Abstract
Although delusions represent one of the core symptoms of psychotic disorders, it is remarkable that few studies have investigated distinct delusional themes. We analyzed data from a large sample of first-episode psychosis patients (n=245) to understand relations between delusion types and demographic and clinical correlates. First, we conducted a principal component analysis (PCA) of the 12 delusion items within the Scale for the Assessment of Positive Symptoms (SAPS). Then, using the domains derived via PCA, we tested a priori and exploratory hypotheses related to delusional content. PCA revealed five distinct components: Delusions of Influence, Grandiose/Religious Delusions, Paranoid Delusions, Negative Affect Delusions (jealousy, and sin or guilt), and Somatic Delusions. The most prevalent type of delusion was Paranoid Delusions, and such delusions were more common at older ages at onset of psychosis. The level of Delusions of Influence was correlated with the severity of hallucinations and negative symptoms. We ascertained a general relationship between different childhood adversities and delusional themes, and a specific relationship between Somatic Delusions and childhood neglect. Moreover, we found higher scores on Delusions of Influence and Negative Affect Delusions among cannabis and stimulant users. Our results support considering delusions as varied experiences with varying prevalences and correlates.
Keywords: Childhood adversities, Delusions, Depression, Drugs of abuse, Hallucinations, Paranoia, Persecutory delusions
1. Introduction
Despite the growing interest in first-episode psychosis, a paucity of research on delusions is noticeable in this area of study (Compton et al., 2012; Rajapakse et al., 2011). It is remarkable how, at the present time, although delusions represent one of the core symptoms of schizophrenia and related psychotic disorders, it remains unclear as to whether or not these phenomena should be considered unitary or diversified (Sass and Byrom, 2015), and few studies have investigated distinct delusional themes, in particular in first-episode psychosis samples.
Moreover, very few studies have focused on possible underlying dimensions of different delusional themes. There has been some interest in detecting the factor structure of psychotic symptoms generally (Emsley et al., 2003; Peralta et al., 2013), and one of the advantages of this analytic approach (i.e., factor analysis) is that it allows for the reduction of heterogeneity in data from a measurement instrument by identifying a group of coherent dimensions. Across different types of available tools measuring delusions, the Scale for the Assessment of Positive Symptoms (SAPS; Andreasen, 1984) has been extensively utilized, and several studies have performed factor analyses in order to identify the latent dimensions amongst its items (e.g., John et al., 2003; Minas et al., 1994; Peralta and Cuesta, 1999; Toomey et al., 1997). Those studies conducted an item-level factor analysis of SAPS items, and they included both delusions and non-delusion items. Conversely, only three studies (Ellersgaard et al., 2014; Kimhy et al., 2005; Vázquez-Barquero et al., 1996) conducted a factor analysis specifically using only the 12 SAPS delusion items. They found three different solutions, respectively composed of five, three, and four factors, meaning that their findings concurred only partially, which could be related to the characteristics of the study samples. Vázquez-Barquero et al. (1996) studied first-episode schizophrenia patients (without severe psychotic symptoms) from a rural community in Cantabria, Spain (n=86; range = 15–54 years). Participants (n=411; range = 18–45 years) included in the study of Ellersgaard et al. (2014) were inpatients and outpatients affected by schizophrenia-spectrum disorders (i.e., not only schizophrenia) coming from the two most populous cities in Denmark (i.e., Copenhagen and Aarhus). Lastly, the study of Kimhy et al. (2005) enrolled antipsychotic-free (for at least 14 days) inpatients (n=83; range = 18–60 years) with diagnoses of schizophrenia/schizoaffective disorder (i.e., not a first-episode psychosis sample) in New York.
Several studies have investigated the prevalence of distinct delusional themes and their correlations with demographic or clinical variables (e.g., Freeman's extensive work on persecutory delusions (e.g., Freeman, 2007; Freeman and Garety, 2014), Startup's work on delusions of reference (e.g., Startup et al., 2009; Startup and Startup, 2005), Langdon and Coltheart's work on bizarre delusions (e.g., Langdon and Coltheart, 2000)). As reported in first-episode psychosis studies by Kim et al. (2011) and Rajapakse et al. (2011), persecutory delusions are the most prevalent type of delusions in this patient population. With respect to sociodemographic variables, first-episode psychosis studies have reported evidence showing a relationship between persecutory delusions and older age at onset (Galdos and van Os, 1995; Häfner et al., 1993), while there is not strong evidence for a relationship between persecutory delusions and sex. According to first-episode psychosis studies by Birchwood et al., 2005 and Drake et al., 2004, as well as findings among chronic patients described by Hartley et al., 2013, persecutory delusions are positively correlated with depression. On the other hand, such delusions are negatively associated with grandiose delusions, as reported by Garety et al., 2013 (though this study also did not involve first-episode psychosis patients in particular). Furthermore, persecutory delusions have been proven to be related to cannabis use in the general population (Freeman et al., 2011; Freeman et al., 2013).
In this study, we made use of in-depth clinical research data from a large sample of hospitalized first-episode psychosis patients to test hypotheses related to delusional thought content. We had three objectives. The first was to conduct a principal component analysis (PCA) of the 12 delusion items of the SAPS. Second, we tested three a priori hypotheses. Third, we examined three exploratory research questions. In testing a priori and exploratory hypotheses, we planned to use the extracted domains from the PCA.
With regard to PCA, given differences in the socio-demographic characteristics of prior studies (Ellersgaard et al., 2014; Kimhy et al., 2005; Vázquez-Barquero et al., 1996) and the limited literature available, such a factor analysis was warranted in our sample. Specifically, factor analysis of the 12 delusion items has never been performed among a hospitalized, predominantly African American, male, low income, and socially disadvantaged sample. Thus, rather than relying on results from different first-episode samples from other countries and settings, we first wanted to examine the factor structure in our unique sample.
Similar purposes guided our first a priori hypothesis; we investigated the prevalence of delusions, and in particular the prevalence of different delusional themes. We hypothesized that persecutory delusions would be the most prevalent type. Although the finding of persecutory delusions as the most prevalent type of delusions has been replicated, we wanted to prove this finding in our unique sample. Based on the limited prior literature, we second hypothesized that patients with persecutory delusions would be older in age at onset, but that there would be no particular relationships with sex. Finally, we also had the a priori hypothesis that depression would be linked positively with persecutory delusions and negatively with grandiose delusions.
After testing our hypotheses, we carried out exploratory analyses again based on limited previous research not specifically involving first-episode psychosis patients. First, we explored the relationship between the total scores on the extracted delusion domains and the SAPS hallucinations total score, as well as the Scale for the Assessment of Negative Symptoms (SANS; Andreasen, 1983) total score. Second, we explored whether greater childhood adversity would be associated with a greater severity of one or more of the various types of delusional thought content. Third, based on the aforementioned Freeman et al. studies (2011 (2013), we explored how cannabis use is related to delusional content (i.e., persecutory delusions, as well as the other types of delusions included in our sample), and also how the use of other drugs is associated with delusional content.
2. Method
2.1. Participants and Procedure
Patients were selected using a preexisting database of 247 consecutively admitted patients with first-episode psychosis (see Birnbaun et al., 2015; Fresan et al., 2015; Kelley et al., 2015 for detailed information regarding recruitment sites, eligibility criteria, and assessment procedures). All patients met the following inclusion criteria: (1) were English-speaking, (2) were within the age range of 18–40 years, (3) did not have known or suspected mental retardation, (4) had a Mini-Mental State Examination (Folstein et al., 1975, Cockrell and Folstein, 1988) score of ≥24, (5) did not have a significant medical condition compromising ability to participate, and (6) were able to provide informed consent. All patients were considered “first-episode” in that they had never been hospitalized for psychosis prior to three months before their index hospitalization (for most, this was the very first hospitalization) and they had received less than three months of treatment with an antipsychotic (for most, they had never been treated with an antipsychotic prior to index hospitalization). Having full data on the SAPS was the criterion for extraction from the previous database and inclusion in the present one; only two patients were excluded for missing values (resulting in n=245).
2.2. Assessments
Patients were administered an extensive battery to evaluate diverse clinical variables, psychopathology, and diagnosis. The SAPS was used to assess hallucinations, delusions, bizarre behavior, and positive formal thought disorder (Andreasen, 1984). The SANS was used to assess affective flattening or blunting, alogia, avolition-apathy, anhedonia-asociality, and attention (Andreasen, 1983). The SAPS has 34 items, including the 12 types of delusions, while the SANS includes 25 items. Items on both scales are rated 0–5 (“none,” “questionable,” “mild,” “moderate,” “marked,” “severe”). Test-retest reliability and construct validity have been demonstrated for both instruments previously (Rogers, 2001) and in the current sample (see Birnbaum et al., 2015). Moreover, the Positive and Negative Syndrome Scale (PANSS) was used as global symptom severity measure (Kay et al., 1987). The PANSS depression item was used as a measure of depression severity, as it has been shown to give a valid approximation of depression in patients with schizophrenia (El Yazaji et al., 2002). Diagnoses of psychotic disorders and substance-related disorders were assessed using the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID; First et al., 1998).
Childhood adversity was assessed using seven instruments: the Childhood Trauma Questionnaire–Short Form (CTQ-SF; Bernstein et al., 2003), Trauma Experiences Checklist (TEC; Cristofaro et al., 2013), Parental Nurturance (Barnes and Windle, 1987), Parental Harsh Discipline (Ge et al., 1994; Mrug et al., 2008), Violence Exposure (Mrug et al., 2008), Friends' Delinquent Behavior (Mrug et al., 2012), and School Connectedness Scale (Sieving et al., 2001). In the present analysis, in order to reduce the subscales of these measures of childhood adversity to their latent constructs, we relied on factors derived from a previously conducted factor analysis in this sample (McGuire et al., in progress). The factors from the resulting model were named Environmental Violence (which included Violence Exposure at school, Violence Exposure in the neighborhood, Friends' Delinquent Behavior, TEC – Violence, Death, and Legal Involvement; i.e., scales pertaining to extreme risk, danger, and violence exposure), Interpersonal Abuse (including CTQ – physical abuse, CTQ – emotional abuse, CTQ – sexual abuse, TEC – Interpersonal Abuse and Family Stress, Parental Harsh Discipline, Violence Exposure at home; i.e., scales tapping abuse and harsh conditions in the family or at home), and Neglect (which included CTQ – emotional neglect, Parental Nurturance, School Connectedness, CTQ – physical neglect; i.e., scales referring to physical/emotional neglect and lack of connectedness or support at home and school).
2.3. Data Analysis
Descriptive statistics and distributional properties of all variables of interest were first examined. Thereafter, the 12 delusion items of the SAPS were subjected to a Principal Component Analysis (PCA) in order to identify any latent or underlying dimensions within the items. The analysis had exploratory (rather than confirmatory) objectives.
Prior to performing PCA, we verified the applicability of the data for the analysis. The case-to-variable ratio was 20.4 (which well exceeds the recommended minimum of 10; Nunnally, 1978), indicating adequacy of the sample size. The Kaiser-Meyer-Olkin sampling adequacy measure was 0.709 (the recommended value being ≥0.6), and the Bartlett's Test of Sphericity was significant, both of which supported the factorability of the correlation matrix. Eigenvalues >1.0 were chosen as the criterion for factor extraction. Components were rotated using Varimax rotation. A minimum factor loading of 0.3 was deemed to indicate a meaningful loading and for including each item on the respective component.
Then, in reference to the hypotheses and exploratory analyses previously described, we analyzed the relationship between each extracted delusion domain identified via PCA and sociodemographic and clinical variables. Notably, in stating our hypotheses above, we referred to a specific type of delusions (e.g., persecutory delusions), though in testing the hypothesis we used the PCA-derived domain containing that specific type of delusions (i.e., even if it is not the only type of delusion loading on that domain). All hypothesis tests and exploratory analyses were carried out using chi-square tests, Mann-Whitney U tests, analysis of variance (ANOVA), and Pearson or Spearman correlations, as appropriate, using IBM SPSS Statistics version 21.0.
3. Results
3.1. Sociodemographic Analysis
Sociodemographic features, as well as diagnoses of psychotic disorders and substance use disorders, are summarized in Table 1. Of the 245 subjects, 182 were men and 63 were women. The mean age was 23.9±4.7 years (range = 18–39 years). Regarding race, the majority of patients were African American (86.1%). Schizophrenia was the most common SCID-based diagnosis (57.6%). In Table 2, we report the frequency of each SAPS delusion item. A score of ≥2 (mild) was chosen as requisite for including a patient in the respective delusional theme category. Remarkably, a total of 235 patients (95.9%) manifested at least one type of delusion. The three most common delusion items with a ≥2 (mild) score were: persecutory (182, 74.3%), reference (165, 67.4%), and grandiose (113, 46.2%). The three least common were somatic (44, 18.0%), sin or guilt (32, 13.0%), and jealousy (25, 10.2%).
Table 1. Sociodemographic Characteristics of the Study Sample (n=245).
| Total | M | SD |
|---|---|---|
| Mean age | 23.9 | 4.7 |
| Years of school completed | 11.9 | 2.2 |
|
| ||
| n | % | |
|
| ||
| Male | 182 | 74.3 |
| Admission Legal status | ||
| Voluntary | 59 | 24.1 |
| Race | ||
| Asian | 4 | 1.6 |
| African American | 211 | 86.1 |
| White | 19 | 7.8 |
| Other | 11 | 4.5 |
| Marital status (n =244) | ||
| Single, never married | 211 | 86.1 |
| Married or living with a partner | 12 | 4.9 |
| Separated | 12 | 4.9 |
| Divorced | 8 | 3.3 |
| Widowed | 1 | 0.4 |
| Being a parent (n=244) | 74 | 30.2 |
| Living conditions | ||
| Alone | 16 | 6.5 |
| Parents, siblings, other family | 160 | 65.3 |
| Boyfriend or girlfriend | 10 | 4.1 |
| Spouse or partner | 7 | 2.9 |
| Friends | 10 | 5.3 |
| Structured living arrangement | 2 | 0.8 |
| Homeless | 24 | 9.8 |
| Other | 13 | 5.3 |
| Brought up with | ||
| Mother | 110 | 44.9 |
| Father | 15 | 6.1 |
| Both parents | 72 | 29.4 |
| Other family members | 39 | 15.9 |
| Foster family | 4 | 1.6 |
| Other | 5 | 2.0 |
| Currently employed | 76 | 31.0 |
| Religious affiliation | ||
| Baptist | 91 | 37.1 |
| Other Protestant | 61 | 24.9 |
| Catholic | 12 | 4.9 |
| Muslim | 11 | 4.5 |
| None or Agnostic | 33 | 13.5 |
| Other | 37 | 15.1 |
| Been incarcerated (n=234) | 136 | 55.5 |
| SCID substance-related disorders diagnosis | ||
| Alcohol abuse/dependence (n=232) | 68 | 27.7 |
| Current abuse | 11 | 4.5 |
| Lifetime abuse (past 5 years) | 12 | 4.9 |
| Current dependence | 27 | 11.0 |
| Lifetime dependence (past 5 years) | 18 | 7.3 |
| Cannabis abuse/dependence (n=231) | 147 | 59.9 |
| Current abuse | 25 | 10.2 |
| Lifetime abuse (past 5 years) | 18 | 7.3 |
| Current dependence | 76 | 31.0 |
| Lifetime dependence (past 5 years) | 28 | 11.4 |
| Cocaine abuse/dependence (n=234) | 20 | 8.1 |
| Current abuse | 2 | 0.8 |
| Lifetime abuse (past 5 years) | 4 | 1.6 |
| Current dependence | 9 | 3.7 |
| Lifetime dependence (past 5 years) | 5 | 2.0 |
| Other substances abuse/dependence (n=234) | 31 | 12.7 |
| Current abuse | 5 | 2.0 |
| Lifetime abuse (past 5 years) | 7 | 2.9 |
| Current dependence | 12 | 4.9 |
| Lifetime dependence (past 5 years) | 7 | 2.9 |
| SCID diagnosis | ||
| Schizophrenia | 141 | 57.6 |
| Paranoid | 95 | 38.8 |
| Catatonic | 2 | 0.8 |
| Disorganized | 11 | 4.5 |
| Undifferentiated | 33 | 13.5 |
| Schizophreniform Disorder | 29 | 11.8 |
| Psychotic Disorder NOS | 38 | 15.5 |
| Schizoaffective Disorder | 31 | 12.6 |
| Bipolar | 5 | 2.0 |
| Depressive | 26 | 10.6 |
| Brief Psychotic Disorder | 2 | 0.8 |
| Delusional Disorder | 4 | 1.6 |
Table 2. Descriptive Statistics of SAPS Delusion Items, and Principal Component Analysis Results.
| Factorsa and Factor Loadings | |||||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| SAPS item delusion | n (%) ≥ 2 (mild) | mean±SD | 1 | 2 | 3 | 4 | 5 |
| Persecutory | 182 (74.3) | 2.64±1.60 | 0.10 | -0.20 | 0.78* | 0.05 | 0.11 |
| Jealousy | 25 (10.2) | 0.27±0.69 | -0.03 | 0.08 | 0.24 | 0.48* | -0.09 |
| Sin or Guilt | 32 (13.0) | 0.47±0.93 | 0.04 | -0.02 | -0.01 | 0.86* | 0.11 |
| Grandiose | 113 (46.2) | 1.39±1.44 | 0.06 | 0.77* | 0.16 | -0.18 | 0.22 |
| Religious | 87 (35.6) | 1.19±1.52 | 0.14 | 0.71* | -0.19 | 0.33 | -0.03 |
| Somatic | 44 (18.0) | 0.73±1.34 | 0.08 | 0.08 | 0.02 | 0.02 | 0.93* |
| Reference | 165 (67.4) | 2.44±1.78 | 0.05 | 0.34 | 0.74* | 0.18 | -0.10 |
| Being Controlled | 83 (33.9) | 1.09±1.42 | 0.69* | 0.05 | 0.02 | 0.20 | 0.20 |
| Mind Reading | 110 (44.9) | 1.53±1.68 | 0.48* | 0.51 | 0.12 | 0.05 | -0.18 |
| Thought Broadcasting | 84 (34.2) | 1.20±1.54 | 0.72* | 0.12 | 0.18 | 0.01 | -0.12 |
| Thought Insertion | 71 (29.0) | 1.00±1.39 | 0.73* | 0.05 | 0.05 | -0.07 | 0.01 |
| Thought Withdrawal | 47 (19.2) | 0.63±1.19 | 0.77* | 0.08 | -0.08 | -0.07 | 0.09 |
|
| |||||||
| Eigenvalues | 2.83 | 1.41 | 1.20 | 1.04 | 1.00 | ||
|
| |||||||
| Explained variance (%) | 23.6 | 11.7 | 10.0 | 8.6 | 8.4 | ||
Factor 1 was named “Delusions of Influence”; Factor 2 was named “Grandiose/Religious Delusions”; Factor 3 was named “Paranoid Delusions”; Factor 4 was named “Negative Affect Delusions”; Factor 5 was named “Somatic Delusions” Factor loadings > 0.40 are in boldface.
Items loading on the respective factor.
3.2. Principal Component Analysis
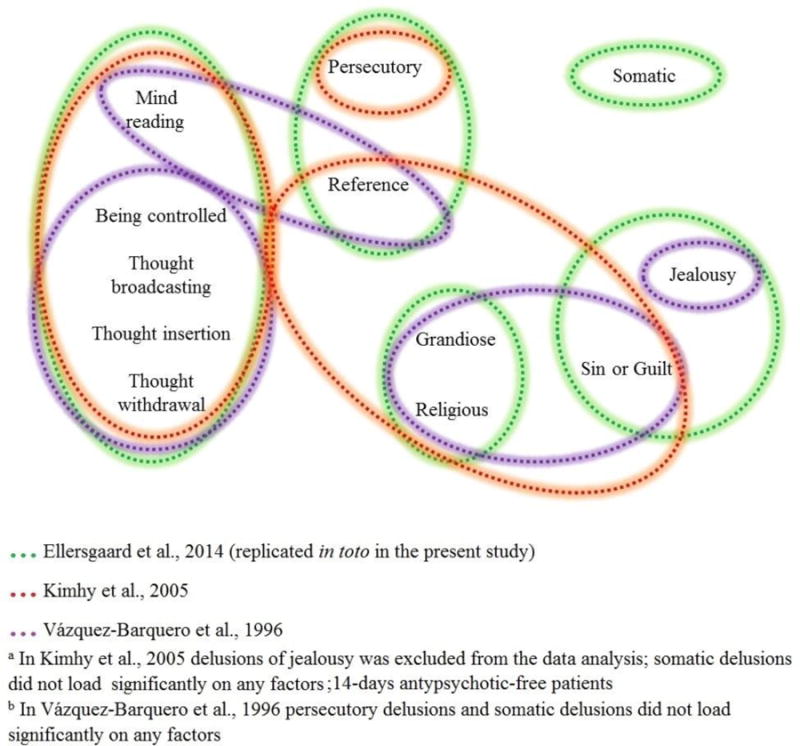
PCA revealed five distinct components with eigenvalues >1, explaining 62.4% of the total variance. As shown in Table 2, the delusions of being controlled, mind reading, thought broadcasting, thought insertion, and thought withdrawal loaded significantly on factor 1, hereafter referred to as Delusions of Influence, in line with Kimhy et al. (2005). Grandiose and religious delusions comprised factor 2, hereafter called Grandiose/Religious Delusions. Persecutory delusion as well as delusions of reference made up factor 3; Startup and Startup (2005) already showed an association between persecutory delusions and one of the two form of delusions of reference they recognize (i.e., referential delusions of observation). This factor is subsequently referred to as Paranoid Delusions. Delusions of jealousy and of sin or guilt loaded onto factor 4, subsequently named Negative Affect Delusions. Only the somatic delusion item loaded significantly as factor 5 and we consequently referred to it as Somatic Delusions. Notably, delusions of mind reading loaded on factor 2 (0.51) in addition to factor 1 (0.48). However, in considering the previous study of Ellersgaard et al. (2014), and taking into consideration the clinical overlap between delusions of mind reading and delusions of being controlled, thought broadcasting, thought insertion, and thought withdrawal, (which all loaded onto factor 1), we decided to include delusions of mind reading in factor 1 rather than factor 2. The SAPS scores composing the five extracted delusion factors are summarized in Table 3. A visual comparison of our derived domains, in relation to the results of Ellersgaard et al. (2014), Kimhy et al. (2005) and Vázquez-Barquero et al. (1996) is given in Figure 1.
Table 3. Descriptive Statistics for the Five PCA-Derived Domains (or “Subscales”) of Delusions.
| Subscale based on factor analysis | Possible subscale score range | Observed subscale score range | Mean±SD subscale score | Standardized Mean±SD* | N (%) ≥2 (mild) |
|---|---|---|---|---|---|
| Delusions of Influence | 0–25 | 0–20 | 5.45±5.05 | 1.09±1.01 | 49 (20.0) |
| Grandiose/Religious Delusions | 0-10 | 0-10 | 2.58±2.41 | 1.29±1.21 | 76 (31.0) |
| Paranoid Delusions | 0-10 | 0-10 | 5.08±2.70 | 2.54±1.35 | 177 (72.2) |
| Negative Affect Delusions | 0-10 | 0-7 | 0.75±1.21 | 0.38±0.61 | 6 (2.4) |
| Somatic Delusions | 0-5 | 0-5 | 0.73±1.36 | 0.73±1.36 | 44 (18.0) |
The “standardized score” refers to the mean subscale score divided by the number of items in the subscale.
Figure 1. A visual comparison of our derived domains, in relation to the results of the only previous studies which have investigated dimensions underling the 12 SAPS delusion items by conducting an item-level PCA.
By categorizing patients on the basis of the highest standardized domain scores (minimum score value ≥2), it was possible to identify a predominant delusional theme for 181 participants (73.9%): 129 (71.3%) presented with Paranoid Delusions as the predominant theme, 21 (11.6%) with Somatic Delusions, 20 (11.0%) with Grandiose/Religious Delusions, and 11 (6.1%) with Delusions of Influence. None of them presented Negative Affect Delusions as predominant theme. Otherwise, for 64 patients (26.1%), it was not possible to identify a predominant delusional theme (i.e., no scores ≥2 in any of the domains or equal scores in two or more domains).
3.3. Testing of A Priori Hypotheses
As hypothesized, we found a significant difference between the percentages of different types of delusions (χ2=208.02; df=3; p<0.001). Also as hypothesized, no significant relationship was found between gender and the presence of Paranoid Delusions (131 (72.0%) of males and 46 (73.0%) of females; χ2=0.03; df=1; p=0.874).
With regard to our hypothesis pertaining to age, our data supported the expectation that patients with persecutory delusions would be older in age at onset: 22.1±5.2 (median of 21.6) among the 167 patients with Paranoid Delusions, compared to 20.4±4.0 (median of 20.6) among the 55 patients without Paranoid Delusions (Mann-Whitney U-test p=0.010). When age by sex was checked, no significant interaction was found with respect to Paranoid Delusions (F=0.138; df=1, 217; p=0.711). Moreover, the severity of Paranoid Delusions was correlated, though modestly, with age at onset (ρ=0.136; p=0.043). Interestingly, when we performed the same correlation with age at hospitalization instead of age at onset (as another approach to the above Mann-Whitney U test), the magnitude was higher (ρ=0.211; p=0.001). Redoing this Spearman correlation in two subsamples based on a median split by age (to determine whether the correlation was more apparent among younger or older patients), revealed a correlation of ρ=0.046 (p=0.617) in those 18–22 years of age (n=119), and ρ=0.104 (p=0.244) in those 23–40 years of age (n=128).
With regard to our hypothesis pertaining to the correlations—positive and negative, respectively—between depression and persecutory delusions and grandiose delusions, our results did not confirm our expectations: no significant correlation was observed between depression and Paranoid Delusions (ρ=0.042; p=0.516) or between depression and Grandiose/Religious Delusions (ρ= -0.121; p=0.059).
3.4. Exploratory Analyses
Results of correlation analyses pertaining to the delusion domains and SAPS hallucinations scale, SANS total score, and the three childhood adversity factors are summarized in Table 4. The magnitude of correlations between hallucinations and Delusions of Influence (ρ=0.485; p <0.001) was more than double the magnitude of correlation showed by any other delusion domain. Delusions of Influence was the only domain correlated with negative symptoms (ρ=0.214; p=0.001). Environmental Violence and Interpersonal Abuse correlated significantly with all delusional themes revealed by the PCA (except for the nonsignificant relationship between Environmental Violence and Somatic Delusions); though the degree of correlations was overall modest. Somatic Delusions was the only domain showing a correlation with Neglect.
Table 4. Correlation between the Five PCA-Derived Domains and Hallucinations, SANS Global Score, and Three Aspects of Childhood Adversity.
| Hallucinationsa | SANS Total Scoreb | Environmental Violencec | Interpersonal Abusec | Neglectc | |
|---|---|---|---|---|---|
| Delusion of Influence | 0.485** | 0.214** | 0.179* | 0.234** | 0.033 |
| Grandiose/Religious Delusions | 0.107 | -0.040 | 0.236** | 0.196* | -0.064 |
| Paranoid Delusions | 0.162* | -0.081 | 0.172* | d0.200** | 0.045 |
| Negative Affect Delusions | 0.197** | 0.020 | 0.202** | 0.284** | 0.072 |
| Somatic Delusions | 0.146* | 0.123 | -0.048 | 0.164* | 0.259** |
Indicates the total score of SAPS hallucinations scale
Indicates the SANS total score
Environmental Violence, Interpersonal Abuse, Neglect represent the factors used to describe childhood adversity
The correlation between Interpersonal Abuse and Paranoid Delusion is the only case of Pearson Correlation (r; i.e., both variables were normally distributed); in all the other cases Spearman correlation (ρ) was provided.
p < 0.05;
p < 0.01
With regard to the relationship between delusional themes and substances of abuse, we grouped the abuse/dependence of each substance into three categories: no abuse/dependence, current or lifetime abuse, and current or lifetime dependence. Moreover, we combined the two groups of cocaine abuse/dependence and other substance (e.g., ecstasy, methamphetamine, PCP) abuse/dependence. No statistically significant difference was found in scores on each delusion domain between subjects with no abuse/dependence (n=164), alcohol abuse (n=23), and alcohol dependence (n=45); all five F values were <1.50, all p>0.22). With regard to cannabis use (no abuse/dependence n=84, abuse n=43, dependence n=104), a statistically significant difference was found in scores on Delusions of Influence (no abuse/dependence: 0.8±0.9, current or lifetime abuse: 1.2±1.0, current or lifetime dependence: 1.4±1.1; F=8.505, df=2, 228, p<0.001) and on Negative Affect Delusions (no abuse/dependence: 0.3±0.6, current or lifetime abuse: 0.4±0.7, current or lifetime dependence: 0.5±0.7; F=3.333, df=2, 228, p=0.037). On the other hand, cannabis use category was not associated with severity of Grandiose/Religious Delusions (F=2.066, df=2, 228, p=0.129), Paranoid Delusions (F=1.820, df=2, 228, p=0.164) or Somatic Delusions (F=1.929, df=2, 228, p=0.148). Similarly, regarding cocaine/other substance use (no abuse/dependence n=191, abuse n=16, dependence n=27), a statistically significant difference was found in scores on Delusions of Influence (no abuse/dependence: 1.0±1.0, current or lifetime abuse: 1.7±1.1, current or lifetime dependence: 1.3±1.1; F=3.262, df=2, 231, p=0.040) and on Negative Affect Delusions (no abuse/dependence: 0.3±0.5, current or lifetime abuse: 0.4±0.6, current or lifetime dependence: 0.7±0.9; F=3.404, df=2, 231, p=0.035). The cocaine/other drug use category was not significantly related to severity of Grandiose/Religious Delusions (F=0.497, df=2, 231, p=0.609), Paranoid Delusions (F=0.168, df=2, 231, p=0.846), or Somatic Delusions (F=0.668, df=2, 231, p=0.514).
4. Discussion
To the best of our knowledge, only two studies have investigated dimensions underling the 12 SAPS delusion items by conducting an item-level PCA in a first-episode psychosis sample (Ellersgaard et al., 2014; Vázquez-Barquero et al., 1996). Our PCA findings replicate in toto the result of Ellersgaard et al. (2014): the same items grouped into the same five factors. In Vázquez-Barquero et al. (1996), a PCA of SAPS delusion items revealed four factors. Delusions of being controlled, thought broadcasting, thought insertion, and thought withdrawal loaded on the first factor; grandiose delusions, religious delusions, and delusions of sin or guilt loaded on the second; delusions of mind reading and delusions of reference loaded on the third; and delusions of jealousy loaded alone on the fourth factor. One additional PCA has been conducted, though not in a first-episode psychosis sample (Kimhy et al., 2005), revealing three factors. Factor 1 (Delusions of Influence) consisted of the same delusion items as our Delusions of Influence. Factor 2 (Delusions of Self-Significance) consisted of delusions of grandeur, reference, guilt/sin, and religious delusions. Factor 3 (Delusions of Persecution) consisted only of persecutory delusions. Referring to the abovementioned studies, delusion of being controlled, mind reading, thought insertion, thought broadcasting, and thought withdrawal consistently load on a recognizable factor (Ellersgaard et al., 2014; Kimhy et al., 2005), with the exception of Vázquez-Barquero et al., 1996, in which delusions of mind reading loaded on a distinct factor. Similarly, grandiose and religious delusions load together on a distinct factor (Ellersgaard et al., 2014) or along with delusions of sin or guilt (Vázquez-Barquero et al., 1996), or along with delusions of sin or guilt and reference (Kimhy et al., 2005). Somatic delusions load alone (Ellersgaard et al., 2014) or do not load on any factors (Kimhy et al., 2005; Vázquez-Barquero et al., 1996). It is remarkable that the only two studies conducting a factor analysis of SAPS delusion items in an adequately large first-episode psychosis sample (n=245, our study; n=411, Ellersgaard et al., 2014) revealed exactly the same results. The non-first-episode sample (Kimhy et al., 2005), the small samples (n=83, Kimhy et al., 2005; n=86 Vázquez-Barquero et al., 1996), as well as the different sociodemographic features (see the Introduction), could account for the discrepancies between these factor analytic studies and our results. These findings mean that the relationships among the SAPS delusion items that we found are overall consistent with previous studies (see Figure 1). Of note, one other study (Shtasel et al., 1992) conducted an item-level factor analysis in a first-episode sample, but included items of the SAPS, SANS, and Brief Psychiatric Rating Scale, and other studies have done factor analyses of SAPS items but included items other than delusions in a non-first-episode sample (e.g., Arora et al., 1999; John et al., 2003; Minas et al., 1994; Lin et al., 1998; Peralta and Cuesta, 1999; Toomey et al., 1997).
With regards to our a priori hypotheses, first, we confirmed that the persecutory delusions domain is the most prevalent, which is in line with all prior studies using the SAPS (Kim et al., 2001) or other instruments (e.g., Jørgensen and Jensen, 1994; Rajapakse et al., 2011; Raune et al., 2006) in first-episode psychosis. The majority of previous studies focused on putative underlying factors leading to the genesis and maintenance of persecutory delusions (e.g., reviews of Bentall et al., 2001 and Freeman, 2007), and they generally agree with a multidimensional model involving both external precipitating events and reasoning biases. Yet, the exact reasons why Paranoid Delusions are the most common type of delusions, irrespective of socio-cultural context (Stompe et al., 1999; Skodlar et al., 2008), are unclear. In Stompe et al. (1999), despite the fact that cultural factors substantially influence delusional content—as shown by the different prevalence of specific delusional themes in Austrian and Pakistani samples—persecutory delusions were the most prevalent type of delusions in both countries and their prevalences were not significantly different. Similarly, in Skodlar et al. (2008), persecutory delusions, along with delusions of reference (i.e., our Paranoid Delusions domain), are the most frequent type of delusions from 1881 to 2000. Moreover, the prevalence of Paranoid Delusion, according to that report, increased over time, but the impact of social-cultural changes affect this type of delusions less than other types. Therefore, despite the influence of socio-cultural events, paranoid delusions seem to be less susceptible to such influence, and the most constant and prevalent across time and culture, which may mean that they are linked to basic brain responses to environmental stress. We hypothesize that paranoid thinking is a defense mechanism in response to chronic mental stress, leading to paranoid delusions in individuals showing a certain vulnerability. Further research is needed to address whether paranoid delusions could be innately and evolutionarily linked to response to stressors.
Second, the presence and the severity of Paranoid Delusions was modestly associated with older age, but was not associated with sex. Our results seem to be similar to first-episode psychosis findings reported by Häfner et al. (1993), who found persecutory delusions to be more frequent at older ages regardless of sex, and by Galdos and van Os (1995) who found an increased likelihood of displaying persecutory delusions with age in both sexes. They suggest (Galdos and van Os, 1995), in keeping with Frith (1994), that the distinction between accidental and intentional behavior is part of a maturational process; therefore, persecutory delusions cannot be displayed unless the ability of inferring intentions of others is completely developed. Such interpretation agrees with the findings of Häfner et al. (1993), who reported the tendency toward undifferentiated delusions in adolescence compared to systematized persecutory delusions in adulthood. Freeman (2007) described a multifactorial cognitive model of persecutory delusions in which developing delusions requires biases in reasoning involving the ability to correctly interpret mental states of others, so that it seems to be feasible that the relationship between persecutory delusions and older age is linked with the altered maturation of that process (i.e., the acquisition of the ability of inferring others' mental states accompanied by deficits in correctly interpreting such states). Said hypothesis seems to agree with the correlation we found between severity of Paranoid Delusions and both age of onset and with age in general. However, within our sample with a restricted age range, the correlation was not observed among only the younger participants (18–22 years), but rather across the entire age range (18–40 years).
Third, our results do not confirm a significant relationship between depression and delusional themes; neither positively with Paranoid Delusions, nor negatively with Grandiose/Religious Delusions. The review of Hartley et al. (2013), and both first-episode (Birchwood et al., 2005; Drake et al., 2004) and non-first-episode (e.g., Bentall et al., 2009; Chadwick et al., 2005; Green et al., 2006) studies, have previously reported a relationship between depression and persecutory ideation. However, all cited studies included in their samples persecutory deluded patients or provided a measure exclusively of persecutory delusions or paranoid ideation and no other delusional themes. Only the studies of Garety et al. (2013) and Smith et al. (2006) measured grandiose delusions in addition to persecutory delusions (but no other delusional themes) and found a positive relationship between persecutory delusions and depression and a negative one between grandiose delusions and depression. On account of the limited research exploring different delusional themes, our results comply with Hartley et al. (2013)—conclusions cannot yet be drawn about the relationship between specific types of delusions and depression, particularly in a first-episode sample.
With regard to our exploratory analyses, Delusions of Influence were much more correlated with the severity of hallucinations and negative symptoms compared to the other domains of delusions. There have been remarkably few studies addressing the relationship between specific delusional themes and other domains of psychopathology. The only study performing similar analyses (i.e., between extracted factors among 12 SAPS delusion items and other SAPS/SANS scores) (Kimhy et al., 2005) similarly found a significant relationship between delusions of influence (composed of the same five delusion items as our Delusions of Influence) and hallucinations (a correlation of 0.46, similar to our 0.49) as well as the SANS subscale of avolition/apathy. Of note, these two associations would seem to be unique, non-redundant associations because the correlation between hallucination severity and negative symptom severity was modest (ρ=0.24). Bias toward attributing self/other-generated experiences have been proposed respectively for hallucinations (Woodward et al., 2007) and Delusions of Influence (Woodward et al., 2006). It is conceivable that these source-monitoring biases share overlapping cognitive operations leading to the associations between Delusions of Influence and hallucinations.
Then, we found a widespread relationship between childhood adversities and delusional themes, in line with a recent meta-analysis reporting an association with an increased risk of psychosis associated with a wide range of adverse childhood experiences (Matheson et al., 2013; Varese et al., 2012). There is growing interest focusing on putative relationships between specific childhood adversities and specific psychotic symptoms (Bentall et al., 2014). With regards to delusions, a specific relationship between persecutory delusions and physical abuse has been suggested (Bentall et al., 2012; Rajkumar, 2015). However, such findings have not been replicated (Longden et al., 2015; Read et al., 2003; Uçok and Bıkmaz, 2007; van Nierop et al., 2014), and a more global model of associations, in which no differential associations between particular adversities and specific delusions exists, has been proposed (Longden et al., 2015). Whereas Interpersonal Abuse was modestly correlated with the severity of all five types of delusions, Environmental Violence was modestly correlated with the severity of four of them (all but Somatic Delusions). However, we found that Neglect was correlated only with Somatic Delusions. Therefore, we could hypothesize that experiencing violence “outside the house” or serious danger events (Environmental Violence), as well as experiencing violence “inside the house” or being abused (Interpersonal Abuse), could generally increase risk for delusional ideation. On the other hand, Neglect is instead particularly linked with Somatic Delusions.
Finally, looking at the relationship between delusional themes and substance abuse/dependence, remarkably, we found a significant progressive increase of severity of Delusions of Influence and Negative Affect Delusions in patients who did not take drugs, who abused, and who were dependent on cannabis and cocaine/other substances. Few studies have focused on the presence of specific delusional themes, generally reporting an increased incidence of persecutory/paranoid ideation among cannabis (Freeman et al., 2011; Freeman et al., 2013), methamphetamine (Ali et al., 2010; Zweben et al., 2004), or cocaine (Brady et al., 1991) users, though these studies primarily focused on substance users and not patients with psychotic disorders. Meanwhile, our results suggest a linear relationship between the severity of cannabis and cocaine/other drug use (but not alcohol use) and the severity of specific non-paranoid delusions in first-episode psychosis patients. Although a clear distinction between substance-induced psychosis and primary psychotic disorders is still challenged (Hides et al., 2015; Mathias et al., 2008), we could hypothesize that paranoid ideation relates to substance-induced psychosis, while Delusions of Influence and Negative Affect Delusions could be particular correlates of substance use among those with a primary psychotic disorder. This distinction, if confirmed, could possibly help clinically in distinguishing the two conditions.
Our study is subject to a number of limitations. First, our measure of depression consisted only of the depression item from the PANSS; to truly test that hypothesis, we would need to measure depression in a much more extensive way. Future studies should rely on depression scales with greater variability. Second, we chose an exploratory factor analysis (rather than confirmatory) since the limited literature available (coming from different samples in different settings/countries) did not allow us to clearly identify a pre-defined model to confirm; nonetheless, we replicated a previously reported model (e.g., Ellersgaard et al., 2014). Third, the varimax rotation used in our exploratory approach assumes that the different factors are orthogonal, which makes it impossible to test for associations between covariates (i.e., the different types of delusions). Therefore, our analytic strategy might have underestimated differential effects of specific types of delusions as several patients had more than one type of delusions of different severity (e.g., patients presenting Paranoid Delusions as a predominant theme likely display also other types of delusions as a secondary theme). Fourth, all demographic and clinical variables (e.g., depression severity, experiences of childhood adversity) were based on the patient's self-report, and delusion items were rated based on present and past-month symptomatology only. Further work could incorporate objective measures and longitudinal ratings of delusions.
Delusions are a heterogeneous phenomenon. It seems to be unlikely that distinct delusional themes share exactly the same clinical features; likewise, it is unlikely that different variables affect delusional thoughts irrespective of their contents. Our results support considering delusions not as a unitary construct, but rather as different experiences with varying prevalences and correlates. Further research is needed in order to more fully unpack the heterogeneity of these phenomena. Improved knowledge in this area could lead to a better understanding of the mechanisms involved in the genesis of delusions and offer clinical insights in terms of tailoring therapies.
Highlights.
Paranoid Delusions is the most prevalent type of delusion, and such delusions are more common at older ages at onset of psychosis
The level of Delusions of Influence is correlated with the severity of hallucinations and negative symptoms
Childhood Neglect is correlated with Somatic Delusions, while Environmental Violence and Interpersonal Abuse showed a correlation with the majority of our delusion domains
Cannabis and stimulant users have higher scores on Delusions of Influence and Negative Affect Delusions (jealousy, and sin or guilt)
Acknowledgments
Research reported in this publication was supported by National Institute of Mental Health grant R01 MH081011 (“First-Episode Psychosis and Pre-Onset Cannabis Use”) to the last author. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or National Institute of Mental Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting galley proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ali R, Marsden J, Srisurapanont M, Agueda S, Baigent M, Monteiro M. Methamphetamine psychosis in Australia, Philippines, and Thailand: recommendations for acute care and clinical inpatient management. Addict Disord Their Treat. 2010;9:143–9. [Google Scholar]
- Andreasen NC. The Scale for the Assessment of Negative Symptoms (SANS) Department of Psychiatry, College of Medicine, The University of Iowa; Iowa City, IA: 1983. [Google Scholar]
- Andreasen NC. Scale for the Assessment of Positive Symptoms (SAPS) Department of Psychiatry, College of Medicine, The University of Iowa; Iowa City, IA: 1984. [Google Scholar]
- Arora A, Avasthi A, Kulhara P. Subsyndromes of chronic schizophrenia: a phenomenological study. Acta Psychiatr Scand. 1997;96:225–9. doi: 10.1111/j.1600-0447.1997.tb10155.x. [DOI] [PubMed] [Google Scholar]
- Barnes GM, Windle M. Family factors in adolescent alcohol and drug abuse. Pediatrician. 1987;14:13–8. [PubMed] [Google Scholar]
- Bentall RP, Corcoran R, Howard R, Blackwood N, Kinderman P. Persecutory delusions: A review and theoretical interpretation. Clin Psychol Rev. 2001;21:1143–92. doi: 10.1016/s0272-7358(01)00106-4. [DOI] [PubMed] [Google Scholar]
- Bentall RP, de Sousa P, Varese F, Wickham S, Sitko K, Haarmans M, Read J. From adversity to psychosis: pathways and mechanisms from specific adversities to specific symptoms. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1011–22. doi: 10.1007/s00127-014-0914-0. [DOI] [PubMed] [Google Scholar]
- Bentall RP, Rowse G, Shryane N, Kinderman P, Howard R, Blackwood N, Moore R, Corcoran R. The cognitive and affective structure of Paranoid Delusions: a transdiagnostic investigation of patients with schizophrenia spectrum disorders and depression. Arch Gen Psychiatry. 2009;66:236–47. doi: 10.1001/archgenpsychiatry.2009.1. [DOI] [PubMed] [Google Scholar]
- Bentall RP, Wickham S, Shevlin M, Varese F. Do specific early-life adversities lead to specific symptoms of psychosis? A study from the 2007 the Adult Psychiatric Morbidity Survey. Schizophr Bull. 2012;38:734–40. doi: 10.1093/schbul/sbs049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Stokes J, Handelsman L, Mendrano M, Desmond D, Zule W. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse and Negl. 2003;27:169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Birchwood M, Iqbal Z, Upthegrove R. Psychological pathways to depression in schizophrenia - studies in acute psychosis, post psychotic depression and auditory hallucinations. Eur Arch Psychiatry Clin Neurosci. 2005;255:202–12. doi: 10.1007/s00406-005-0588-4. [DOI] [PubMed] [Google Scholar]
- Birnbaum M, Ramsay Wan C, Broussard B, Compton MT. Associations between duration of untreated psychosis and domains of positive and negative symptoms Early. Interv Psychiatry. 2015 doi: 10.1111/eip.12256. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brady KT, Lydiard RB, Malcolm R, Ballenger JC. Cocaine-induced psychosis. J Clin Psychiatry. 1991;52:509–12. [PubMed] [Google Scholar]
- Chadwick PD, Trower P, Juusti-Butler TM, Maguire N. Phenomenological evidence for two types of paranoia. Psychopathology. 2005;38:327–33. doi: 10.1159/000089453. [DOI] [PubMed] [Google Scholar]
- Cockrell JR, Folstein MF. Mini-Mental State Examination (Mmse) Psychopharmacol Bull. 1988;24(4):689–692. [PubMed] [Google Scholar]
- Coltheart M, Langdon R, McKay R. Schizophrenia and Monothematic Delusions. Schizophr Bull. 2007;33:642–647. doi: 10.1093/schbul/sbm017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Compton MT, Potts AA, Wan CR, Ionescu DF. Which came first, delusions or hallucinations? An exploration of clinical differences among patients with first-episode psychosis based on patterns of emergence of positive symptoms. Psychiatry Res. 2012;200:702–7. doi: 10.1016/j.psychres.2012.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cristofaro SL, Cleary SD, Ramsay Wan C, Broussard B, Chapman C, Haggard PJ, Jananeh S, Myers NL, Compton MT. Measuring trauma and stressful events in childhood and adolescence among patients with first-episode psychosis: initial factor structure, reliability, and validity of the Trauma Experiences Checklist. Psychiatry Res. 2013;210:618–25. doi: 10.1016/j.psychres.2013.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drake RJ, Pickles A, Bentall RP, Kinderman P, Haddock G, Tarrier N, Lewis S. The evolution of insight, paranoia and depression during early schizophrenia. Psychol Med. 2004;34:285–92. doi: 10.1017/s0033291703008821. [DOI] [PubMed] [Google Scholar]
- Ellersgaard D, Mors O, Thorup A, Jørgensen P, Jeppesen P, Nordentoft M. Prospective study of the course of delusional themes in first-episode non-affective psychosis. Early Interv Psychiatry. 2014;8:340–7. doi: 10.1111/eip.12059. [DOI] [PubMed] [Google Scholar]
- El Yazaji M, Battas O, Agoub M, Moussaoui D, Gutknecht C, Dalery J, d'Amato T, Saoud M. Validity of the depressive dimension extracted from principal component analysis of the PANSS in drug-free patients with schizophrenia. Schizophr Res. 2002;56:121–127. doi: 10.1016/s0920-9964(01)00247-x. [DOI] [PubMed] [Google Scholar]
- Emsley R, Rabinowitz J, Torreman M RIS-INT-35 Early Psychosis Global Working Group. The factor structure for the Positive and Negative Syndrome Scale (PANSS) in recent-onset psychosis. Schizophr Res. 2003;61:47–57. doi: 10.1016/s0920-9964(02)00302-x. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M. Structured Clinical Interview for the DSM-IV Axis I Disorders. Biometrics Research Department, New York State Psychiatric Institute; New York, NY: 1998. [Google Scholar]
- Folstein MF, Folstein SE, McHugh PR. “Mini-Mental State” A Practical Method for Grading the Cognitive State of Patients for the Clinician. J Psychiatr Res. 1975;12(3):189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Freeman D. Suspicious minds: the psychology of persecutory delusions. Clin Psychol Rev. 2007;27:425–57. doi: 10.1016/j.cpr.2006.10.004. [DOI] [PubMed] [Google Scholar]
- Freeman D, Garety P. Advances in understanding and treating persecutory delusions: a review. Soc Psychiatry Psychiatr Epidemiol. 2014;49:1179–1189. doi: 10.1007/s00127-014-0928-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freeman D, McManus S, Brugha T, Meltzer H, Jenkins R, Bebbington P. Concomitants of paranoia in the general population. Psychol Med. 2011;41:923–36. doi: 10.1017/S0033291710001546. [DOI] [PubMed] [Google Scholar]
- Freeman D, Morrison PD, Murray RM, Evans N, Lister R, Dunn G. Persecutory ideation and a history of cannabis use. Schizophr Res. 2013;148:122–5. doi: 10.1016/j.schres.2013.06.008. [DOI] [PubMed] [Google Scholar]
- Fresan A, Apiquian R, Robles-García R, Balducci PM, Broussard B, Ramsay Wan C, Compton MT. Similarities and differences in associations between duration of untreated psychosis (DUP) and demographic, premorbid, and symptom severity measures in two samples of first-episode psychosis patients from Mexico and the United States. Manuscript submitted for publication. 2015 doi: 10.1007/s11126-020-09736-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galdos P, van Os J. Gender, psychopathology, and development: from puberty to early adulthood. Schizophr Res. 1995;14:105–12. doi: 10.1016/0920-9964(94)00020-9. [DOI] [PubMed] [Google Scholar]
- Garety PA, Gittins M, Jolley S, Bebbington P, Dunn G, Kuipers E, Fowler D, Freeman D. Differences in cognitive and emotional processes between persecutory and grandiose delusions. Schizophr Bull. 2013;39:629–39. doi: 10.1093/schbul/sbs059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ge X, Conger RD, Elder GH., Jr Pubertal transition, stressful life events, and the emergence of gender differences in adolescent depressive symptoms. Dev Psychol. 2001;37:404–17. doi: 10.1037//0012-1649.37.3.404. [DOI] [PubMed] [Google Scholar]
- Green C, Garety PA, Freeman D, Fowler D, Bebbington P, Dunn G, Kuipers E. Content and affect in persecutory delusions. Br J Clin Psychol. 2006;45:561–77. doi: 10.1348/014466506X98768. [DOI] [PubMed] [Google Scholar]
- Häfner H, Maurer K, Loffler W, Riecher-Rossler A. The influence of age and sex on the onset and early course of schizophrenia. Br J Psychiatry. 1993;162:80–6. doi: 10.1192/bjp.162.1.80. [DOI] [PubMed] [Google Scholar]
- Hartley S, Barrowclough C, Haddock G. Anxiety and depression in psychosis: a systematic review of associations with positive psychotic symptoms. Acta Psychiatr Scand. 2013;128:327–46. doi: 10.1111/acps.12080. [DOI] [PubMed] [Google Scholar]
- Hides L, Dawe S, McKetin R, Kavanagh DJ, Young RM, Teesson M, Saunders JB. Primary and substance-induced psychotic disorders in methamphetamine users. Psychiatry Res. 2015;226:91–6. doi: 10.1016/j.psychres.2014.11.077. [DOI] [PubMed] [Google Scholar]
- John JP, Khanna S, Thennarasu K, Reddy S. Exploration of dimensions of psychopathology in neuroleptic-naïve patients with recent-onset schizophrenia/schizophreniform disorder. Psychiatry Res. 2003;121:11–20. doi: 10.1016/s0165-1781(03)00199-9. [DOI] [PubMed] [Google Scholar]
- Jørgensen P, Jensen J. Delusional beliefs in first admitters. A clinical description Psychopathology. 1994;27:100–12. doi: 10.1159/000284854. [DOI] [PubMed] [Google Scholar]
- Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–76. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- Kelley ME, Ramsay Wan C, Broussard B, Crisafio A, Cristofaro S, Johnson S, Reed TA, Amar P, Kaslow NJ, Walker EF, Compton MT. Earlier and escalating premorbid marijuana use is associated with earlier age at onset of schizophrenia and related psychotic disorders. Manuscript submitted for publication. 2015 doi: 10.1016/j.schres.2016.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JS, Baek JH, Choi JS, Lee D, Kwon JS, Hong KS. Diagnostic stability of first-episode psychosis and predictors of diagnostic shift from non-affective psychosis to bipolar disorder: a retrospective evaluation after recurrence. Psychiatry Res. 2011;188:29–33. doi: 10.1016/j.psychres.2010.09.017. [DOI] [PubMed] [Google Scholar]
- Kimhy D, Goetz R, Yale S, Corcoran C, Malaspina D. Delusions in individuals with schizophrenia: factor structure, clinical correlates, and putative neurobiology. Psychopathology. 2005;38:338–44. doi: 10.1159/000089455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin AS, Chen CH, Hwu HG, Lin HN, Chen JA. Psychopathological dimensions in schizophrenia: a correlational approach to items of the SANS and SAPS. Psychiatry Res. 1998;77:121–30. doi: 10.1016/S0165-1781(97)00150-9. [DOI] [PubMed] [Google Scholar]
- Langdon R, Coltheart M. The Cognitive Neuropsychology of Delusions. Mind & Language. 2000;15:184–218. doi: 10.1111/1468-0017.00129. [DOI] [Google Scholar]
- Longden E, Sampson M, Read J. Childhood adversity and psychosis: generalised or specific effects? Epidemiol Psychiatr Sci. 2015:1–11. doi: 10.1017/S204579601500044X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matheson SL, Shepherd AM, Pinchbeck RM, Laurens KR, Carr VJ. Childhood adversity in schizophrenia: a systematic meta-analysis. Psychol Med. 2013;43:225–38. doi: 10.1017/S0033291712000785. [DOI] [PubMed] [Google Scholar]
- Mathias S, Lubman DI, Hides L. Substance-induced psychosis: a diagnostic conundrum. J Clin Psychiatry. 2008;69:358–67. doi: 10.4088/jcp.v69n0304. [DOI] [PubMed] [Google Scholar]
- McGuire LA, Ramsay Wan C, Compton MT. Effects of Diverse Forms of Childhood Adversity on Symptom Severity and Neurocognitive Deficits in First-Episode Psychosis. Manuscript in preparation [Google Scholar]
- Minas IH, Klimidis S, Stuart GW, Copolov DL, Singh BS. Positive and negative symptoms in the psychoses: principal components analysis of items from the Scale for the Assessment of Positive Symptoms and the Scale for the Assessment of Negative Symptoms. Compr Psychiatry. 1994;35:135–44. doi: 10.1016/0010-440x(94)90059-q. [DOI] [PubMed] [Google Scholar]
- Mrug S, Loosier PS, Windle M. Violence exposure across multiple contexts: individual and joint effects on adjustment. Am J Orthopsychiatry. 2008;78:70–84. doi: 10.1037/0002-9432.78.1.70. [DOI] [PubMed] [Google Scholar]
- Mrug S, Madan A, Windle M. Temperament alters susceptibility to negative peer influence in early adolescence. J Abnorm Child Psychol. 2012;40:201–9. doi: 10.1007/s10802-011-9550-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nunnally JC. Psychometric Theory. second. McGraw Hill; New York, NY: 1978. [Google Scholar]
- Peralta V, Cuesta MJ. Dimensional structure of psychotic symptoms: an item-level analysis of SAPS and SANS symptoms in psychotic disorders. Schizophr Res. 1999;38:13–26. doi: 10.1016/s0920-9964(99)00003-1. [DOI] [PubMed] [Google Scholar]
- Peralta V, Moreno-Izco L, Calvo-Barrena L, Cuesta MJ. The low- and higher-order factor structure of symptoms in patients with a first episode of psychosis. Schizophr Res. 2013;147:116–24. doi: 10.1016/j.schres.2013.03.018. [DOI] [PubMed] [Google Scholar]
- Rajapakse T, Garcia-Rosales A, Weerawardene S, Cotton S, Fraser R. Themes of delusions and hallucinations in first-episode psychosis. Early Interv Psychiatry. 2011;5:254–8. doi: 10.1111/j.1751-7893.2011.00281.x. [DOI] [PubMed] [Google Scholar]
- Rajkumar RP. The impact of childhood adversity on the clinical features of schizophrenia. Schizophr Res Treatment. 2015;2015:532082. doi: 10.1155/2015/532082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raune D, Bebbington P, Dunn G, Kuipers E. Event attributes and the content of psychotic experiences in first-episode psychosis. Psychol Med. 2006;36:221–30. doi: 10.1017/S003329170500615X. [DOI] [PubMed] [Google Scholar]
- Read J, Agar K, Argyle N, Aderhold V. Sexual and physical abuse during childhood and adulthood as predictors of hallucinations, delusions and thought disorder. Psychol Psychother. 2003;76:1–22. doi: 10.1348/14760830260569210. [DOI] [PubMed] [Google Scholar]
- Rogers R. Handbook of Diagnostic and Structured Interviewing. The Guilford Press; New York, NY: 2001. [Google Scholar]
- Sass L, Byrom G. Phenomenological and neurocognitive perspectives on delusions: A critical overview. World Psychiatry. 2015;14:164–173. doi: 10.1002/wps.20205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith B, Fowler DG, Freeman D, Bebbington P, Bashforth H, Garety P, Dunn G, Kuipers E. Emotion and psychosis: links between depression, self-esteem, negative schematic beliefs and delusions and hallucinations. Schizophr Res. 2006;86:181–8. doi: 10.1016/j.schres.2006.06.018. [DOI] [PubMed] [Google Scholar]
- Shtasel DL, Gur RE, Gallacher F, Heimberg C, Cannon T, Gur RC. Phenomenology and functioning in first-episode schizophrenia. Schizophr Bull. 1992;18:449–62. doi: 10.1093/schbul/18.3.449. [DOI] [PubMed] [Google Scholar]
- Sieving RE, Beuhring T, Resnick MD, Bearinger LH, Shew M, Ireland M, Blum RW. Development of adolescent self-report measures from the National Longitudinal Study of Adolescent Health. J Adolesc Health. 2001;28:73–81. doi: 10.1016/s1054-139x(00)00155-5. [DOI] [PubMed] [Google Scholar]
- Skodlar B, Dernovsek MZ, Kocmur M. Psychopathology of schizophrenia in Ljubljana (Slovenia) from 1881 to 2000: changes in the content of delusions in schizophrenia patients related to various sociopolitical, technical and scientific changes. Int J Soc Psychiatry. 2008;54:101–11. doi: 10.1177/0020764007083875. [DOI] [PubMed] [Google Scholar]
- Startup M, Bucci S, Langdon R. Delusions of reference: a new theoretical model. Cogn Neuropsychiatry. 2009;14:110–126. doi: 10.1080/13546800902864229. [DOI] [PubMed] [Google Scholar]
- Startup M, Startup S. On two kinds of delusion of reference. Psychiatry Res. 2005;137:87–92. doi: 10.1016/j.psychres.2005.07.007. [DOI] [PubMed] [Google Scholar]
- Stompe T, Friedman A, Ortwein G, Strobl R, Chaudhry HR, Najam N, Chaudhry MR. Comparison of delusions among schizophrenics in Austria and in Pakistan. Psychopathology. 1999;32:225–34. doi: 10.1159/000029094. [DOI] [PubMed] [Google Scholar]
- Toomey R, Kremen WS, Simpson JC, Samson JA, Seidman LJ, Lyons MJ, Faraone SV, Tsuang MT. Revisiting the factor structure for positive and negative symptoms: evidence from a large heterogeneous group of psychiatric patients. Am J Psychiatry. 1997;154:371–7. doi: 10.1176/ajp.154.3.371. [DOI] [PubMed] [Google Scholar]
- Uçok A, Bikmaz S. The effects of childhood trauma in patients with first-episode schizophrenia. Acta Psychiatr Scand. 2007;116:371–7. doi: 10.1111/j.1600-0447.2007.01079.x. [DOI] [PubMed] [Google Scholar]
- van Nierop M, Lataster T, Smeets F, Gunther N, van Zelst C, de Graaf R, ten Have M, van Dorsselaer S, Bak M, Myin-Germeys I, Viechtbauer W, van Os J, van Winkel R. Psychopathological mechanisms linking childhood traumatic experiences to risk of psychotic symptoms: analysis of a large, representative population-based sample. Schizophr Bull. 2014;40(Suppl 2):S123–30. doi: 10.1093/schbul/sbt150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varese F, Smeets F, Drukker M, Lieverse R, Lataster T, Viechtbauer W, Read J, van Os J, Bentall RP. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophr Bull. 2012;38:661–71. doi: 10.1093/schbul/sbs050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vázquez-Barquero JL, Lastra I, Cuesta Nuñez MJ, Herrera Castanedo S, Dunn G. Patterns of positive and negative symptoms in first episode schizophrenia. Br J Psychiatry. 1996;168:693–701. doi: 10.1192/bjp.168.6.693. [DOI] [PubMed] [Google Scholar]
- Woodward TS, Menon M, Hu X, Keefe RS. Optimization of a multinomial model for investigating hallucinations and delusions with source monitoring. Schizophr Res. 2006;85:106–112. doi: 10.1016/j.schres.2006.03.008. [DOI] [PubMed] [Google Scholar]
- Woodward TS, Menon M, Whitman JC. Source monitoring biases and auditory hallucinations. Cogn Neuropsychiatry. 2007;12:477–494. doi: 10.1080/13546800701307198. [DOI] [PubMed] [Google Scholar]
- Zweben JE, Cohen JB, Christian D, Galloway GP, Salinardi M, Parent D, Iguchi M. Methamphetamine Treatment Project. Psychiatric symptoms in methamphetamine users. Am J Addict. 2004;13:181–90. doi: 10.1080/10550490490436055. [DOI] [PubMed] [Google Scholar]


