Abstract
Objective
Oregon has implemented legislation expanding the scope of pharmacists to directly prescribe short-acting hormonal contraception (pill and patch) without a medical prescription. Pharmacists are critical to the success of the new law, but relatively little is known about their intent to prescribe contraception, or the motivators or barriers in providing this service.
Methods
Cross-sectional survey of pharmacists practicing in Oregon prior to legislative implementation. We analyzed responses to assess contraceptive knowledge, motivation to participate in direct provision and perception of barriers to pharmacist prescription of contraception. A logistic regression model was used to examine the association between years in pharmacy practice and intent to provide direct access to contraception.
Results
509 pharmacists responded (17%). If training and reimbursement were offered, over half of pharmacists would potentially be interested in prescribing contraception, managing side effects or transitioning women to a different hormonal method (57%, 61% and 54% respectively). However, only 39.1% of pharmacists surveyed planned to actually prescribe hormonal contraception when the legislation took effect. Shortage of pharmacy staff to provide services, concerns about liability, and a need for additional training were the three largest barriers to participation. Pharmacists practicing in urban locations (OR 1.73 95%CI 1.11–2.70) or currently offering emergency contraception (OR 2.23 95%CI 1.47–3.40) were significantly more likely to be planning to participate.
Conclusion
Preliminary data indicate a need to support pharmacists with education on contraceptive provision and development of interventions to facilitate counseling in the pharmacy setting.
Keywords: contraception, pharmacists, direct provision
Introduction
Oregon and California are the first two states to pass legislation allowing pharmacists to prescribe short acting hormonal contraception (HC) to women without a clinic visit. Oregon implemented this policy January 1, 2016. Prescription of HC by pharmacists, without a doctor’s visit or authorization, has been proposed as a strategy to improve access to contraception and reduce unintended pregnancy [1–5].
Unintended pregnancy is endemic in the United States (US), with significant health and cost consequences, for the individual, her family and the community [6–8]. Contraception is effective at preventing unintended pregnancy but multiple barriers exist to effective and consistent use [2]. Access to and cost of contraceptives are common reasons for nonuse or gaps in use [9,10]. A survey of women in the US, at risk for unintended pregnancy, demonstrated that one out of four experienced challenges in obtaining either a prescription or a refill of their chosen method [11]. Barriers to obtaining contraception from a doctor’s office include: difficulty obtaining an appointment such as long waits, high co-pays, or inconvenient clinic hours, and not wanting to get a pelvic exam [11].
Two different strategies have been proposed to improve access to contraception through pharmacies: over-the-counter access and pharmacist prescription of contraception. There are advantages and disadvantages to each strategy. Over-the-counter status is determined by the Food and Drug Administration, not state legislation. The safety of HC is well established, and there is data to support changing its status to over-the-counter [12–14]. A national survey of women at risk of unintended pregnancy found that 68% of women were interested in over-the-counter access to HC without a prescription (pill, patch, ring and emergency contraception)[11]. Several studies have established that women can self-screen and non-physicians can safely evaluate for contraindications to HC use [13,15]. One cohort study suggests that continuation rates may even be improved with over-the-counter access in pharmacies [13, 14, 16, 17]. The American College of Obstetricians and Gynecologists (ACOG) supports over-the-counter access to HC as a means to safely improve contraceptive use and decrease unintended pregnancy [12]. Over-the-counter access to HC was considered in Oregon, but the legislature ultimately decided to proceed with pharmacist prescription of contraception. The legislature cited concerns about the safety of over-the-counter access, in particular for adolescents, and that this could potentially jeopardize insurance coverage of contraception.
Pharmacist prescription of HC expands the scope of pharmacists who choose to participate in the program to screen women and to prescribe and dispense self-administered, short-acting HC. Oregon’s House Bill 2879 allows pharmacists to directly prescribe HC including the patch and pill without a clinic visit. Women over 18 years of age can either initiate or continue contraceptive care with a pharmacist. For adolescents under age 18, the law allows for them to only continue a HC prescription previously initiated by a clinician. Within the Oregon program, the cost of the contraceptive and the pharmacist visit are billed to insurance.
The Oregon Board of Pharmacy convened a multidisciplinary task force to guide implementation of the policy. Pharmacist participation is voluntary. Prior to participating in the program, pharmacists must complete a five hour training module. The training modules cover a range of information from the mechanism of action and efficacy of modern contraceptives, to counseling patients on different issues (e.g pill adherence, side effects and potential interactions), to how to use the tools developed by the Board of Pharmacy. Checklists for both providing care and referral were developed by the Oregon Board of Pharmacy, based on the World Health Organization and Center for Disease Control’s Medical Eligibility Criteria for Contraceptive Use [18, 19]. The Oregon Board of Pharmacy has published these tools and resources online (https://www.oregon.gov/pharmacy/Pages/ContraceptivePrescribing.aspx#Tool-Kit_Resources). The policy was implemented throughout Oregon on January 1, 2016.
In the context of increased pharmacy access to emergency contraception, a 2004 national survey evaluated pharmacist interest and attitudes towards providing access to other types of HC. In this study, a majority of pharmacists expressed interest in prescribing HC (85%) with 50% stating that they were “very interested [5].” Pharmacists in this study expressed a need for additional training in screening and counseling women on HC use, and identified lack of payment mechanisms and liability issues as key barriers to pharmacist prescription of contraception [5]. In Canada, a survey of community pharmacists indicated a willingness to prescribe HC, but reported concern about start-up costs of offering the service as a significant barrier [4]. Much has changed since these surveys were conducted. Emergency contraception is now nationally available by pharmacists, and new contraceptive methods have been added to the method mix, specifically progestin implants and intrauterine systems. Building on this previous work, we wanted to identify perceived barriers and motivators for Oregon pharmacists to prescribe HC under this new legislation.
The objective of this study was to gather baseline data on Oregon pharmacists’ intent to provide hormonal contraception prior to implementation of House Bill 2879, as well as to identify motivators and perceived barriers to directly providing HC. We hypothesized that pharmacist interest in prescribing contraception will be high, but that concerns about liability and cost will limit participation. We further hypothesized that pharmacists who had been in practice the longest would be the most comfortable with an expanded role to include prescribing contraception, and expected that length of time in practice would be associated with increased odds of participating.
Materials and Methods
We utilized the Oregon Board of Pharmacy electronic listserv (n=6,470) to gain access to our desired study population, pharmacists licensed and primarily practicing in Oregon. All pharmacists licensed in Oregon received the email. Only individuals currently practicing in Oregon were eligible to complete the study (n=3,041). Additionally, we confirmed eligibility by collecting the zipcode of the primary practice location. Survey questions were drafted after a review of the existing literature on pharmacist prescription of contraception [3–5]. Our survey builds off of previous work that explored Canadian and American pharmacists interests in prescribing HC [4,5]. The survey was administered in fall 2015, subsequent to the legislation passing in Oregon but prior to implementation of the policy or to wide-spread education of pharmacists detailing the guidelines for participation. Responses were collected by SurveyMonkey Inc (Palo Alto, CA, USA). Responses were collected over a six week period. Three reminders to complete the survey were sent, no incentives for participating were provided. The institutional review board at Oregon Health & Science University reviewed and approved the study protocol.
Variables
Demographic data collected on survey respondents included: age, sex, years in practice, type of pharmacy (e.g chain, independent, hospital), and their current position. Age, sex and years since pharmacy degree were recorded as categorical variables. Pharmacy type was categorized as: department-mass merchandise, chain, independent, hospital or other [4]. For pharmacy position, respondents were asked to check all that applied (full-time, part-time, floater, pharmacy manager, hospital pharmacist, other). The zipcode of their primary pharmacy location was used to assign urban or rural location. Pharmacist knowledge of both the new legislation and different types of contraceptives was assessed. Pharmacists were asked to self-rate on a scale of one to five their knowledge of different categories of contraception. Pharmacist interest in offering contraceptive information and services was evaluated. Again, using a scale from “Strongly Agree” to “Strongly Disagree” pharmacists were asked to respond to several statements pertaining to prescribing contraception. They were asked to respond to each statement below as best described their views regarding pharmacist prescription of HC.
Pharmacist provision of hormonal contraception is an important health and community service.
I plan to provide hormonal contraception in my pharmacy.
Provision of hormonal contraception will easily fit within my current scope of practice.
I am comfortable following a clinical protocol to determine eligibility for hormonal contraceptive use.
I need additional training on contraception to comfortably and safely provide hormonal contraception.
Providing hormonal contraception within my pharmacy is not feasible currently.
Analyses
We used descriptive statistics to characterize the sample and evaluate contraceptive knowledge, motivation to participate in the program and perception of barriers to direct provision. We developed a logistic regression model to examine the association between years in pharmacy practice and intent to provide direct access to contraception. Our key independent variable was years of practice as a pharmacist. We estimated the odds of intent to provide HC by years in practice and included pharmacist and pharmacy-level covariates in all models. We selected covariates based on a literature review and our a priori assumptions about which covariates were likely to influence behavior. Survey questions were designed in part to capture pharmacist characteristics that were expected to influence behavior. We tested for interactions of potential moderators such as age, using the likelihood ratio test. Covariates included age, sex, urban/rural pharmacy location defined using zip code, and clinical services currently offered (e.g emergency contraception provision). Definitions for rural and urban locations were based on zipcode designations from the state of Oregon’s Office of Rural Health. All analyses were conducted in Stata version 13.2 (StataCorp LP, College Station, Texas, USA).
Results
Our sample included 509 respondents who were currently primarily practicing in Oregon and eligible to complete the survey for a response rate of 17%, with geographic representation across the state.
Descriptive findings
The sample included 42.2% male and 50.5% female pharmacist respondents (Table 1). Our sample included a large proportion of the most experienced pharmacists: 42.6% had been in practice for longer than 20 years. The largest proportions of our sample were either working as full time pharmacists (37.7%) or pharmacy managers (25.1%). A range of types of pharmacies were represented, with the largest group working at chain pharmacies (31.8%). A majority of pharmacists were practicing in urban pharmacies (54.4%).
Table 1.
Demographics of pharmacists
| Sample % (n=509) | |
|---|---|
|
| |
| Age (years) | |
| 18–34 | 20.1 |
| 35–44 | 22.6 |
| 45–54 | 21.8 |
| 55–64 | 20.2 |
| >65 | 8.6 |
| Missing | 6.7 |
|
| |
| Sex | |
| Male | 42.2 |
| Female | 50.6 |
| Missing | 7.2 |
|
| |
| Years in practice | |
| <2 | 3.7 |
| 2–5 | 17.3 |
| 6–10 | 10.4 |
| >10 | 19.8 |
| >20 | 42.6 |
| Missing | 6.2 |
|
| |
| Current pharmacy position | |
| Full-time | 30.5 |
| Part-time | 11.8 |
| Floater | 10.0 |
| Pharmacy manager | 24.1 |
| Other | 11.7 |
| Missing | 11.9 |
|
| |
| Type of pharmacy | |
| Department-mass merchandise | 11.9 |
| Chain | 31.7 |
| Independent | 11.1 |
| Hospital | 17.0 |
| Other | 18.7 |
| Missing | 9.6 |
|
| |
| Rural location* | 31.1 |
| Urban | 54.0 |
| Missing | 14.9 |
|
| |
| Clinical services currently offered | |
| Emergency contraception | 39.3 |
| Influenza and pneumoccal vaccines | 63.9 |
| Health screenings | 24.0 |
| Smoking cessation | 9.6 |
| Missing | 18.4 |
Rural defined using pharmacy zip codes
Awareness of House Bill 2879 was high: nearly all pharmacists had heard about the new legislation prior to the survey (91.0%). We asked pharmacists to self-report their current knowledge of contraindications, compliance considerations and the recognition and management of routine and rare side effects following use of contraception. Less than half described themselves as knowledgeable or highly knowledgeable with respect to use of the combined pill (46.0%), patch (41.7%) or ring (42.1%) or the progestin-only pill (46.8%). Knowledge of long acting reversible contraceptive methods was lower; only 30.7% of pharmacists rated themselves as knowledgeable or highly knowledgable with progestin injectable, 18.6% with the implant and 21.3% about the intrauterine device.
However, interest in providing contraceptive and reproductive health services was relatively high. With training and reimbursement offered, over half of pharmacists would be interested in prescribing contraceptive therapy, managing side effects or transitioning women to a different hormonal method (57%, 61% and 54% respectively). A smaller group of pharmacists would be interested in further expanding services to include offering administration of projestin injectables or implants (36.0% and 13.6). A quarter of survey respondents did not answer as to whether they would like to see the legislation expanded to include pharmacist prescription of other contraceptive methods (25.4% missing data).
However, only 39.1% of pharmacists surveyed planned to provide direct contraception when the legislation went into effect. A large majority of pharmacists expressed an interest in additional training, both in general contraceptive information (61.4%) and identifying women with medical contraindications (72.0%). Additionally, training on contraceptive counseling was identified as a need, with 65.6% of pharmacists requesting guidance.
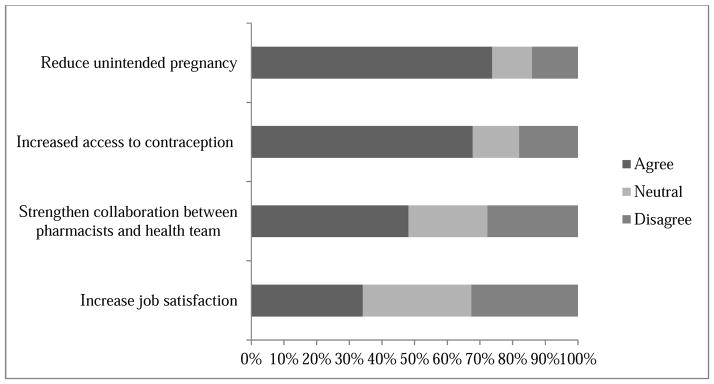
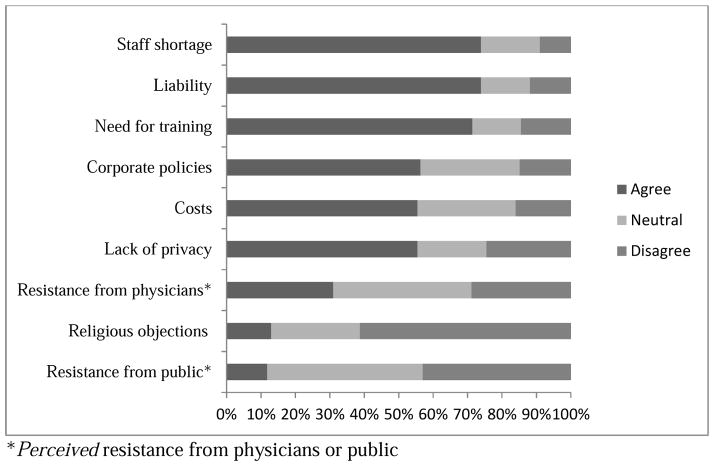
A majority of pharmacists surveyed agreed that direct provision would increase contraceptive access and reduce unintended pregnancy (60.5% and 65.8%). These were the two main motivators for pharmacists in providing care (Figure 1). Several key perceived barriers to direct provision were reported (Figure 2). The top three included: a shortage of pharmacy staff to provide services, concerns about liability, and a need for additional training.
Figure 1.
Reported motivators for pharmacists to provide hormonal contraception
Figure 2.
Pharmacists perceived barriers to direct provision of hormonal contraception
Logistic regression
We used a logistic regression model to evaluate what pharmacist factors are associated with intent to participate in the direct provision of contraception at baseline. Contrary to our hypothesis, years in practice was not associated with increased odds of providing direct access to contraception: no significant difference was seen by length of time in practice (Table 2). Pharmacists currently providing emergency contraception were significantly more likely to plan to provide HC (OR 2.23, 95% CI 1.47–3.40). Pharmacists practicing in rural locations were less likely to plan on offering this service (OR 0.58, 95%CI 0.37–0.89). When we examined whether female or male pharmacists had increased odds of participating, our finding just approached statistical significance, with men less likely to intend to provide (OR 0.67, 95% CI 0.42–1.0).
Table 2.
Association between pharmacist years in practice and intent to provide direct access to hormonal contraception
| Odds Ratio | 95% CI | |
|---|---|---|
|
| ||
| Years in Practice (reference >20 years) | ||
| <2 years | 0.30 | 0.07–1.2 |
| 2–5 years | 0.65 | 0.24–1.8 |
| 6–10 years | 0.47 | 0.17–1.2 |
| >10 years | 0.71 | 0.33–1.5 |
|
| ||
| Age (reference age>65) | ||
| 18–34 years old | 2.28 | 0.63–8.3 |
| 35–44 years old | 1.24 | 0.41–3.8 |
| 45–54 years old | 0.74 | 0.30–1.8 |
| 55–64 years old | 0.49 | 0.20–1.2 |
|
| ||
| Male sex (reference female) | 0.65 | 0.42–1.0 |
|
| ||
| Urban location (reference rural) | 1.70 | 1.11–2.70 |
|
| ||
| EC provision (reference do not provide) | 2.23 | 1.47–3.40 |
Discussion
Direct prescription of HC by pharmacistsis a potential strategy to improve access to contraception and reduce unintended pregnancy. Healthy People 2020 prioritizes prevention of unintended pregnancy and identifies access to contraceptive services as an area of strategic importance. Our findings demonstrate strong baseline interest among Oregon pharmacists in prescribing contraception. Pharmacists who are currently prescribing EC and are practicing in urban locations are significantly more likely to plan on prescribing HC. Differing from earlier work, our study does not demonstrate an association between years in practice and interest in prescribing HC. Our study supports previous literature demonstrating that while pharmacist interest in prescribing contraception is overall high, multiple perceived barriers to participation exist [3–5].
Our study showed that the three main barriers perceived by pharmacists are: shortage of pharmacy staff to provide services, concerns about liability, and a need for additional training. These are similar to concerns previously reported in the literature. As with any new service, mechanisms must be identified to ensure there are trained staff with adequate time and coverage to provide care. One successful model comes from a program in Washington State which introduced pharmacist prescribed HC at a number of community pharmacies and evaluated the medical appropriateness of prescribing practices, pharmacist experiences and patient experiences. The study showed high continuation rates of HC, high acceptance among patients for pharmacist-prescribed HC, and identified reimbursement for pharmacist time as an ongoing challenge [3]. Reimbursement and trained staff are both necessary to ensure the sustainability of the practice [3].
Our survey was conducted prior to implementation of the policy, and before the state released the contraceptive training modules and algorithms for care. It is probable that the training modules have addressed the need for additional training in contraception, and possible that as pharmacists gain experience in prescribing contraception that concerns regarding staff time needed for the service will change. Similar to previous literature, our survey identified concerns about liability as a barrier to pharmacist prescription of contraception [3–5]. As this represents an expansion of the pharmacist role, it is possible that pharmacist malpractice insurance needs will change [5]. Longitudinal data will be helpful in determining how pharmacist attitudes have changed over time with increased experience in prescribing contraception.
The Oregon Board of Pharmacy has taken a proactive approach to facilitating the full implementation of the legislation in Oregon. The task force worked to create a clear referral process for women unable to access care in pharmacies due to cost or medical considerations. The Oregon Board of Pharmacy paid particular attention to training pharmacists to educate women on the most effective methods to prevent pregnancy (long acting reversible and permanent methods) and referral sources to access this care, even though pharmacists cannot provide this care directly. Adding to the cohort of knowledgeable providers on the differential efficacy of methods is likely to benefit women by creating more opportunities to gain information about contraceptive options.
Our study should be interpreted with the following limitations in mind. First, our response rate was low, and pharmacists who chose to respond may differ from the general population of pharmacists in Oregon. This is a potential source of bias, and could bias our results away from the null. However, our sample contains over 500 pharmacists across the state, working in a wide range of pharmacies. Demographic characteristics of respondents are well balanced, which may help mitigate this bias. Furthermore, our ability to stratify by employment position is limited. Our categories for pharmacy position allowed respondents to select multiple options, and thus are not mutually exclusive. Our data was also collected prior to the release of the training modules and other resources for implementation of House Bill 2879. Our findings thus are baseline information on pharmacist attitudes and practices, and do not reflect change over time.
However, while this is a small cross-sectional survey, our findings have important implications for Oregon and the nation. Reduction in unintended pregnancy is a national priority, and multiple interventions are needed to improve access to contraceptive information and services [20]. Direct provision by pharmacists using an evidence-based protocol and checklist is one strategy. Similar legislation has been passed, and other states are considering how to best expand access to contraception. In California, the legislation will also include pharmacist prescription of the vaginal ring and progestin injectable [21].
Oregon has long been at the forefront of reproductive health policies. Since 1999, Oregon has administered a Medicaid waiver that extends Medicaid eligibility for contraceptive service to individuals up to 250% of the federal poverty level through a program called Oregon ContraceptiveCare (CCare). These services are delivered through a statewide network of public and private clinics, many of whom receive Title X funds and specialize in reproductive health care. Previous research has established the efficacy of these family planning waiver programs in preventing unintended births and reducing Medicaid costs [22, 23]. Legislation requiring insurance companies to provide three months of a method on contraceptive initiation, and 12 months worth at time of refill was also passed in Oregon in 2015 (House Bill 3343)[21]. House Bill 2879, allowing pharmacist provision of HC, is the latest contraceptive innovation out of Oregon. There is a need to understand how these changes to the health system affect contraceptive initiation, continuation and satisfaction with care.
Preliminary data indicate a need to support pharmacists with education on contraceptive provision (in particular the intrauterine device and implant), and development of interventions to facilitate contraceptive counseling in the pharmacy setting. There are many reasons to expect legislation like Oregon’s to spread to other states. Oregon offers an opportunity to understand the benefits and challenges to pharmacists prescribing contraception directly. Our survey suggests a high degree of interest among pharmacists. Success of the policy will be contingent on proper training programs and support for services.
Implications.
Under new legislation, Oregon pharmacists will begin prescribing hormonal contraception. This study provides information about pharmacist attitudes towards the legislation and their intent to participate.
Acknowledgments
Funding: Dr Rodriguez is a Women’s Reproductive Health Research fellow; grant 1K12HD085809
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Grossman D. Moving oral contraceptives over the counter as a strategy to reduce unintended pregnancy. Annals of internal medicine. 2013 Jun 4;158(11):839–40. doi: 10.7326/0003-4819-158-11-201306040-00629. [DOI] [PubMed] [Google Scholar]
- 2.Grossman D, Fuentes L. Over-the-counter access to oral contraceptives as a reproductive healthcare strategy. Current opinion in obstetrics & gynecology. 2013 Dec;25(6):500–5. doi: 10.1097/GCO.0000000000000019. [DOI] [PubMed] [Google Scholar]
- 3.Gardner JS, Miller L, Downing DF, Le S, Blough D, Shotorbani S. Pharmacist prescribing of hormonal contraceptives: results of the Direct Access study. J Am Pharm Assoc (2003) 2008;48(2):212–21. doi: 10.1331/JAPhA.2008.07138. 5 p following 21. [DOI] [PubMed] [Google Scholar]
- 4.Norman WV, Soon JA, Panagiotoglou D, Albert A, Zed PJ. The acceptability of contraception task-sharing among pharmacists in Canada--the ACT-Pharm study. Contraception. 2015;92(1):55–61. doi: 10.1016/j.contraception.2015.03.013. [DOI] [PubMed] [Google Scholar]
- 5.Landau S, Besinque K, Chung F, et al. Pharmacist interest in and attitudes toward direct pharmacy access to hormonal contraception in the United States. J Am Pharm Assoc (2003) 2009;49(1):43–50. doi: 10.1331/JAPhA.2009.07154. [DOI] [PubMed] [Google Scholar]
- 6.Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspectives on sexual and reproductive health. 2006 Jun;38(2):90–6. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- 7.Finer LB, Zolna MR. Shifts in intended and unintended pregnancies in the United States, 2001–2008. American journal of public health. 2014;104(Suppl 1):S43–8. doi: 10.2105/AJPH.2013.301416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sonfield A, Kost K, Gold RB, Finer LB. The public costs of births resulting from unintended pregnancies: national and state-level estimates. Perspectives on sexual and reproductive health. 2011 Jun;43(2):94–102. doi: 10.1363/4309411. [DOI] [PubMed] [Google Scholar]
- 9.Frost JJ, Singh S, Finer LB. Factors associated with contraceptive use and nonuse, United States, 2004. Perspect Sex Reprod Health. 2007 Jun;39(2):90–9. doi: 10.1363/3909007. [DOI] [PubMed] [Google Scholar]
- 10.Frost JJ, Singh S, Finer LB. U.S. women’s one-year contraceptive use patterns, 2004. Perspectives on sexual and reproductive health. 2007 Mar;39(1):48–55. doi: 10.1363/3904807. [DOI] [PubMed] [Google Scholar]
- 11.Landau SC, Tapias MP, McGhee BT. Birth control within reach: a national survey on women’s attitudes toward and interest in pharmacy access to hormonal contraception. Contraception. 2006 Dec;74(6):463–70. doi: 10.1016/j.contraception.2006.07.006. [DOI] [PubMed] [Google Scholar]
- 12.ACOG Committee on Gynecologic Practice. Committee Opinion No 544: Over-the-counter access to oral contraceptives. Obstetrics and gynecology. 2012 Dec;120(6):1527–31. doi: 10.1097/01.AOG.0000423818.85283.bd. [DOI] [PubMed] [Google Scholar]
- 13.Grossman D, Fernandez L, Hopkins K, Amastae J, Garcia SG, Potter JE. Accuracy of self-screening for contraindications to combined oral contraceptive use. Obstetrics and gynecology. 2008 Sep;112(3):572–8. doi: 10.1097/AOG.0b013e31818345f0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shotorbani S, Miller L, Blough DK, Gardner J. Agreement between women’s and providers’ assessment of hormonal contraceptive risk factors. Contraception. 2006 May;73(5):501–6. doi: 10.1016/j.contraception.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 15.Gardner JS, Miller L, Downing DF, Le S, Blough D, Shotorbani S. Pharmacist prescribing of hormonal contraceptives: results of the Direct Access study. Journal of the American Pharmacists Association : JAPhA. 2008 Mar-Apr;48(2):212–21. doi: 10.1331/JAPhA.2008.07138. 5 p following 21. [DOI] [PubMed] [Google Scholar]
- 16.Doshi JS, French RS, Evans HE, Wilkinson CL. Feasibility of a self-completed history questionnaire in women requesting repeat combined hormonal contraception. The journal of family planning and reproductive health care / Faculty of Family Planning & Reproductive Health Care, Royal College of Obstetricians & Gynaecologists. 2008 Jan;34(1):51–4. doi: 10.1783/147118908783332203. [DOI] [PubMed] [Google Scholar]
- 17.Potter JE, McKinnon S, Hopkins K, Amastae J, Shedlin MG, Powers DA, et al. Continuation of prescribed compared with over-the-counter oral contraceptives. Obstetrics and gynecology. 2011 Mar;117(3):551–7. doi: 10.1097/AOG.0b013e31820afc46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Medical Eligibility Criteria for Contraceptive Use. WHO Guidelines Approved by the Guidelines Review Committee. 5. Geneva: 2015. [Google Scholar]
- 19.Centers for Disease C, Prevention. U S. Medical Eligibility Criteria for Contraceptive Use, 2010. MMWR Recommendations and reports : Morbidity and mortality weekly report Recommendations and reports / Centers for Disease Control. 2010 Jun 18;59(RR-4):1–86. [PubMed] [Google Scholar]
- 20.ACOG Committee on Health Care for Underserved Women. Committee opinion no. 615: Access to contraception. Obstetrics and gynecology. 2015 Jan;125(1):250–5. doi: 10.1097/01.AOG.0000459866.14114.33. [DOI] [PubMed] [Google Scholar]
- 21.Barot S. Moving oral contraceptives to over-the-counter status: policy versus politics Guttmacher Policy Review. 2015. Fall [Google Scholar]
- 22.Amaral G, Foster DG, Biggs MA, Jasik CB, Judd S, Brindis CD. Public savings from the prevention of unintended pregnancy: a cost analysis of family planning services in California. Health Serv Res. 2007 Oct;42(5):1960–80. doi: 10.1111/j.1475-6773.2007.00702.x. Epub 2007/09/14. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lindrooth RC, McCullough JS. The effect of Medicaid family planning expansions on unplanned births. Womens Health Issues. 2007 Mar-Apr;17(2):66–74. doi: 10.1016/j.whi.2007.02.012. Epub 2007/04/04. eng. [DOI] [PubMed] [Google Scholar]