Description
A 73-year-old woman was referred to our gynaecology clinic with a 2-week history of pelvic and vaginal pain. The pelvic ultrasound and CT scan suggested a 10 cm haematometra and a 4 cm cervical cyst (figures 1–4).
Figure 1.

Pelvic ultrasound scan featuring a large haematometra.
Figure 2.

Tranvaginal ultrasound scan—cystic area at cervix initially reported as a nabothian cyst.
Figure 3.

CT scan sagittal view—uterus enlarged with haematometra.
Figure 4.
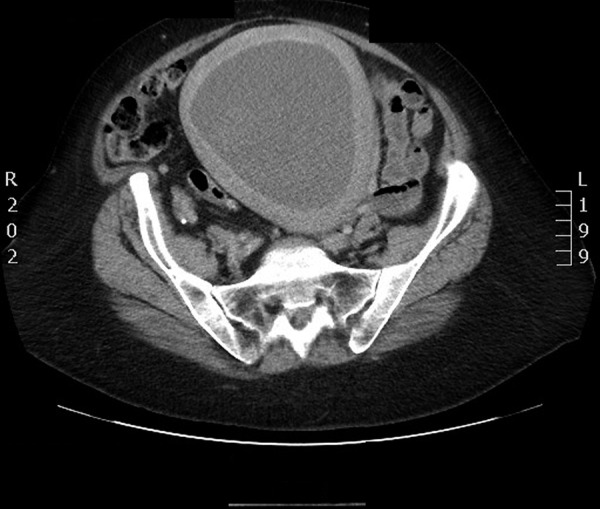
Uterus enlarged with haematometra.
She had no history of postmenopausal bleeding and her most recent pap smear was normal.
The patient had been using tamoxifen for the previous 10 years for primary breast cancer.
Examination revealed a large, mobile uterus and what appeared to be a cervical mass obscuring the cervical os.
She was booked for an examination under anaesthesia and hysteroscopy.
Prior to the procedure she presented with worsening suprapubic pain. She was febrile and tender suprapubically. An emergency EUA was performed with a presumptive diagnosis of an infected haematometra.
At time of surgery the initial cervical mass was found to be a large haematocervix with stenosis of the external os. The cervix was incised and dilated which drained 800 mL of old blood from the cervix and uterus. The underlying endometrium appeared normal on hysteroscopy. Histology was also normal.
She was discharged home well on day 4 postoperatively.
Learning points.
Cervical stenosis can occur as a result of hypo-oestrogenism and vaginal atrophy.1
Haematometra in a postmenopausal woman requires investigation for underlying malignancy.
Footnotes
Contributors: ME-B was consultant gynaecologist in charge of the case. EH managed the emergency admission and performed the procedure. NE collected data and images for the article. All authors contributed to the article.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
Reference
- 1.Pandit L, Ouslander GJ. Post menopausal vaginal atrophy and atrophic vaginitis. Am J Med Sci 1997;314:228–31. [DOI] [PubMed] [Google Scholar]


