Abstract
A 46-year-old man was referred to our ear, nose and throat department after the accidental discovery of a large retrotracheal mass. In order to obtain the diagnosis and to plan treatment he underwent a full battery of tests (CT, MRI, blood tests, hormonal assays, ultrasounds, thyroid scintigraphy, urine tests and fine-needle aspiration of the mass), but none of these was able to define the true nature of such cervical mass. Only after surgical excision and histological evaluation, it was diagnosed as an exceptional case of giant non-functional parathyroid adenoma.
Background
Parathyroid adenoma is the most common cause of primary hyperparathyroidism (pHPT). Usually, the baseline secretion of parathyroid hormone (PTH) is increased1 and blood tests (increased calcium and PTH serum levels) allow a swift diagnosis.2 At present, the majority of patients with pHPT are asymptomatic (80%).3–5 Only few patients become symptomatic, with classical hypercalcaemia-related problems such as recurrent nephrolithiasis, asthenia, peptic ulcer disease, bone pain, etc.6 In these patients, the sole diagnostic challenge is localising the adenoma and correctly identifying the few cases of multiple adenomas or hyperplasia. On the other hand, silent parathyroid adenomas not associated with abnormal PTH secretion are extremely uncommon.
Sometimes adenomas are larger than normal glands and, anecdotally, they can grow to a relevant size (the so-called ‘giant’ adenomas).7–10 Giant adenomas are defined as weighting ≥95th centile or ≥3.5 g11 and virtually all of them are PTH-secreting.
This report describes an exceptional case of non-functional parathyroid adenoma. The clinical challenges related to approaching a totally non-secreting mass are considered in depth.
Case presentation
An otherwise healthy 46-year-old man was referred to the neurosurgery department on reporting increasing cervical pain, radiating to the right upper limb, and paraesthesia. A plain MRI (figure 1) showed an extramedullary expansive lesion located at C5 (12 mm). Unexpectedly MRI also showed a huge retrotracheal mass (5.3 cm, extending from C6 to D3), which was clearly not associated with the neurological symptoms. Being the neck mass asymptomatic and since the C5 lesion was causing excruciating pain, the patient was first referred for neurosurgical treatment. After undergoing neurosurgical excision of the first mass (right C4–C5 hemilaminectomy) the patient was referred to our ear, nose and throat department in order to define the nature of the retrotracheal mass.
Figure 1.

MRI showing the presence of an extramedullary lesion and a retrotracheal mass.
Investigations
A thorough medical history review, the head and neck physical examination and flexible upper aerodigestive tract endoscopy yielded no results. The patient was asymptomatic (specifically, he denied compressive symptoms such as dyspnoea or dysphagia) and no further clinical sign could be identified.
A chest and neck CT scan with contrast medium was performed (figure 2). The radiology report described a paraoesophageal and prevertebral mass (40×36×53 mm), located posteriorly to the right thyroid pole and extending from C6 to D3. The lesion showed an inhomogeneous contrast enhancement.
Figure 2.
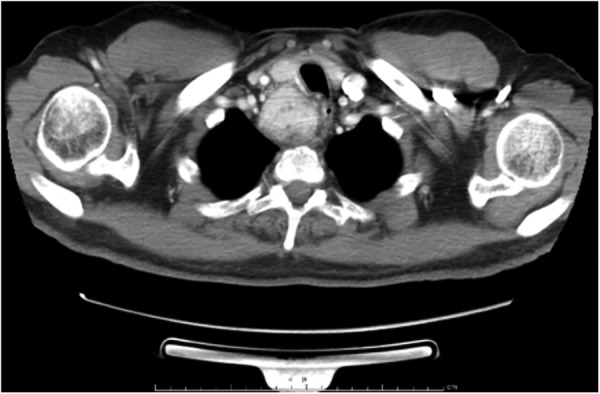
CT scan with contrast medium confirms the presence of a retrotracheal, retrothyroideal, prevertebral and paraesophageal mass (40×36×53 mm).
Even if the patient did not report any specific symptoms, the radiological findings and local anatomy showed a benign thyroid or parathyroid-related neoplasm. The patient was therefore prescribed blood calcium, phosphorus and hormonal assays. In order to rule out an atypical pheochromocytoma, urinary vanillylmandelic acid was tested too. Table 1 shows the results of blood and urine tests.
Table 1.
Blood and urine test results
| Results | Range | |
|---|---|---|
| Calcium (serum) (mg/dL) | 9.2 | 8.4–10.2 |
| Phosphorus (serum) (mg/dL) | 4.4 | 2.5–4.5 |
| PTH (serum) (pg/mL) | 70.03 | 8.7–79.6 |
| TSH (serum) (µIU/L) | 0.13 | 0.465–4.680 |
| FT3 (serum) (pg/mL) | 4.93 | 2.77–5.27 |
| FT4 (serum) (ng/mL) | 1.98 | 0.78–2.19 |
| Vanillymandelic acid (urine) (mg/hour) | 2.76/24 | 1–11/24 |
FT3, free triiodothyronine; FT4, free thyroxine; PTH, parathyroid hormone; TSH, thyroid-stimulating hormone.
Following the report of reduced thyroid-stimulating hormone (TSH), the patient underwent neck ultrasound (US) scanning and thyroid scintigraphy, which yielded unspecific results.
The results of calcium, phosphorous and PTH serum levels were all within normal limits. Consequently, parathyroid scintigraphy (99mTc sestamibi) was deemed worthless and the presence of parathyroid adenoma was ruled out.
The patient therefore underwent an endoscopic US-guided transoesophageal fine-needle aspiration, aiming to determine the cytological and immunophenotypic features of the mass. The immunophenotypes were: chromogranin A and synaptophysin positive and PTH, calcitonin, thyroglobulin and p63 negative; Ki67 was 1%. The final cytological report described the lesion as an unspecified cell proliferation with neuroendocrine differentiation.
Having failed all the other investigations, the only way to discover the real nature of the mass was the histological examination following the complete surgical excision. Microscopically there was no necrosis, no mitosis and Ki67 was <2%. The immunophenotypes were cytokeratin 8, 18 and 19 and synaptophysin positive and PTH and ps100 were negative. The whole proliferation was partially delimited by a thin PTH+layer. The mass was finally diagnosed as a giant non-PTH-secreting parathyroid adenoma.
Differential diagnosis
In this case differential diagnosis is clearly wide and challenging.
The radiological features of the mass (moderate contrast enhancement, inhomogeneity, absence of necrosis or local invasion) showed a benign neoplasm but a reliable diagnosis could not be formulated.
The first hypothesis was a thyroid nodule, which should be diagnosed either through hormonal assays (TSH reflex), US or thyroid scintigraphy.
The second hypothesis was a parathyroid adenoma, which can manifest with increased calcium and PTH serum levels. In this case the blood tests were normal, so a parathyroid adenoma was ruled out and other investigations such as technetium parathyroid scintigraphy12 were not performed.
The previous potential differential diagnosis was a neuroendocrine mass: more specifically, pheochromocytomas may be located outside of the adrenal glands, presenting as paragangliomas. Pheochromocytomas cause abnormal catecholamine secretion and high levels of urinary vanillylmandelic acid usually allow the diagnosis.
Since the diagnosis was not clear even after the most thorough evaluations, the only chance for a conclusive diagnosis was histological analysis following surgical excision.
Treatment
The patient underwent excision of the mass under general anaesthesia via an open cervical approach extended to the right side (figure 3). After the anatomical dissection of the cervical layers, the mass was identified posteriorly to the trachea and the recurrent laryngeal nerve, firmly adhering to the inferior pole of the right thyroid lobe. Surprisingly enough, the mass was similar to a parathyroid gland in its appearance and texture (figure 3). After ligating some major neovessels, the mass was excised en bloc and sent for histological evaluation. On macroscopic examination the mass appeared brownish and homogeneous. The mass measured 5.5×4×2.5 cm (figure 4) and weighed about 42 g.
Figure 3.
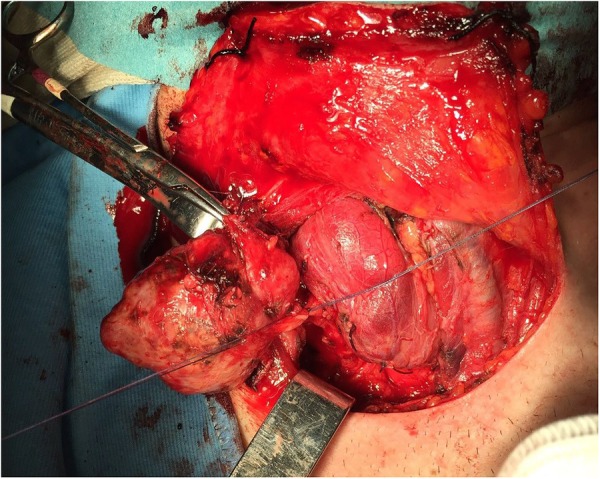
Open cervical approach extended to the right side. Excision of the mass.
Figure 4.

Mass excised (5.5×4×2.5 cm).
After positioning two active closed drains, the suture was closed.
Outcome and follow-up
The patient had an unremarkable postoperative recovery. Calcium and PTH serum levels were measured every other day and their levels always were within normal limits. The patient was discharged on day 5. Radiological and clinical 1year follow-up showed no signs of recurrence, while blood electrolytes and serum PTH, measured every 3 months always were within normal limits.
Discussion
Parathyroid adenomas are the most common cause of pHPT13 14 and usually induce increased calcium and PTH serum levels or clinically manifest with classical signs and symptoms (recurrent nephrolithiasis, asthenia, etc).
Sometimes adenomas grow noticeably, reaching relevant sizes and becoming ‘giant adenomas’; the biggest adenoma currently reported in the literature measured 8×5×3.5 cm and weighed 110 g.10 There are few reported cases in the literature concerning giant parathyroid adenomas7–10 and most of them were responsible for increased PTH and calcium serum levels.15–17 Some authors postulated a correlation between the weight of the adenoma, the functional activity of the gland and the severity of the blood tests alteration.18–20
Spanheimer et al11 referred to giant adenomas as a distinct clinical entity. They tried to characterise the patients with giant parathyroid adenoma and compared them with other patients with pHPT; they concluded that ‘giant adenomas present with increased serum calcium and PTH levels and have higher rate of asymptomatic disease’.
In exceptional cases parathyroid adenomas are clinically silent due to a non-PTH-secreting behaviour.21–23 In these cases differential diagnosis is way more challenging, blood tests results being misleading (calcium and PTH serum levels within normal limits).
This case is particularly interesting because it is very uncommon to find a parathyroid adenoma that is giant and non-PTH secreting; to the best of our knowledge only Kiverniti et al24 described a similar case. Probably the pathophysiological mechanism underlying this kind of lesions is different from classical parathyroid adenoma; more studies are needed to understand such atypical and rare neoplasms.
Concluding, it is important to point out the difficulties of approaching a mass that is totally non-secreting: in our case the parathyroid origin of the mass was confirmed only after histological analysis.
Learning points.
Parathyroid adenomas are the most common cause of primary hyperparathyroidism.
Parathyroid adenomas are usually characterised by an increased secretion of PTH and, consequently, hypercalcaemia.
Sometimes adenomas are bigger than normal parathyroid glands and in rare cases they reach relevant dimensions (‘giant adenoma’).
Non-PTH-secreting parathyroid adenomas are extremely uncommon lesions. Giant non-secreting parathyroid adenomas should be considered exceptional findings. In these cases the diagnostic challenge is raised and the real nature of the mass can be revealed only after histological analysis.
Footnotes
Contributors: AM and LDP performed the surgery. AM is a senior ENT consultant. LDP is a senior endocrine surgeon consultant. AMS and CM wrote the article.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Harms H, Schlinke E, Neubauer O. Pulse amplitude and frequency modulation of parathyroid hormone in primary hyperparathyroidism. J Clin Endocrinol Metab 1994;78:53–7. [DOI] [PubMed] [Google Scholar]
- 2.Bilezikian J, Brandi ML, Rubin M et al. Primary hyperparathyroidism: new concepts in clinical, densitometric and biochemical features. J Intern Med 2005;257:6–17. 10.1111/j.1365-2796.2004.01422.x [DOI] [PubMed] [Google Scholar]
- 3.Fraser WD. Hyperparathyroidism. Lancet 2009;374:145–58. 10.1016/S0140-6736(09)60507-9 [DOI] [PubMed] [Google Scholar]
- 4.Agarwal G, Prasad KK, Kar DK et al. Indian primary hyperparathyroidism patients with parathyroid carcinoma do not differ in clinicoinvestigative characteristics from those with benign parathyroid pathology. World J Surg 2006;30:732–42. 10.1007/s00268-005-0366-5 [DOI] [PubMed] [Google Scholar]
- 5.Rubin MR, Bilezikian JP, McMahon DJ et al. The natural history of primary hyperparathyroidism with or without parathyroid surgery after 15 years. J Clin Endocrinol Metab 2008;93:3462–70. 10.1210/jc.2007-1215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kelly KJ, Chen H, Sippel RS. Primary hyperparathyroidism. Cancer Treat Res 2010;153:87–103. 10.1007/978-1-4419-0857-5_6 [DOI] [PubMed] [Google Scholar]
- 7.Neagoe RM, Sala DT, Borda A et al. Clinicopathologic and therapeutic aspects of giant parathyroid adenomas—three case reports and short review of the literature. Rom J Morphol Embryol 2014;55(Suppl 2):669–74. [PubMed] [Google Scholar]
- 8.Sisodiya R, Kumar S, Palankar N et al. Case report on giant parathyroid adenoma with review of literature. Indian J Surg 2013;75:21–2. 10.1007/s12262-011-0306-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tsuchiya A, Endo S, Abe R. Giant adenoma of the parathyroid: report of a case. Surg Today 1993;23:465–7. 10.1007/BF00309509 [DOI] [PubMed] [Google Scholar]
- 10.Power C, Kavanagh D, Hill AD et al. Unusual presentation of a giant parathyroid adenoma: report of a case. Surg Today 2005;35:235–7. 10.1007/s00595-004-2902-6 [DOI] [PubMed] [Google Scholar]
- 11.Spanheimer PM, Stoltze AJ, Howe JR et al. Do giant parathyroid adenomas represent a distinct clinical entity? Surgery 2013;154:714–19. 10.1016/j.surg.2013.05.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.https://www.aimn.it/pubblicazioni/LG/RP_AIMN_paratiroidi.pdf (accessed 26 Feb 2016).
- 13.van Heerden JA, Grant CS. Surgical treatment of primary hyperparathyroidism: an institutional perspective. World J Surg 1991;15:688–92. 10.1007/BF01665301 [DOI] [PubMed] [Google Scholar]
- 14.van Heerden JA, Beahrs OH, Woolner LB. The pathology and surgical management of primary hyperparathyroidism. Surg Clin North Am 1977;57:557–63. [DOI] [PubMed] [Google Scholar]
- 15.Fahey T, Hibbert E, Brady P et al. Giant double parathyroid adenoma presenting as a hypercalcaemic crisis. Anz J Surg 1995;65:292–4. 10.1111/j.1445-2197.1995.tb00634.x [DOI] [PubMed] [Google Scholar]
- 16.Furrer M, Leutenegger AF, Rüedi T. Thoracoscopic resection of an Ectopic giant parathyroid adenoma: indication, technique, and three years follow-up. Thorac Cardiovasc Surg 1996;44:208–9. 10.1055/s-2007-1012018 [DOI] [PubMed] [Google Scholar]
- 17.Agarwal A, Pradhan R, Kumari N, et al.. Molecular characteristics of large parathyroid adenomas. World J Surg 2016;40:607–14. 10.1007/s00268-015-3380-2 [DOI] [PubMed] [Google Scholar]
- 18.Rao DS, Honasoge M, Divine GW et al. Effect of vitamin D nutrition on parathyroid adenoma weight: pathogenetic and clinical implications. J Clin Endocrinol Metab 2000;85:1054–8. [DOI] [PubMed] [Google Scholar]
- 19.Mòzes G, Curlee K, Rowland C et al. The predictive value of laboratory findings in patients with primary hyperparathyroidism. J Am Coll Surg 2002;194: 126–30. 10.1016/S1072-7515(01)01139-5 [DOI] [PubMed] [Google Scholar]
- 20.Hedbäck G, Odén A, Tisell L. Parathyroid adenoma weight and the risk of death after treatment for primary hyperparathyroidism. Surgery 1995;117:134–9. 10.1016/S0039-6060(05)80076-5 [DOI] [PubMed] [Google Scholar]
- 21.Sekine O, Hozumi Y, Takemoto N et al. Parathyroid adenoma without hyperparathyroidism. Jpn J Clin Oncol 2004;34:155–8. 10.1093/jjco/hyh028 [DOI] [PubMed] [Google Scholar]
- 22.Marchesi M, Biffoni M, Benedetti RN et al. Incidental parathyroid adenomas with normocalcemia discovered during thyroid operations: report of three cases. Surg Today 2001;31:996–8. 10.1007/s005950170009 [DOI] [PubMed] [Google Scholar]
- 23.Poppe K, Pipeleers-Marichal M, Flamen P, et al.. Non-secreting atypical parathyroid adenoma. J Endocrinol Invest 2001;24:107–10. 10.1007/BF03343823 [DOI] [PubMed] [Google Scholar]
- 24.Kiverniti E, Kazi R, Rhys-Evans P et al. Airway obstruction due to giant non-parathyroid hormone-producing parathyroid adenoma. J Can Res Ther 2008;4:197 10.4103/0973-1482.44292 [DOI] [PubMed] [Google Scholar]


