Abstract
It is crucial to examine patient reactions to genomics-informed approaches to weight management within a clinical context, and understand the influence of patient characteristics (here, emotion and race). Examining nonverbal reactions offers a window into patients’ implicit cognitive, attitudinal and affective processes related to clinical encounters. We simulated a weight management clinical interaction with a virtual reality-based physician, and experimentally manipulated patient emotional state (anger/ fear) and whether the physician made genomic or personal behavior attributions for weight. Participants were 190 overweight females who racially identified as either Black or White. Participants made less visual contact when receiving genomic information in the anger condition, and Black participants exhibited lowered voice pitch when receiving genomic information. Black participants also increased their interpersonal distance when receiving genomic information in the anger condition. By studying non-conscious nonverbal behavior, we can better understand the nuances of these interactions.
Keywords: Nonverbal behavior, paraverbal behavior, physician-patient interaction, genomics, emotion, obesity, race
Genomic information is increasingly being integrated into medical practice (Manolio et al., 2013). Although not yet typically applied to weight management and obesity-related practice, genomics is believed to be a promising avenue for future prevention and treatment efforts in this area (Bray et al., 2016). Genomics may have a sizeable influence on body weight. Estimates suggest that between 40–70% of one’s weight is inherited, with several genes influential in weight and weight-related processes like eating behavior (Bray et al., 2016). Even in the absence of applicable genomic technologies, concepts related to genomics and body weight emerge in conversations about family history, new clinical discoveries, and media reports.
In addition to the promise of genomics for direct patient care, research has shown that discussion of genomics could also have the added benefit of improving patient-provider communication and relationships (Persky & Eccleston, 2011; Persky & Street, 2015). Patient-provider communication and relationships are crucial in their influence on the quality of medical care and ultimately patient health (Epstein & Street, 2007). Bolstering the quality of communication may be especially beneficial in encounters that pertain to overweight and obesity, where much of the clinical visit revolves around interpersonal counseling, and where there is often an atmosphere of stigma (Puhl & Heuer, 2009).
Importantly, the genomic attributions a provider appears to make about the causes of a patient’s condition can have repercussions for the patient’s attitudes and beliefs toward the provider (Persky & Street, 2015), a line of reasoning that stems from Attribution Theory. To the extent a health condition is perceived to be controllable, stable, and internal, it is theorized to lead to more stigmatization (Weiner, Perry, & Magnusson, 1998). Making a genomic attribution for one’s weight can evoke lower control and thereby less blame and stigma (Crandall, 1994). As such, a provider who discusses genomic underpinnings of weight could be perceived as less blaming and stigmatizing. However, a genomic attribution is also internal and stable, so could alternatively be associated with increased stigma. Patients may also react negatively to perceptions that they are being told they are not in control of their bodies or their health (Brehm & Brehm, 1981). It is an open question as to what factors will cause patients to interpret genomic information such that it leads to more positive versus more negative outcomes related to perceptions of the provider. In addition, research so far has focused on summary, self-report outcomes following clinical visits; little attention has been paid to how the in vivo experience of genomic communication influences patient perceptions and reactions.
Nonverbal and Paraverbal Communication
Interpersonal communication between patients and providers includes both verbal content as well as nonverbal and paraverbal processes (e.g., posture and voice quality, respectively). Examining patient’s nonverbal communication during a consultation can provide a window into patient reactions to a provider over the course of a consultation. Nonverbal communication is central to human social interactions, including patient-provider interactions (Schmid Mast, 2007), and can influence the patient-provider relationship via patient satisfaction, health care utilization, and health outcomes (Ambady, Koo, Rosenthal, & Winograd, 2002; Henry, Fuhrel-Forbis, Rogers, & Eggly, 2012; Prkachin, Schultz, & Hughes, 2007). Many nonverbal communication behaviors are largely non-conscious (Ambady & Weisbuch, 2010). Thus, examining nonverbal communication may give researchers unique access to implicit cognitive, attitudinal and affective processes (Bessenoff & Sherman, 2000; Dovidio, Kawakami, Johnson, Johnson, & Howard, 1997; Richeson & Shelton, 2005). Nonverbal communication behaviors can differ based on social status in an interaction, but importantly are also often associated with positive or negative attitudes toward one’s interaction partner (Bessenoff & Sherman, 2000; McCall, Blascovich, Young, & Persky, 2009; Mehrabian, 1968). Thus, examining nonverbal behaviors may provide insight into implicit patient evaluations of a provider or interaction without disrupting the flow of communication.
There is a rich literature on nonverbal processes that occur between individuals who are from high- versus low-status groups. In the health care interaction, we could consider the provider to be of higher status, and overweight/obese patients of lower status given their relative situational power and the inherent stigma of being overweight. Generally, low-status group members show vigilant nonverbal behaviors, and exhibit less approach behavior and more defensiveness (Dovidio, Hebl, Richeson, & Shelton, 2006). In these contexts, researchers often examine behaviors such as interpersonal distance, lean, visual gaze and touch (Ambady & Weisbuch, 2010; Hall, Coats, & LeBeau, 2005). In particular, averted gaze and backward lean are considered to be markers of disengaged communication (Levine & Ambady, 2013; Robinson, 2006).
Vocal qualities have also been noted as an important paraverbal factor to consider (Ambady & Rosenthal, 1998; Henry et al., 2012), although few studies examine what voice changes mark disengagement. In general, lower pitch is associated with lower psychological engagement states, such as boredom and indifference (Banse & Scherer, 1996; Scherer, 2003). Individuals in a lower status situation may also exhibit lower pitched voices and higher levels of pitch variability (Ko, Sadler, & Galinsky, 2014). In all, one might expect that overweight patients perceiving bias from a physician would exhibit a pattern of lower visual gaze and vocal pitch, and increased interpersonal distance and pitch variability.
Moderating Factors: Emotion
In considering factors that may influence patients’ interpretation of genomic information and their resulting interpersonal reactions, a patient’s emotional state has great potential. Emotions can influence many of the social and cognitive processes, such as medical decision-making, that occur in the clinical setting (Angie, Connelly, Waples, & Kligyte, 2011; Levine & Pizarro, 2004). Further, emotions are commonly evoked in medical settings (Finset, 2012). For example, a patient may be angry due to long wait times or fearful due to medical test results or impending tests or procedures. Emotions can be expected to modify patient experience and interpretation of the clinical communication encounter, with different emotions having different effects. Recent research has demonstrated that emotional state influences some of the health behavior-related attitudes and cognitions individuals have in response to provision of genomic information. In an internet-based study, for example, individuals who received weight-related genomic information while in a fear state were more defensive and likely to disengage from that information (Persky, Ferrer, & Klein, 2016). However, the potential moderating influence of emotion on patient’s interpersonal reactions to physician provision of genomic information is unknown.
Theoretically, according to the Appraisal Tendency Framework, perceptions of control are higher in an angry state and lower in a fear state (Lerner & Keltner, 2000). Consequently, patients in an anger state may reject and feel negatively toward a provider who gives a genomic attribution message if they perceive that the message implies that they have less control over their health. In addition, emotion can also flavor individuals’ reactions to perceived stigma or mistreatment by influencing how they interpret ambiguous social information (DeSteno, Dasgupta, Bartlett, & Cajdric, 2004; Forgas, 1994). Moreover, anger is associated with greater distrust in ambiguous social interactions (Dunn & Schweitzer, 2005; Lerner & Tiedens, 2006). Thus, patients who enter a clinical interaction in an angry state may be more likely to interpret the events of the interaction or the information provided as stigmatizing, which could contribute to perceptions of weight bias.
Moderating Factors: Patient Race
Another factor likely to moderate the influence of genomic information provision on the patient-provider relationship is patient race. Racial minority patients, when faced with providers’ genomic explanations for their overweight, may tend toward more stigmatizing interpretations of those attributions. This is, first, because racial minority patients, particularly those interacting with a racial majority physician, may monitor that physician’s communication for signs of stigma or bias (Shelton & Richeson, 2006). Second, genomic explanations for conditions and traits have historically been associated with distrust among many African-Americans (Peters, Rose, & Armstrong, 2004; Thompson, Valdimarsdottir, Jandorf, & Redd, 2003).
Further, patient race has the potential to interact with patient emotion in shaping these processes. As noted, patients in an angry state may be more likely to interpret the events of the interaction or the information provided as negative, which could contribute to perceptions of weight bias or weight discrimination. This may be even more likely for African-American patients given pre-existing levels of vigilance, particularly in interactions with racial majority physicians. Although these negative reactions to providers’ discussions of genomics might be less likely to emerge in explicit, verbal communication, the non-conscious nature of nonverbal behavior could provide a window into such reactions.
The Current Study
To unite these frameworks, the current analysis examined nonverbal and paraverbal communication behavior stemming from a clinical interaction in which a White, male physician provided genomic versus behavioral information about weight. We further explored the role of contextual factors: the emotional state of patients and whether patients racially identified as Black versus White. We implemented an experimental procedure using immersive virtual reality to simulate and conduct behavioral measurement within a virtual physician-patient interaction. Assessment of naturalistic behavior in a medical setting can be logistically challenging and resource-intensive (Roter, Frankel, Hall, & Sluyter, 2006). Virtual encounters offer a novel way to move beyond hypothetical vignettes and videotapes to capture unconscious, nonverbal behavior in an ecologically valid setting (Persky, 2011). Previous work has shown that research participants react to virtual reality-based human characteristics (e.g., apparent race) and behavior (e.g., social influence behaviors) in ways consistent with reality (Blascovich et al., 2002; McCall et al., 2009; Persky, Kaphingst, Allen, & Senay, 2013). They also perceive virtual humans to be a source of interpersonal evaluation (e.g., blame) (Persky & Street, 2015). Furthermore, collection of nonverbal behavior data can be conducted in a precise and automated fashion (Bailenson, Blascovich, Beall, & Loomis, 2003).
We tested whether participants receiving genomic information related to weight from a White male physician would exhibit more engagement in their a) physical nonverbal behavior (more visual contact, less interpersonal distance) and b) vocal behavior (higher pitch, less pitch variability) than those who received behavioral information. We also tested whether engagement would be influenced by emotional state and race. We hypothesized that participants would show less engagement following genomic information provision in the anger condition and if they were Black.
Method
Participants were randomized to receive an emotion induction to elicit anger or fear. They then interacted with a digital White, male virtual reality-based physician who delivered information related to either genomic or behavioral underpinnings of body weight. Participants were divided by whether they reported their race as Black or White. Analyses were thus based on eight groups resulting from a fully crossed design: information type (genomic/behavioral) by emotion type (anger/fear) by race (Black/White). The Black patients were racially discordant from the virtual physician whereas the White patients were racially concordant with the physician. This research was approved by the Institutional Review Board of the National Human Genome Research Institute.
Participants
Initial participants included a community sample of 249 women who reported being overweight (BMI ≥ 25) and between the ages of 18–50. Forty-six participants either did not schedule or did not arrive at a lab visit. Five participants were excluded from analysis due to equipment problems, and 8 were excluded due to reporting a race other than Black or White. The final number included in analysis was 190. Exclusion criteria were: having a vestibular or seizure disorder; having a high propensity for motion sickness; known pregnancy; uncorrected low vision or hearing; history of eating disorder; previous or current diagnosis with breast cancer (some information delivered in the virtual session related to weight and breast cancer risk); having received information about the study purpose from a previous participant; and being or training to become a physician. Participants were from the Washington, DC metropolitan area and were recruited from the community through flyer posting, online posting (e.g., Craigslist), and databases of individuals who previously indicated interest in clinical trials.
Procedure
Individuals were screened for eligibility over the phone, and if eligible, were directed to a secure website to indicate initial consent to participate and complete a pre-test questionnaire. Participants were re-consented and assigned to condition using a random number generator at a lab visit, typically between 1 and 4 weeks later. The lab portion of the study was presented as two separate tasks within one study. Emotions were induced with a short film clip that had previously been validated to reliably elicit fear (Silence of the Lambs) or anger (My Bodyguard) (Gross & Levinson, 1995). Participants completed a short questionnaire containing items related to the film clip. They were then seated and interacted with the virtual reality-based physician in a virtual clinic room. The virtual encounter was created and administered using the Vizard software package (WorldViz, Santa Barbara, CA), using an nVis SX60 head mounted display and a WorldViz Position Point Tracker tracking system. In the encounter, the virtual physician presented pre-recorded information about weight management and engaged participants in a conversation by asking questions (e.g., “what do you think of this information?”). The content that the virtual physician presented differed by assigned condition such that half of the sample received information primarily about genomic underpinnings of weight (e.g., weight is quite heritable), and the other about behavioral underpinnings of weight (e.g., that that extra calories eaten can add up over time). During this encounter, the virtual reality system unobtrusively recorded participants’ speech in conversation with the physician, the location toward which they gazed, and their chosen distance from the virtual physician. Following the encounter, participants completed a set of self-report measures.
Interpersonal distance
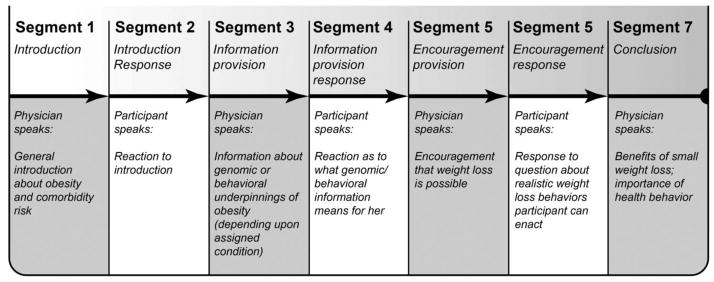
The virtual reality program tracked the distance in centimeters between the participants’ heads and the virtual physician’s head and reported an average for each segment of the conversation (see Figure 1). We assessed the pattern of interpersonal distance behavior over the course of the interaction.
Figure 1.
Nonverbal communication behavior measurement segments within the virtual physician-participant interaction
Visual contact
The virtual reality program automatically determined what part of the virtual environment was in the center of participants’ view during the interaction. A threshold was determined a priori such that the virtual physician’s face was considered centered when it was within a radius of 110 pixels from the center of the participant’s view. The program determined whether the physician was inside or outside the central part of the participant’s view at 2 Hz during the interaction. The percentage of time participants had the physician’s face in the center of their view was determined for each conversation segment. As with interpersonal distance, we assessed the pattern of visual contact over the course of the interaction.
Vocal cues
The recordings of the participants’ verbal responses to the physician were analyzed for pitch (fundamental frequency in Hz) and pitch variability (standard deviation) using the software package Praat (Boersma & Weenink, 2008). We compared the pitch and pitch variability between two target segments (where genomic or behavioral information was presented versus the segment that preceded; segments 4 versus 2, see Figure 1). We assessed the difference between two segments only because there were many segments where participants did not speak and therefore vocal cues could not be assessed.
Self-reported perceived stigmatization and trust
Following the virtual interaction, participants responded to two items that assessed the extent to which they felt stigmatized by the physician due to weight: “this physician thinks less of me because of my weight” and “this physician believes I won’t follow his advice” (r=0.64, p<.0001). Two items assessed trust in the physician: “if this were your physician, how much would you trust him?” and “I would feel comfortable if this physician were my physician” (r=.70, p<.0001). These items were created de novo as suitable items did not exist. All responses were on a 1–7 scale (1 = strongly disagree to 7 = strongly agree).
Data Analysis
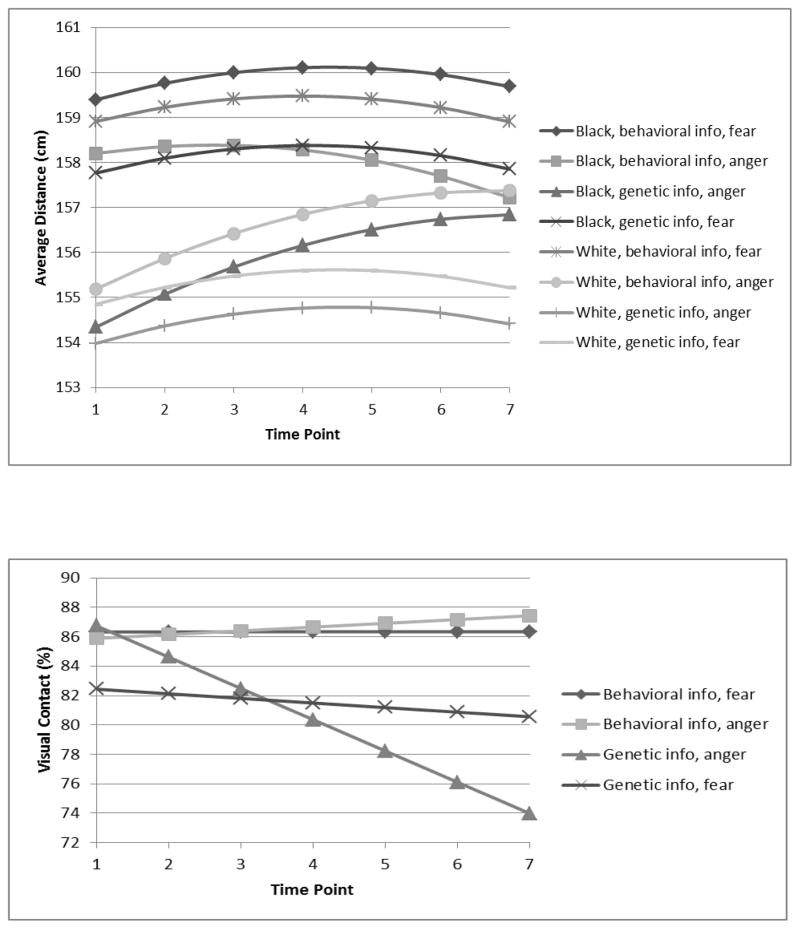
We estimated growth curve models for each outcome across the seven segments to describe patterns of change throughout the interaction. For both outcomes, time was centered on the segment where the physician provided genomic or behavioral information about weight to the participant (segment 3). The growth curve model for the interpersonal distance measure was a quadratic fixed effect and a quadratic random effect (see Figure 2). The growth curve model for the visual contact measure was a linear fixed effect and a linear random effect (see Figure 2).
Figure 2.
Growth curve model predicted means for nonverbal behavior measures. 1) Interpersonal distance: information type by emotion type by participant race, 2) Visual contact; information type by emotion type
Interactions were also tested with fixed effects of time to determine how race, information type, and emotion type were linked to change over time in each of the outcomes. We focused on interactions with time given our interest in change in nonverbal behavior through the course of the interaction. To interpret significant interactions we plotted change over time for each of the groups (i.e., the different combination of variables that significantly interacted with time), tested the significance in change over time for each of the groups, and tested for significant differences in change over time between each pair of groups. For voice pitch and pitch variability, we ran separate ANCOVAS that assessed the influence of the conditions on the difference between pitch and pitch variability during the segment in which genomic/behavioral information was given versus the segment that came before. We also assessed the effect of condition on the self-reported outcomes (perceived weight stigma and trust) using an independent ANCOVA for each outcome. Participant BMI and education level (college graduate, yes or no) were included as covariates in all analyses. We also controlled for amount of time the participant spent in the interaction for the vocal cue measures. We assessed significance at p<.05, but report effects at p<.10 for higher-order interactions.
Results
Demographics
See Table 1 for demographics by group. There was no difference in participant age by group. Differences in participant BMI by race were significant, F(1,182)=9.05.72, p=.003, as were differences in education level, Χ2 (7, n=190)=42.47, p<.0001 (which were strongly associated with race). Thus, BMI and education were entered as covariates in all analyses.
Table 1.
Demographics by study group (Information type, Emotion type, Race); means and standard deviations or n and percent
| Behavioral, fear, Black (n=32) | Genomic, fear, Black (n=25) | Behavioral, anger, Black (n=25) | Genomic, anger, Black (n=17) | Behavioral, fear, White (n=14) | Genomic, fear, White (n=22) | Behavioral, anger, White (n=23) | Genomic, anger, White (n=32) | Total (n=190) | |
|---|---|---|---|---|---|---|---|---|---|
| BMI | 34.78 (8.51) | 36.85 (7.70) | 34.18 (8.37) | 31.66 (6.88) | 30.68 (4.25) | 30.86 (5.96) | 32.74 (5.01) | 30.85 (5.12) | 33.03 (7.02) |
| Age | 33.34 (8.86) | 37.88 (8.65) | 35.44 (8.11) | 33.06 (10.47) | 35.86 (9.40) | 36.77 (10.41) | 33.09 (8.97) | 36.34 (9.50) | 35.13 (9.23) |
| College graduate | 15 (47%) | 10 (40%) | 11 (44%) | 7 (41%) | 12 (86%) | 21 (96%) | 21 (91%) | 26 (81%) | 127 (64%) |
Interpersonal Distance
Adding predictors and their interactions with fixed effects of time to the quadratic growth curve model yielded a significant interaction among information type, emotion type, participant race and linear time γ=−0.97, p=.0082. See Figure 2. Participants who received genomic information, were in the anger condition and were Black exhibited a significant linear increase in distance over time, γ =0.54, p=.0005, as predicted. This pattern was also seen among participants who received behavioral information, were in the anger condition and were White, γ =0.49, p=.0003. This pattern indicates that both Black participants who received genomic information, and White participants who received behavioral information increasingly distanced themselves from the physician as the interaction continued, but only when they were in the anger condition. Participants who received genomic information, were in the anger condition, and were Black were significantly different in their linear increase in interpersonal distance over time from 3 of the other 7 conditions (ps <.05), and were different from 3 additional condition at trend level (ps <.10). The group that received behavioral information, were in the anger condition and were White were significantly different in their linear increase from 2 of the 7 conditions (ps <.05), and trended towards showing a difference from four additional conditions (ps <.10). Other interactions were also significant in the overall growth curve model (emotion type x race x time and information type x emotion type x time), but were qualified by the higher-order interaction described above.
Visual Contact
Adding predictors and all interactions with fixed effects of time to the linear growth curve model revealed a trend-level interaction among information type, emotion type and linear time γ =−0.46, p=.052. See Figure 2 for graph. Consistent with predictions, participants who received genomic information while in the anger condition exhibited a significant linear decrease in visual contact over time, γ =−2.12, p=.0096. Thus, regardless of race, participants who were in the anger condition and received genomic information increasingly looked away from the physician as the interaction progressed. This group was significantly different in its change over time from the behavioral anger group (p<.05), however differences did not achieve significance relative to the other two groups (ps<.12). No other relevant interactions reached significance in the overall growth curve model. Thus, the pattern was consistent for both Black and White participants.
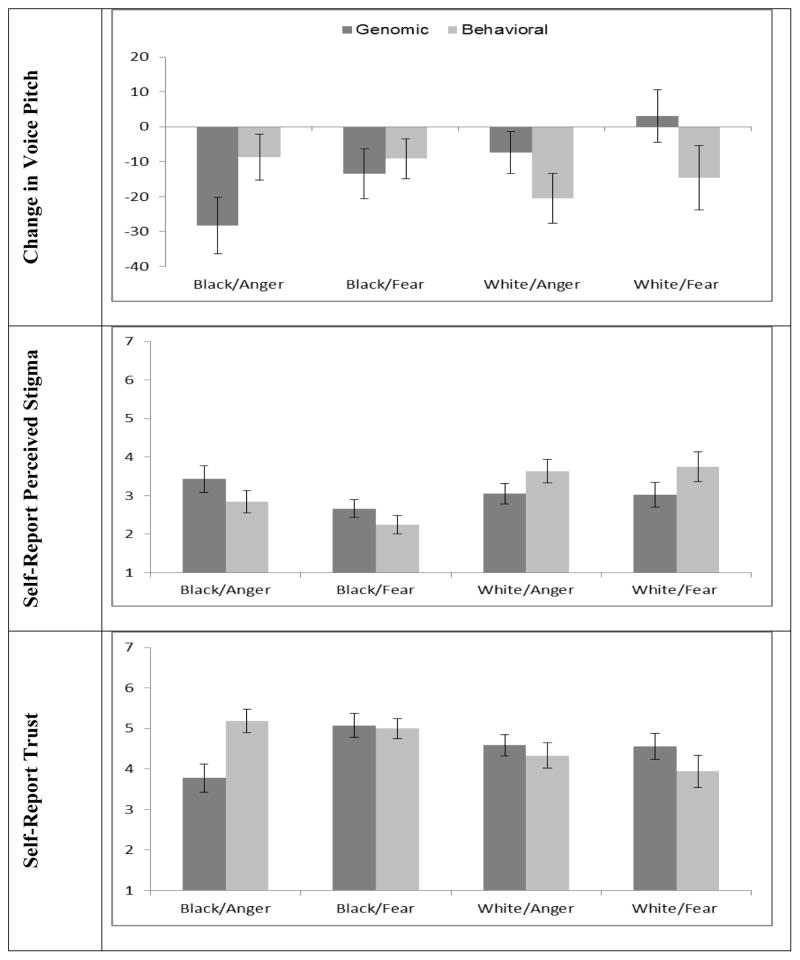
Vocal Cues
For voice pitch there was an information type x race interaction, F(1,173)=7.77, p=.006, partial η2=.043. Black participants dropped their pitch more in discussing information about genomic underpinnings of weight than White participants, regardless of emotional state (Figure 3). There were no significant effects of condition on pitch variability.
Figure 3.
Outcomes for mean pitch difference from segment 4 to segment 2, and self-report outcomes collected at post-test. All are estimated marginal means.
Self-Report Outcomes
For ratings of perceived weight-based stigmatization from the physician, there was a main effect of race such that White participants felt more stigmatized than Black participants, F(1,180)=6.48, p=.012, partial η2=.035; see Figure 3. There was also a significant interaction between race and information type [F(1,180)=6.73, p=.010, partial η2=.036] such that Black participants felt more stigmatized when they received genomic information (consistent with findings for interpersonal distance), but White participants felt less stigmatized when they received genomic information. There were no other significant main effects or interactions.
For ratings of trust, there was similarly an information type-by-race interaction [F(1,180)=6.24, p=.013, partial η2=.034] such that Black participants trusted the physician less when he provided genomic information. There was also an information type-by-emotion type interaction [F(1,188)= 4.82, p=.029, partial η2=.026] such that for those in the anger condition, trust was lower following receipt of genomic information; for those in the fear condition, trust was lower following receipt of behavioral information. There were no other significant main effects or interactions.
Discussion
Clinical encounters are crucial for patient health, but can be very complex interpersonally, particularly with the added dimensions of potentially sensitive topics related to weight management, genomic content, patient emotion, and issues around racial/ethnic identity. We explored patient response to these interaction components by assessing implicitly-driven behaviors that can be indicative of the quality of the patient-provider relationship. Importantly, nonverbal behaviors appear to be reactive to elements of the interaction (i.e., patient emotion) that may not be consciously accessible to the patients themselves.
Findings suggested that patients’ interpersonal behaviors and reactions are influenced by both their emotional state and their race. Influential dimensions varied by measure, with many outcomes detecting effects that were dependent on two of the three predictor variables tested. Even so, these patterns were largely consistent with predictions based on the genomic testing, emotion, and intergroup literatures, as well as our conjectures about how these literatures might dovetail. Overall, Black participants reacted more negatively to genomic information presented by a White male physician on the self-report items and as indicated by voice pitch, regardless of emotional state. However, only those in the anger condition also increased their interpersonal distance from the physician during the encounter. It may be that those Black participants who were in the fear condition and who received genomic information attempted to regulate their nonverbal behaviors to maintain a more harmonious interaction. Alternatively, being in an anger state may have been necessary to elevate negative reactions enough to carry-over into one’s interpersonal distance behavior.
Consideration of patients with this cluster of characteristics is also important practically; African-American patients are more likely to distrust the medical system (Armstrong et al., 2013), and it is therefore possible that they may be predisposed to experience anger in medical settings. Moreover, African Americans’ perceived stigma in medical encounters may also predispose anger, given evidence from other domains that stigmatization results in emotions like anger (Smart Richman, 2009). The potential for such anger to arise may thus need to be considered in contexts related to provision of genomic or genomic information as this information may lend itself to being viewed in a way that evokes perceptions of stigma or race-based mistreatment.
Whereas for the interpersonal distance outcome, White participants in the anger condition reacted negatively to behavioral information and Black participants in the anger condition reacted negatively to genomic information, the visual contact outcome was not sensitive to participant race. Here, all participants in the anger condition reacted more negatively to genomic information. This is consistent with theoretical predictions, such that high control tendencies associated with anger should lead to more negative reactions to genomic information to the extent that the information is interpreted as being low-control (Lerner & Keltner, 2000). On the other hand, this is inconsistent with other findings in the study which suggested that White participants react positively to provision of genomic information by the physician. This may be, in part, due to a power issue. The effect here appears to be primarily driven by Black participants in this group, whereas the pattern of visual contact behavior for the White participants in this group is not highly differentiated from the other conditions.
Similarly, findings for voice pitch were sensitive to provision of genomic versus behavioral information and to race effects in the predicted direction, but were not moderated by emotional state. Very little is known about the influences on voice pitch in this context and more investigation is warranted. However, pitch does seem to be a sensitive indicator of some of the nuances of interpersonal communication.
Self-reported perceived stigma and trust followed the pattern found for voice pitch. Among White participants, provision of weight-related genomic information was either neutral or beneficial for the patient-provider relationship, largely consistent with previous research (Persky & Street, 2015). However, as predicted, among Black participants genomic information was more likely to be detrimental. Analyses also revealed main effects of participant race such that White participants perceived more weight stigma in the interaction than Black participants. It is not surprising that Black women in our sample felt weight-based stigma less acutely given that race-based stigma may present itself as a possibility in the interaction with the White physician, and given lower levels of weight stigma in this population more generally (Hebl, King, & Perkins, 2009). The fact that the Black women in our sample also reported more trust in the physician than White women is a bit more difficult to explain. It may be that some of the distrust among the White women is related to perceived stigma. In addition, all participants in the current study likely have some baseline level of trust in physicians in order to agree to study participation. In all, however, the current work demonstrates that contextual factors outside of communication content can influence how genomic content is perceived and responded to on both an implicit and explicit level.
The Role of Incidental Emotion
In the current study, participant emotion was incidental (elicited outside of the clinical interaction context by stimuli not relevant to the content of the interaction) as opposed to integral (normatively related to the interaction). In general, effects of incidental and integral emotions are believed to be consistent. and incidental emotion inductions have the advantage of greater experimental control, allowing one to identify the effects of emotion unconfounded with other study stimuli (Lerner & Keltner, 2000; Loewenstein & Lerner, 2003). The current results point to an intriguing possibility that incidental emotions may be more influential than integral emotions on nonverbal behaviors. This is because the cause and therefore the influence of the emotion on one’s cognition and behavior is more likely to be beneath conscious awareness given that they are elicited in another context. The current findings do not directly address this interesting hypothesis.
Strengths and Limitations
Notably, this study occurred in a virtual reality-based clinical simulation. This approach allowed for a scenario more closely approaching a clinical visit in terms of visual and psychological realism relative to other traditional simulation techniques, and one maintaining the tight experimental control required to address our research questions (Persky, 2011). In addition, because body movement directly drives operation of the virtual reality system, assessment of nonverbal communication behaviors was automatic, continuous and unobtrusive. The primary limitation of using this approach was that we did not capture all of the complexity and the reciprocal nature of the interaction as it would occur in a real clinic visit.
There are additional strengths and limitations of this study. We included only a small set of measures of nonverbal communication behavior. Assessment of a wider array of behaviors may provide a clearer picture of participant response. However, the current study was able to bring together non-conscious behaviors that have not been frequently linked, and these behaviors demonstrated relatively consistent patterns. An additional weakness is that the self-report assessments were short and created for this study, as existing measures were not suitable. Moreover, the virtual physician was always White and therefore racially discordant with Black participants, but concordant with White participants. Although this is a common occurrence in the health care system (Saha, Komaromy, Koepsell, & Bindman, 1999), in the context of our study this means that the influences of participant race versus racial concordance with the virtual physician cannot be teased apart. Finally, cell sizes between conditions were uneven as we did not recruit or employ block randomization based on participant race.
Conclusion
In sum, the coming precision medicine era will likely bring genomic information into weight management-oriented clinical interactions. The effects of this information will not be uniform, but instead will be influenced by contextual aspects of the interaction. The current study demonstrated that by studying non-conscious nonverbal and paraverbal behavior, we can better understand the nuances of these interactions and identify contexts that may be problematic in these encounters. This is crucial, as interpersonal elements of the clinical encounter can be a major influence on quality of care and patient health outcomes (Epstein & Street, 2007). In addition, patients’ nonverbal behaviors directly influence physician attitudes, beliefs and behavior, as well as outcomes of the medical visit itself (Schmid Mast, 2007), and are therefore crucial to understand in their own right. By fully exploring these processes we may be able to inform development of approaches to improve communication of genomic information and relationships between patients and providers, and gain an understanding how we may contribute to the reduction of health disparities in genomic medicine.
Acknowledgments
Funding: This study was funded by the Intramural Research Program of the National Human Genome Research Institute
This research was supported by the Intramural Research Program of the National Human Genome Research Institute, National Institutes of Health. The authors thank Paul Han, MD for advice and feedback during study development. We acknowledge Peter Hanna, Stephanie Browning, Rachel Ullah, and Leah Abrams for assistance with data collection, and Allison Sypher for assistance with data coding.
Footnotes
Conflict of Interest: The authors declare that they have no conflicts of interest.
Trial registry: clinicaltrials.gov NCT01888913
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
References
- Ambady N, Koo J, Rosenthal R, Winograd C. Physical therapists’ nonverbal communication predicts geriatric patients’ health outcomes. Psychol Aging. 2002;17(3):443–452. doi: 10.1037/0882-7974.17.3.443. [DOI] [PubMed] [Google Scholar]
- Ambady N, Rosenthal R. Nonverbal Communication. Encyclopedia of Mental Health. 1998;2:775–782. [Google Scholar]
- Ambady N, Weisbuch M. Handbook of Social Psychology. John Wiley & Sons, Inc; 2010. Nonverbal Behavior. [Google Scholar]
- Angie AD, Connelly S, Waples EP, Kligyte V. The influence of discrete emotions on judgement and decision-making: A meta-analytic review. Cognition & Emotion. 2011;25(8):1393–1422. doi: 10.1080/02699931.2010.550751. [DOI] [PubMed] [Google Scholar]
- Armstrong K, Putt M, Halbert CH, Grande D, Schwartz JS, Liao K, … Shea J. Prior experiences of racial discrimination and racial differences in health care system distrust. Medical Care. 2013;51(2):144–150. doi: 10.1097/MLR.0b013e31827310a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bailenson JN, Blascovich J, Beall AC, Loomis JM. Interpersonal distance in immersive virtual environments. Personality and Social Psychology Bulletin. 2003;29:1–15. doi: 10.1177/0146167203029007002. [DOI] [PubMed] [Google Scholar]
- Banse R, Scherer KR. Acoustic profiles in vocal emotion expression. J Pers Soc Psychol. 1996;70(3):614–636. doi: 10.1037//0022-3514.70.3.614. [DOI] [PubMed] [Google Scholar]
- Bessenoff GR, Sherman JW. Automatic and Controlled Components of Prejudice Toward Fat People: Evaluation Versus Stereotype Activation. Social Cognition. 2000;18(4):329–353. [Google Scholar]
- Blascovich J, Loomis J, Beall A, Swinth K, Hoyt C, Bailenson J. Immersive virtual environment technology as a research tool for social psychology. Psychological Inquiry. 2002;13:103–125. [Google Scholar]
- Boersma P, Weenink D. Praat: Doing Phonetics by Computer. 2008 Retrieved from http://www.praat.org/
- Bray M, Loos R, McCaffrey J, Ling C, Franks P, Weinstock G … Group TCW. NIH working group report - using genomic information to guide weight management: From universal to precision treatment. Obesity. 2016;24(1):14–22. doi: 10.1002/oby.21381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brehm S, Brehm J. Psychological Reactance: A Theory of Freedom and Control. New York: Academic Press; 1981. [Google Scholar]
- Crandall C. Prejudice against fat people: Ideology and self-interest. Journal of Personality and Social Psychology. 1994;66:882–894. doi: 10.1037//0022-3514.66.5.882. [DOI] [PubMed] [Google Scholar]
- DeSteno D, Dasgupta N, Bartlett M, Cajdric A. Prejudice from thin air: The effect of emotion on automatic intergroup attitudes. Psychological Science. 2004;15(5):319–324. doi: 10.1111/j.0956-7976.2004.00676.x. [DOI] [PubMed] [Google Scholar]
- Dovidio J, Kawakami K, Johnson C, Johnson B, Howard A. On the Nature of Prejudice: Automatic and Controlled Processes. Journal of Experimental Social Psychology. 1997;33(5):510–540. [Google Scholar]
- Dovidio JF, Hebl M, Richeson J, Shelton J. Nonverbal Communication, Race and Intergroup Interaction. The SAGE Handbook of Nonverbal Communication. 2006;25:481–500. [Google Scholar]
- Dunn J, Schweitzer M. Feeling and believing: The influence of emotion on trust. Journal of Personality and Social Psychology. 2005;88(5):736. doi: 10.1037/0022-3514.88.5.736. [DOI] [PubMed] [Google Scholar]
- Epstein RM, Street RL. Patient-Centered Communication in Cancer Care: Promoting Healing and Reducing Suffering. Bethesda, MD: 2007. (Publication No. 07–6225) [Google Scholar]
- Finset A. “I am worried, doctor!” Emotions in the doctor-patient relationship. Patient Educ Couns. 2012;88(3):359–363. doi: 10.1016/j.pec.2012.06.022. [DOI] [PubMed] [Google Scholar]
- Forgas JP. The role of emotion in social judgments: An introductory review and an affect infusion model (AIM) European Journal of Social Psychology. 1994;24(1):1–24. [Google Scholar]
- Gross J, Levinson R. Emotion elicitation using films. Cognition & Emotion. 1995;9(1):87–108. [Google Scholar]
- Hall JA, Coats EJ, LeBeau LS. Nonverbal behavior and the vertical dimension of social relations: a meta-analysis. Psychol Bull. 2005;131(6):898–924. doi: 10.1037/0033-2909.131.6.898. [DOI] [PubMed] [Google Scholar]
- Hebl M, King E, Perkins A. Ethnic differences in the stigma of obesity: Identification and engagement with the thin ideal. Journal of Experimental Social Psychology. 2009;45(6):1165–1172. [Google Scholar]
- Henry SG, Fuhrel-Forbis A, Rogers MA, Eggly S. Association between nonverbal communication during clinical interactions and outcomes: a systematic review and meta-analysis. Patient Educ Couns. 2012;86(3):297–315. doi: 10.1016/j.pec.2011.07.006. [DOI] [PubMed] [Google Scholar]
- Ko SJ, Sadler MS, Galinsky AD. The Sound of Power: Conveying and Detecting Hierarchical Rank Through Voice. Psychological Science. 2014 doi: 10.1177/0956797614553009. [DOI] [PubMed] [Google Scholar]
- Lerner JS, Keltner D. Beyond valence: Toward a model of emotion-specific influences on judgement and choice. Cognition and Emotion. 2000;14(4):473–493. [Google Scholar]
- Lerner JS, Tiedens L. Portrait of the angry deision maker: How appraisal tendencies shape anger’s influence on cognition. Journal of Behavioral Decision Making. 2006;19(2):115–137. [Google Scholar]
- Levine C, Ambady N. The role of non-verbal behaviour in racial disparities in health care: implications and solutions. Med Educ. 2013;47(9):867–876. doi: 10.1111/medu.12216. [DOI] [PubMed] [Google Scholar]
- Levine LJ, Pizarro DA. Emotion and Memory Research: A Grumpy Overview. Social Cognition. 2004;22(5):530–554. [Google Scholar]
- Loewenstein G, Lerner JS. The role of affect in decision making. In: Davidson RJ, Scherer KR, Goldsmith HH, editors. Handbook of Affective Sciences. Oxford University Press; 2003. [Google Scholar]
- Manolio TA, Chisholm RL, Ozenberger B, Roden DM, Williams MS, Wilson R. Implementing genomic medicine in the clinic: The future is here. Genetics in Medicine. 2013;15(4):258–267. doi: 10.1038/gim.2012.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mast MS. On the importance of nonverbal communication in the physician-patient interaction. Patient Educ Couns. 2007;67(3):315–318. doi: 10.1016/j.pec.2007.03.005. [DOI] [PubMed] [Google Scholar]
- McCall C, Blascovich J, Young A, Persky S. Using immersive virtual environments to measure proxemic behavior and to predict aggression. Social Influence. 2009;4:138–154. [Google Scholar]
- Mehrabian A. Relationship of attitude to seated posture, orientation, and distance. Journal of Personality and Social Psychology. 1968;10(1):26–30. doi: 10.1037/h0026384. [DOI] [PubMed] [Google Scholar]
- Persky S. Employing immersive virtual environments for innovative experiments in health care communication. Patient Educ Couns. 2011;82(3):313–317. doi: 10.1016/j.pec.2010.12.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persky S, Eccleston C. Impact of genetic causal information on medical students’ clinical encounters with an obese virtual patient: Health promotion and social stigma. Annals of Behavioral Medicine. 2011;41(3):363–372. doi: 10.1007/s12160-010-9242-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persky S, Ferrer R, Klein W. Genomic Information may Inhibit Weight-Related Behavior Change Inclinations among Individuals in a Fear State. Annals of Behavioral Medicine. 2016;50(3):452–9. doi: 10.1007/s12160-016-9771-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persky S, Kaphingst K, Allen VJ, Senay I. Effects of patient-provider race concordance and smoking status on lung cancer risk perception accuracy among African-Americans. Annals of Behavioral Medicine. 2013;45(3):308–317. doi: 10.1007/s12160-013-9475-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Persky S, Street RL. Evaluating approaches for communication about genomic influences on body weight. Annals of Behavioral Medicine. 2015;49(5):675–684. doi: 10.1007/s12160-015-9701-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peters N, Rose A, Armstrong K. The Association between Race and Attitudes about Predictive Genetic Testing. Cancer Epidemiology Biomarkers & Prevention. 2004;13(3):361–365. [PubMed] [Google Scholar]
- Prkachin KM, Schultz IZ, Hughes E. Pain behavior and the development of pain-related disability: the importance of guarding. Clin J Pain. 2007;23(3):270–277. doi: 10.1097/AJP.0b013e3180308d28. [DOI] [PubMed] [Google Scholar]
- Puhl RM, Heuer CA. The stigma of obesity: A review and update. Obesity. 2009;17(5):941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- Richeson J, Shelton JN. Brief Report: Thin Slices of Racial Bias. Journal of Nonverbal Behavior. 2005;29(1):75–86. [Google Scholar]
- dRobinson JD. Nonverbal Communication and Physician-Patient Interaction: Review and New Directions. Thousand Oaks, CA: SAGE Publications, Inc; 2006. [Google Scholar]
- Roter DL, Frankel RM, Hall JA, Sluyter D. The expression of emotion through nonverbal behavior in medical visits. Mechanisms and outcomes. J Gen Intern Med. 2006;21(Suppl 1):S28–34. doi: 10.1111/j.1525-1497.2006.00306.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saha S, Komaromy M, Koepsell T, Bindman A. Patient-physician racial concordance and the perceived quality and use of health care. Archives of Internal Medicine. 1999;159(9):997–1004. doi: 10.1001/archinte.159.9.997. [DOI] [PubMed] [Google Scholar]
- Scherer KR. Vocal communication of emotion: A review of research paradigms. Speech Communication. 2003;40(1–2):227–256. [Google Scholar]
- Shelton J, Richeson J. Interracial interactions: A relational approach. Advances in Experimental Social Psychology. 2006;38:121–181. [Google Scholar]
- Smart Richman L, Leary MR. Reactions to discrimination, stigmatization, ostracism, and other forms of interpersonal rejection: a multimotive model. Psychological Review. 2009;116:365–383. doi: 10.1037/a0015250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson HS, Valdimarsdottir HB, Jandorf L, Redd W. Perceived disadvantages and concerns about abuses of genetic testing for cancer risk: differences across African American, Latina and Caucasian women. Patient Educ Couns. 2003;51(3):217–227. doi: 10.1016/s0738-3991(02)00219-7. [DOI] [PubMed] [Google Scholar]
- Weiner B, Perry R, Magnusson J. An attributional analysis of reactions to stigmas. Journal of Personality and Social Psychology. 1998;55(5):736–748. doi: 10.1037//0022-3514.55.5.738. [DOI] [PubMed] [Google Scholar]