Abstract
Objectives
There has been little examination of the structural validity of the Parenting Stress Index–Short Form (PSI-SF) for minority populations in clinical contexts in the Unites States. This study aimed to test prespecified factor structures (one-factor, two-factor, and three-factor models) of the PSI-SF.
Methods
This study used confirmatory factor analysis in a sample of 240 predominantly Black and Latino caregivers of children with behavioral difficulties.
Results
The three-factor model fit was reasonable, and the criterion validity for the subscale and total scores was good supporting continued cautious use of the PSI-SF for clinical minority populations.
Conclusions
The PSI-SF could be integrated as part of screening and intake assessment procedures, which could allow social work practitioners to make more informed decisions about treatment planning, as well as facilitate conversations with caregivers around identifying sources of stress and developing healthy coping strategies.
Keywords: Parenting Stress Index–Short Form, confirmatory factor analysis, minority clinical population
Parenting stress (PS) is one of the most common concerns that parents face daily (Chang & Fine, 2007) and its impact on child rearing and children’s social adjustment is significant (Haskett, Ahern, Ward, & Allaire, 2006). PS is associated with negative parenting characteristics such as low levels of parental warmth, unhealthy parenting styles, harsh discipline, and child neglect or abuse potential (Haskett, Scott, & Ward, 2004; McPherson, Lewis, Lynn, Haskett, & Behrend, 2009; Rodriguez & Green, 1997) and has direct impacts on children’s behavior problems (Abidin, 1995; Neece, Green, & Baker, 2012). This is especially true among those residing in low-income communities, where poverty and low socioeconomic status (SES) are related to a number of stressful circumstances, including heightened neighborhood crime and violence, unemployment, and unstable housing conditions, as well as scarce protective resources that further increase both parental stress and youth behavior problems (Appleyard, Egeland, van Dulmen, & Sroufe, 2005; Burke, Loeber, & Birmaher, 2002; Luthar, 1999; McLoyd, 1998; Warner & Weist, 1996).
When children have behavioral difficulties, parenting becomes more challenging, resulting in disproportionately higher parental stress relative to other parents (Gourley, Wind, Henninger, & Chinitz, 2012). In turn, children’s behavior problems further exacerbate (Abidin, 1995), resulting in billions of dollars spent each year as youth with behavioral difficulties tend to incur extensive costs related to psychological, educational, correctional, and legal needs (Burke et al., 2002; Loeber, Burke, Lahey, Winters, & Zera, 2000). Moreover, families’ ability to seek and retain mental health treatment for their children can be impeded by significant parental stressors (Thompson et al., 2007). Parents are less motivated to seek help or have insufficient resources to comply with children’s treatment needs when there are substantial family problems (Harrison, McKay, & Bannon, 2004; Leslie, Aarons, Haine, & Hough, 2007).
Given that social work practitioners frequently work with vulnerable children and their families impacted by poverty, accurate assessment of parental stress can be useful in a number of clinical contexts focused on child mental health and parenting, such as publicly funded mental health and child welfare settings (Haskett et al., 2006). However, PS is a complex construct that involves multiple components of child and parent interaction such as behavioral, cognitive, and affective characteristics, as well as family situations (Everly & Lating, 2002). Therefore, it is important for professionals to use a reliable and valid measure of PS. The PS Index–Short Form (PSI-SF; Abidin, 1995) is one of the most common and widely used instruments of PS for clinical and research purposes (Haskett et al., 2006; Zaidman-Zait et al., 2010). However, to date, there has been little examination of the PSI-SF on minority populations in clinical contexts in the United States. Latinos, especially, have rarely been involved in validating the PSI-SF. At the same time, Latino populations are increasing rapidly and are expected to comprise 31% of the U.S. population by 2060 (U.S. Census Bureau, 2010). Therefore, this study aims to address an important gap in research by examining the psychometric properties of the PSI-SF in a sample of Black and Latino caregivers of children with behavioral difficulties.
Literature Review
The PSI consists of 120 items representing child and parent characteristics domains (101 items) and an optional stressful life events scale (19 items); the 47 items in the child domain are combined into six subscales, and the 54 items in the parent domain are combined into seven subscales (Abidin, 1995). The child domain rates child-level features including adaptability, demandingness, mood, distractibility/hyperactivity, acceptability of child to the parent, and child’s reinforcement of the parent. The parent domain assesses parental depression, attachment to the child, social isolation, sense of competence in the parenting role, relationship with spouse/parenting partner, role restrictions, and health (Abidin, 1997).
Using a series of exploratory factor analyses (EFA), the PSI-SF was developed by deriving 36 items from the long form to meet the need for a psychometrically sound but brief measure of PS (Reitman, Currier, & Stickle, 2002). Abidin’s (1995) stress model assumes that parental distress (PD), child difficulty, and parent–child dysfunctional interactions (PCDI) are the key factors contributing to PS, which further leads to negative parenting and direct influences on child behavior. The PSI-SF operationalizes these factors in the Difficult Child (DC; 12 items; e.g., “My child seems to cry or fuss more often than most children”), PD (12 items; e.g., “I often feel I cannot handle things well”), and PCDI (12 items of; e.g., “My child rarely does things for me that make me feel good”) subscales.
To date, validation of PSI-SF psychometric properties has been mostly limited to samples of parents with healthy, nonclinical children from White and African American families (Abidin, 1995; Deater-Deckard & Scarr, 1996, Haskett et al., 2006; Reitman et al., 2002), with limited support for the three-factor structure across diverse populations. For example, Deater-Deckard and Scarr (1996) assessed the factorial validity of the PSI-SF with 589 married, upper-middle class, and mostly Caucasian parents. After confirming that the three-factor structure of 36 items did not yield a good fit using confirmatory factor analyses (CFAs), the authors conducted EFA with a randomly split sample and found a well-fitting three-factor model consisting of 17 items after discarding items that cross-loaded and items with loadings <.40. Reitman, Currier, and Stickle (2002) tested one-factor, two-factor, and three-factor models using CFA with a sample of 192 parents who were mostly low-income and African American (85%). Although none of the models demonstrated a good fit, they concluded that the three-factor model was superior to the more parsimonious one- and two-factor models because the three-factor model was supported by the stronger relationship between the subscales and psychosocial and demographic measures.
Haskett, Ahern, Ward, and Allaire (2006) also used CFA and found that the three-factor model did not fit well with a sample of 185 African American (68%) and Caucasian (34%) parents. Haskett et al. then conducted EFA with the same sample and concluded that a two-factor structure fit the data better than the one-factor and three-factor structures because the two-factor structure had the fewest cross-loadings and yielded two interpretable factors: (1) PD comprised of the 12 items from the original PD scale and (2) Child rearing Stress (CS) comprised of the 24 items from the original PCDI and DC scales.
No studies on the validation of the PSI-SF were found that involved a clinical sample or that included Latino or minority populations other than African Americans in the United States. Considering the common use of the PSI-SF as a screening measure in clinical settings (Zaidman-Zait et al., 2010), it is critical to investigate the validity of the PSI-SF with a clinical minority population including Latinos who constitute the third largest proportion of individuals involved the U.S. welfare system (15.7%; Welfare Statistics, 2013). In addition, it is surprising that only a few studies have used CFA to examine the factor structure validity of the PSI-SF despite its wide and common use. CFA provides empirical tests of theory-driven and a priori factor structures and method variance (Reitman et al., 2002). Therefore, this study examined the factor structure validity of the PSI-SF in a sample of minority caregivers that includes Latino parents of children with clinical levels of behavioral difficulties. Specifically, using CFA, this study investigated which factor structure, among three prespecified factor structures (one-factor, two-factor, and three-factor), best fits the study sample data.
In addition to the three prespecified models identified in the literature, a second-order model of the PSI-SF that has not been investigated in the previous studies was examined. This second-order model is equivalent to the three-factor model, but is a conceptually different model representing the total PSI-SF score (calculated as the sum of the three subscales), which is used as an indication of total PS (see Figures 1 and 2 for the difference between the two 3-factor models). In summary, the four prespecified models to be examined are as following: (1) one-factor model with all 36 items based on the use of the total score of the full PSI-SF; (2) two-factor model with PD and the CS subscales, combining the original PCDI and DC factors into one factor consistent with the work of Haskett et al. (2006); (3) three-factor model consisting of the original three factors (Abidin, 1995; Reitman et al., 2002); and (4) second-order model.
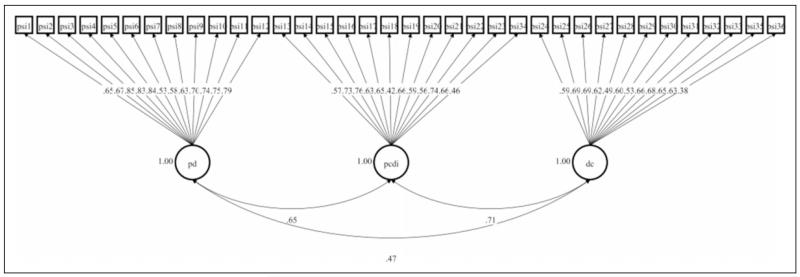
Figure 1.
Three-factor CFA model fully standardized estimates. Note. CFA = confirmatory factor analysis.
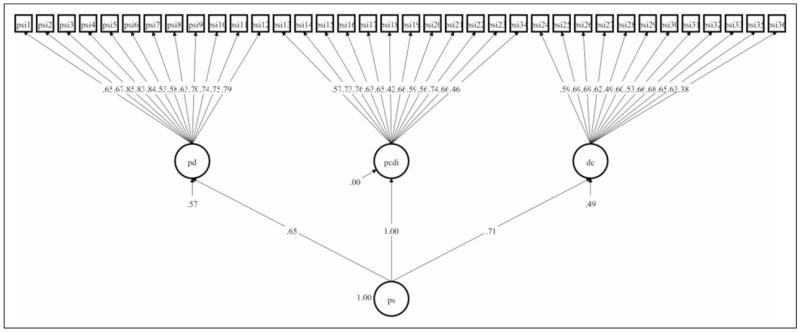
Figure 2.
Second-order factor CFA model fully standardized estimates.
Construct validity was further examined by investigating relationships between the PSI-SF with criterion measures. Abidin’s (1995) stress model earlier proposed that PS as measured by the PSI-SF has a negative impact on child behavior, causing an increase in behavioral adjustment problems. In addition, empirical studies have found that PS is linked to child behavior and parent depression. When parents demonstrated higher level of PS, they were more likely to manifest depressive symptoms and their children tended to exhibit more behavior problems (Anthony et al., 2005; Neece et al., 2012; Ross, 2013). Therefore, parent mental health and child behavior have been used as criterion constructs to examine construct validity of PS (Haskett et al., 2006; McKelvey et al., 2009; Reitman et al., 2002; Whiteside-Mansell et al., 2007). The current study specifically examined whether or not the PSI-SF demonstrates significant positive correlations with caregiver depression and child behavior.
Method
Participants and Data Source
This study used de-identified secondary data from a longitudinal, experimental study of Multiple Family Groups (MFG) and was determined to be Non-Human Subjects Research by the university institutional review board. The MFG study conducted by McKay and colleagues (Chacko et al., in press; McKay et al., 2011) was a 16-week program designed to help strengthen parenting skills and family relationships among school-aged, inner-city children with behavioral difficulties and their families. Families were recruited from 13 outpatient community-based clinics in the New York City Metropolitan area between October 2006 and October 2010 (Gopalan, Dean-Assael, Klingenstein, Chacko, & McKay, 2011). Interested families were referred to the MFG study by the clinic staffs who identified eligible families at intake. Self-administered questionnaires were used to collect data. The questionnaires included information on youth externalizing behavior, youth social skills, family support, family communication, parent–child interaction, parenting skills, PS, parent depression, and parent coping. Data were collected at five time points: (1) baseline (pre), (2) 8 weeks after starting MFG (mid), (3) 16 weeks after starting MFG (post), (4) 6 months follow-up, and (5) 18 months follow-up. Data from baseline assessments were used for this study.
The MFG study sample consisted of 320 youth and their families. Age of the youth ranged from 7 to 11 and the youth met diagnostic criteria for oppositional defiant or conduct disorders (CD). After excluding 75 cases that answered the Spanish version of the MFG assessment tools and five cases with no response across all items of the PSI-SF at baseline, data from 240 study participants were used for this study.
Sample Description
The characteristics of the sample are presented in Table 1. The total number of the sample does not sum to 240 due to missing data. The sample consisted of 235 caregivers including 204 (86.8%) mothers, 7 (3%) fathers, 1 (0.4%) participant who identified himself or herself as parent, 10 (4.2%) grandparents, and 13 (5.5%) others such as aunt and legal guardian. Almost 90% of participants were minorities consisting of African Americans (n = 96, 40.2%), Latinos (n = 98, 41%), and others such Native American and Asian (n = 16, 6.6%); only 12.1% (n = 29) were White. About 70% were single parents (n = 163, 68.8%). More than half of the participants had high school or lower level of education (n = 142, 59.6%). The level of family income was mostly low; 67.9% (n = 154) of the participants earned US$19,999 or less annually and only 8.8% (n = 20) of them earned US$40,000 or more. The age of caregivers ranged from 21 to 72 and the mean age was 36.74 (SD = 9.15). Almost 70% of their children were boys (n = 167) and the mean age was 8.86 years (range = 7–11, SD = 1.42).
Table 1.
Demographic Characteristics.
| Caregiver | Relationship with the child (N = 235) | |
|---|---|---|
| Parents (including 204 mothers, 7 fathers, and 1 parent) |
212 (90.3%) | |
| Grandparents | 10 (4.2%) | |
| Others (e.g., aunt and legal guardian) | 13 (5.5%) | |
| Race/ethnicity (N = 239) | ||
| Black/African Americans | 96 (40.2%) | |
| Latinos | 98(41.0%) | |
| White/Caucasian | 29 (12.1%) | |
| Others | 16 (6.6%) | |
| Marital status (N = 237) | ||
| Single/divorced/separated/widowed | 163 (68.8%) | |
| Married/common law marriage/domestic partnership |
70 (29.5%) | |
| Other | 4 (1.7%) | |
| Highest education level (N = 238) | ||
| Eighth grade or below | 11 (4.6%) | |
| Some/complete high school (GED) | 131 (55.0%) | |
| Some/complete college | 76 (31.9%) | |
| Graduate or above | 20 (8.4%) | |
| Family income (N = 227) | ||
| Less than $9,999 | 93 (41.0%) | |
| US$10,000–$19,999 | 61 (26.9%) | |
| US$20,000–$29,999 | 30 (13.2%) | |
| US$30,000–$39,999 | 23 (10.1%) | |
| US$40,000 and above | 20 (8.8%) | |
| Child | Gender (N = 239) | |
| Boys | 167 (69.9%) | |
| Girls | 72 (30.1%) |
Note. GED = general equivalency diploma.
Measures
PSI-SF
The PSI-SF (Abidin, 1995) is designed to assess PS in the parent–child system and to identify families most in need of follow-up services. Parents with children aged 12 years and younger report on 36 items. Thirty-three items use response options of 1 (strongly disagree) to 5 (strongly agree); the other 3 items have different response options. One item has response options of not very good at being a parent, a person who has some trouble being a parent, an average parent, a better than average parent, to a very good parent. Another item had choices of 10 and plus, 8–9, 6–7, 4–5, and 1–3. Choices for the third non-Likert-type item are much harder, somewhat harder, about as hard as, somewhat easier, to much easier. The PSF-SF is divided into three subscales of 12 items each: (1) PD, (2) PCDI, and (3) DC. The PD subscale captures parents’ level of distress related to conflicts with a partner, social support, and stresses resulting from life restrictions due to child rearing. The PCDI subscale reflects parents’ dissatisfaction about interaction with their children and parents’ perception of their children compared to other children. The DC subscale assesses parents’ perception of their children’s self-regulatory abilities such as temperament, defiance, non-compliance, and demandingness. Scores can be calculated separately for the three subscales by summing scores of the 12 items on each subscale, with possible scores ranging from 12 to 60. A total score is calculated by summing the three subscale scores, with possible scores ranging from 36 to 180. Higher scores indicate higher levels of PS.
Cronbach’s α is the most frequently used internal consistency reliability statistic for composite measures (Whiteside-Mansell et al., 2007). Abidin (1995) reported an α of .91 for the PSI-SF, .87 for PD, .80 for PCDI, and .85 for DC; test–retest correlations after 6 months ranged from .68 to .85. Reitman et al. (2002) reported αs of .95 for the PSI-SF, .88 for PD, .88 for PCDI, and .89 for DC. Haskett et al. (2006) reported αs of .83 for the PSI-SF, .78 for PD, and .91 for CS. We also found similarly high internal consistencies in the current study: .92 for the PSI-SF, .89 for PD, .82 for PCDI, and .83 for DC.
The Center for Epidemiologic Studies Depression (CES-D) Scale
Caregiver depression was assessed with the CES-D (Radloff, 1977), a 20-item self-report measure that does not indicate a diagnosis of clinical depression but distinguishes depressed from nondepressed patients (Ross, Mirowsky, & Huber, 1983). Respondents use scales ranging from 0 (none of the time) to 3 (most/all of the time) to indicate the amount of time having a particular depressive symptom in the past week. Higher scores mean more depressive symptoms. Good internal consistency reliabilities have been reported ranging from .75 to .89 (McKelvey et al., 2009; Whiteside-Mansell et al., 2007) and α = .90 in the current study.
The Inattention/Overactivity with Aggression (IOWA) Rating Scale
Child externalizing behavior was measured with the IOWA (Loney & Milich, 1982), which was developed by Loney and Milich (1982) based on the brief Conners’ Teacher Rating Scale (Waschbusch & Willoughby, 2008). The IOWA consists of 10 items and two subscales, inattention–impulsivity–overactivity (IO) and oppositional defiance (OD), with 5 items for each subscale (Waschbusch & Willoughby, 2008). Parents report on scales ranging from 0 (not at all) to 3 (very much) about their children’s disruptive behavior problems. Higher summed scores indicate greater severity of symptoms. Each subscale has good reliability ranging from .86 to .91 (Waschbusch & Willoughby, 2008) and α = .80 for each subscale in the current study.
Data Analysis
Statistical Software for the Social Sciences 18.0 was used for data cleaning and reliability and correlation tests. Mplus 7.11 was used for CFAs with weighted least squares mean- and variance-adjusted (WLSMV). WSLMV is appropriate for ordinal data with two to five categories (Schmitt, 2011) and where violations of normality occur (Muthén & Kaplan, 1985). As noted earlier, 33 of the 36 items use Likert-type responses, but 3 items use different response options. In addition, analysis of the distributions of items indicated violations of normality across all 36 items, although skewness and kurtosis indices for the items were in the acceptable ranges (Kline, 2011). WSLMV estimation was also used in the some of the previous studies on the validation of the PSI-SF subscales (McKelvey et al., 2009; Whiteside-Mansell et al., 2007).
When the WSLMV estimator is used, Mplus utilizes pairwise deletion for missing data. Although pairwise deletion has known limitations (Little & Rubin, 2002) and is not ideal for structural equation modeling (Kline, 2011), Asparouhov and Muthén (2010) supported the use of pairwise deletion when using the WLSMV estimator as this method uses more information than listwise deletion. Especially when the amount of missing data is minimal, pairwise deletion is acceptable (Kline, 2011). In this study, 1.5% or less of responses on each item of the PSI-SF was missing.
Multiple fit indices were examined to compare fit of the tested CFA models because they assess different aspects of model fit (Byrne, 2012). The χ2 goodness-of-fit index should not be significant when a hypothesized model is close to perfect fit (Byrne, 2012). The comparative fit index (CFI; Bentler, 1990) and Tucker–Lewis fit index (TLI; Tucker & Lewis, 1973) are the most commonly used incremental indices (Byrne, 2012). For both, a value of .95 or greater indicates a model fits the data well (Byrne, 2012). The root mean square error of approximation (RMSEA) accounts for the error of approximation in the population (Byrne, 2012). When a model has perfect fit to the data, RMSEA = 0 (Browne & Cudeck, 1993); values of .06 or less indicate good fit (Hu & Bentler, 1999) and a value of .08 indicates reasonable errors of approximation (Browne & Cudeck, 1993). In addition, for RMSEA, an upper bound on the 90% confidence interval of no greater than .10 and preferably no greater than .08 is recommended; there is reason to believe the model fit could be improved through modifications when the upper bound exceeds .08 (Hoyle, 2011).
Results
CFAs
All items for each factor in the prespecified four models loaded significantly in the expected direction (p < .001). The correlation between factors in the two-factor model was .629 (p < .001). For the three-factor model, the correlations were .654 between PD and PCDI, .434 between PD and DC, and .656 between PCDI and DC. All the correlations were significant, in the expected direction, and suggested reasonable discriminant validity among the factors.
The model fit indices are presented in Table 2 (the covariance matrix is available from the first author). Chi-square statistics were significant for all four models, suggesting areas of misfit. RMSEA indicated a poor fit (.109) for the one-factor model, mediocre fit (.087) for the two-factor model, and reasonable errors of approximation (.08) for the three-factor model and the second-order model. None of the models yielded a value of .95 or greater for the CFI and TLI, but the three-factor model had the highest value of the CFI (.86) and TLI (.85).
Table 2.
Fit Indices of CFA models.
| Three-factor modified model |
|||||||
|---|---|---|---|---|---|---|---|
| Index | One-factor | Two-factor | Three-factor | Second-order | Modification 1 | Modification 2 | Modification 3 |
| χ 2 | 2,294.649 | 1,678.331 | 1,493.64 | 1,493.64 | 1,438.737 | 1,401.212 | 1,386.711 |
| df | 594 | 593 | 591 | 591 | 590 | 589 | 588 |
| P | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 |
| RMSEA | .109 | .087 | .080 | .080 | .077 | .076 | .075 |
| RMSEA 90% CI | [.105, .114 | [.082, .092 | [.075, .085 | [.075, .085 | [.072, .083 | [.071, .081 | [.070, .080 |
| P | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 | <.001 |
| CFI | .735 | .831 | .860 | .860 | .868 | .874 | .876 |
| TLI | .719 | .821 | .850 | .850 | .859 | .865 | .867 |
Note. RMSEA = root mean square error of approximation; CI = confidence interval; CFI = comparative fit index; TLI = Tucker–Lewis fit index; CFA = confirmatory factor analysis.
Although none of the four models met all the criteria for a well-fitting model, the three-factor model and its equivalent second-order model manifested better fit indices than the one-factor and two-factor models. Therefore, the three-factor model and the second-order model were examined further. The unstandardized and standardized estimates for the three-factor model are presented in Table 3 and the fully standardized model is presented in Figure 1. The fully standardized second-order model is presented in Figure 2. The exact loading of the PCDI and the PS in the second-order model is .998 because the estimates were rounded off.
Table 3.
Unstandardized and Standardized Estimates for Three-Factor Model.
| Unstandardized |
Standardized |
|||||||
|---|---|---|---|---|---|---|---|---|
| Loadings | Estimates | SE | Est./SE | p Value | Estimates | SE | Est./SE | p Value |
| PD | ||||||||
| psi 1 | 1.0 | 00 | 999 | 999 | .65 | .04 | 16.20 | .00 |
| psi 2 | 1.03 | .08 | 12.73 | .00 | .67 | .04 | 17.08 | .00 |
| psi 3 | 1.30 | .08 | 16.46 | .00 | .85 | .02 | 37.12 | .00 |
| psi 4 | 1.27 | .08 | 15.70 | .00 | .83 | .02 | 35.03 | .00 |
| psi 5 | 1.29 | .08 | 16.80 | .00 | .84 | .02 | 35.51 | .00 |
| psi 6 | .82 | .09 | 8.75 | .00 | .53 | .05 | 10.70 | .00 |
| psi 7 | .89 | .08 | 11.05 | .00 | .58 | .04 | 13.16 | .00 |
| psi 8 | .97 | .09 | 10.97 | .00 | .63 | .05 | 13.20 | .00 |
| psi 9 | 1.07 | .09 | 12.22 | .00 | .70 | .04 | 18.59 | .00 |
| psi 10 | 1.14 | .09 | 13.05 | .00 | .74 | .03 | 21.95 | .00 |
| psi 11 | 1.16 | .08 | 14.75 | .00 | .75 | .03 | 36.06 | .00 |
| psi 12 | 1.22 | .09 | 14.39 | .00 | .79 | .03 | 25.71 | .00 |
| PCDI | ||||||||
| psi 13 | 1.0 | 00 | 999 | 999 | .57 | .04 | 13.28 | .00 |
| psi 14 | 1.27 | .10 | 12.66 | .00 | .73 | .03 | 21.26 | .00 |
| psi 15 | 1.33 | .11 | 11.75 | .00 | .76 | .03 | 23.18 | .00 |
| psi 16 | 1.10 | .12 | 9.24 | .00 | .63 | .04 | 14.37 | .00 |
| psi 17 | 1.13 | .10 | 11.72 | .00 | .65 | .05 | 14.17 | .00 |
| psi 18 | .73 | .11 | 6.43 | .00 | .42 | .06 | 7.61 | .00 |
| psi 19 | 1.16 | .10 | 11.13 | .00 | .66 | .04 | 17.87 | .00 |
| psi 20 | 1.03 | .10 | 10.29 | .00 | .59 | .04 | 13.51 | .00 |
| psi 21 | .98 | .11 | 9.12 | .00 | .56 | .05 | 12.35 | .00 |
| psi 22 | 1.32 | .10 | 13.91 | .00 | .74 | .04 | 21.46 | .00 |
| psi 23 | 1.15 | .11 | 10.80 | .00 | .66 | .04 | 16.18 | .00 |
| psi 34 | .80 | .13 | 6.34 | .00 | .46 | .06 | 8.13 | .00 |
| DC | ||||||||
| psi 24 | 1.0 | .00 | 999 | 999 | .59 | .05 | 13.25 | .00 |
| psi 25 | 1.16 | .11 | 10.69 | .00 | .69 | .05 | 14.72 | .00 |
| psi 26 | 1.16 | .10 | 11.82 | .00 | .69 | .04 | 18.17 | .00 |
| psi 27 | 1.05 | .11 | 9.61 | .00 | .62 | .04 | 14.64 | .00 |
| psi 28 | .83 | .10 | 8.35 | .00 | .49 | .05 | 9.21 | .00 |
| psi 29 | 1.0 | .09 | 10.71 | .00 | .60 | .05 | 13.21 | .00 |
| psi 30 | .89 | .10 | 9.19 | .00 | .53 | .05 | 10.39 | .00 |
| psi 31 | 1.12 | .12 | 9.67 | .00 | .67 | .05 | 14.01 | .00 |
| psi 32 | 1.16 | .11 | 10.77 | .00 | .69 | .04 | 16.14 | .00 |
| psi 33 | 1.09 | .11 | 9.67 | .00 | .65 | .05 | 13.14 | .00 |
| psi 35 | 1.06 | .10 | 10.61 | .00 | .63 | .05 | 14.02 | .00 |
| psi 36 | .64 | .11 | 5.74 | .00 | .38 | .06 | 6.11 | .00 |
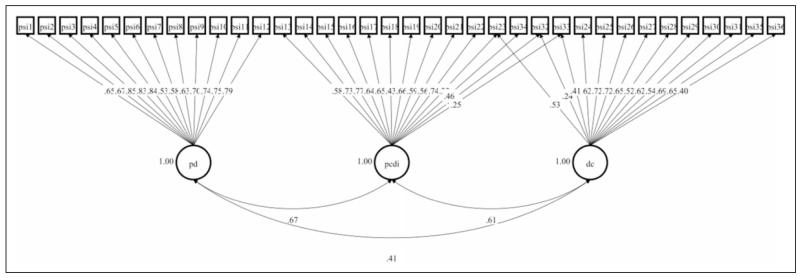
Although the model fit indices of the second-order model were equivalent to those of the three-factor model, modification to the data was conducted based on the three-factor model because it was more commonly examined in previous studies (Abidin, 1995; Reitman et al., 2002). Further, although previous studies were not clear about which items cross loaded on which factors, the studies clearly stated that there were some cross-loadings in the PSI-SF (Deater-Deckard & Scarr, 1996; Haskett et al., 2006). Therefore, only cross-loadings between items were allowed in the modification process. Further, items under the PCDI were allowed to cross-load on either the PD or the CD because the three factors originated from two domains, child and parent characteristics of the PSI. Items to cross-load were selected based on modification indices (MIs) and expected parameter change (EPC) values. Changes in fit indices at each modification are reported in Table 2. The modified model is presented in Figure 3 and the estimates were reported in Table 4.
Figure 3.
Modified three-factor model standardized estimates.
Table 4.
Unstandardized and Standardized Estimates for Modified Three-Factor Model.
| Unstandardized |
Standardized |
|||||||
|---|---|---|---|---|---|---|---|---|
| Loadings | Estimates | SE | Est./SE | p Value | Estimates | SE | Est./SE | p Value |
| PD | ||||||||
| psi 1 | 1.0 | 00 | 999 | 999 | .65 | .04 | 16.20 | .00 |
| psi 2 | 1.03 | .08 | 12.75 | .00 | .67 | .04 | 17.12 | .00 |
| psi 3 | 1.30 | .08 | 16.47 | .00 | .85 | .02 | 37.20 | .00 |
| psi 4 | 1.27 | .08 | 15.70 | .00 | .83 | .02 | 35.14 | .00 |
| psi 5 | 1.29 | .08 | 16.79 | .00 | .84 | .02 | 36.51 | .00 |
| psi 6 | .82 | .09 | 8.77 | .00 | .53 | .05 | 10.73 | .00 |
| psi 7 | .89 | .08 | 11.02 | .00 | .58 | .04 | 13.13 | .00 |
| psi 8 | .97 | .09 | 11.10 | .00 | .63 | .05 | 13.25 | .00 |
| psi 9 | 1.07 | .09 | 12.25 | .00 | .70 | .04 | 18.68 | .00 |
| psi 10 | 1.14 | .09 | 13.07 | .00 | .74 | .03 | 22.02 | .00 |
| psi 11 | 1.16 | .08 | 14.75 | .00 | .75 | .03 | 26.13 | .00 |
| psi 12 | 1.22 | .08 | 14.42 | .00 | .79 | .03 | 25.75 | .00 |
| PCDI | ||||||||
| psi 13 | 1.0 | 00 | 999 | 999 | .58 | .04 | 13.44 | .00 |
| psi 14 | 1.26 | .10 | 12.75 | .00 | .73 | .03 | 21.40 | .00 |
| psi 15 | 1.32 | .11 | 11.83 | .00 | .77 | .03 | 23.34 | .00 |
| psi 16 | 1.09 | .12 | 9.23 | .00 | .64 | .05 | 14.25 | .00 |
| psi 17 | 1.12 | .10 | 11.81 | .00 | .65 | .05 | 14.19 | .00 |
| psi 18 | .73 | .11 | 6.49 | .00 | .43 | .06 | 7.68 | .00 |
| psi 19 | 1.14 | .10 | 11.22 | .00 | .66 | .04 | 17.99 | .00 |
| psi 20 | 1.02 | .10 | 10.31 | .00 | .59 | .04 | 13.48 | .00 |
| psi 21 | .96 | .11 | 9.10 | .00 | .56 | .06 | 12.16 | .00 |
| psi 22 | 1.28 | .10 | 12.61 | .00 | .74 | .04 | 21.15 | .00 |
| psi 23 | .38 | .11 | 3.47 | .00 | .22 | .06 | 3.62 | .00 |
| psi 34 | .79 | .13 | 6.34 | .00 | .46 | .06 | 8.12 | .00 |
| psi 32 | .77 | .12 | 6.26 | .001 | .45 | .07 | 6.84 | .00 |
| psi 33 | .43 | .11 | 3.80 | .00 | .25 | .06 | 3.93 | .00 |
| DC | ||||||||
| psi 24 | 1.0 | .00 | 999 | 999 | .62 | .05 | 13.64 | .00 |
| psi 25 | 1.16 | .11 | 10.88 | .00 | .72 | .05 | 15.45 | .00 |
| psi 26 | 1.17 | .10 | 12.24 | .00 | .72 | .04 | 19.71 | .00 |
| psi 27 | 1.06 | .11 | 10.03 | .00 | .65 | .04 | 15.79 | .00 |
| psi 28 | .84 | .10 | 8.79 | .00 | .52 | .05 | 9.97 | .00 |
| psi 29 | 1.02 | .09 | 11.17 | .00 | .63 | .04 | 14.25 | .00 |
| psi 30 | .89 | .10 | 9.31 | .00 | .55 | .05 | 10.52 | .00 |
| psi 31 | 1.12 | .11 | 9.96 | .00 | .69 | .05 | 14.51 | .00 |
| psi 32 | .39 | .11 | 3.55 | .00 | .24 | .06 | 3.70 | .00 |
| psi 33 | .67 | .11 | 6.19 | .00 | .41 | .06 | 7.05 | .00 |
| psi 35 | 1.05 | .10 | 10.71 | .00 | .65 | .05 | 13.97 | .00 |
| psi 36 | .64 | .11 | 5.95 | .00 | .40 | .06 | 6.38 | .00 |
| psi 23 | .86 | .10 | 8.63 | .00 | .53 | .05 | 9.87 | .00 |
Note. PD = Parental Distress; PCDI = parent–child dysfunctional interactions.
Four modifications were examined for the three-factor model. First, Item 23 (“Sometimes my child does things that bother me just to be mean”) on PCDI was allowed to cross-load on DC (MI = 58.139, EPC = 1.082). The model demonstrated a better fit to the data than the three-factor model with a smaller, though still significant, χ2-square statistic, χ2(590) = 1438.737, p < .001; RMSEA also became smaller (.077) and the values of CFI (.868) and TLI (.859) increased, all indicating improved model fit though still not meeting criteria for a well-fitting model. Second, Item 32 (“My child turned out to be more of a problem than I had expected”) on DC was next allowed to cross-load on PCDI (MI = 39.621, EPC = .785). The value of the χ2 goodness of fit became smaller than the first modification, although it remained significant, χ2(589) = 1,401.212, p < .001; RMSEA became smaller (.076) and the values of CFI (.874) and TLI (.865) increased. In the third modification, Item 33 (“My child makes more demands on me than most children”) on DC was allowed to cross-load on PCDI (MI = 22.310, EPC = .324). The value of the χ2 goodness of fit went down to 1,386.711 (df = 588, p < .001), although it remained significant. The RMSEA decreased slightly (.075) and the upper bound of the RMSEA 90% confidence interval decreased to .08. The values of CFI (.875) and TLI (.866) improved slightly. The fourth and final modification yielded the identical RMSEA value as the one from the third modification and there was little change in other fit indices. In the third modification, although the RMSEA indicated adequate fit or reasonable errors of approximation, the other fit indices still indicated that the model did not fit the data well. Given the minimal improvement in model fit with the modifications, it was concluded that the three-factor structure without modifications fit the data as well as the modified three-factor model. Therefore, the modification process was stopped and the more parsimonious three-factor model without modifications was retained.
Tests of Criterion Validity
Relationships between the PSI-SF and criterion measures were examined based on the original three-factor model (see Table 5). The PSI-SF total score showed moderate to large (Cohen (1988): small = .10, moderate = .30, large = .50) positive relationships with the criterion measures (CES-D: r = .61, p < .01; IOWA-IO: r = .26, p < .01; IOWA-OD: r .45, p < .01). The two subscales, the PCDI and the DC, showed significant positive correlations with all the criterion measures. The PCDI showed small to moderate relationships with the CES-D (r = .44, p < .01), IOWA-IO (r = .19, p < .01), and IOWA-OD (r = .37, p < .01). The DC had moderate to large associations with the CES-D (r = .36, p < .01), IOWA-IO (r = .36, p < .01), and IOWA-OD (r = .55, p < .01). Although the PD showed a large association with the CES-D (r = .68, p < .01) and a moderate association with the IOWA-OD (r = .26, p < .01), the correlation with IOWA-IO was not significant (r = .10, p = .14).
Table 5.
Correlations Between the PSI-SFa and Criterion Measures.
| PSI-SFa |
||||
|---|---|---|---|---|
| Total Score | PD | PCDI | DC | |
| CES-D | .61** (n = 203) | .68** (n = 214) | .44** (n = 219) | .36** (n = 212) |
| IOWA-IO | .26** (n = 214) | .10 (n = 226) | .19** (n = 233) | .36** (n = 226) |
| IOWA-OD | .45** (n = 203) | .24** (n = 213) | .37** (n = 219) | .55** (n = 214) |
Note. CES-D = Center for Epidemiologic Studies Depression; IOWA = Intention/Overactivity with Aggression Rating Scale (IO = inattention–impulsivity–over-activity; OD = oppositional defiance); PCDI = Parent–Child Dysfunctional Interaction; PD = Parental Distress; DC = Difficult Child;
PSI-SF = Parenting Stress Index–Short Form. aPSI-SF is the original three-factor model without modification.
p < .05.
p <.01.
Discussion
The purpose of this study was to examine the factor and construct validity of the PSI-SF in a clinical minority population. Despite long and common use of the PSI for almost two decades followed by the development and use of the PSI-SF, there has not been a validation study of this measure that targeted a Latino or clinical population. Therefore, this study will be potentially valuable for professionals who work with minorities in clinical settings, as well as those involved in research with clinical populations.
The results of this study were consistent with previous studies that failed to find a well-fitting three-factor structure for the PSI-SF (Deater-Deckard & Scarr, 1966; Haskett et al., 2006; Reitman et al., 2002). Although it is possible that the combined sample of caregivers from different ethnicities and races in this study may have contributed to the overall limited model fit, this may suggest that the failure of a three-factor solution is likely to manifest across multiple different populations rather than specific to one sample (Haskett et al., 2006). Nonetheless, of the models tested in this study, the original three-factor model was retained for several reasons. First, the three-factor model had slightly better fit indices than the one-factor and two-factor models, contrary to Reitman and colleagues’ (2002) findings of equivalent model fit indices across the three models (one-factor, two-factor, and three-factor). Second, modifications did not substantially improve the fit of the three-factor model. Third, the correlations between the three factors were significant but less than .85, which supports discriminant validity among the subscales of the PSI-SF (Brown, 2006). And, finally, the significant positive relationships between the PSI-SF and the criterion measures (CES-D, IOWA-IO, and IOWA-OD) supported the construct validity of the PSI-SF three-factor model. Therefore, this study supports the utility of the PSI-SF three-factor structure for minority parents with children of behavior problems, including Latinos and African Americans.
The second-order three-factor model, representing the PSI-SF total score proposed by Abidin (1995), is equivalent to the three-factor model. Because these models are statistically equivalent, they both fit the data equally well. In addition, as noted previously, the PSI-SF subscale and total scores are significantly related to the criterion measures explored in this study, suggesting that both the total and subscale scores may be useful indicators of total and subtypes of PS, respectively.
Based on the previous findings that there were cross-loadings between some items of the PSI-SF (Deater-Deckard & Scarr, 1966; Haskett et al., 2006), this study allowed 3 items to cross-load during the modification process resulting in slight improvements in model fit indices. Two items under PCDI were allowed to cross-load on DC. Item 21 refers to how the child has difficulty complying with new things and Item 23 refers to difficulty of child’s self-regulation. One item under DC was allowed to cross-load on PCDI. Item 32 reflects parent’s degree of dissatisfaction with their child. The cross-loadings presented some overlap with the earlier study by Haskett et al. (2006), which suggests combining the PCDI and DC subscales into one CS subscale. This may suggest the need for further investigation in future studies.
There are some limitations that should be noted in this study. SES poses great threats to the psychometric integrity of self-report instruments (Brody, Flor, & Gibson, 1999; Gutman & Eccles, 1999), as lower education and literacy levels may impact self-report responses on the PSI-SF. In addition, the minority group in this study included about 35% of caregivers who were bilingual. Specifically, these caregivers used Spanish or a second language other than English, which may suggest that their English literacy level could further vary. As a result, it is possible that errors in self-reporting may have occurred, as some caregivers may not have fully understood all the items. Although such a situation could lead to less than ideal fitting CFA models, the findings in this study that the model fit reasonably well may suggest the possible use of the three-factor model of the PSI-SF among bilingual and low-SES individuals in practice and research settings.
The available sample size also created some limitations in the current study. Cabrera-Nguyen (2010) suggested one rule to calculate appropriate sample size for factor analyses, which is a person-to-item ratio of 10:1. Although this rule of thumb has been criticized by researchers because it cannot be determined without knowing the features of the gathered data (Cabrera-Nguyen, 2010), the interpretation of CFA results in the current study should take the relatively small sample size into account, given the number of items of the PSI-SF (n = 36). In addition, there are some suggestions to be explored in future studies that this study could not address due to the limited sample size.
Our study sample is likely to be representative of urban low-income predominantly single-parent families, including mostly mothers and more grandparents and legal guardians than fathers as primary caregivers (Fantuzzo, McWayne, Perry, & Childs, 2004). The study findings were consistent with the previous study that had only low-income mothers (Reitman et al., 2002). However, it would be informative to compare PSI-SF models between mothers and fathers of children with disruptive behaviors because mothers demonstrate higher PS than fathers when they have chronically ill children (Frank et al., 1991; Hauenstein, 1990). In terms of child gender distribution, more boys than girls were in the current sample, which has also been reported in previous studies on the PSI-SF validation (Deater-Deckard & Scarr, 1996; Haskett et al., 2006; Reitman et al., 2002). The current study’s sample is likely to be representative of children with disruptive behavior because boys tend to demonstrate more disruptive behaviors than girls in general (Lahey et al., 2000; Loeber et al., 2000). In an initial test of possible gender differences, we examined the fit of the three-factor model for the subsample of boys in the current study; fit indices of the three-factor model were very similar to those found for the full sample (RMSEA = .077; CFI = .87; TLI = .862), suggesting child gender may not have a large effect on the model. However, our sample of boys was small and further study is needed.
In addition, parenting is influenced by cultures that exist within larger ethnicity categories (Deater-Deckard, Dodge, Bates, & Pettit, 1996; Varela et al., 2004). Although this study extended the utility of the PSI-SF to Latino caregivers by including a significant number of Latinos in the study sample, we did not have a sufficiently large sample size to test a model for Latinos only nor were we able to examine diversity within the Latino population. Future studies with a larger sample of Latino parents are needed to more fully examine the utility of the PSI-SF within this population.
As an additional limitation, nonrandom sampling weakens generalizability of the findings to the target population, which is a clinical minority population. It is unknown whether or not there is a difference between the study participants and nonparticipants who refused to participate. Consequently, findings should be interpreted cautiously when generalizing to other populations. Nonetheless, the use of the CFA method to examine prespecified models of the PSI-SF is an important strength of this study. To date, CFA has been rarely used in validation studies of the PSI-SF. This study also extended utility of the PSI-SF in a new population by examining the psychometric properties for a clinical minority population.
Discussion and Implications to Social Work
Although the three-factor model was retained as the best fitting model in this study, consistent with prior research, this model does not meet the criteria for a well-fitting model, suggesting that further research is needed on the factor structure of the PSI-SF. However, the three-factor model fit was reasonable and the criterion validity for the subscale and total scores was good supporting continued cautious use of the PSI-SF. For example, the PSI-SF may be a useful screening measure in settings that serve children with behavioral difficulties, such as child welfare and child mental health contexts. Child behavioral difficulties are more prevalent in low-income communities compared to nationwide estimates (Angold & Costello, 2001; Gorman-Smith, Tolan, Henry, & Florsheim, 2000; Rowe, Maughan, Pickles, Costello, & Angold, 2002). Moreover, they are among the most common mental health referrals (Frick, 1998; Frick & Muñoz, 2006). In addition, children involved in the child welfare system manifest disproportionately higher rates of behavioral difficulties than children in the general population (Burns et al., 2004; Casanueva, Ringeisen, Wilson, Smith, & Dolan, 2011). Consequently, high parental stress is likely to coincide with high rates of child behavioral difficulties, with implications for treatment prognosis and future maltreatment if parental stress is not appropriately addressed. The PSI-SF could be integrated as part of screening and intake assessment procedures, which could allow social work practitioners to make more informed decisions about treatment planning, as well as facilitate conversations with caregivers around identifying sources of stress and developing healthy coping strategies. Such conversations may uncover further treatment needs for caregivers as well.
Use of the three-factor structure, in particular, may help social work practitioners discern whether parental stress is specifically related to DC behavior, parents’ own internal feelings of distress, or interactions between parents and children. Such differentiation in sources of parental stress can be a useful decision aid for treatment planning, such that social work practitioners can use assessment results to target interventions to reduce child behavior difficulties, provide additional emotional support and coaching for parents, and/or improve the quality of interactions between parents and children. Given the high levels of stress experienced by parents whose children manifest behavioral difficulties, the validation of such a tool for low-income, Black, and Latino families may support the PSI-SF as a valuable resource for social work practitioners working with minority populations.
Acknowledgments
Funding
The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Funding for this study was obtained through R01 MH072649 (PI: McKay).
Footnotes
The content is solely the responsibility of the author and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health.
Declaration of Conflicting Interests
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Abidin RR. Parenting stress index, third edition: Professional manual. Psychological Assessment Resources; Odessa, FL: 1995. [Google Scholar]
- Abidin RR. Parenting stress index: A measure of the parent-child system. In: Zalaquett CP, Wood RJ, editors. Evaluating stress: A book of resources. Scarecrow Education; Lanham, MD: 1997. pp. 277–291. [Google Scholar]
- Angold A, Costello EJ. The epidemiology of disorders of conduct: Nosological issues and comorbidity. In: Hill J, Maughan B, editors. Conduct disorders in childhood and adolescence. Cambridge University Press; New York, NY: 2001. pp. 126–168. [Google Scholar]
- Anthony LG, Anthony BJ, Glanville DN, Naiman DQ, Waanders C, Shaffer S. The relationships between parenting stress, parenting behaviour and preschoolers’ social competence and behaviour problems in the classroom. Infant and Child Development. 2005;14:133–154. doi:10.1002/icd.385. [Google Scholar]
- Appleyard K, Egeland B, van Dulmen MHM, Sroufe LA. When more is not better: The role of cumulative risk in child behavior outcomes. Journal of Child Psychology and Psychiatry. 2005;46:235–245. doi: 10.1111/j.1469-7610.2004.00351.x. doi:10.1111/j.1469-7610.2004.00351.x. [DOI] [PubMed] [Google Scholar]
- Asparouhov T, Muthén B. Weighted least squares estimation with missing data. 2010 Retrieved from http://www.statmodel.com/downlad/GstrucMissingRevision.pdf.
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. doi:10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Brody GH, Flor DL, Gibson NM. Linking maternal efficacy beliefs, developmental goals, parenting practices, and child competence in rural single-parent African American families. Child Development. 1999;70:1197–1208. doi: 10.1111/1467-8624.00087. doi:10.1111/1467-8624.00087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown TA. Confirmatory factor analysis for applied research. Guilford Press; New York, NY: 2006. [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Sage; Newbury Park, CA: 1993. pp. 136–162. [Google Scholar]
- Burke JD, Loeber R, Birmaher B. Oppositional defiant disorder and conduct disorder: A review of the past 10 years, part II. Journal of the American Academy of Child & Adolescent Psychiatry. 2002;41:1275–1293. doi: 10.1097/00004583-200211000-00009. doi:10.1097/01.CHI.0000024839.60748.E8. [DOI] [PubMed] [Google Scholar]
- Burns BJ, Phillips SD, Wagner HR, Barth RP, Kolko DJ, Campbell Y, Landsverk J. Mental health need and access to mental health services by youth involved with child welfare: A national survey. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:960–970. doi: 10.1097/01.chi.0000127590.95585.65. doi:10.1097/01.chi.0000127590.95585.65. [DOI] [PubMed] [Google Scholar]
- Byrne BM. Structural equation modeling with Mplus: Basic concepts, applications, and programming. Routledge; New York, NY: 2012. [Google Scholar]
- Cabrera-Nguyen P. Author guidelines for reporting scale development and validation results in the Journal of the Society for Social Work and Research. Journal of the Society for Social Work and Research. 2010;1:99–103. doi:10.5243/jsswr.2010.8. [Google Scholar]
- Casanueva C, Ringeisen H, Wilson E, Smith K, Dolan M. NSCAW II baseline report: Child well-being. OPRE, Administration for Children and Families, U.S. DHHS; Washington, DC: 2011. OPRE Report #2011-27b. [Google Scholar]
- Chacko A, Gopalan G, Franco L, Dean-Assael K, Jackson J, Marcus S, McKay MM. Multiple Family Group service model for children with disruptive behavior disorders: Child outcomes at post-treatment. Journal of Emotional and Behavioral Disorders. doi: 10.1177/1063426614532690. in press. doi:10.1177/1063426614532690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang Y, Fine MA. Modeling parenting stress trajectories among low-income young mothers across the child’s second and third years: Factors accounting for stability and change. Journal of Family Psychology. 2007;21:45–59. doi: 10.1037/0893-3200.21.4.584. doi:10.1037/0893-3200.21.4.584. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. Erlbaum; Hillsdale, NJ: 1988. [Google Scholar]
- Deater-Deckard K, Dodge KA, Bates JE, Pettit GS. Physical discipline among African American and European American mothers: Links to children’s externalizing behavior. Developmental Psychology. 1996;32:1065–1072. doi:10.1037/0012-1649.32.6.1065. [Google Scholar]
- Deater-Deckard K, Scarr S. Parenting stress among dual-earner mothers and fathers: Are there gender differences? Journal of Family Psychology. 1996;10:45–59. doi:10.1037/0893-3200.10.1.45. [Google Scholar]
- Everly GS, Jr., Lating J. A personality-guided approach to the treatment of posttraumatic stress disorder. American Psychological Association; Washington, DC: 2002. [Google Scholar]
- Fantuzzo J, McWayne C, Perry MA, Childs S. Multiple dimensions of family involvement and their relations to behavioral and learning competencies for urban, low-income children. School Psychology Review. 2004;33:467–480. Retrieved from http://eportfoliocathymendoza.pbworks.com/f/Fantuzzo.pdf. [Google Scholar]
- Frank SJ, Olmstead CL, Wagner AE, Laub CC, Freeark K, Breitzer GM, Peters JM. Child illness, the parenting alliance, and the parenting stress. Journal of Pediatric Psychology. 1991;16:361–371. doi: 10.1093/jpepsy/16.3.361. doi:10.1093/jpepsy/16.3.361. [DOI] [PubMed] [Google Scholar]
- Frick PJ. Conduct disorders and severe antisocial behavior. Plenum Press; New York, NY: 1998. [Google Scholar]
- Frick PJ, Muñoz L. Oppositional defiant disorder and conduct disorder. In: Essau C, editor. Child and adolescent psychopathology: Theoretical and clinical implications. Routledge/Taylor & Francis Group; New York, NY: 2006. pp. 26–51. [Google Scholar]
- Gopalan G, Bannon W, Dean-Assael K, Fuss A, Gardner L, LaBarbera B, McKay M. Mutiple Family Groups: an engaging intervention for child welfare-involved families. Child Welfare. 2011;90:135–156. Retrieved from http://eds.b.ebscohost.com.proxy-hs.researchport.umd.edu/ehost/pdfviewer/pdfviewer?sid=934f3747-26b9-4ce1-9491-686cd5e4297f%40sessionmgr112&vid=1&hid=101. [PMC free article] [PubMed] [Google Scholar]
- Gopalan G, Dean-Assael K, Klingenstein K, Chacko A, McKay MM. Caregiver depression and youth disruptive behavior difficulties. Social Work in Mental Health. 2011;9:56–70. doi: 10.1080/15332985.2010.494528. doi:10.1080/15332985.2010.494528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorman-Smith D, Tolan PH, Henry D, Florsheim P. Patterns of family functioning and adolescent outcomes among urban African American and Mexican American families. Journal of Family Psychology. 2000;14:436–457. doi: 10.1037//0893-3200.14.3.436. doi:10.1037/0893-3200.14.3.436. [DOI] [PubMed] [Google Scholar]
- Gourley L, Wind C, Henninger EM, Chinitz S. Sensory processing difficulties, behavioral problems, and parental stress in a clinical population of young children. Journal of Child and Family Studies. 2012;22:912–921. doi: 10.1007/s10826-012-9650-9. doi:10.1007/s10826-012-9650-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutman LM, Eccles JS. Financial strain, parenting behaviors, and adolescents’ achievement: Testing model equivalence between African American and European American single- and two-parent families. Child Development. 1999;70:1464–1476. doi: 10.1111/1467-8624.00106. doi:10.1111/1467-8624.00106. [DOI] [PubMed] [Google Scholar]
- Harrison ME, McKay MM, Bannon WM., Jr. Innercity child mental health service use: The real question is why youth and families do not use services. Community Mental Health Journal. 2004;40:119–131. doi: 10.1023/b:comh.0000022732.80714.8b. doi:10.1023/B:COMH.0000022732.80714.8b. [DOI] [PubMed] [Google Scholar]
- Haskett ME, Ahern LS, Ward CS, Allaire JC. Factor structure and validity of the parenting stress index-short form. Journal of Clinical Child and Adolescent Psychology. 2006;35:302–312. doi: 10.1207/s15374424jccp3502_14. doi:10.1207/s15374424jccp3502_14. [DOI] [PubMed] [Google Scholar]
- Haskett ME, Scott S, Ward C. Subgroups of physically abusive parents based on cluster analysis of parenting behavior and affect. American Journal of Orthopsychiatry. 2004;74:436–447. doi: 10.1037/0002-9432.74.4.436. doi:10.1037/0002-9432.74.4.436. [DOI] [PubMed] [Google Scholar]
- Hauenstein EJ. The experience of distress in parents of chronically ill children: Potential or likely outcome? Journal of Clinical Child Psychology. 1990;19:356–364. Retrieved from http://eds.b.ebscohost.com.proxy-hs.researchport.umd.edu/ehost/pdfviewer/pdfviewer?sid=e8afc989-7eef-4b35-a3c6-1793aadd059e%40sessionmgr115&vid=1&hid=101. [Google Scholar]
- Hoyle RH. Structural equation modeling for social and personality psychology. Sage; Thousand Oaks, CA: 2011. [Google Scholar]
- Hu L-T, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternative. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 3rd ed. The Guilford Press; New York, NY: 2011. [Google Scholar]
- Lahey BB, Schwab-Stone M, Goodman SH, Waldman ID, Canino G, Rathouz PJ, Jensen PS. Age and gender differences in oppositional behavior and conduct problems: A cross-sectional household study of middle childhood and adolescence. Journal of Abnormal Psychology. 2000;109:488–503. doi:10.1037/0021-843X.109.3.488. [PubMed] [Google Scholar]
- Leslie LK, Aarons GA, Haine RA, Hough RL. Caregiver depression and medication use by youths with ADHD who receive services in the public sector. Psychiatric Services. 2007;58:131–134. doi: 10.1176/ps.2007.58.1.131. doi:10.1176/appi.ps.58.1.131. [DOI] [PubMed] [Google Scholar]
- Little RJ, Rubin DB. Statistical analysis with missing data. 2nd ed. John Wiley; New York, NY: 2002. [Google Scholar]
- Loeber R, Burke JD, Lahey BB, Winters A, Zera M. Oppositional defiant and conduct disorder: a review of the past 10 years, part I. Journal of the American Academy of Child & Adolescent Psychiatry. 2000;39:1468–1484. doi: 10.1097/00004583-200012000-00007. doi:10.1097/00004583-200012000-00007. [DOI] [PubMed] [Google Scholar]
- Loney J, Milich R. Hyperactivity, inattention, and aggression in clinical practice. In: Wolraich M, Routh D, editors. Advances in developmental and behavioral pediatrics. Vol. 3. JAI; Greenwich, CT: 1982. pp. 134–147. [Google Scholar]
- Luthar SS. Poverty and children’s adjustment. Sage; Thousand Oaks, CA: 1999. [Google Scholar]
- McKay MM, Gopalan G, Franco L, Dean-Assael K, Chacko A, Jackson J, Fuss A. A collaboratively designed child mental health service model: Multiple Family Groups for urban children with conduct difficulties. Research on Social Work Practice. 2011;21:664–674. doi: 10.1177/1049731511406740. doi:10.1177/1049731511406740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKelvey LM, Whiteside-Mansell L, Faldowski RA, Shears J, Ayoub C, Hart AD. Validity of the short form of the Parenting Stress Index of fathers of toddlers. Journal of Children and Family Studies. 2009;18:102–111. doi:10.1007/s10826-008-9211-4. [Google Scholar]
- McLoyd VC. Socioeconomic disadvantage and child development. American Psychologist. 1998;53:184–204. doi: 10.1037//0003-066x.53.2.185. doi:10.1037/0003-066X.53.2.185. [DOI] [PubMed] [Google Scholar]
- McPherson AV, Lewis KM, Lynn AE, Haskett ME, Behrend TS. Predictors of parenting stress for abusive and nonabusive mothers. Journal of Children and Family Studies. 2009;18:61–69. doi:10.1007/s10826-008-9207-0. [Google Scholar]
- Muthén B, Kaplan D. A comparison of some methodologies for the factor analysis of non-normal Likert variables. British Journal of Mathematical and Statistical Psychology. 1985;38:171–189. doi:10.1111/j.2044-8317.1985.tb00832.x. [Google Scholar]
- Neece CL, Green SA, Baker BL. Parenting stress and child behavior problems: A transactional relationship across time. American Journal on Intellectual and Developmental Disabilities. 2012;117:48–66. doi: 10.1352/1944-7558-117.1.48. doi:10.1352/1944-7558-117.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Reitman D, Currier RO, Stickle TR. A critical evaluation of the Parenting Stress Index-Short-Form (PSI-SF) in a head start population. Journal of Clinical Child and Adolescent Psychology. 2002;31:384–392. doi: 10.1207/S15374424JCCP3103_10. doi:10.1207/S15374424JCCP3103_10. [DOI] [PubMed] [Google Scholar]
- Rodriguez CM, Green AJ. Parenting stress and anger expression as predictors of child abuse potential. Child Abuse & Neglect. 1997;21:367–377. doi: 10.1016/s0145-2134(96)00177-9. doi: http://dx.doi.org.proxy-hs.researchpor-t.umd.edu/10.1016/S0145-2134(96)00177-9. [DOI] [PubMed] [Google Scholar]
- Ross A. Military parent mental health, parenting stress and child functioning at reintegration: A snapshot guiding intervention development; In 141st APHA Annual Meeting; November 2-6, 2013; APHA; Nov, 2013. Retrieved from https://apha.confex.com/apha/141am/webprogramadapt/Paper292277.html. [Google Scholar]
- Ross CE, Mirowsky J, Huber J. Dividing work, sharing work, and in-between: Marriage patterns and depression. American Sociological Review. 1983;48:809–823. [PubMed] [Google Scholar]
- Rowe R, Maughan B, Pickles A, Costello E, Angold A. The relationship between DSM-IV oppositional defiant disorder and conduct disorder: Findings from the Great Smoky Mountains Study. Journal of Child Psychology and Psychiatry. 2002;43:365–373. doi: 10.1111/1469-7610.00027. doi:10.1111/1469-7610.00027. [DOI] [PubMed] [Google Scholar]
- Schmitt TA. Current methodological considerations in exploratory and confirmatory factor analysis. Journal of Psychoeducational Assessment. 2011;29:304–321. doi:10.1177/0734282911406653. [Google Scholar]
- Thompson R, Lindsey MA, English DJ, Hawley KM, Lambert S, Browne DC. The influence of family environment on mental health need and service use among vulnerable children. Child Welfare. 2007;86:57–74. Retrieved from http://eds.a.ebscohost.com.proxy-hs.researchport.umd.edu/ehost/pdfviewer/pdfviewer?sid=82bd3440-8678-43b4-a72a-3d835e207f2f%40sessionmgr4001&vid=2&hid=4103. [PubMed] [Google Scholar]
- Tucker LR, Lewis C. A reliability coefficient from maximum likelihood factor analysis. Psychometrika. 1973;38:1–10. [Google Scholar]
- U.S. Census Bureau The Hispanic Americans by the numbers. 2010 Retrieved from http://www.infoplease.com/spot/hhmcensus1.html.
- Varela RE, Vernberg EM, Sanchez-Sosa JJ, Riveros A, Mitchell M, Mashunkashey J. Parenting style of Mexican, Mexican American, and Caucasian-non-Hispanic families: Social context and cultural influences. Journal of Family Psychology. 2004;18:651–657. doi: 10.1037/0893-3200.18.4.651. doi:10.1037/0893-3200.18.4.651. [DOI] [PubMed] [Google Scholar]
- Warner BS, Weist MD. Urban youth as witness to violence: Beginning assessment and treatment efforts. Journal of Youth and Adolescence. 1996;25:361–378. Retrieved from http://link.springer.com.proxy-hs.researchport.umd.edu/article/10.1007/BF01537390#page-2. [Google Scholar]
- Waschbusch DA, Willoughby MT. Attention-deficit/hyperactivity disorder and callous-unemotional traits as moderators of conduct problems when examining impairment and aggression in elementary school children. Aggressive behavior. 2008;34:139–153. doi: 10.1002/ab.20224. doi:1002/ab.20224. [DOI] [PubMed] [Google Scholar]
- Welfare Statistics 2013 Retrieved from http://www.statisticbrain.com/welfare-statistics/
- Whiteside-Mansell L, Ayoub C, McKelvey L, Faldowski RA, Hart A, Shears J. Parenting stress of low-income parents of toddlers and preschoolers: Psychometric properties of a short form of the Parenting Stress Index. Parenting: Science and Practice. 2007;7:26–56. doi:10.1080/15295190709336775. [Google Scholar]
- Zaidman-Zait A, Mirenda P, Zumbo BD, Wellington S, Dua V, Kalynchuk K. An item response theory analysis of the Parenting Stress Index-Short Form with parents with children with autism spectrum disorders. Journal of Child Psychology and Psychiatry. 2010;51:1269–1277. doi: 10.1111/j.1469-7610.2010.02266.x. doi:10.1111/j.1469-7610.02266.x. [DOI] [PubMed] [Google Scholar]