Abstract
Hospital length of stay (LOS) after burn injury is commonly estimated at one day per percent burn but LOS often exceeds that estimate. The study purpose is to develop a novel method for estimating burn hospital LOS at any time during hospitalization. We used the ABA National Burn Repository (NBR) from 2000–9 to directly estimate the median residual hospital length of stay (MRLOS) of patients hospitalized for burn injuries and who survived to discharge. The MRLOS is the median of how many more days a burn patient will be hospitalized given that the person has been in-hospital for a specified time period. We also estimated the 25th and 75th percentiles of residual length of stay and quantified the relationship between MRLOS and LOS with ordinary least squares for all burn patients, by burn size and by presence of inhalation injury. MRLOS increased with increasing LOS confirming that discharge estimates change over time. Patients with inhalation injury had longer MRLOS than patients without inhalation injury in the first 100 hospital days. Patients with large burns (>25%) had large MRLOS consistent with prolonged hospitalization, but patients with small burns (<25%), also had steadily increasing MRLOS during hospitalization (i.e. the longer the patient was in the hospital, the longer the predicted LOS regardless of initial LOS estimate). Estimating remaining hospital LOS at any time during admission has been problematic; MRLOS can be used to provide an estimate of remaining hospital LOS and resource utilization to families, administrators, and other medical professionals.
Introduction
Burn patients are a unique population with unique characteristics that distinguish them from trauma and other forms of injury. The systematic perturbations of burn injury result in prolonged length of stay (LOS)multiple operations andutilization of numerous costly physical resources compared to other forms of trauma. The prolonged LOS and high resource consumption associated with burn treatment generate increased scrutiny by both administrators and insurance providers, who are charged with decreasing costs by minimizing both hospital LOS and resource utilization. From an administrative standpoint, longer lengths of stay have been associated with poor quality of care; hence, burn centers are at risk for decreased reimbursement for services provided. (1) The trend toward bundled payments and payment based on results with predefined LOS targets has increased the emphasis on limiting LOS. (2–5) In the U.S., burn patient LOS is generally estimated as one day per percent burn; this estimate is often presented to the family, who understandably are anxious to know hospitalization duration. (6, 7) However, this estimate is far from perfect, and patients often exceed their projected admission duration due to a differential response to injury, complications encountered during hospitalization, or lack of healing. (8, 9) A dynamic method of estimating length of stay that could be applied continuously at any time during hospitalization could better inform families, administrators, and clinicians on resource utilization and quality of care. When hospital length of stay exceeds the initial projection, clinicians are unable to accurately predict how long a patient will remain hospitalized.
The purpose of this study was to develop a method for estimating burn hospital length of stay at any time during hospitalization. We hypothesized that duration of hospitalization (i.e. how long a patient has been in the hospital) influences the prediction of remaining hospital LOS (i.e. how long the patient will be in the hospital). We used the American Burn Association National Burn Repository (NBR) to directly estimate median residual length of stay which is the remaining hospital LOS for a burn patient at any time during hospitalization.
Methods
This study was approved by the University of California Davis Human Subjects Review Board. We utilized records from the 2009 NBR release to analyze admissions after 2000 using previously described methodology. (10) From the 210,683 records of initial visit admissions after 2000 we eliminated records missing survival to discharge data (12,226), age (5,441), burn size (42,545), inhalation injury (12,861), or LOS (4,471).We also removed 3,218 duplicate records, 6,530 records with unreliable information (e.g., total burn surface area greater than 100, age ≤0), 23,084 readmissions, 1,038 records of patients transferred to another primary care facility and 3,690 non-burn injuries. Finally, we restricted the analysis to patients who survived to discharge. This screening left 91,467 patients with the minimum information for necessary analysis (i.e. patient age, a burn or inhalation injury, hospital discharge status, and LOS).
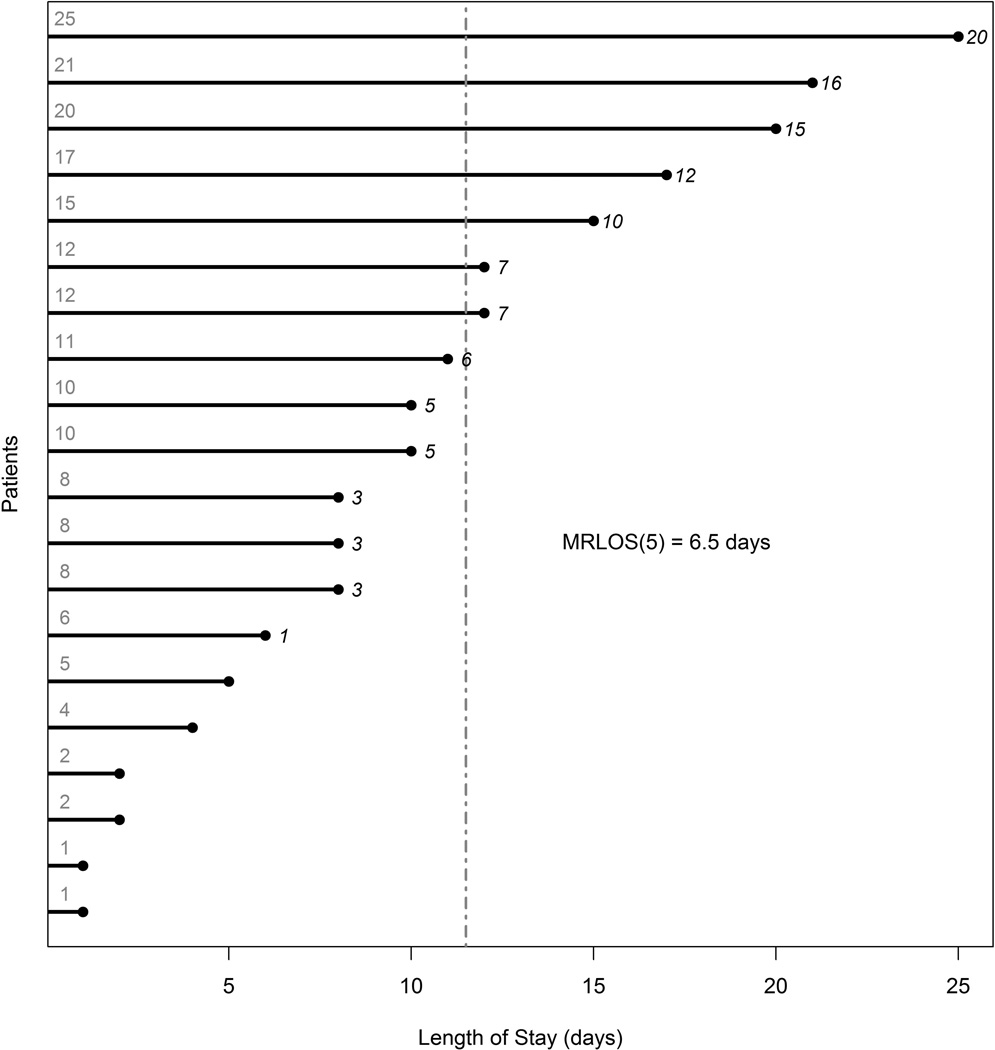
Median residual length of stay (MRLOS) was calculated for all patients, patients with and without inhalation injury, and for burn sizes in quartiles. Because of the large sample size available with the NBR and lack of censoring, we directly calculated the MRLOS by taking the difference between each patient’s total LOS and the hospitalization time of interest (t) and calculating the median of across all patients still hospitalized at time t. MRLOS is calculated separately for each day of hospitalization using patients still hospitalized. For each patient still hospitalized on each day we took the difference between total LOS and the day of hospitalization. We then calculated the median of all patient values on any given day. That number represents the MRLOS for that day. The process was repeated for each day using data from patients that were still hospitalized. These calculations are illustrated in Figure 1 which shows the MRLOS calculation at 5 days. The horizontal lines indicate each patient’s entire LOS (depicted numerically by the gray numbers on the left). The italicized numbers to the right of the hortizontal lines show the remaining length of stay for each patient after 5 days of hospitalization. The median of the italicized numbers gives the median residual length of stay at 5 days. In this example the MRLOS at 5 days is 6.5 days and is shown by the dashed line.
Figure 1.
Illustration of Median Residual Length of Stay (MRLOS) calculation for 20 patients at hospital day 5. The horizontal lines and gray numbers indicate each patient’s LOS. The italicized numbers to the right of each horizontal line show the remaining length of stay for each patient on day 5 of hospitalization. The median of the italicized numbers gives the median residual length of stay at 5 days. In this example the MRLOS at day 5 is 6.5 days and is shown by the gray dashed line.
Results
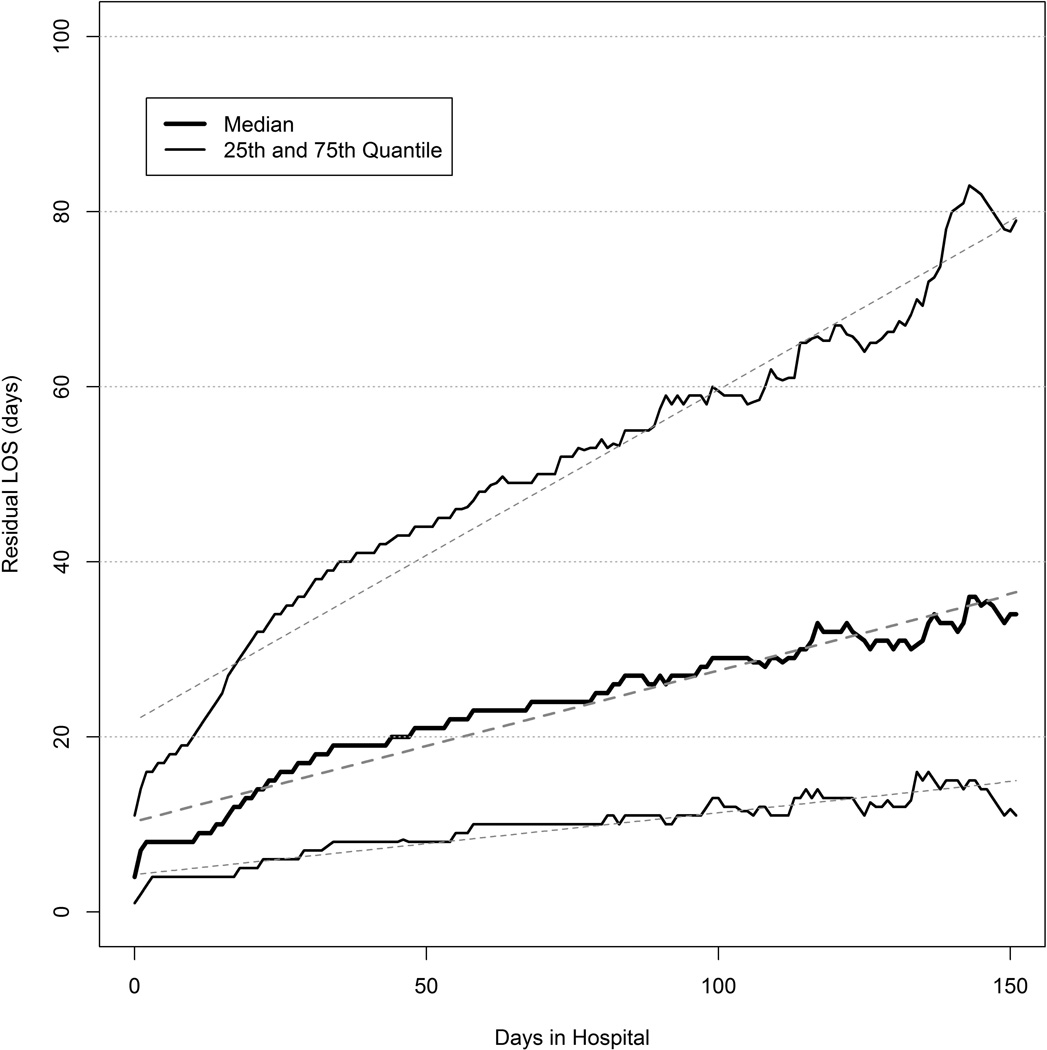
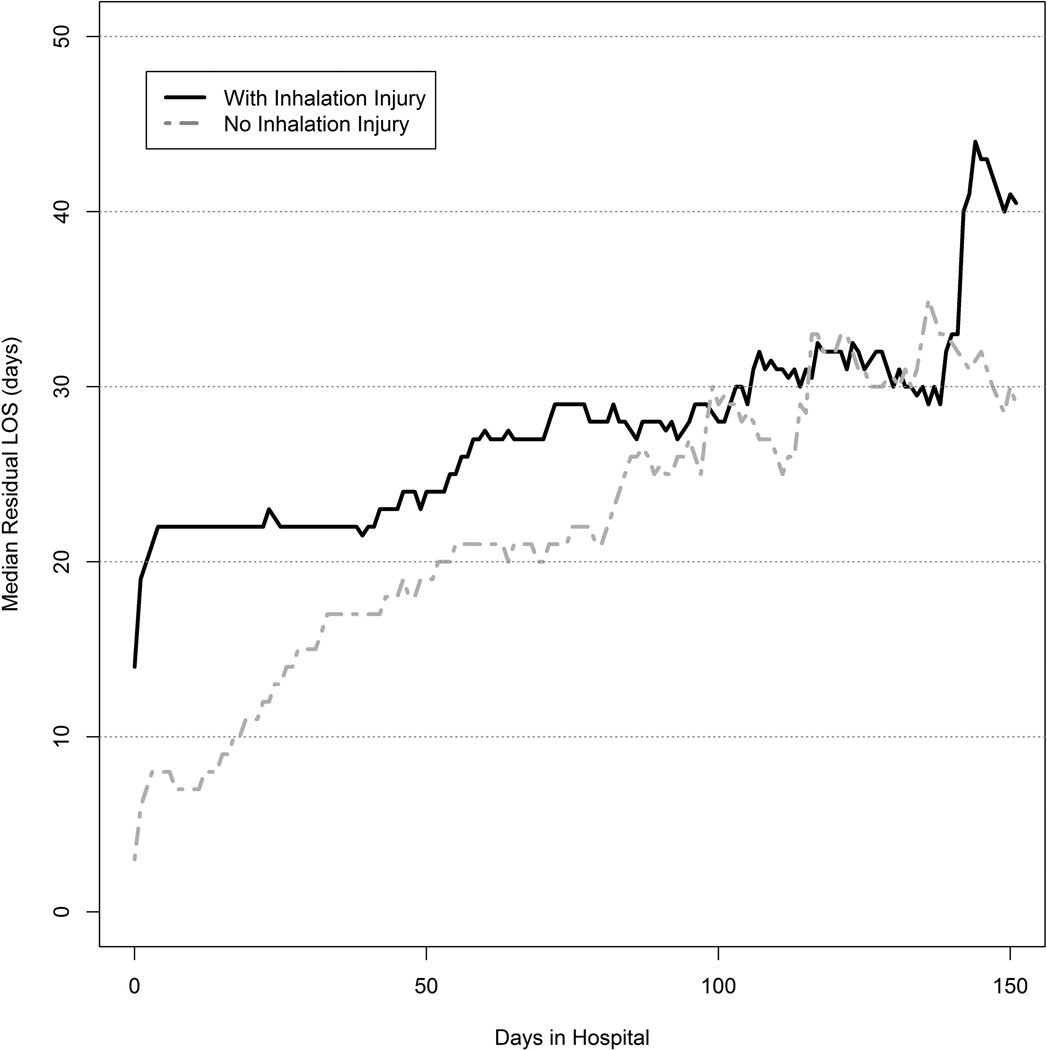
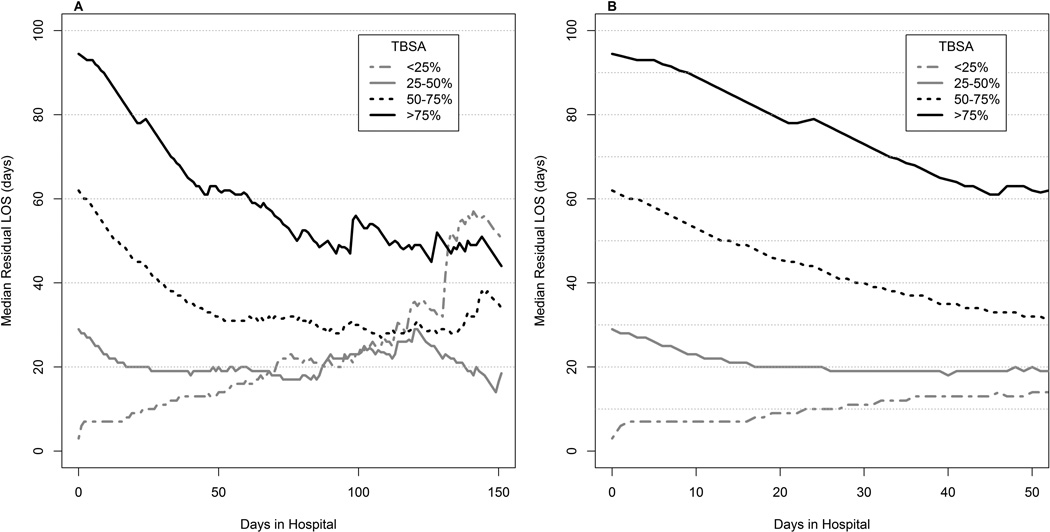
Demographics are depicted in Table 1. Median age was 28 years, and consistent with previous reports, the vast majority of burns were less than 25% TBSA. Approximately 7% had inhalation injury. Overall median length of stay was 4 days [IQR: (1, 11)]. Figures 2, 3, and 4 illustrate the MRLOS calculation for all patients, patients with inhalation injury, and for TBSA burn <25%, 25–50%, 51–75%, and >75%, respectively. As depicted in Figure 1, the longer the patient is in the hospital, the longer the patient is likely to remain in the hospital. Hence, MRLOS increases throughout hospitalization. Patients with inhalation injury (Figure 2) have longer predicted MRLOS for the first 100 days of hospitalization compared to patients without inhalation injury. The relationship between MRLOS and burn size is more complicated. For patients with small burns ( < 25%), MRLOS increases with longer LOS, but for patients with larger burns, MLR initially declines and before largely stabilizing at 50 to 100 days (Figure 3). Although MRLOS declines initially, the overall length of stay for patients with larger burns remains high.
Table 1.
Summary Statistics of Patient Records Used for Median Residual Length of Stay (MRLOS) Assessment
| Variable | N | Median [25th, 75th percentiles] |
Total Length of Stay (Days) Median [25th, 75th percentiles] |
|---|---|---|---|
| Age (years) | 91,467 | 28.0 [8.9, 45.8] | 4 [1, 11] |
| TBSA (%) All Patients | 91,467 | 5 [2, 10] | 4 [1, 11] |
| < 25% | 85,540 | 4 [2, 9] | 3 [1, 10] |
| 25–50% | 4,752 | 32 [28,38] | 29 [17, 48] |
| 50–75% | 984 | 58 [53, 65] | 62 [41, 93] |
| > 75% | 190 | 82 [79, 88] | 93 [58, 141] |
| With Inhalation Injury | 6,618 | 7.23% | 14 [3, 26] |
| No Inhalation Injury | 84,849 | 92.77% | 3 [1, 10] |
The median, 25th and 75th percentiles of patient ages and TBSA are shown for the entire data set. In addition, the median 25th and 75th percentiles of TBSA are shown for each TBSA group analyzed. Inhalation injury is summarized as the percentages of patients with and without inhalation injury. Finally, the median, 25th and 75th percentiles of total length of stay (days) are shown for each patient grouping.
Figure 2.
Median Residual Length of Stay(MRLOS) for all patients. Thickest black line is MRLOS. The thinner solid black lines show the 25th and 75th percentiles. Gray dashed lines are the ordinary least squares fitted values. These estimates are for patients that were discharged alive.
Figure 3.
Median Residual Length of Stay(MRLOS) by inhalation injury status. Patients with inhalation injury have longer hospital length of stay for the first 100 days post-injury than those without inhalation injury.
Figure 4.
Median Residual Length of Stay (MRLOS) by burn size.
Discussion
Estimation of burn patient LOS is typically done at admission to provide clinicians and families with a discharge goal date. This allows families to plan activities and clinicians to estimate resource utilization. When LOS exceeds the estimation, families become increasingly anxious and request further estimates; the clinician is left without a method to revise the initial LOS estimate. Understandably, when patient stay exceeds the initial estimate, families request an updated estimate, for which there are no objective guidelines, and clinicians are forced to either extrapolate from personal experience or not provide the family with this important information.
Two burn patient populations that frequently do not adhere to the day per percent burn rule are patients with inhalation injury and large TBSA burn. (11–13) Clinically, both are associated with greater physiologic perturbation and higher incidence of complications, particularly infections. (14–16) MRLOS graphically depicts the impact of these factors on burn LOS. In addition to providing LOS information to families and clinicians, MRLOS could potentially help inform quality of care determinations and satisfy payor justifications for prolonged LOS. As demonstrated in this paper, the LOS for both inhalation injury and large burns is variable and continues to change for the first 100 days after admission.
The differences in MRLOS patterns can provide insight into the causes for deviation from the one day per percent burn rule. For patients with small burns, who make up the vast majority of the data, prolonged hospital stays are likely due to factors other than the burn injury, such as comorbidities, complications, or other difficult to measure factors. Inhalation injury, which has well documented effects on mortality, also has a longer MRLOS. (17, 18) Similar to smaller burns, after prolonged hospitalization the initial injury plays a smaller role in determining outcomes. Finally, in larger burns MRLOS decreases and then stabilizes. This could be due to the prolonged nature of wound healing which could dilute the impact of any single complication on LOS.
LOS estimates are used administratively as well clinically. A consensus conference in 1987 encouraged the use of the one day per percent burn rule to estimate hospital LOS after burn injury for any burn DRG (diagnosis related group). (6) As such, this standard may be applied to burn reimbursement by hospital payors. Clinicians may thus be held accountable for not reaching discharge targets and not be reimbursed for care exceeding these estimates. In addition, quality of care has been linked to LOS in burns, particularly with respect to wound healing. (19) Finally, estimation of LOS enables clinicians and burn clinicians to estimate resource utilization, supplies, and staffing. MRLOS can provide a rough estimate for those patients who deviate from the one day per percent rule and can be used at any time during hospitalization (from day 1 onwards, including the perioperative period) to estimate LOS.
MRLOS can potentially improve research efforts by providing information on inhalation injury and large burn “outliers” for hospital LOS by providing a LOS target for treatment outcome comparisons among survivors of burn injury in those groups. For example, if an intervention is implemented at day 3, the effects of that intervention will not impact the LOS for patients until after that time. Being able to estimate how much the LOS outcome trajectory is changed by the intervention depends on an accurate estimation of how long the patient will be hospitalized at the point of time the intervention occurred.
This study has limitations that must be acknowledged. The NBR is a large data set that represents the experience of >80 burn centers. However, each center collects data independently and thus introduces the potential for variability in diagnosis of burn size and inhalation injury. Second, the incompleteness of the data may raise concern regarding data validity. We performed an extensive data validation process to minimize inaccuracies and inconsistencies in data. (10) Any data set will have concerns of data quality, but we exhaustively applied stringent criteria to minimize data irregularities. Improvements in NBR data quality occurred with each rendition (including the addition of a validation tool at the point of data entry), and the validated data remained consistent, suggesting that the data has validity in the aggregate. Second, MRLOS, although of assistance in providing estimates of LOS for populations, represents summary statistics and may or may not accurately depict LOS for any given patient or for a constellation of specific patient characteristics. As such, it must be used with caution until validated in a prospective manner. Likewise, despite the large number of patients in the database, the relatively small sample size for patients with large burns and extremely prolonged LOS limits the accuracy of estimates. Finally, while MRLOS can provide revised LOS estimates during the course of hospitalization, it does not elucidate the cause of prolonged LOS. Nonetheless, MRLOS represents a unique method for estimating LOS throughout hospitalization, not just at admission.
The physiologic status of burn patients changes throughout hospitalization due to variability in response to treatment, injury characteristics, and a variety of other factors. To date hospital LOS predictions have been static and reflect the patient status solely at the time of admission. MRLOS provides a simple, yet novel method of predicting burn patient hospital LOS throughout the changing phases of care. Further prospective validation and modeling of the MRLOS can provide better insight into patient outcomes.
Supplementary Material
Acknowledgments
Supported by National Center for Research Resources, National Institutes of Health, through grant #UL1 RR024146, the National Center for Advancing Translational Sciences, National Institutes of Health, grant #TR 000002 and by USAMRMC Award #W81XWH-09-1-069
Footnotes
Presented at the 46th Annual American Burn Association Meeting, Boston, MA March 2014
References
- 1.Porter ME. What is value in health care? N Engl J Med. 2010;363:2477–2481. doi: 10.1056/NEJMp1011024. [DOI] [PubMed] [Google Scholar]
- 2.Burns J. Bundled payment: hospitals see the advantages, but face big challenges too. Hosp Health Netw. 2013;87:26–31. [PubMed] [Google Scholar]
- 3.Delisle DR. Big things come in bundled packages: implications of bundled payment systems in health care reimbursement reform. Am J Med Qual. 2013;28:339–344. doi: 10.1177/1062860612462740. [DOI] [PubMed] [Google Scholar]
- 4.Wallis KL, Malic CC, Littlewood SL, Judkins K, et al. Surviving "Payment by Results": a simple method of improving clinical coding in burn specialised services in the United Kingdom. Burns. 2009;35:232–236. doi: 10.1016/j.burns.2008.06.008. [DOI] [PubMed] [Google Scholar]
- 5.Sánchez JL1, Perepérez SB, Bastida JL, Martínez MM. Cost-utility analysis applied to the treatment of burn patients in a specialized center. Arch Surg. 2007;142:50–57. doi: 10.1001/archsurg.142.1.50. [DOI] [PubMed] [Google Scholar]
- 6.Gillespie R, Carroll W, Dimick AR, Haith L, et al. Diagnosis-related groupings (DRGs) and wound closure: roundtable discussion. J Burn Care Rehabil. 1987 May-Jun;8(3):199–209. doi: 10.1097/00004630-198705000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Saffle JR, Davis B, Williams P. Recent outcomes in the treatment of burn injury in the United States: a report from the American Burn Association Patient Registry. J Burn Care Rehabil. 1995 May-Jun;16(3 Pt 1):219–232. doi: 10.1097/00004630-199505000-00002. discussion 288-9. [DOI] [PubMed] [Google Scholar]
- 8.Myers J, Lehna C. Where are Length of Stays Longer and Total Charges Higher for Pediatric Burn Patients? J Burn Care Res. 2014 Aug 5; doi: 10.1097/BCR.0000000000000012. (in press) [DOI] [PubMed] [Google Scholar]
- 9.National Burn Repository 2014 Report. Chicago, IL: American Burn Association; [Google Scholar]
- 10.Taylor SL, Lee D, Nagler T, Lawless MB, et al. A validity review of the National Burn Repository. J Burn Care Res. 2013 Mar-Apr;34(2):274–280. doi: 10.1097/BCR.0b013e3182642b46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hussain A, Dunn KW. Predicting length of stay in thermal burns: a systematic review of prognostic factors. Burns. 2013 Nov;39(7):1331–1340. doi: 10.1016/j.burns.2013.04.026. [DOI] [PubMed] [Google Scholar]
- 12.Thombs BD, Singh VA, Halonen J, Diallo A, Milner SM. The effects of preexisting medical comorbidities on mortality and length of hospital stay in acute burn injury: evidence from a national sample of 31,338 adult patients. Ann Surg. 2007 Apr;245(4):629–634. doi: 10.1097/01.sla.0000250422.36168.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lim J, Liew S, Chan H, Jackson T, et al. Is the length of time in acute burn surgery associated with poorer outcomes? Burns. 2014 Mar;40(2):235–240. doi: 10.1016/j.burns.2013.06.005. [DOI] [PubMed] [Google Scholar]
- 14.Santucci SG, Gobara S, Santos CR, Fontana C, Levin AS. Infections in a burn intensive care unit: experience of seven years. J Hosp Infect. 2003 Jan;53(1):6–13. doi: 10.1053/jhin.2002.1340. [DOI] [PubMed] [Google Scholar]
- 15.Theodorou P, Thamm OC, Perbix W, Phan VT. Pseudomonas aeruginosa bacteremia after burn injury: the impact of multiple-drug resistance. J Burn Care Res. 2013 Nov-Dec;34(6):649–658. doi: 10.1097/BCR.0b013e318280e2c7. [DOI] [PubMed] [Google Scholar]
- 16.Theodorou P, Lefering R, Perbix W, Spanholtz TA, et al. Staphylococcus aureus bacteremia after thermal injury: the clinical impact of methicillin resistance. Burns. 2013 May;39(3):404–412. doi: 10.1016/j.burns.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 17.Smith DL, Cairns BA, Ramadan F, et al. Effect of inhalation injury, burn size, and age on mortality: a study of 1447 consecutive burn patients. J Trauma. 1994;37:655–659. doi: 10.1097/00005373-199410000-00021. [DOI] [PubMed] [Google Scholar]
- 18.Dries DJ, Endorf FW. Inhalation injury: epidemiology, pathology, treatment strategies. Scand J Trauma Resusc Emerg Med. 2013;21:31. doi: 10.1186/1757-7241-21-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gibran NS, Wiechman S, Meyer W, Edelman L, et al. American Burn Association consensus statements. J Burn Care Res. 2013 Jul-Aug;34(4):361–385. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.