and ran to the end of March 1997. After two years of operation, 1111 cases had been registered but the response from some health districts was poor. Major primary causes of asplenia were trauma (264), other surgical (198), lymphoproliferative disease (154), and idiopathic thrombocytopenic purpura (147). There were 664 patients on prophylactic antibiotics, of whom 498 were on continuous antibiotics. Only 18 had any type of warning bracelet. Antibody measurements were carried out at least once on 75% of patients; 306 patients had satisfactory antibody levels on first blood sample in year 1, rising to 405 in year 2; 43 patients failed to make any antibody response to Pneumovax despite multiple immunisations, and three patients failed to respond to Hib vaccine. Sixteen patients with satisfactory antibody levels in year 1 had low levels in year 2 requiring vaccine boosters. Sixteen deaths were reported, two of which were directly attributable to overwhelming sepsis. CONCLUSIONS: Registration has been successful and has raised awareness of the management of asplenia. Compliance with antibiotic prophylaxis and immunisation was initially poor. A potential high risk group of vaccine non-responders has been identified and poor persistence of pneumococcal antibodies has been identified which is likely to alter approaches to immunisation in asplenic patients.
Full text
PDF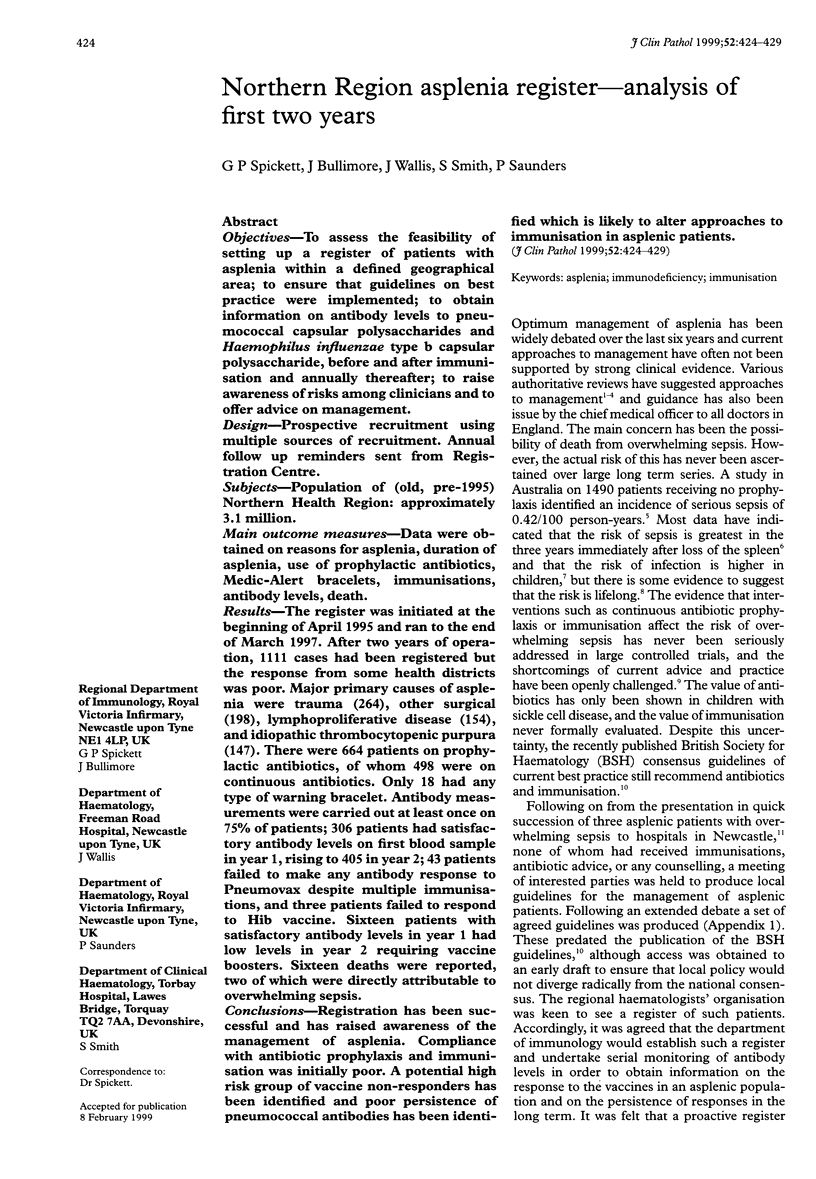


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Booy R., Taylor S. A., Dobson S. R., Isaacs D., Sleight G., Aitken S., Griffiths H., Chapel H., Mayon-White R. T., Macfarlane J. A. Immunogenicity and safety of PRP-T conjugate vaccine given according to the British accelerated immunisation schedule. Arch Dis Child. 1992 Apr;67(4):475–478. doi: 10.1136/adc.67.4.475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cullingford G. L., Watkins D. N., Watts A. D., Mallon D. F. Severe late postsplenectomy infection. Br J Surg. 1991 Jun;78(6):716–721. doi: 10.1002/bjs.1800780626. [DOI] [PubMed] [Google Scholar]
- Evans D. I. Postsplenectomy sepsis 10 years or more after operation. J Clin Pathol. 1985 Mar;38(3):309–311. doi: 10.1136/jcp.38.3.309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaines A. D., Buckley R. H. Impaired antibody response to polysaccharides in association with functional asplenia. J Pediatr. 1989 Jan;114(1):89–91. doi: 10.1016/s0022-3476(89)80607-9. [DOI] [PubMed] [Google Scholar]
- Hargreaves R. M., Lea J. R., Griffiths H., Faux J. A., Holt J. M., Reid C., Bunch C., Lee M., Chapel H. M. Immunological factors and risk of infection in plateau phase myeloma. J Clin Pathol. 1995 Mar;48(3):260–266. doi: 10.1136/jcp.48.3.260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hassan I. S., Snow M. H., Ong E. L. Overwhelming pneumoccoccal sepsis in two patients splenectomised more than ten years previously. Scott Med J. 1996 Feb;41(1):17–19. doi: 10.1177/003693309604100107. [DOI] [PubMed] [Google Scholar]
- Holdsworth R. J., Irving A. D., Cuschieri A. Postsplenectomy sepsis and its mortality rate: actual versus perceived risks. Br J Surg. 1991 Sep;78(9):1031–1038. doi: 10.1002/bjs.1800780904. [DOI] [PubMed] [Google Scholar]
- Konradsen H. B., Rasmussen C., Ejstrud P., Hansen J. B. Antibody levels against Streptococcus pneumoniae and Haemophilus influenzae type b in a population of splenectomized individuals with varying vaccination status. Epidemiol Infect. 1997 Oct;119(2):167–174. doi: 10.1017/s0950268897007978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lortan J. E. Management of asplenic patients. Br J Haematol. 1993 Aug;84(4):566–569. doi: 10.1111/j.1365-2141.1993.tb03128.x. [DOI] [PubMed] [Google Scholar]
- MacInnes J., Waghorn D. J., Haworth E. Management of asplenic patients in South Buckinghamshire: an audit of local practice. Commun Dis Rep CDR Rev. 1995 Nov 10;5(12):R173–R177. [PubMed] [Google Scholar]
- McElroy P. J., Henderson F. I., Brown D. L. Immune status and response to immunization with polysaccharide vaccines of a healthy, congenitally asplenic woman. Clin Exp Immunol. 1989 Dec;78(3):402–405. [PMC free article] [PubMed] [Google Scholar]
- McMullin M., Johnston G. Long term management of patients after splenectomy. BMJ. 1993 Nov 27;307(6916):1372–1373. doi: 10.1136/bmj.307.6916.1372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mufson M. A., Krause H. E., Schiffman G., Hughey D. F. Pneumococcal antibody levels one decade after immunization of healthy adults. Am J Med Sci. 1987 May;293(5):279–284. doi: 10.1097/00000441-198705000-00001. [DOI] [PubMed] [Google Scholar]
- Pimpl W., Dapunt O., Kaindl H., Thalhamer J. Incidence of septic and thromboembolic-related deaths after splenectomy in adults. Br J Surg. 1989 May;76(5):517–521. doi: 10.1002/bjs.1800760528. [DOI] [PubMed] [Google Scholar]
- Reid M. M. Splenectomy, sepsis, immunisation, and guidelines. Lancet. 1994 Oct 8;344(8928):970–971. doi: 10.1016/s0140-6736(94)91635-7. [DOI] [PubMed] [Google Scholar]
- Siber G. R., Gorham C., Martin P., Corkery J. C., Schiffman G. Antibody response to pretreatment immunization and post-treatment boosting with bacterial polysaccharide vaccines in patients with Hodgkin's disease. Ann Intern Med. 1986 Apr;104(4):467–475. doi: 10.7326/0003-4819-104-4-467. [DOI] [PubMed] [Google Scholar]
- Sullivan J. L., Ochs H. D., Schiffman G., Hammerschlag M. R., Miser J., Vichinsky E., Wedgwood R. J. Immune response after splenectomy. Lancet. 1978 Jan 28;1(8057):178–181. doi: 10.1016/s0140-6736(78)90612-8. [DOI] [PubMed] [Google Scholar]