Abstract
Congenital tufting enteropathy is a rare condition which presents in early infancy. It is a condition which should be suspected in infants who present with diarrhoea soon after birth. A rare association with arthritis has been observed with a handful of cases documented in the literature. Our case differs as the arthritis described is erosive in nature, a feature which is not present in other cases.
Background
Tufting enteropathy is a rare autosomal recessive cause for chronic diarrhoea in infancy. The literature regarding the association of chronic arthritis and tufting enteropathy is scarce. The associated arthritis is severe and debilitating resulting in increased morbidity. The lack of knowledge related to the subject makes this association even more overwhelming to the affected individuals as this affects treatment issues and the expected prognosis.
Case presentation
A 19-year-old female patient, suffering from congenital tufting enteropathy, confirmed on jejunal biopsies in her early infancy, presented with joint pains which started when she was 16 years old. There was no known family history of congenital tufting enteropathy. She initially reported of pain in her feet and some non-specific hip pain which resulted in her limping. This pain was worse on weight-bearing and was felt irrespective of the time of day. Two years later she began to suffer from knee pain which was gradually becoming worse and interfering with her mobility. She also developed hip pain which improved spontaneously. Morning stiffness was present for just a few minutes.
She was diagnosed as suffering from a chronic arthritis with clinical features suggesting an inflammatory nature. Both small and large joints were affected with early radiological investigations appearing normal. Radiological signs of chronic arthritis only appear 2 years after symptom onset.
Investigations
Multiple radiological investigations were performed. Baseline plain radiography was normal in the early stages of presentation with dramatic changes occurring over a span of 2 years.
Plain radiographs of the ankle 6 months apart (figure 1) demonstrated the dramatic progression of joint changes. The result was complete loss of joint space in the posterior subtalar articular surfaces with subchondral cysts and sclerosis.
Figure 1.
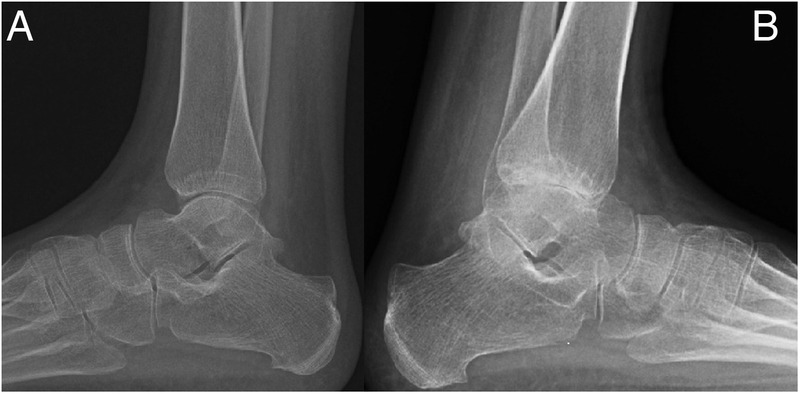
Plain radiographs of the ankle 6 months apart. (A) Demonstrating early changes; however, the joint spaces are still relatively well preserved. There is dramatic progression in a span of 6 months as seen in (B) showing complete loss of joint space in the posterior subtalar articular surfaces with subchondral cysts and sclerosis.
MRI was performed to try and quantify the degree of articular cartilage damage (figure 2). This showed multifocal areas of subchondral cystic change with surrounding marrow oedema on either side of the tibiotalar articulation, in association with a globally reduced joint space.
Figure 2.
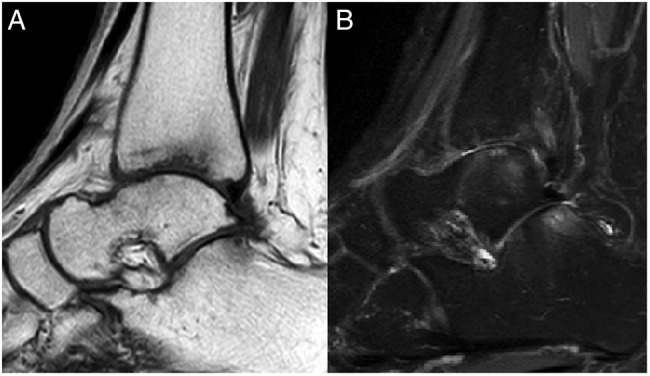
MRI ((A) PD image and (B) T2-weighted fat-saturated image) of the ankle showing subchondral cystic change with surrounding marrow oedema like signal intensity on either side of the tibiotalar articulation, in association with a globally reduced joint space.
Degenerative changes with chronic looking erosive changes were also visible in the smaller joints of the hands and feet. In the feet changes were observed at the first, second and third metatarsophalangeal joints (figure 3).
Figure 3.

Plain radiograph of feet demonstrating loss of joint space at the first, second and third metatarsophalangeal joints.
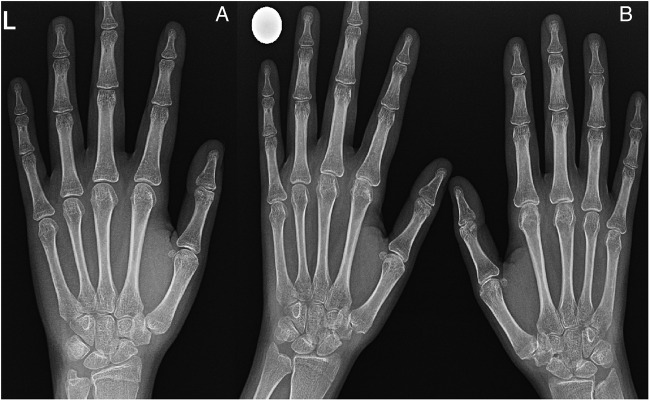
In the hands, subtle but definite loss of metacarpophalangeal joint space was present in relation to the left index and middle fingers bilaterally. Mild erosion of the right ulnar styloid was also observed on plain radiographs (figure 4).
Figure 4.
Plain radiographs of the hands a few years apart showing changes at the metacarpophalangeal joint spaces of the left index and middle fingers with mild erosion of the right ulnar styloid (B). Initially the X-ray of her left hand appeared unremarkable (A).
MRI of the patient's shoulders was also performed as she reported of severe pain and restricted movement on abduction. This showed evidence of established articular cartilage damage at the level of the glenohumeral joint, with loss of joint space and associated subchondral marrow signal changes (figure 5).
Figure 5.

Axial T2-weighted fat-saturated image of the shoulder demonstrating established articular cartilage damage in the glenohumeral joint with loss of joint space and associated subchondral marrow signal changes.
None of the larger joints were spared with similar changes seen in hip joints (figure 6) and knees. Aspiration of a knee joint effusion was performed during a flare-up revealing no evidence of septic arthritis (figures 7 and 8).
Figure 6.
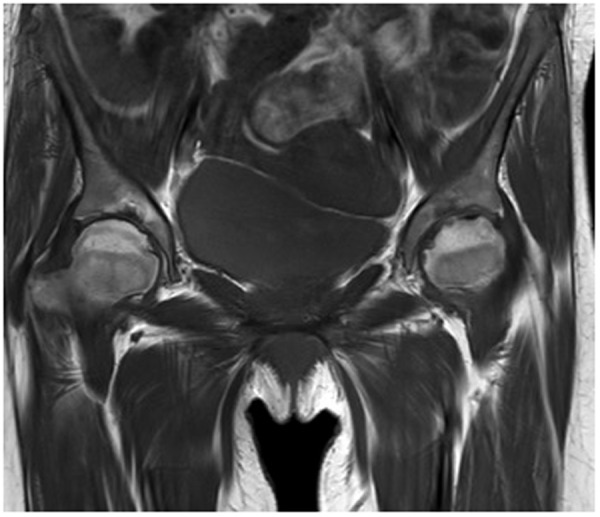
PD coronal image of hip joints demonstrating established articular cartilage damage bilaterally with erosive changes and loss of joint space, worse on the left.
Figure 7.

Plain radiographs of the knees. (A) Demonstrating severe patellofemoral arthritis with irregularity of the articular surface. (B) Showing similar changes in the medial compartment of the knee.
Figure 8.
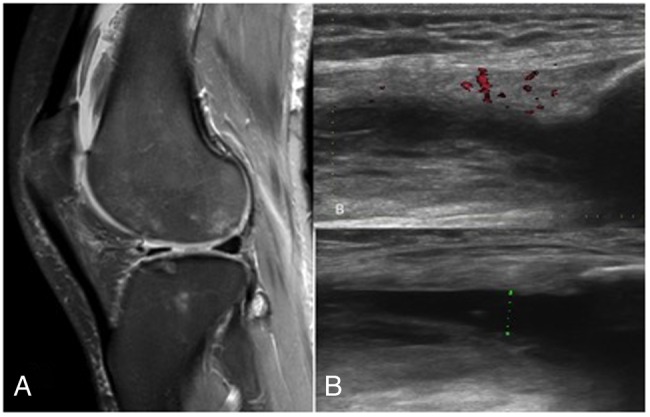
Unenhanced non-arthrographic MRI of the knee showing a moderate knee joint effusion with ongoing active synovitis. Multifocal areas of chondral damage are appreciated (A). An ultrasound scan of the same knee demonstrating a significant knee joint effusion with suprapatellar extension and evidence of florid ongoing synovitis, as seen in (B) with increased flow on Doppler assessment. A diagnostic aspirate to exclude septic arthritis was performed at this stage (B and C).
These changes were seen on a background of severe osteopenia worst in the hips.
Blood tests revealed inflammatory markers including erythrocyte sedimentation rate (ESR) and C reactive protein (CRP) were normal. They were only raised during the acute flare-up.
Differential diagnosis
The combination of arthralgia, chronic arthritis and osteoporosis are common manifestations of rheumatoid arthritis. Chronic diarrhoea and arthritis starting in infancy does not lead to a wide differential diagnosis.
Inflammatory bowel disease is a reasonable differential; nevertheless, this is not well described in infants. This diagnosis would be confirmed on endoscopy.
Coeliac disease may also sometimes present with polyarthritis.1 A simple blood test for IgA tissue transglutaminase antibodies will help steer the diagnosis towards coeliac disease.
A histological diagnosis is, however, paramount in confirming the underlying gastrointestinal condition. Thus, endoscopy with intestinal biopsies is the key investigation in making the diagnosis of the primary gastrointestinal condition.
The pathophysiology of chronic arthritis in congenital tufting enteropathy still eludes us.
Treatment
Shortly after being diagnosed with congenital tufting enteropathy the patient was started on total parenteral nutrition. Although her appetite was fair she continued to lose weight with chronic loose stools. Her medical history was complicated by superior vena cava thrombosis related to central line insertion. This resulted in treatment with warfarin which she still currently receives. Despite several months of treatment with sulfasalazine, there was persistent evidence of ongoing joint synovitis clinically. Methotrexate was therefore added to the treatment. She was started on this treatment based on clinical and radiological findings, while inflammatory markers remained stable.
No improvement was noted so treatment was escalated to infliximab which appeared to provide more symptom relief. She was monitored while on treatment with regular blood tests including a complete blood count, liver function and renal function tests.
Outcome and follow-up
The patient continued to be followed up closely, with radiological investigations performed during flare-ups. It is noteworthy that the inflammatory markers, including ESR and CRP, remained stable even during flare-ups. Other routine blood tests remained within normal limits. The patient's symptoms remained debilitating and continued to limit her activities of daily living, especially walking.
Discussion
Intestinal epithelial dysplasia or tufting enteropathy is thought to be related to abnormal development or differentiation of enterocytes. Jejunal biopsies confirm the diagnosis with histology showing various degrees of villous atrophy with disorganisation of surface enterocytes and associated focal crowding which resemble tufts. This disease is more common in patients of Arabic origin. The prevalence is also high in the Maltese islands although the phenotype appears to be milder.2
Al-Mayouf et al describe two cases of congenital tufting enteropathy who also presented with chronic arthritis. Although the patients described were younger than our patient the pattern of joint involvement is similar with both small and large joints affected. High inflammatory markers were however, seen in these cases. Imaging showed severe osteopenia with no evidence of erosions.1 On the contrary, radiological changes in the case we describe demonstrated chronic erosive changes.
Another case report described a young girl also known to suffer from congenital tufting enteropathy who presented at the age of 5 years with pain in wrists and proximal interphalangeal joints. Radiological findings in this case included osteoporosis, soft tissue swelling and joint space narrowing.3 She was subsequently diagnosed with juvenile rheumatoid arthritis and treated with prednisolone.
Learning points.
Congenital tufting enteropathy may be associated with a chronic debilitating arthritis.
Radiological investigations and symptomatology point towards a picture of active synovitis which develops into a chronic form of arthritis.
Only a handful of cases are described in the literature making this condition difficult to manage.
Footnotes
Contributors: CA performed the literature review and drafted the article. EP and BC are the caring physicians of the patient and SGS made the radiological diagnosis. All authors contributed in overseeing the preparation of this case.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Al-Mayouf S, Alswaied N, Alkuraya F et al. Tufting enteropathy and chronic arthritis: a newly recognized association with a novel EpCAM gene mutation. J Pediatr Gastroenterol Nutr 2009;49:642–4. 10.1097/MPG.0b013e3181acaeae [DOI] [PubMed] [Google Scholar]
- 2.Goulet O, Salomon J, Ruemmele F et al. Intestinal epithelial dysplasia (tufting enteropathy). Orphanet J Rare Dis 2007;2:20 10.1186/1750-1172-2-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ko J, Seo J, Shim J et al. Tufting enteropathy with EpCAM mutations in two siblings. Gut Liver 2010;4:407–10. 10.5009/gnl.2010.4.3.407 [DOI] [PMC free article] [PubMed] [Google Scholar]