Abstract
A healthy female presented with upper extremity (UE) swelling of several days duration. Admission laboratories were normal except for an elevated D-dimer. An UE ultrasound with Doppler revealed a thrombus in the right subclavian vein. A subsequent chest CT angiogram further characterised the subclavian vein thrombus and also identified a pulmonary embolus. A thorough history and laboratory evaluation showed that her only risk factors were long-time contraceptive pills and a recent cycle of ovarian hyperstimulation (OH) 7 weeks prior to presentation. Anticoagulation treatment was started and the patient's remaining outpatient work-up was negative for all other hereditary causes. A complete anatomic work-up showed bilateral thoracic outlet syndrome (TOS). A review of the literature on the occurrence of upper extremity deep venous thrombosis suggests that these usually occur in the presence of a predisposing factor, including catheters, indwelling devices and active malignancies. OH has been shown to precipitate venous thromboembolism events; however, the diagnosis of bilateral TOS as a predisposing risk factor has not been described in a patient who had recently undergone recent OH and in one who was not actively pregnant.
Background
Upper extremity deep venous thrombosis (UEDVT) is far less common than lower extremity deep venous thrombosis (DVT). UEDVTs are characterised as primary or secondary, with the latter making up for about 80% of cases.1 2 UEDVTs commonly occur in association with identifiable risk factors such as malignancy or temporally associated with UE procedures.1 2 Interestingly, the use of oral contraceptive pill (OCP), in the absence of other risk factors for venous thromboembolism (VTE), has not been associated with increased incidence of UEDVT.3
With the increase of assisted reproductive procedures in the past several decades, there have been reports of thromboembolic complications. Assisted reproductive technology (ART) uses exogenous gonadotropins and gonadotropin-releasing analogues for follicular stimulation, maturation and release.4 Most commonly, VTE are found in the setting of ovarian hyperstimulation syndrome (OHSS) and 2–6% of women who undergo ART develop OHSS which is manifested by enlarged ovaries, ascites, pleural effusions and other thromboembolic conditions.5 6 Chan and Ginsberg6 performed a case review where they found that in 20% of cases, clinically overt OHSS was not present prior to the diagnosis of UEDVT.
Thoracic outlet syndrome (TOS) is a well-known risk factor for thrombosis. Paget-Schroetter syndrome, or effort thrombosis, is caused by a tight thoracic outlet leading to repetitive injury to the vein due to frequent arm movements.7 This repetitive endothelial damage predisposes to clot formation. Paget-Schroetter syndrome accounts for 30–40% of spontaneous axillary and subclavian VTE and for 10–20% of all UEDVT.8
This case illustrates an isolated occurrence of UEDVT in the absence of clinical OHSS. This suggests that the risk of thromboembolism is increased by the ART alone, irrespective of pregnancy or OHSS. Her underlying anatomic TOS was previously asymptomatic, but predisposed her to developing a VTE when subjected to hormonal therapy.
Case presentation
A 36-year-old healthy woman, G0P0A0, presented with symptoms of a swollen UE of 1-week duration. Physical examination revealed an erythematous UE with decreased range of motion. There was no history of trauma or hypercoagulability and she denied any history of repetitive UE activities. Her only medication was an oestrogen-containing OCP that she had been prescribed for about 15 years. She travels for work frequently with short flights.
The patient denies any family history of blood clots, strokes, blood disorder and sudden deaths. Her mother had one miscarriage. She has never smoked nor used drugs, and drinks socially.
About 10 weeks prior to the onset of symptoms, the patient underwent one cycle of ovarian stimulation with subsequent egg harvesting. She had no complications from the procedure and in the interim she was asymptomatic until presentation.
Examination on presentation revealed a well-appearing woman with normal vital signs and in no distress. Her body mass index was 20 kg/m2. An Elevated Arm Stress Test and Adson's manoeuvre were negative. She had no facial swelling, neck was supple and with no lymphadenopathy, although she felt the right side of her face was fuller. She had right upper extremity swelling from her hand up to the shoulder with good capillary refill. The remainder of her examination was unremarkable.
Investigations
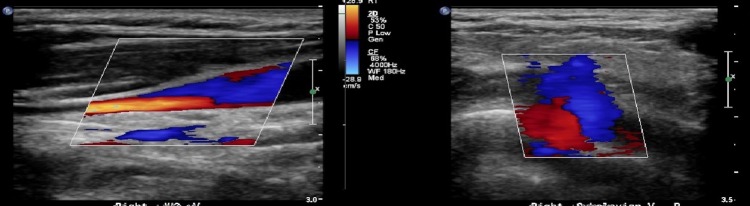
An UE ultrasound with Doppler revealed a thrombus in the right subclavian vein (figure 1). Subsequent chest CT angiogram further characterised the subclavian vein thrombus and identified a pulmonary embolus. Laboratory testing, including basic metabolic panel, pro-BNP and troponin, were all within normal limits. Only a D-dimer was elevated at 0.76.
Figure 1.
7 August 2014. Doppler ultrasound showing R subclavian vein with no flow in the mid and distal portions of the vein, along with visualised thrombus in the lumen. The R axillary vein was non-compressible and did not demonstrate flow or phasicity.
In the following months, she underwent a complete hypercoagulability work-up. Testing included complete blood count, comprehensive metabolic panel, serum protein electrophoresis, anticardiolipin antibody, IgA, IgM, IgG levels, β-2 glycoprotein I antibodies (A, G, M), protein S and protein C functional assay and quantitative level, factor V Leiden mutation, factor II level, lactate dehydrogenase, antinuclear antibody, erythrocyte sedimentation rate, fibrinogen activity, antithrombin activity and factor VIII activity. Haematology consultants at two additional major academic centres evaluated her results and agreed that they did not show a hypercoagulable state.
A work-up for TOS was also performed. Several postadmission venous studies were performed showing right subclavian vein and axillary vein compression with abduction, along with left axillary vein and axillary artery compression with abduction consistent with bilateral TOS, or Paget-Schroetter syndrome.
Differential diagnosis
TOS (Paget-Schroetter syndrome).
Upper extremity deep vein thrombosis.
Treatment
She was treated with therapeutic anticoagulation (rivaroxaban) for 6 months. However, she developed recurrent swelling and D-dimer elevation after stopping for 1 month. Treatment was thus restarted and she underwent treatment for a total of 12 months.
Outcome and follow-up
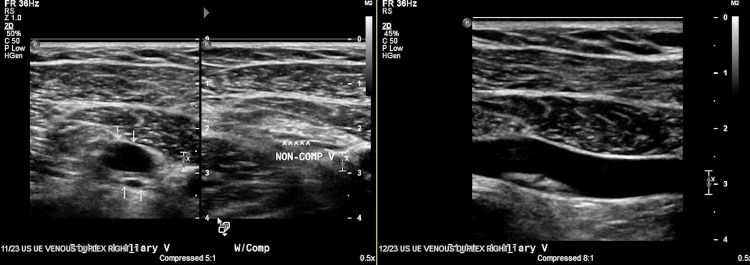
As listed above, she underwent haematology and vascular work-ups. Serial D-dimers remained elevated at 0.65 and 0.60 at 5 and 6 months, respectively. At 6 months, given the continued elevation of D-dimer, a repeat Doppler ultrasound revealed complete resolution of the right upper extremity thrombus, although there was a small focus of non-occlusive (probably chronic) thrombus in the medial right subclavian vein, along with persistent right axillary DVT (figure 2). There was interval restoration of flow in the right brachial veins. The patient resumed rivaroxaban given the D-dimer level and her post-thrombotic symptomatology of continued mild UE swelling. She completed 12 months of therapy and has not had any recurrence. She has been advised that if she were to pursue pregnancy, she should be treated with prophylactic enoxaparin.
Figure 2.
5 December 2014. Ultrasound showing flow and phasicity in the R subclavian vein. No intraluminal thrombus. R axillary vein was partially compressible with some flow and a non-occlusive intraluminal thrombus, which appeared occlusive on the prior study. These findings are compatible with a chronic DVT. DVT, deep venous thrombosis.
Discussion
This is a case of a young and healthy woman with an UEDVT that developed after undergoing OH. While our patient was taking OCPs at the time of her UEDVT, the temporal association of her clinical presentation to recently undergoing OH favours the latter as the most likely causative factor. Additionally, no association between UEDVT and OCP use has been identified.3 We conclude that previously undiagnosed TOS was the underlying predisposing anatomic factor.
While the association of OH and thromboembolic complications has been well reported, this typically occurs in the setting of an active pregnancy or in the setting of clinically overt OHSS.4–6 9 Our case is unique in that our patient was not pregnant nor did she show evidence of OHSS prior to her presentation. While this is the case in 20% of cases,6 the pathogenesis of UEDVT in these women is not understood, as usual risk factors such as catheters, indwelling devices and active malignancies are not present. Jugular or subclavian vein thrombosis has been reported as one of the complications of ART and is estimated to occur in 0.08–0.11% of treatment cycles, usually manifesting when the pregnancy test becomes positive and the clinical signs of OHSS have waned.6 10 The patient described in this case was diagnosed with UEDVT about 6–8 weeks postovarian stimulation, a timeline that parallels other reported cases (40 days after embryonic transfer, or 26.6 days after ovulation induction cycle).6 However, this patient had a previously undiagnosed predisposing anatomic risk factor (bilateral TOS) that makes her case unique. We failed to find a study that investigated whether TOS was present in other patients who developed UEDVT when undergoing ART.
Interestingly, pregnant women who conceived via ART are at higher risk of VTE throughout their pregnancies.11 12 Therefore, it is important that clinicians are aware of this adverse outcome in patients undergoing ovarian stimulation. Our case demonstrates a serious and potentially fatal complication of ART in the absence of pregnancy and in the absence of overt OHSS. Women who are undergoing ART should be counselled on the risk of thromboembolic complications, educated on prevention strategies such as minimising sedentary activities, prolonged travel and taught to recognise the early symptoms of VTE events. While widespread screening for TOS is impractical and likely cost ineffective, providers and patient should be aware of this possible underlying risk factor and assess for it prior to undergoing any ART.
Learning points.
Women undergoing ovarian stimulation are known to be at increased risk for thrombotic events in the presence of ovarian hyperstimulation syndrome.
Even in the absence of ovarian hyperstimulation syndrome, it appears that ovarian stimulation alone can serve as a risk factor for upper extremity deep venous thrombosis (UEDVT).
Thoracic outlet syndrome is a risk factor for UEDVT but can be aggravated by other prothrombotic conditions.
Footnotes
Contributors: ACMC and AWM were equal contributors in writing, editing and researching the manuscript. JA provided editing and scientific feedback, and oversaw the process.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Joffe HV, Kucher N, Tapson VF et al. for the Deep Vein Thrombosis (DVT) FREE Steering Committee. Upper-extremity deep vein thrombosis: a prospective registry of 592 patients. Circulation 2004;110:1605–11. 10.1161/01.CIR.0000142289.94369.D7 [DOI] [PubMed] [Google Scholar]
- 2.Prandoni P, Polistena P, Bernardi E et al. Upper-extremity deep vein thrombosis. risk factors, diagnosis, and complications. Arch Intern Med 1997;157:57–62. 10.1001/archinte.1997.00440220061008 [DOI] [PubMed] [Google Scholar]
- 3.Martinelli I, Battaglioli T, Bucciarelli P et al. Risk factors and recurrence rate of primary deep vein thrombosis of the upper extremities. Circulation 2004;110:566–70. 10.1161/01.CIR.0000137123.55051.9B [DOI] [PubMed] [Google Scholar]
- 4.Chan WS, Dixon ME. The “ART” of thromboembolism: a review of assisted reproductive technology and thromboembolic complications. Thromb Res 2008;121:713–26. 10.1016/j.thromres.2007.05.023 [DOI] [PubMed] [Google Scholar]
- 5.Whelan JG III, Vlahos NF. The ovarian hyperstimulation syndrome. Fertil Steril 2000;73:883–96. 10.1016/S0015-0282(00)00491-X [DOI] [PubMed] [Google Scholar]
- 6.Chan WS, Ginsberg JS. A review of upper extremity deep vein thrombosis in pregnancy: unmasking the ‘ART’ behind the clot. J Thromb Haemost 2006;4:1673–7. 10.1111/j.1538-7836.2006.02026.x [DOI] [PubMed] [Google Scholar]
- 7.Salomon O, Schiby G, Heiman Z et al. Combined jugular and subclavian vein thrombosis following assisted reproductive technology—new observation. Fertil Steril 2009;92:620–5. 10.1016/j.fertnstert.2008.07.1708 [DOI] [PubMed] [Google Scholar]
- 8.Grant J, Stevens S, Woller S et al. Diagnosis and management of upper extremity deep-vein thrombosis in adults. J Thromb Haemost 2012;108:1097–108. 10.1160/TH12-05-0352 [DOI] [PubMed] [Google Scholar]
- 9.Seong SW, Park JH, Shin SK et al. A case with upper extremity deep vein thrombosis after in vitro fertilization. J Cardiovasc Ultrasound 2010;18:98–100. 10.4250/jcu.2010.18.3.98 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bernardi E, Pesavento R, Prandoni P. Upper extremity deep venous thrombosis. Semin Thromb Hemost 2006;32:729–36. 10.1055/s-2006-951458 [DOI] [PubMed] [Google Scholar]
- 11.Henriksson P, Westerlund E, Wallen H et al. Incidence of pulmonary and venous thromboembolism in pregnancies after in vitro fertilisation: cross sectional study. BMJ 2013;346:e8632 10.1136/bmj.e8632 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rao AK, Chitkara U, Milki AA. Subclavian vein thrombosis following IVF and ovarian hyperstimulation: a case report. Hum Reprod 2005;20:3307–12. 10.1093/humrep/dei235 [DOI] [PubMed] [Google Scholar]