Abstract
As demand for global health research training continues to grow, many universities are striving to meet the needs of trainees in a manner complementary to research priorities of the institutions hosting trainees, while also increasing capacity for conducting research. We provide an overview of the first 4 years of the Global Health Program for Fellows and Scholars, a collaboration of 20 U.S. universities and institutions spread across 36 low- and middle-income countries funded through the National Institutes of Health Fogarty International Center. We highlight many aspects of our program development that may be of interest to other multinational consortia developing global health research training programs.
Introduction
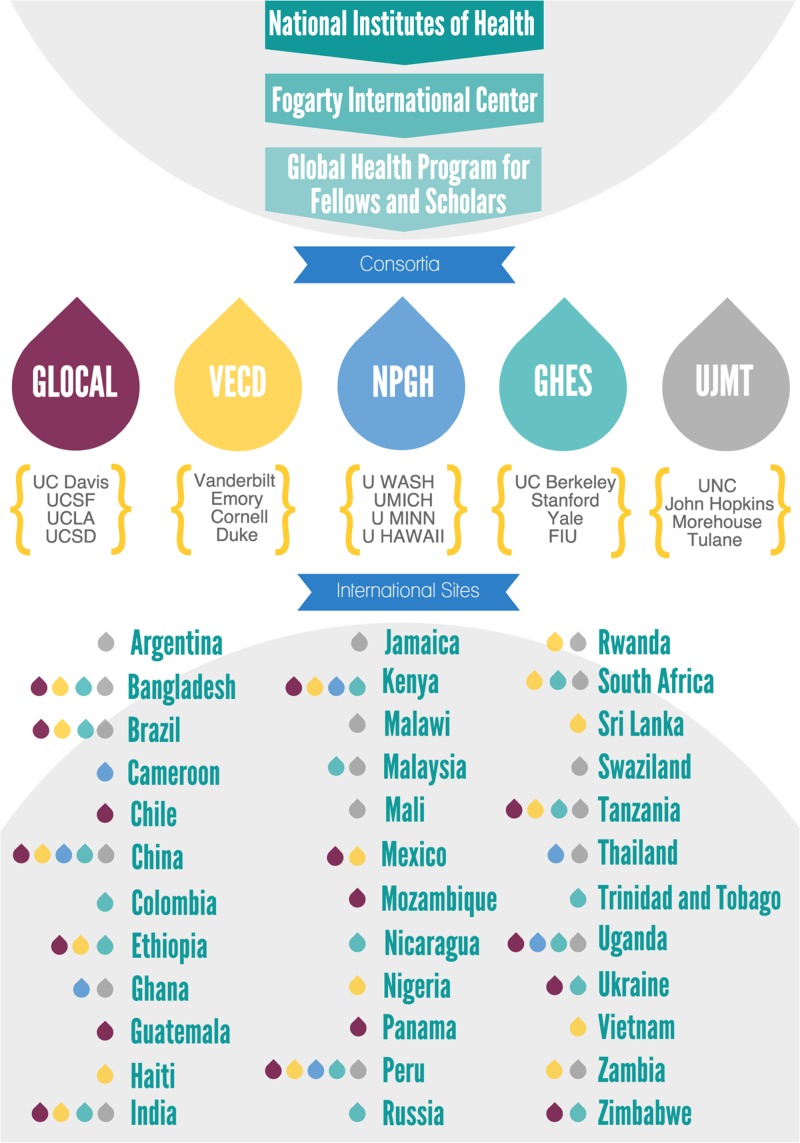
Global health research depends on mutually beneficial and respectful institutional partnerships. Demand for research training to address the myriad of health problems affecting populations living in low- and middle-income countries (LMIC) has grown considerably. In 2012, the National Institutes of Health (NIH) Fogarty International Center (FIC) awarded five grants to U.S. consortia to develop the Global Health Program for Fellows and Scholars (GHF: http://www.fic.nih.gov/Programs/pages/scholars-fellows-global-health.aspx, accessed May 18, 2016). Each consortium includes four U.S. universities with six or more international collaborating institutions per consortium. Collectively, the consortia have collaborations with 36 countries (Figure 1 ). Mentor teams are developed for each trainee that typically included mentors from the United States and the host country. Mentors from the host country often participated in the selection of trainees and identification of research topics of importance to the host country and institution. Each consortium recruits, selects, and supports U.S. and LMIC postdoctoral trainees and doctoral students for a 10- to 11-month mentored research training period at an international collaborating institution.
Figure 1.
Structure of consortia and international collaborating countries. Low- and middle-income countries affiliated with the Global Health Scholars and Fellows Program, by consortium group. FIU = Florida International University; GHES = Global Health Equity Scholars; LA = Los Angeles; MICH = Michigan; MINN = Minnesota; NPGH = Northern Pacific Global Health; SD = San Diego; SF = San Francisco; UC = University of California; UJMT = University of North Carolina, Johns Hopkins University; Morehouse School of Medicine; Tulane University; UNC = University of North Carolina at Chapel Hill; VECD = Vanderbilt, Emory, Cornell, Duke; WASH = Washington.
This GHF program accepts applications from U.S. and international postdoctorate trainees, and U.S. doctoral and professional students in health-related disciplines, including medicine, public health, dentistry, nursing, and veterinary medicine. The NIH required that 80% of trainees were at the postdoctorate level, as measured by the percentage of trainees or funding dollars, and that no more than 25% of trainees were from LMIC. The latter requirement reflects the availability of other opportunities for LMIC postdoctorates available through FIC research training and research education programs at collaborating LMIC institutions. Fellows supported by NIH research training grants (e.g., T32, D43 R25 grant mechanisms) are especially encouraged to apply. Two consortia also accept applications from junior faculty with NIH career development awards—for whom fellowships support a research project but no stipend support, with the objective of better positioning these fellows to compete for future independent funding. The initial funding opportunity announcement for the GHF program encouraged consortia to “enhance research opportunities for participants in diverse global health priority areas such as chronic noncommunicable diseases (NCDs; i.e., malignancy, cardiovascular, hematology, mental health, metabolic diseases, etc.), women's health, child health and developmental health, genetics, injury, communicable diseases including human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS), tuberculosis, malaria, and vaccine-preventable diseases.” However, during the second year of the grant, consortia were requested to prioritize HIV-related research to reflect the 80% support from AIDS-related funding streams of the program from NIH.
Between 2012 and 2015, consortia supported 316 research trainees (Supplemental Table 1). Trainees were expected to be passionate and committed to a career in global health research, and prepared to spend 10–11 months based in one of the eligible LMIC settings where they engage in a mentored research experience. They were expected to generate a product consistent with their level of training, such as data collection, one or more first-authored manuscripts and, whenever appropriate, a grant proposal to support the next step in their global health research careers. Each consortium monitored the progress and milestones of its respective trainees over the course of the year and remained engaged with alumni to track career development in academia and in global health research. In this report, we describe key program innovations and developments over the course of the current grant, providing key lessons for other multinational groups seeking to develop similar collaborative programs in global health.
Administrative Framework
Over the initial 3 years of the program, the principal investigators (PIs) and program managers of all consortia met by phone and in person on a quarterly basis to discuss logistics of developing and managing the program and to plan collaborative research training activities.
Administrative structure.
Fiscal support from NIH for administration was capped at 20% direct costs per project year and each consortium was allowed to design its own administrative structure. On average, each consortium provided partial salary support for four U.S. investigators/mentors (range 2–6) and four program support staff (range 1–7). Although compensated effort was capped, many institutions and mentors provided additional uncompensated support through centralized institutional services, for example, purchasing and services from sponsored programs' offices, through indirect funds. Although international collaborating partners did not receive salary support, their research units/departments received support ($4,000–6,000 per trainee) to offset costs of hosting trainees at their institutions and to increase or maintain research infrastructure at their institutions.
Communication: PI council.
The PI council includes the PI from each of the five U.S. consortia. To promote collaboration and sharing of responsibilities, the chair of the PI council rotated each year. Discussions during council calls and meetings focused on collaborative efforts between consortia, including standardization of recruitment, application processes, and deadlines; development of an annual cross-consortia orientation for new trainees on the NIH campus; creation of regional mentoring and research methodology training workshops; development of online programs for research training; and coordination of alumni panels at the Annual Conference of the Consortium of Universities for Global Health (CUGH), where fellow and scholar alumni present results of their research projects.
Logistical collaboration: Program managers group.
Program managers of the five consortia met quarterly via teleconference to discuss and harmonize recruitment strategies, share best practices regarding logistics of administering awards, such as transferring funds to collaborating institutions and trainees; creating research training materials; and advertising and promoting career development activities and resources for trainees and alumni. These materials were shared using cloud-based data storage and included: trainee handbooks, comprehensive safety and security briefings, presentation templates, and administrative checklists. The group also participated in workshops on the logistics and challenges of implementing international training programs at the annual Society of Research Administrators conference in October 2014.
Recruitment and application process.
Although recruitment activities varied across consortia, there were several common approaches. Consortia advertised fellowship opportunities within their home institutions to schools of health sciences, as well as to programs, centers, and institutes with global activities. PIs and codirectors made a concerted effort to broadcast the goals, expectations, and application deadline of the GHF Program across their own institutional research training and fellowship program leadership (e.g., NIH T32 research training programs) using e-mail contacts, established distribution lists, printed promotional materials, and presentations at departmental conferences and meetings. Recruitment via outside organizations such as the National Medical Association and master's and PhD career fairs were also successful and promoted diversity among the applicants. Since March 2013, CUGH was used as a yearly recruitment venue. Consortia sponsored a promotional booth in tandem with an alumni panel showcasing up to 10 U.S. and LMIC trainees, who presented research findings and shared their experiences in the field.
Over the initial years of the program, we noted an increasing number of applicants who learned of the fellowship through “word of mouth” recommendations from prior Fogarty trainees—many of whom had been appointed as faculty members at academic institutions with significant global health research and training activities. Each year, U.S. and international mentors recruited to mentor research trainees are reminded to encourage their trainees to apply for this fellowship—leading to further globalization of U.S. and international research training programs. In each of the first 4 years of this fellowship, we accepted applications between August and November, with deadlines coordinated among the consortia. Applicants may only apply to one of the five consortia, generally the one to which their home institution belongs, but some applicants have been accepted from other institutions when they proposed to train at a research site of a consortium member. This has encouraged dialogue among PIs and program managers, to ensure that prospective candidates are directed to the consortium that best matches their topical and geographic interests.
Supplemental funding from NIH institutes and centers.
Although the FIC provides financial support for the program, other NIH offices, institutes, and centers (ICs) also provide funding support through FIC. Over the years, 18 ICs and NIH Office of the Director (OD) have supported the program. Each year, NIH ICs and OD provide support for appropriate candidates with research focus relevant to specific ICs and OD. FIC encourages cofunding of applicants with research congruent with the research priorities of offices and ICs, as well as networking with intramural IC researchers. In response to FIC's advice on cofunding from other NIH ICs, the consortia developed a template to distribute standardized information regarding research interests, proposed research projects, and mentoring teams of applicants with congruent interests. To further engage IC directors and program officers, the consortia implemented a quarterly videoconference to showcase research projects of trainees across the globe.
Annual research trainee orientation at NIH.
All research trainees are expected to attend a 1-week orientation on the NIH campus. The orientation includes didactic presentations from experts in health-related disciplines, networking opportunities with NIH IC directors and program officers, skill-building sessions on research methodology, grant and paper writing, and alumni presentations and panels (Table 1). After the orientation, an evaluation survey is administered to each trainee; the PI council reviews the surveys each year and makes changes to the orientation schedule in response to trainee suggestions and critiques. Feedback from trainees has led to the expansion of predeparture safety and security briefings and incorporation of research methodology workshops.
Table 1.
Annual July orientation at the NIH for the Fogarty Global Health Fellows and Scholars Program
| Objective | Activities |
|---|---|
| Field placement planning | Logistics, including transportation, visas, timetables, communications |
| Safety, including vehicular travel and traffic, sexual assault, theft, evacuation | |
| Contingency planning and introduction to program leaders | |
| Training and skill building | Quantitative methods (epidemiology, biostatistics) and qualitative methods |
| Research design and statistical package (Stata®; StataCorp LP, College Station, TX) | |
| Introduction to mixed methods research | |
| Scientific networking | Introduction to the NIH (e.g., NIH Director, and Institute and Center directors) |
| Mentorship from alumni of Fogarty International Clinical Research Scholars and Fellows and Global Health Fellows Programs | |
| Group/individual meetings with program staff of NIH institutes, centers, and offices | |
| Team building and social interaction | Trainees room with a peer and have evening social activities |
| Ice-breaker reception, banquet, evening monument tour in Washington, DC | |
| Country-specific break-out sessions for current/former trainees and mentors | |
| Documentation and career building | Preparation of manuscripts for publication in indexed journals |
| How to present one's work briefly and succinctly (the “elevator speech”) | |
| Photography and social media address style and ethics of engagement with photo subjects | |
| Grant writing, career development awards, other NIH grants including those available to foreign citizens | |
| Current global health initiatives (examples, among many) | The U.S. President's Emergency Plan for AIDS Research |
| Scientific response to global health emergencies (e.g., Ebola virus) | |
| Scientific progress and need to extend to low- and middle-income countries (e.g., Rotavirus vaccine) |
AIDS = acquired immunodeficiency syndrome; NIH = National Institutes of Health.
Research methodology training.
After the first orientation, an optional 1-day training workshop was developed to teach core elements of epidemiological and clinical research design, principles of biostatistics, and highlight research tools, such as REDCap (Vanderbilt University, Nashville, TN) for data management as well as OpenEpi, STATA (Stata Corp., College Station, TX), and NVivo (QSR International, Melbourne, Australia) for quantitative and qualitative data analysis. More recently, the quantitative data analysis workshop was expanded to 2 days and a qualitative research methodology component was added to review core elements of formative research including focus groups, key informants, and other methods used frequently by trainees. Although brief, these workshops serve as a review or introduction to the topics, with expectations of continued learning through facilitated distance learning or self-study over the year of deployment.
Mapping research training activities.
An interactive map was created based on a MapBox template to permit users to view research sites of all five consortia (a beta version of this site can be accessed at http://tinyurl.com/p9yy39y, accessed May 19, 2016). Each research site is marked with a color-coded pin that when clicked displays names of affiliated LMIC and U.S. institutions. Each consortium is represented by a color of the pin. The description also includes a hyperlink connected to a more detailed website for each of the consortia and their partner institutions. Thus, from a single pin click, users obtain detailed information on research projects, current and past fellows and scholars, and names of PIs and LMIC mentors and collaborators. A separate drop-down menu lists all LMIC sites, and when clicked identifies where they are located on the world map.
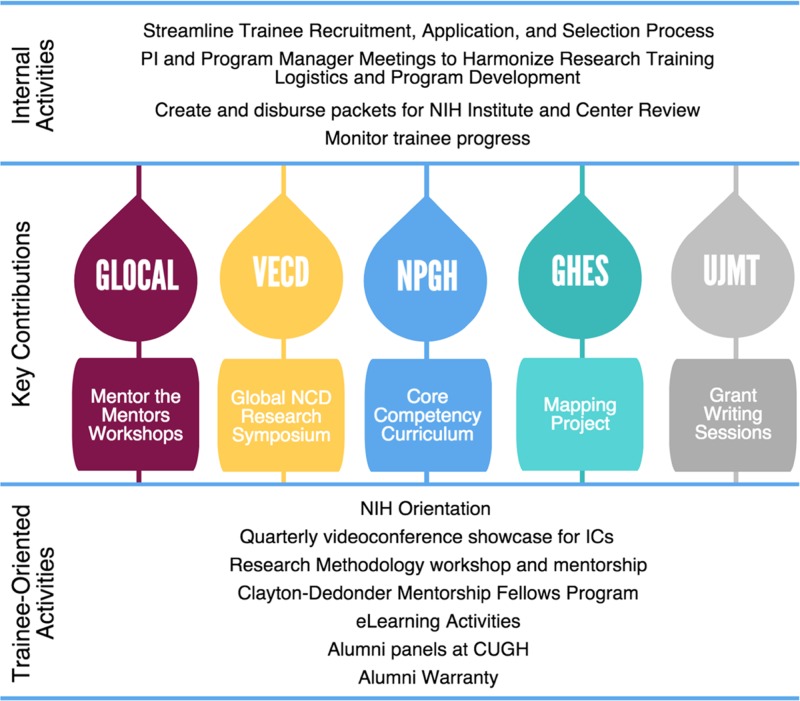
Capacity-Building Initiatives
Support of U.S. and LMIC trainees at LMIC research sites requires a robust research infrastructure at the LMIC host institution. A goal of the program is to enhance this infrastructure to benefit local and visiting trainees from the U.S. institutions. Activities that have supported enhanced capacity are detailed below (Figure 2 ).
Figure 2.
Cross-consortia research training activities. GHES = Global Health Equity Scholars; NPGH = Northern Pacific Global Health; UJMT = University of North Carolina; Johns Hopkins University; Morehouse School of Medicine; Tulane University; VECD = Vanderbilt, Emory, Cornell, Duke.
Mentorship training and support.
Although a strong mentoring network was required of consortia and their member institutions, quality of mentoring varied across institutions and countries. In an effort to enhance mentoring and standardize the approach to mentoring relationships, the consortia developed and facilitated four “Mentoring the Mentor” regional workshops in 1) Lima, Peru, for Spanish-speaking Latin American institutions (May 2013); 2) Mombasa, Kenya, for east African institutions (June 2013); 3) Bangalore, India, for south Asian institutions (November 2014); and 4) Johannesburg, South Africa, for southern African institutions (March 2016). These workshops were based on a successful approach used domestically to improve mentoring for researchers working with early-career investigators from underrepresented backgrounds.1 Each workshop included approximately 30 mid- and senior-level faculty trainees affiliated with at least one of the five consortia from each region. These programs were designed to support both local and visiting U.S. global health researchers as well as help local leaders enhance existing mentorship programs or initiate development of new programs where none existed.
Over the 2-day curriculum, workshops combined generalizable, “standard” didactic, and interactive components with more detailed training modules designed for use within the sociocultural context of the region of the world where the workshop was held. For example, workshops have included skill-based learning in 1) setting goals and expectations for the mentor–mentee relationship, 2) developing a mentoring philosophy, 3) enhancing communication strategies, identifying, and resolving challenges, and 4) creating mentor and mentee evaluation strategies.
Beginning in 2013, through FIC support, the Clayton–Dedonder Mentorship Fellows program was instituted to provide an additional year of support for LMIC alumni to assess mentorship, develop mentoring case vignettes, and initiate efforts to institutionalize mentorship training at their respective international institutions. The objectives of this innovative initiative are to 1) increase the number of global HIV/AIDS research mentors among junior- and mid-career scientists and support a network of these next-generation research mentors in LMICs, 2) incorporate established global HIV/AIDS research mentors from LMICs as mentoring supervisors for the mentorship fellows to enhance mentoring skills and career development of the mentorship fellows, and 3) strengthen mentorship activities and resources at LMIC research training institutions. In the inaugural year (2013–2014), 10 mentorship fellows from seven countries were competitively awarded—from a total of 30 applications—following an administrative review process at the FIC. The following year, an additional five fellows were supported. Advances to date have been extensive and include development of internet-based mentorship-training modules (Peru), handbooks on mentoring (Uganda), mentoring support groups for junior mentors, and fostering institutional conversations about mentoring standards and mentorship-training needs. Also, the current mentoring infrastructure at the University of Malawi College of Medicine was assessed, resulting in the development of training modules for mentors to enhance mentor–mentee interactions. At the University of the Witwatersrand in Johannesburg, South Africa, a mentor grant awardee evaluated an existing mentoring intervention to enhance graduate students' capacity to conduct research and complete their dissertation.
Competency-based curriculum for global health research.
To prepare future global health researchers, practical training in research skills is complemented with a competency-based curriculum that uses a modular, asynchronous, web-based format to reach geographically dispersed trainees. The curriculum has eight core competencies, 36 learning objectives, and 58 assignments, or “artifacts.”2 The curriculum supports and complements knowledge and skills that trainees gain through their mentored research experiences. The curriculum has been modified each year in response to trainee feedback.
Integrating eLearning activities.
To connect trainees across the world, consortia have used different commercially available internet-based platforms, including Elluminate/Blackboard Collaborate, Join.Me, GoToMeeting, and Adobe Connect. For example, 1-hour works-in-progress sessions provide a forum for three trainees to present research plans, challenges, and questions for their peers. Each presenter receives feedback from a panel of three peer trainees who have reviewed the presentations before the session, other trainees on the call and from faculty who facilitate each session. Similarly, we have used this “webinar”-based approach to focus on cultural competence, bioethics, professional development, and safety. By linking trainees and faculty from different sites and different continents, these activities provide an important forum to share experiences, broaden collaborations, and enhance engagement.
Grant-writing support.
To enhance grant-writing skills, a curriculum for grant writing targeting postdoctoral fellows was adapted from the University of North Carolina. The grant-writing course comprised two components. The first component is self-directed, with 11 recorded lectures delivered via DVD to trainees and complemented by assigned readings.3 This asynchronous approach was selected over web-based broadcasting because of its flexibility and because of the variable internet connectivity at sites. In the second component, postdoctoral fellows were divided into small groups of 3–5 members and paired with two faculty mentors. Over 6–8 Skype teleconferencing sessions, trainees developed specific aims and wrote the body of a grant application, with presentations and internal review by group members. The deliverable outputs emphasized core grant components, including a biosketch and specific aims page. The small group format was supplemented by “live” webinar lectures to facilitate discussion among all trainees. These sessions were scheduled early in the academic year; for those well positioned to complete and submit a full grant, additional support was available, including assistance in developing grant-writing timelines, internal review of grant components, and arrangement of mock reviews of a full draft with affiliated faculty.
National conferences for presentation of alumni research.
Ten U.S. and international alumni were selected from across the consortia to present research accomplishments and challenges at a Fogarty Alumni Panel integrated into the annual CUGH meetings in 2013–2016. These sessions have attracted audiences of 75–100 people and provide a valuable venue for disseminating research findings, fostering cross-consortium collaborations, recruiting future trainees, and networking.
Regional workshops and works-in-progress meetings.
Recognizing the major challenges in developing and funding a global NCD research agenda, in September 2014, a U.S. Investigators' Network Symposium on Global Non-Communicable Diseases Research was held at Emory University. Researchers representing 41 institutions, including universities, government agencies, private companies, journals, and foundations in the United States, met to discuss the challenges and identify opportunities for crafting and advancing a global NCD research agenda. Junior investigators were invited to submit abstracts reporting their NCD research. Specific action items emerged from this conference.4 As evidence of impact from the symposium, the National Institute of Diabetes and Digestive and Kidney Diseases and the National Cancer Institute subsequently issued requests for applications for NCD research, spearheaded by representatives of those institutes who participated in the symposium.
Three workshops on molecular epidemiology have been held in Brazil: one in Rio de Janeiro at the Federal Fluminense University and two in Salvador at the Oswaldo Cruz Foundation. Because the workshop held in Salvador was in its 15th year, the Ministry of Health of Brazil provided additional funding to support a 1-day symposium after the workshop in celebration of the workshop.
Measuring Outcomes
The GHF program built upon the previous Fogarty-Ellison Overseas Fellowship in Global Health and Clinical Research (2004–2007) and the Fogarty International Clinical Research Scholars and Fellows (FICRS-F) Program (2008–2012). Investment of NIH ICs into the FICRS-F program yielded substantial research productivity in the early years following the trainees' completion of support.1,5,6 Using traditional metrics of peer-reviewed publications, new academic positions and grants awarded, the impact of the GHF program has been impressive. In the first 3 years, trainees have published 871 peer-reviewed publications, 320 of which were first-authored by the trainee (Table 2). Given the typical lag between project completion and dissemination of results, we anticipate even greater productivity in the coming years. Measuring the impact of this research training program upon research capacity in the LMIC collaborating partner institutions is more complex and requires consideration of additional factors, such as new scientists and mentors trained, new technologies acquired, and institutionalization of research and mentorship-training activities. Through the collaborative framework fostered by the GHF program, the five consortia are working together to define new metrics, not only for U.S. academic trainees focused in global health, but also for the global partnerships that are critical to the advancement of science and to long-term career success of research trainees.
Table 2.
Trainee publications by year and category
| Program years | 2013 | 2014 | 2015 | First author all dates | |
|---|---|---|---|---|---|
| Fellows | 2012–2013 | 68 | 90 | 106 | 83 |
| 2013–2014 | 32 | 96 | 143 | 98 | |
| 2014–2015 | 0 | 90 | 162 | 116 | |
| Year totals | 100 | 276 | 411 | 297 | |
| Total fellow publications | 787 | ||||
| Scholars | 2012–2013 | 12 | 15 | 18 | 15 |
| 2013–2014 | 4 | 8 | 7 | 5 | |
| 2014–2015 | 0 | 5 | 15 | 3 | |
| Year totals | 16 | 28 | 40 | 23 | |
| Total scholar publications | 84 | ||||
| Fellows and scholars by calendar year | 116 | 304 | 451 | 320 | |
| Total output | 871 | ||||
Alumni warranty.
An “alumni warranty” represents the consortia's commitment to remain engaged with global health fellows and scholars after their initial training period to facilitate entry into independent careers in global health research, so they can become the next generation of global health researchers and leaders. Each consortium has handled alumni support differently, typically leveraging resources available from the participating universities. Examples of opportunities include 1) using supplementary institutional funding to extend length of stay by an additional year for trainees demonstrating exceptional research skills; 2) funding and mentoring of all alumni to present research findings at CUGH or other global health conference and prepare manuscripts for publication; 3) ongoing mentoring for U.S. and international trainees to develop proposals for new global health grants, such as Fogarty International Research Scientist Development Award K01, Emerging Global Leader Award (K43), Independent Scientist in Global Health Award K02 grants, other K awards, including Clinical and Translational Science Awards and Foundation awards; and 4) an alumni and mentor network for posting new publications, funding and job postings and opportunities to obtain career advice through consortium-sponsored alumni career luncheons at U.S. and partner international universities and CUGH Conferences, as well as list serves to all alumni.
Challenges and recommendations.
Although the GHF program has grown in scope and depth—and has been successful by many traditional metrics of academic productivity—our consortia have encountered challenges. Many trainees, for example, may benefit from additional time to complete research at the LMIC site, but our current grant mechanism limits the length of training to 11 months. A second year of support provides time to complete projects, publish research results, develop grant applications, and transition to junior faculty positions. Each consortium has been able to leverage other funding streams to support additional time overseas, including funds from other research projects, departmental funding, and other institutional training grants (e.g., NIH T32), but these opportunities have been sparse and sporadic. Although funding agencies like FIC have a portfolio of funding opportunities to support career development at various stages, opportunities for short-term “bridge” funding to build upon existing GHF investments and promote entry into the early stage of global health research are limited. Development of a mechanism to support additional training is a logical next step for programs like GHF that aim to train the next generation of globally focused academicians and researchers.
Over the course of the program, the consortia have been required to emphasize HIV-related research, to meet funding requirements of NIH with an HIV research mandate. Requiring 80% of trainees to conduct HIV-related research has limited trainees' ability to address local research priorities and to expand research capacity into areas of global health research that have been traditionally overlooked (e.g., women's health, genetics, chronic NCDs, trauma, and other surgery/anesthesia–relevant topics). Together, our consortia—under the leadership of FIC—have sought additional funding to extend global health research to support a wider variety of disciplines and areas relevant to global health, such as cofunding by ICs for individual trainees with congruent scientific interests, and leveraging funds provided by the host country and private foundations. We are hopeful that over time, the benefits of a global health research training platform addressing a wide variety of health conditions will result in greater research capacity in collaborating LMIC countries, engagement of more diverse trainees and collaborators, and a more global understanding of health that should lead to improved treatments and outcomes across the globe.
One additional benefit of diversifying trainee background is that returning postdoctorate fellows will contribute to globalization of NIH-funded T32 programs at their respective U.S. universities in a variety of disciplines not traditionally involved in global health research, such as nephrology and cardiology. This globalization will potentially lead to creation of independently funded global health research programs; programs that should be interdisciplinary by design.
Conclusions
Like its FIC-supported predecessors, the GHF program was created to meet increasing demands from health professional trainees interested in developing careers in global health research in diverse topical areas. Our goal was to build capacity for both LMIC and U.S. research trainees to conduct research in high-priority areas of importance to both HIC and LMIC through combining LMIC-based, binationally mentored research with research training and networking opportunities at the NIH orientation, followed by practical research experience in an LMIC setting.
The framework for global health research training at participating U.S. and LMIC institutions has become stronger as a direct result of harmonization of best practices, development of practical solutions across consortia, and sharing of applications, templates, and training tools. The logistical and administrative support provided by LMIC mentors and staff has been essential to the acculturation, safety, and success of trainees. The process of developing the consortia and cross-consortia activities has also strengthened development of research and mentorship-training collaborations across institutions within the United States and cross-nationally, and has led to new opportunities for LMIC trainees to become junior mentors for incoming trainees.
Strengthening international research partnerships through closer collaboration between U.S. and LMIC institutions should result in increased capacity to prepare the next generation of global health researchers and leaders at all participating institutions. One unexpected outcome of the NIH orientation has been the development of friendships that are producing new south–south collaborations. Facilitating the development of these collaborations, and institutionalization of mentorship and research training would be a laudable goal for upcoming years.
Future research training programs should consider providing competitive sources of funding for extending training for up to 2 years, transitional grants to assist promising LMIC and U.S. alumni in obtaining junior faculty appointments and independent funding, and resources to institutionalize the culture of scientific research and mentorship across collaborating institutions. Maintaining contact with geographically dispersed trainees will continue to be a challenge, but should become easier as connectivity improves across the globe.
Supplementary Material
ACKNOWLEDGMENTS
We gratefully acknowledge the leadership at the NIH Fogarty International Center who made this program possible: Roger Glass, Director; Maria ‘Mili’ Ferriera, Global Health Program Specialist; and Myat Htoo Razak, Program Officer during the inception and first 4 years of the program, and Flora Katz, current Program Officer. Without the tireless efforts of Myat Htoo Razak on behalf of our trainees—both domestic and international—none of this would have been possible.
Footnotes
Financial support: This project was supported by NIH Research Training Grants R25TW009345, R25TW009343, R25TW009337, R25TW009340, R25TW009338 funded by the Fogarty International Center, the NIH Office of the Director, (including Office of AIDS Research and Office of Research on Women's Health, Office of Behavioral and Social Sciences Research), Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Cancer Institute, National Eye Institute, National Heart, Lung, and Blood Institute, National Institute of Allergy and Infectious Diseases, National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institute of Biomedical Imaging and Bioengineering, National Institute of Dental and Craniofacial Research, National Institute of Diabetes and Digestive and Kidney Diseases, National Institute on Drug Abuse, National Institute of General Medical Sciences, National Institute of Mental Health, National Institute of Neurological Disorders and Stroke, and National Institute of Nursing Research.
Authors' addresses: Joseph R. Zunt and Nicole Hobbs, Department of Global Health, University of Washington, Seattle, WA, E-mails: jzunt@u.washington.edu and hobbsn@uw.edu. Benjamin H. Chi, Kathyrn Salisbury, and Charles van der Horst, Department of Obstetrics and Gynecology, University of North Carolina at Chapel Hill, Chapel Hill, NC, E-mails: benjamin_chi@med.unc.edu, kathryn_salisbury@med.unc.edu, and charles_vanderhorst@med.unc.edu. Douglas C. Heimburger and Sten H. Vermund, Institute for Global Health, Vanderbilt University, Nashville, TN, E-mails: douglas.heimburger@vanderbilt.edu and sten.vermund@vanderbilt.edu. Craig R. Cohen, Department of Obstetrics, Gynecology and Reproductive Services, University of California San Francisco, San Francisco, CA, and University of California Global Health Institute, San Francisco, CA, E-mail: craig.cohen@ucsf.edu. Steffanie Strathdee, Department of Medicine, University of California San Diego, San Diego, CA, E-mail: sstrathdee@ucsd.edu. Yolanda Thomas, Fogarty International Clinical Research Scholars and Fellow Program, Rambiss Consulting Group, Washington, DC, E-mail: ythomas@ficrsconsultant.com. Kimberly Bale, University of California Global Health Institute, San Francisco, CA, E-mail: kimberly.bale@ucsf.edu. Maria T. Hernandez, Division of Epidemiology, School of Public Health, University of California Berkeley, Berkeley, CA, and Division of Infectious Diseases and Vaccinology, School of Public Health, University of California Berkeley, Berkeley, CA, E-mail: maria.hernandez@berkeley.edu. Lee W. Riley, School of Public Health, University of California Berkeley, Berkeley, CA, E-mail: lwriley@berkeley.edu.
References
- 1.Gandhi M, Fernandez A, Stoff DM, Narahari S, Blank M, Fuchs J, Evans CH, Kahn JS, Johnson MO. Development and implementation of a workshop to enhance the effectiveness of mentors working with diverse mentees in HIV research. AIDS Res Hum Retroviruses. 2014;30:730–737. doi: 10.1089/aid.2014.0018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ton TG, Gladding SP, Zunt JR, John C, Nerurkar VR, Moyer CA, Hobbs N, McCoy M, Kolars JC. The development and implementation of a competency-based curriculum for training in global health research. Am J Trop Med Hyg. 2015;92:163–171. doi: 10.4269/ajtmh.14-0398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hulley SB, Cummings SR, Browner WS, Grady DG, Newman TB. Designing Clinical Research. 4th edition. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams and Wilkins; 2013. [Google Scholar]
- 4.Jaacks LM, Ali MK, Bartlett J, Bloomfield GS, Checkley W, Gaziano TA, Heimburger DC, Kishore SP, Kohler RE, Lipska KJ, Manders O, Ngaruiya C, Peck R, Pena MB, Watkins DA, Siegel KR, Narayan KM. Global noncommunicable disease research: opportunities and challenges. Ann Intern Med. 2015;163:712–714. doi: 10.7326/M15-1068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Heimburger DC, Carothers CL, Gardner P, Primack A, Warner TL, Vermund SH. Nurturing the global workforce in clinical research: the National Institutes of Health Fogarty International Clinical Scholars and Fellows Program. Am J Trop Med Hyg. 2011;85:971–978. doi: 10.4269/ajtmh.2011.11-0141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Heimburger DC, Carothers CL, Blevins M, Warner TL, Vermund SH. Impact of global health research training on scholarly productivity: the Fogarty International Clinical Research Scholars and Fellows Program. Am J Trop Med Hyg. 2015;93:1201–1207. doi: 10.4269/ajtmh.15-0432. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.