Abstract
Background
Workforce experts predict a future shortage of cardiologists that is expected to impact rural areas more severely than urban areas. However, there is little research on how rural patients are currently served through clinical outreach. This study examines the impact of cardiology outreach in Iowa, a state with a large rural population, on participating cardiologists and on patient access.
Methods and Results
Outreach clinics are tracked annually in the Office of Statewide Clinical Education Programs Visiting Medical Consultant Database (University of Iowa Carver College of Medicine). Data from 2014 were analyzed. In 2014, an estimated 5460 visiting consultant clinic days were provided in 96 predominantly rural cities by 167 cardiologists from Iowa and adjoining states. Forty‐five percent of Iowa cardiologists participated in rural outreach. Visiting cardiologists from Iowa and adjoining states drive an estimated 45 000 miles per month. Because of monthly outreach clinics, the average driving time to the nearest cardiologist falls from 42.2±20.0 to 14.7±11.0 minutes for rural Iowans. Cardiology outreach improves geographic access to office‐based cardiology care for more than 1 million Iowans out of a total population of 3 million. Direct travel costs and opportunity costs associated with physician travel are estimated to be more than $2.1 million per year.
Conclusions
Cardiologists in Iowa and adjoining states have expanded access to office‐based cardiology care from 18 to 89 of the 99 counties in Iowa. In these 71 counties without a full‐time cardiologist, visiting consultant clinics can accommodate more than 50% of office visits in the patients’ home county.
Keywords: access to care, cardiology, geographic variation, rural outreach, workforce
Subject Categories: Health Services
Introduction
Heart disease is the leading cause of death in the United States.1 While the mortality rate from cardiovascular disease (CVD) has fallen over time, the number of patients with CVD is growing and will accelerate as the population ages.2 Lifestyle factors including obesity, diabetes, inactivity, and smoking will contribute to this growth.3 In addition to higher demand, another factor impacting access is the prediction that cardiologists may be retiring at a higher rate than expected, based on past experience.4 This has prompted rising concern about the adequacy of the overall cardiology workforce.4, 5
The future incidence of CVD may be higher among the 62 million Americans6 living in rural areas. This higher rate of CVD is attributable to the out‐migration of young people and the in‐migration of retirees, suggesting that the population of rural America is aging more rapidly than in urban areas.7, 8 Rural residents report higher levels of CVD risk factors including smoking, obesity, and inactivity than people in urban areas.9 Rural residents also report higher levels of heart disease, hypertension, and stroke than their urban counterparts.9
Because of various factors, cardiologists are less likely to establish a full‐time practice in rural areas.10 This shortage has persisted despite the growth in the overall cardiology workforce in recent years.11 Consequently, rural patients have fewer overall visits to specialists and tend to rely more on care provided locally by primary care physicians.12
Recent research suggests that rural patients with CVD might benefit from care provided by a cardiologist rather than relying solely on one's primary care provider. For example, patients with unstable angina treated by cardiologists were more likely to receive effective treatments and had lower mortality than those being treated solely by an internist.13 Other studies show that follow‐up care (post–emergency room discharge) involving a cardiologist and primary care physician reduced the likelihood of mortality for heart failure patients.14, 15 In addition, a follow‐up consultation with a cardiologist reduced the likelihood of mortality for both low‐risk16 and high‐risk17 patients admitted to the emergency room for chest pain. Therefore, if rural patients with CVD had better access to cardiologists, their outcomes could improve.
In 2007, the American College of Cardiology commissioned a study to assess the future supply of cardiologists and the demand for their services.4 This report, released in 2009, concluded that the United States had a then‐current shortfall of 1700 general cardiologists, which could grow almost 10‐fold by 2025.18 The same report18 suggested that “the growing shortage of cardiologists is likely to affect traditionally underserved communities such as low income or rural communities most profoundly.” One of their recommendations was to research best practices for serving outreach communities.18 This would include assessing the costs and benefits of outreach as well as tracking access in underserved rural and low‐income communities.18
One option for serving rural communities is telehealth. In New Mexico, Project ECHO connects rural primary care providers with university‐based specialists using teleheath.19 The University of Virginia Center for Telehealth supports telehealth access for many locations across the state.20 Patients using the face‐to‐face video service have avoided many miles of travel by seeing a specialist without leaving their own communities.20 Medicare does allow for reimbursement for telehealth office visits for patients living in rural areas,20 so long as patients are located in an approved facility within a rural health professional shortage area or a critical access hospital.21
There are challenges to using telehealth to expand access to cardiologists in rural areas. For example, few rural hospitals have operational cardiology‐related telehealth programs. Using data from 2013, a recent national study of 4727 US hospitals22 found that only 6.2% of rural hospitals had an operational cardiology, stroke, or heart attack telehealth program (the comparable figure for urban hospitals was 7.2%). Overall, 66% of rural hospitals had no operational telehealth programs of any kind (the comparable figure for urban hospitals is 68%). In addition to organizational barriers, patient attitudes towards telehealth are not always supportive. For example, a recent general population survey of patients in Montana, a state with multiple telehealth networks serving many rural areas, found that more than 43% of respondents were “unequivocally averse to telemedicine” despite the obvious benefits of reducing patient travel.23 Given these conditions, quickly expanding rural access to cardiology care through telemedicine may be difficult.
A second option for providing access to cardiology care in rural communities, and the focus of this study, is the visiting consultant clinic (VCC) approach.24, 25 A VCC is an arrangement for regular visits to a rural site by a cardiologist, usually one from a nearby urban area.24, 25 These clinics are a collaborative effort between a cardiology practice and a rural hospital (or clinic) located in communities that are too small to support their own specialist.24
Specialist physician outreach involving physician travel to rural locations has been a strategy to expand access to health care in many countries.26 A Cochrane review of the clinical literature suggests that specialist outreach improves access to specialty care for rural residents, increases the quality of care available in rural areas, and results in better health outcomes.26 In other countries, the programs of visiting specialists are organized by national‐ or regional‐level health planners.26 In contrast, VCC in the United States are a “market‐driven” solution and originate from agreements between independent entities.27
In this study, we focus on the VCC approach to rural outreach in Iowa, a state with a large rural population (ie, 36% in 2010). Iowa provides an interesting case study to evaluate the costs and benefits of rural outreach through VCCs. Based on data from 2014, the per capita cardiologist ratio in Iowa is 6.82 per 100 000 in population. This compares to the national average of 7.82 cardiologists per 100 000 in population in 2013.28 Despite the apparent shortage, cardiologists from Iowa and surrounding states have been staffing a large number of VCCs in predominantly rural areas of the state for many years.24
It must be noted that telemedicine usage in Iowa lags behind much of the country. As of 2014, Iowa was 1 of only 4 states that did not cover telemedicine under Medicaid with exceptions for selected mental health conditions,29 and Iowa did not require private insurers to cover telemedicine services.21 One indicator of the state of telehealth in Iowa is that the Iowa Board of Medicine did not establish physician practice standards for telemedicine until June 2015.30
In this study, we examined data from a statewide workforce database documenting the location, frequency, and physician participation in cardiology VCCs in Iowa for the year 2014. The goals of the study were to evaluate the extent of involvement of cardiologists in rural outreach, the costs to participating cardiologists, and the benefits of this approach of providing cardiology care in rural communities.
Methods
Study Setting
The cardiology VCC is similar to any office visit in which the cardiologist obtains patient histories, conducts physical examinations, and orders available lab and radiology tests. Cardiologists can provide preprocedure evaluations and postprocedure follow‐up. In the VCC setting, cardiologists are limited to noninvasive procedures, usually diagnostic tests such as stress tests, treadmill tests, Holter monitors, ECGs and, where available, echocardiograms. The visiting cardiologists also consult with patients’ primary care physicians, increasing the opportunity for better‐coordinated care for patients. For more invasive procedures, patients seen in the VCC setting are referred to larger, urban hospitals with the appropriate staff and equipment.21 The relationship between the visiting cardiologist and hosting institution is codified in an agreement that covers such issues as clinic frequency, services to be offered in the rural hospital/clinic, and payments for the space used by the visiting cardiologist.
While the focus of this study is the effect of cardiology VCCs on access for rural patients, a primary motivation for cardiologists to staff these clinics is to expand and maintain their referral base.24, 25, 27 At the same time, participating hospitals benefit from these arrangements since they retain the revenue from lab, radiology, and other tests that might otherwise go to a larger urban hospital where the cardiologist has his or her primary practice location. In addition, rural hospitals that host VCCs may improve their overall status within the community by facilitating access to specialty care in a patient's own community. Furthermore, by providing regular contact with specialists, VCCs can reduce the perceived professional isolation of the local medical community.24, 25, 26, 27
Data Sources
The Office of Statewide Clinical Education Programs at the University of Iowa Carver College of Medicine maintains the Iowa Physician Information System. This statewide registry of all practicing physicians in Iowa is updated through various means including twice per year telephone census of all work sites in Iowa that employ health professionals. The Iowa Physician Information System tracks a physician's practice locations including visiting consultant clinic sites. The Iowa Physician Information System also contains information about the physician's self‐identified specialty, age, sex, medical school, and location/dates of graduate medical education.
The VCC data used in this study come from the Annual Report on Iowa's Visiting Medical Consultant Activity. These data include the locations and frequencies of all cardiology VCCs as well as the names and affiliations of the physicians involved with each outreach site. Statewide data collection on VCCs began in 1989.
Physician Involvement Statistics
We tested for differences in VCC participation by sex and specialty using the χ2 statistic. The difference in age by VCC participation was tested using a t statistic.
To estimate driving distances, locations of the primary practice sites for cardiologists and the VCC sites were identified using the latitude and longitude data provided by US Census Bureau place (city) data. Driving distances for visiting cardiologists (ie, from primary practice locations to VCC locations) were estimated using MPMileCharter and Microsoft MapPoint. Differences in driving distances between Iowa‐based and out‐of‐state cardiologists were tested using a t statistic.
Costs for Participating Cardiologists
To estimate the costs of providing cardiology care through VCC outreach, we estimated the direct travel costs and opportunity costs associated with travel for participating cardiologists. Opportunity costs associated with travel time and distance were estimated following the methods used in studies of specialist outreach clinics in the United Kingdom31, 32 and psychiatrist outreach to Native American populations in New Mexico.33
To estimate travel costs, driving times and distances for visiting cardiologists (ie, from primary practice locations to VCC locations) were also estimated using MPMileCharter and Microsoft MapPoint using the latitude/longitude information described above. For mileage costs, we used the 2014 Internal Revenue Service business mileage rate of $0.56/per mile. Using the government mileage rate is consistent with recent research evaluating physician travel costs to rural sites.34
To estimate the time for each trip to an outreach site, we used the estimated travel time from the cardiologist's primary practice location to the VCC site.33 For each VCC, the total travel time estimate is the 1‐way travel time×average number of trips per month×24 (2 trips per clinic day and 12 months a year).
Data from 2013 estimates the average compensation for a cardiologist at $351 000.35 Assuming a yearly workload of 2080 hours, this translates into average hourly compensation of $168.75.
Benefits
Rural outreach by physicians—either in‐person or virtual—benefits patients by reducing the distance and time they need to travel to receive medical care.36 Evaluations of rural outreach programs in the United States use a reduction in travel distance for patients and the number of patient visits as measures of success whether the encounter is face‐to‐face37 or facilitated via telehealth technology.20 To assess the potential benefits of cardiology VCCs in Iowa, we measure how VCCs affect the average travel distance for patients in all census tracts. This approach is consistent with prior studies of rural access to specialist physicians.12, 38
The impact of cardiology VCCs on average patient travel time is likely to vary based on whether the patient lives in an urban area or an isolated rural area. Each census tract was classified using the zip code–level rural–urban commuting area codes from 2010.39 The 10 primary rural–urban commuting area codes designations were aggregated into 4 categories: Urban area (codes 1, 2, and 3), large rural city (codes 4, 5, and 6), small rural town (code 7, 8, and 9), and isolated rural area (code 10). The first category includes urban or metropolitan areas (ie, population centers of 50 000 or more residents). The second category consists of large rural cities with population centers between 10 000 and 49 999. The third category includes small rural towns with population centers between 2500 and 9999. Finally, there are isolated rural areas with population centers of less than 2500. These latter 3 categories (large rural cities, small rural towns, and isolated rural areas) are all considered rural (or nonmetropolitan) areas.
We used latitude and longitude data from the 2010 US Census at the census tract level. Driving times between census tract centroids and all cardiology primary practice locations were estimated using MPMileCharter and Microsoft MapPoint. This allows us to determine the closest primary practice location for each census tract in Iowa. In addition, we estimated the driving times between each VCC site and every census tract centroid. This allows us to identify the closest VCC location for each census tract. The difference between these 2 figures was determined for each census tract for the set of all cardiology VCC locations and a subset of cardiology VCC with a monthly frequency of 4 or more. The differences in driving distances were tested using the paired‐comparison t test for urban areas, large rural cities, small rural towns, isolated rural areas, and all rural census tracts. All estimates of driving distance were weighted by the population of the census tract relative to all census tracts with same designation (eg, all urban census tracts).
To illustrate the effect of cardiology VCCs at the population level, we computed the cumulative distribution of the population located within a given driving time (eg, 10, 20, 30, etc minutes) of the nearest primary practice location of a cardiologist in Iowa or an adjoining state. Population estimates for all census tracts in Iowa (2010) were obtained from the US Census. This summary measure has been used in prior research to illustrate the overall level of access to specialist physicians based on travel distance for the entire population of patients (ie, across all urban and rural areas).38, 40, 41, 42, 43
Demand for Cardiology Office Visits in Rural Iowa
To provide context for the amount of cardiology care being provided through VCCs, we estimated the demand for office‐based cardiology care in those Iowa counties without a full‐time cardiologist where a regular VCC is available. Using estimates from prior research,31, 44, 45 we also estimated the number of office visits facilitated by the VCCs in rural Iowa.
To estimate the demand for cardiology office visits in rural counties of Iowa, we used the national demand estimates for cardiology office visits by age and sex from the 2010 National Ambulatory Medical Care Survey.46 Using national census data from 2010, we recalibrated the demand per 100 persons for 8 age–sex groups (<45, 45–64, 65–74, >75, and male/female). The number of residents by age and sex for each Iowa county was retrieved from the 2010 US Census. The resulting figures were combined to estimate the number of cardiology office visits by county.
We estimated the number of patients seen during each VCC day using data from the 2010 National Ambulatory Medical Care Survey.44 The average office visit for specialists in cardiovascular diseases was 21.4 minutes. Due to travel time, past research has assumed that a VCC day provides 5 hours of contact between the cardiologists and patients.45 Using the mean time figure would imply that cardiologists would see an average of 14 patients per clinic day. This figure is consistent with prior research in the UK on visiting specialist clinics.31 The mean number of patients seen across multiple visiting specialists in the United Kingdom (including cardiologists) was 15.8.
All statistical analyses were conducted using SPSS (Windows version 23).
Because this research used only publicly available data, institutional review board approval was not required.
Results
As of June 2014, the Iowa Physician Information System shows a total of 222 physicians with self‐identified specialties in cardiovascular disease (N=195), interventional cardiology (N=17), and clinical cardiac electrophysiology (N=10) practicing in Iowa. Overall, this results in a per capita ratio of 7.15 cardiologists per 100 000 in population. Excluding the specialists in clinical cardiac electrophysiology, the per capita ratio in Iowa is 6.82 cardiologists per 100 000 in population. This compares to the national average of 7.82 cardiologists (specialists in cardiovascular disease and interventional cardiology) in 2013.39 Their primary practice locations were in 18 of Iowa's 99 counties.
To reach patients in rural areas, in 2014, cardiologists from Iowa and surrounding states staffed 140 separate cardiology outreach clinics in 96 cities. Thirty‐five cities hosted multiple cardiology VCCs conducted by different cardiologists. A descriptive summary of these outreach clinics is presented in Table 1.
Table 1.
Profile of Cardiology VCCs in Iowa (2014)
| Count of cardiology VCCs: 140 in 96 different communities | |
| Community hospital | 122 (110 are in Critical Access Hospitals) |
| Community clinic | 18 |
| Estimated total clinic days in 2014: 5460 | |
| Distribution of location of cardiology VCC clinic days | |
| Urban area | 8% |
| Large rural city | 19% |
| Small rural town | 58% |
| Isolated rural area | 15% |
| Total number of cardiologists participating in VCC outreach: 167 | |
| Iowa | 100 |
| Nebraska | 30 |
| Minnesota | 13 |
| South Dakota | 12 |
| Illinois | 6 |
| Wisconsin | 6 |
| Distribution of visit frequency | |
| 1 visit per month | 26 |
| 2 to 3 visits per month | 57 |
| 4 or more visits per month | 57 |
| One‐way driving distances to VCC sites from primary practice locations | |
| <20 miles | 3 |
| 20 to 29 miles | 20 |
| 30 to 39 miles | 28 |
| 40 to 49 miles | 21 |
| 50 to 74 miles | 48 |
| 75 to 99 miles | 17 |
| 100+ miles | 3 |
VCCs indicates visiting consultant clinics.
Collectively, outreach through VCCs extended monthly access to a cardiologist to 71 additional counties. Based on data from the 2010 Census and 2010 National Ambulatory Medical Care Survey, the expected number of office visits to specialists in cardiovascular disease for the population residing in the 71 counties served by VCC outreach is 130 460.
Of the estimated 5460 VCC clinic days, only 8% were held in sites located in urban areas. More than 90% of VCC clinic days were held in locations considered to be rural. A total of 5052 clinic days were held in counties without a full‐time cardiologist. The estimated number of office visits facilitated through VCC outreach is 70 728. This represents 54% of the demand for office visits to specialists in cardiovascular disease for the population residing in these 71 counties.
A high proportion of cardiology VCC clinics days (72%) were staffed by Iowa physicians (105 clinics). One hundred (100) cardiologists from Iowa participated in a VCC in 2014. Based on the overall number of cardiologists practicing in Iowa in 2014 (N=222), 45% are involved in rural outreach activities. In addition, 67 cardiologists from adjoining states also staffed cardiology VCCs in Iowa in 2014.
Participation in VCC outreach was marginally related to sex (male VCC participation=47%, female VCC participation=32%, P<0.11) and unrelated to physician age (participating=52.7±9.9 years, nonparticipating=52.3±12.4 years, P<0.83) or self‐identified specialty (cardiovascular medicine VCC participation=47%, clinical cardiac electrophysiology VCC participation=40%, interventional cardiology VCC participation=29%, P<0.37).
Figure 1 contains a map of the primary practice sites and VCC sites in 2014. This map shows the locations of the VCCs and the primary practice locations of the participating cardiologists. The different colored lines are intended to help the reader distinguish between VCCs originating from different cities.
Figure 1.
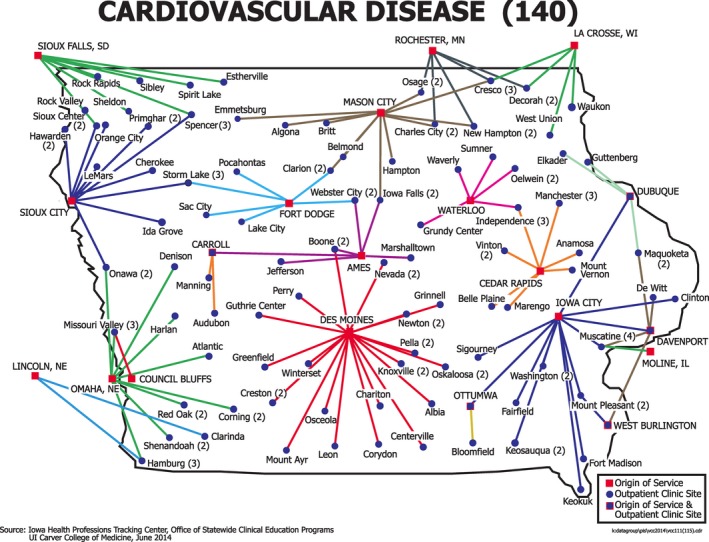
Locations of cardiology VCCs and primary practice locations of involved physicians (2014). VCCs indicates visiting consultant clinics.
The mean 1‐way (estimated) driving distance for all cardiologists participating in VCC activity is 46.5±18.6 miles. For non‐Iowa physicians, the comparable figure is 65.5±20.7 miles. This difference is significant (t=5.00, P<0.001).
Based on the estimated number of visits per month and driving distance, cardiologists from Iowa and adjoining states drive 45 813 miles per month to staff rural outreach clinics. On a yearly basis, the direct cost of travel to VCC sites is $307 865 per year (=549 759 miles per year×$0.56 per mile).
Assuming that only 1 cardiologist staffs each VCC day, total travel time for all VCCs in 2014 added up to a total of 10 939 hours at $168.75 per hour. The estimated yearly opportunity costs associated with travel to rural VCC sites is $1 845 956.
Effects of Cardiology VCCs on Patient Travel Distances
The mean 1‐way travel times for urban areas, large rural cities, small rural towns, and isolated rural areas were computed separately. The results are presented in Table 2.
Table 2.
Mean One‐Way Travel Times in Minutes by Urban/Rural Location: Iowa Census Tracts (2014)
| Urban Area | Large Rural City | Small Rural Town | Isolated Rural Town | All Rural Census Tracts | |
|---|---|---|---|---|---|
| A: Distance to nearest cardiologist primary practice location | 16.7±9.5 | 29.9±18.7 | 44.0±17.0 | 53.4±17.0 | 42.4±20.0 |
| B: Distance to nearest cardiologist primary practice location or cardiology VCC location with visit frequency of 1+ times per month | 14.9±6.9* | 13.4±11.1* | 10.3±9.5* | 20.9±9.7* | 14.7±11.0* |
| C: Distance to nearest cardiologist primary practice location or cardiology VCC location with a visit frequency of 4+ times per month | 15.4±7.6* | 14.4±11.5* | 15.4±13.6* | 29.5±12.8* | 19.5±14.3* |
| Number of census tracts | 420 | 121 | 131 | 152 | 404 |
VCC indicates visiting consultant clinic.
Significantly different from mean in Row A (Travel time to nearest cardiologist primary practice location) for a 2‐tailed, paired‐comparison t test. *P<0.001.
For patients living in urban areas, the average 1‐way travel time to the nearest cardiology primary practice site is 16.7±9.5 minutes. For Iowans in large rural cities, the mean 1‐way travel time to the nearest cardiology primary practice location is 29.9±18.7 minutes. For those living in small rural towns, the comparable average travel time is 44.0±17.0 minutes. For residents of isolated rural areas, the comparable average travel time is 53.4±17.0 minutes.
Travel times from all Iowa census tracts for a combined set of treatment locations (ie, cardiologist primary practice locations and VCC locations) were estimated. We conducted separate analyses for VCC sites with at least 1 clinic day per month and those with 4 or more clinic days per month. These results are also presented in Table 2.
For urban areas, there was a small (average=1.8 minutes) but statistically significant reduction in the travel time (t=6.1, P<0.001) as a result of the additional VCC locations.
Including the monthly VCC locations has a much larger impact on the estimated travel times for patients in rural areas of Iowa. The mean travel time for large rural cities drops from 29.9 to 13.4 minutes (t=9.1, P<0.001). For small rural towns, the mean travel time fell from 44.0 to 10.3 minutes (t=20.2, P<0.001). The mean travel time for isolated small towns fell from 53.4 to 20.9 minutes (t=21.9, P<0.001). For all rural census tracts, the mean travel time falls from 42.2 to 14.7 minutes (t=26.8, P<0.001). For cardiology VCC sites with a visit frequency of 4 or more times per month, the results are comparable.
To assess the impact of VCCs on patient access at the population level, the cumulative distribution of the population located within a given driving time (eg, 10, 20, 30, etc minutes) of the nearest primary practice location of a cardiologist in Iowa or an adjoining state was computed. These results are presented in Figure 2.
Figure 2.
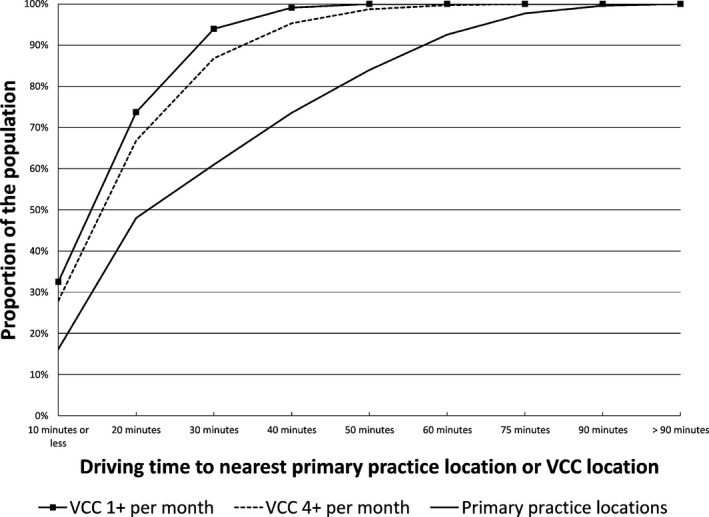
The effect of cardiology visiting consultant clinics on travel times for Iowa residents (2014). VCC indicates visiting consultant clinic.
Sixty‐one percent of Iowa's population resides in census tracts within a 30‐minute drive of a primary practice location of a cardiologist. This is consistent with the 2010 census data, which say that about 64% of Iowa's population lives in urban areas. These data show that 39% of Iowa's population lives further than a 30‐minute drive from the primary practice location of the closest cardiologist.
The population‐level analysis was repeated with the inclusion of the information regarding the locations and frequencies of cardiology VCCs. The first analysis determined the cumulative proportion of the population living within a given driving time of the closer of the nearest cardiologist's primary practice location or VCC location. The second analysis restricted the VCC locations to those sites with a visit frequency of at least 4 per month. The results are also presented in Figure 2.
The percentage of the population living within a 30‐minute drive of any cardiology VCC site is 94%. If we only consider those VCC sites where a cardiologist is present at least 4 or more times per month, the proportion of the population is 87%.
Discussion
The 2009 Lewin Group report recommended research into ways to serve rural areas since they are likely to be more negatively impacted by future shortages in the general cardiology workforce.18 To this end, this study represents an attempt to document the extent of cardiology outreach through visiting consultant clinics in rural communities in Iowa.
Several findings reported here are of particular interest. First, in 2014, cardiologists from Iowa and surrounding states staffed 5052 clinic days in 71 counties without a full‐time cardiologist. These clinic days could be expected to accommodate 70 728 visits by patients in their own community hospital or clinic. To put this level of outreach in perspective, consider that the UVA Center for Telehealth estimates that, between 1994 and 2013, it has facilitated some 30 000 clinical patient encounters across more than 40 medical specialties47 involving patients in rural areas of Virginia. This level of activity makes the UVA “a model for other telehealth centers around the country” and it has been designated as 1 of 14 regional telehealth resource centers by the federal government.48 The yearly number of patient encounters facilitated by cardiology VCCs in Iowa is about 10 times the yearly number of patient encounters (≈7000 in 2015) of the entire UVA telehealth system.48 It should also be noted that Virginia has more 900 000 more citizens living in rural areas than does Iowa.
The second key finding is the effect of VCC outreach on patient travel distances for the entire state of Iowa. Due to cardiology VCCs, an additional 33% of the population lives within a 30‐minute drive of a location where they can meet with a cardiologist on at least a monthly basis. Based on a population of about 3 million people, this translates to more than 1 million rural residents of Iowa improving their access to office‐based care from cardiologists. As noted above, the care delivered by cardiologists in the VCC setting is limited compared to the more expansive set of treatment options available in an urban hospital.
We emphasize the 30‐minute travel standard since it is used to define Health Professional Shortage Areas. In addition, there is limited research suggesting that travel distance may be a barrier for patients to meet with a cardiologist. A small‐scale (N=45) study of rural women with heart failure in New York State finds that 100% of these patients met regularly with their primary care physician.49 The average travel distance to their primary care physician was 6.4 miles. In contrast, only 50% regularly met with a cardiologist with an average distance traveled of 32 miles. We do not know the travel distance to the nearest cardiologist for the 50% of the sample who did not regularly meet with their cardiologist. Since the entire sample was drawn from similar areas of the state, we could assume that the travel distances for all patients were comparable. The 50% difference in regular meeting frequency between one's primary care physician (average distance=6.4 miles) and cardiologist (censored average distance=32 miles) suggests that for some rural patients, a relatively long travel distance can serve as a barrier to seeking care from a cardiologist. This should be of concern given the evidence that heart failure patients receive better care from cardiologists than from primary care physicians alone.14
Third, increased access comes at a cost to the participating cardiologists. As a group, they spend a great deal of time on the road traveling to and from the rural locations. The opportunity costs due to driving time and direct travel expenses are considerable. We have estimated these costs to be more than $2.1 million per year. We have not included additional costs such as rental payments to the hosting institution or any costs for nursing staff that may accompany the visiting cardiologist. We have provided descriptive data on some of the costs of providing distant access from visiting cardiologists. Future research on other costs related to cultural, monetary, and temporal issues for both patient and provider need to be explored.
The impact of the additional travel and patient care coordination issues associated with VCC involvement on physician job satisfaction and turnover are unknown. In addition, consider that 45% of Iowa‐based cardiologists regularly participate in rural outreach. If this model of providing care to rural communities is to be maintained, there may be implications for the training of existing and future cardiologists.
Fourth, the visits by Iowa‐based cardiologists as well as those from adjoining states to outreach sites may be thought of as the importation of specialist physician services into underserved areas. Based upon the 5 hours of clinic time per VCC day,46 visiting cardiologists are providing about 27 300 hours of care in communities outside their primary practice locations per year. Based on a 2080‐hour work year, this translates to an average of 13.13 full‐time equivalent cardiologists.
Some suggest that financial incentives be used to convince cardiologists to practice in rural areas.11 As a thought experiment, consider the effect of convincing 13 members of the existing cardiology workforce to move to an unserved rural county, increasing the number of counties with a full‐time cardiologist from 18 to 31. While this is a substantial improvement, this is well below the 89 counties currently being served through the VCC model. Of course, a resident cardiologist in a heretofore unserved rural county would provide more temporal access than the current VCCs provide. However, it is not certain that there would be enough patients for the rural practice to survive, thus increasing the subsidy costs required to maintain access for a smaller number of rural patients.
This study has a number of limitations. First, our analysis does not include patient‐level data. Therefore, we cannot determine precisely how many patients are seen in the VCC setting or their diagnoses, exact travel distances, or the services they received in the local hospital.
Second, we focused on the involvement of cardiologists in rural outreach in a single state with some unique features. Besides the regulatory issues with telemedicine, there may be other circumstances specific to Iowa such as geography or the medical insurance environment that do not generalize to other states. Furthermore, we did not evaluate the quality of the medical care provided by visiting cardiologists, the utilization of the VCC, or its effect on outcomes. These are additional areas for future research.
In conclusion, this study attempts to fill a significant gap in the literature about cardiology outreach in rural areas. Based upon this study, the visiting consultant clinic does appear to be an effective means to improve access to office‐based cardiologists for rural Iowans. The VCC approach increased access from 18 counties to 89 of the 99 counties in Iowa. The 5052 clinic days staffed in these 71 counties provides the opportunity for more than 50% of the population's office visits to cardiologists to occur in the patient's own county.
Of all cardiologists practicing in Iowa, 45% participated in VCCs in 2014. These outreach clinics resulted in the redistribution of the equivalent of 13.13 full‐time equivalent cardiologists from their urban‐based practices to underserved rural areas. Despite aggregate direct and opportunity costs associated with physician travel of more than $2.1 million per year, this level of rural outreach activity implies a perceived positive cost/benefit for the participating cardiologists.
Disclosures
None.
(J Am Heart Assoc. 2016;5:e002909 doi: 10.1161/JAHA.115.002909)
This article was handled independently by Holli A. DeVon, PhD, RN, as a guest editor. The editors had no role in the evaluation of this manuscript or in the decision about its acceptance.
References
- 1. Xu J, Kochanek KD, Murphy SL, Arias E. Mortality in the United States, 2012. NCHS Data Brief. 2014;168:1–7. [PubMed] [Google Scholar]
- 2. Foot DK, Lewis RP, Pearson TA, Beller GA. Demographics and cardiology, 1950–2050. J Am Coll Cardiol. 2000;35:1067–1081. [DOI] [PubMed] [Google Scholar]
- 3. Ramrakha P, Hill J, eds. Oxford Handbook of Cardiology. Oxford: Oxford University Press; 2012. [Google Scholar]
- 4. Rodgers GP, Conti JB, Feinstein JA, Griffin BP, Kennett JD, Shah S, Walsh MN, Williams ES, Williams JL. ACC 2009 survey results and recommendations: addressing the cardiology workforce crisis: a report of the ACC Board of Trustees Workforce Task Force. J Am Coll Cardiol. 2009;54:1195–1208. [DOI] [PubMed] [Google Scholar]
- 5. Grover A, Gorman K, Dall TM, Jonas R, Lytle B, Shemin R, Wood D, Kron I. Shortage of cardiothoracic surgeons is likely by 2020. Circulation. 2009;120:488–494. [DOI] [PubMed] [Google Scholar]
- 6. Office of Rural Health Policy . 2009 annual report. Health Resources and Services Administration, U.S. Department of Health and Human Services; 2011. [Google Scholar]
- 7. Kirschner A, Berry EH, Glasgow N. The changing faces of rural America In: Kandel WA, Brown DL, eds. Population Change and Rural Society. Netherlands: Springer; 2006:53–74. [Google Scholar]
- 8. Rogers CC. The older population in 21st century rural America. Rural America 2002;17, Economic Research Service, U.S. Department of Agriculture.
- 9. Jones CA, Parker TS, Ahearn M, Mishra AK, Variyam JN. Health Status and Health Care Access of Farm and Rural Populations. Washington, DC: USDA Economic Research Service, Economic Information Bulletin No. (EIB‐57); 2009. [Google Scholar]
- 10. Chen FM, Doescher MP, Hart G. 2005 Physician Supply and Distribution in Rural Areas of the United States. Seattle, WA: WWAMI Rural Health Research Center, University of Washington, School of Medicine, Department of Family Medicine; 2007. [Google Scholar]
- 11. Aneja S, Ross JS, Wang Y, Matsumoto M, Rodgers GP, Bernheim SM, Rathore SS, Krumholz HM. US cardiologist workforce from 1995 to 2007: modest growth, lasting geographic maldistribution especially in rural areas. Health Aff (Millwood). 2011;30:2301–2309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Chan L, Hart LG, Goodman DC. Geographic access to health care for rural Medicare beneficiaries. J Rural Health. 2006;22:140–146. [DOI] [PubMed] [Google Scholar]
- 13. Schreiber TL, Elkhatib A, Grines CL, O'Neill WW. Cardiologist versus internist management of patients with unstable angina: treatment patterns and outcomes. J Am Coll Cardiol. 1995;26:577–582. [DOI] [PubMed] [Google Scholar]
- 14. Ezekowitz JA, van Walraven C, McAlister FA, Armstrong PW, Kaul P. Impact of specialist follow‐up in outpatients with congestive heart failure. CMAJ. 2005;172:189–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Lee DS, Stukel TA, Austin PC, Alter DA, Schull MJ, You JJ, Chong A, Henry D, Tu JV. Improved outcomes with early collaborative care of ambulatory heart failure patients discharged from the emergency department. Circulation. 2010;122:1806–1814. [DOI] [PubMed] [Google Scholar]
- 16. Czarnecki A, Wang JT, Tu JV, Lee DS, Schull MJ, Lau C, Farkouh ME, Wijeysundera HC, Ko DT. The role of primary care physician and cardiologist follow‐up for low‐risk patients with chest pain after emergency department assessment. Am Heart J. 2014;168:289–295. [DOI] [PubMed] [Google Scholar]
- 17. Czarnecki A, Chong A, Lee DS, Schull MJ, Tu JV, Lau C, Farkouh ME, Ko DT. Association between physician follow‐up and outcomes of care after chest pain assessment in high‐risk patients. Circulation. 2013;127:1386–1394. [DOI] [PubMed] [Google Scholar]
- 18. Lewin Group . Cardiovascular workforce assessment. 2009. Available at: http://content.onlinejacc.org/data/Journals/JAC/23181/1.pdf. Accessed February 21, 2014.
- 19. Arora S, Kalishman S, Dion D, Som D, Thornton K, Bankhurst A, Boyle J, Harkins M, Moseley K, Murata G, Komaramy M, Katzman J, Colleran K, Deming P, Yutzy S. Partnering urban academic medical centers and rural primary care clinicians to provide complex chronic disease care. Health Aff (Millwood). 2011;30:1176–1184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. American Hospital Association . The promise of telehealth for hospitals, health systems and their communities. Available at: http://www.aha.org/research/reports/tw/15jan-tw-telehealth.pdf. Accessed March 10, 2016.
- 21. Thomas L, Capistrandt G. State telemedicine gaps analysis: coverage and reimbursement. American Telemedicine Association; May 2015. [Google Scholar]
- 22. Ward MM, Ullrich F, Mueller K. Extent of telehealth use in rural and urban hospitals, rural health research & policy centers, RUPRI center for rural health policy analysis, University of Iowa College of Public Health. Rural Policy Brief. 2014;4:1–4. [PubMed] [Google Scholar]
- 23. Call VR, Erickson LD, Dailey NK, Hicken BL, Rupper R, Yorgason JB, Bair B. Attitudes toward telemedicine in urban, rural, and highly rural communities. Telemed J E Health. 2015;21:644–651. [DOI] [PubMed] [Google Scholar]
- 24. Wakefield DS, Tracy R, Einhellig J. Trends and implications of visiting medical consultant outpatient clinics in rural hospital communities. Hosp Health Serv Adm. 1997;42:49–66. [PubMed] [Google Scholar]
- 25. Drew J, Cashman SB, Savageau JA, Stenger J. The visiting specialist model of rural health care delivery: a survey in Massachusetts. J Rural Health. 2006;22:294–299. [DOI] [PubMed] [Google Scholar]
- 26. Gruen RL, Weeramanthri TS, Knight SS, Bailie RS. Specialist outreach clinics in primary care and rural hospital settings. Cochrane Database Syst Rev. 2004;1:CD003798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Tracy R, Saltzman KL, Wakefield DS. Considerations in establishing a visiting consultant clinic in a rural hospital community. Hosp Health Serv Adm. 1996;41:255–265. [PubMed] [Google Scholar]
- 28. American Association of Medical Colleges, Center for Workforce Studies . 2014 Physician Specialty Data Book. Available at: https://members.aamc.org/eweb/upload/Physician%20Specialty%20Databook%202014.pdf. Accessed September 21, 2015. [Google Scholar]
- 29. Center for Connected Health Policy . State telehealth policies and reimbursement schedules: a comprehensive plan of the 50 states and District of Columbia. September 2014.
- 30. Iowa Board of Medicine . New rule sets standards of practice for physicians who use telemedicine. Press release dated June 3, 2015.
- 31. Black M, Leese B, Gosden T, Mead N. Specialist outreach clinics in general practice: what do they offer? Br J Gen Pract. 1997;47:558–561. [PMC free article] [PubMed] [Google Scholar]
- 32. Bond M, Bowling A, Abery A, McClay M, Dickinson E. Evaluation of outreach clinics held by specialists in general practice in England. J Epidemiol Community Health. 2000;54:149–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Horn BP, Barragan GN, Fore C, Bonham CA. A cost comparison of travel models and behavioural telemedicine for rural, Native American populations in New Mexico. J Telemed Telecare. 2016;22:47–55. [DOI] [PubMed] [Google Scholar]
- 34. Loh PK, Sabesan S, Allen D, Caldwell P, Mozer R, Komesaroff PA, Talman P, Williams M, Shaheen N, Grabinski O, Withnall D; The Royal Australasian College of Physicians Telehealth Working Group . Practical aspects of telehealth: financial considerations. Intern Med J. 2013;43:829–834. [DOI] [PubMed] [Google Scholar]
- 35. Kane L, Peckham C. Medscape physician compensation report 2014. Available at: http://www.medscape.com/features/slideshow/compensation/2014/public/overview#2. Accessed September 23, 2015.
- 36. Roodenbeke E, Lucas S, Rouzaut A, Bana F. Outreach Services as a Strategy to Increase Access to Health Workers in Remote and Rural Areas: Increasing Access to Health Workers in Rural and Remote Areas. Geneva: World Health Organization; 2011. (Technical Report, No. 2.). Available at: http://www.ncbi.nlm.nih.gov/books/NBK310729/. Accessed May 9, 2016. [PubMed] [Google Scholar]
- 37. Desch CE, Grasso MA, McCue MJ, Buonaiuto D, Grasso K, Johantgen MK, Shaw JE, Smith TJ. A rural cancer outreach program lowers patient care costs and benefits both the rural hospitals and sponsoring academic medical center. J Rural Health. 1999;15:157–167. [DOI] [PubMed] [Google Scholar]
- 38. Onega T, Duell EJ, Shi X, Wang D, Demidenko E, Goodman D. Geographic access to cancer care in the U.S. Cancer. 2008;112:909–918. [DOI] [PubMed] [Google Scholar]
- 39. Morrill R, Cromartie J, Hart G. Metropolitan, urban, and rural commuting areas: toward a better depiction of the United States settlement system. Urban Geogr. 1999;20:727–748. [Google Scholar]
- 40. Lu H, Holt JB, Cheng YJ, Zhang X, Onufrak S, Croft JB. Population‐based geographic access to endocrinologists in the United States, 2012. BMC Health Serv Res. 2015;15:541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Muffly TM, Weterings R, Barber MD, Steinberg AC. Discrepancies in the female pelvic medicine and reconstructive surgeon workforce. Female Pelvic Med Reconstr Surg. 2015;2:99–105. [DOI] [PubMed] [Google Scholar]
- 42. Hsia RY, Shen Y‐C. Changes in geographical access to trauma centers for vulnerable populations in the United States. Health Aff (Millwood). 2011;30:1912–1920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Mayer ML, Beil HA, von Allmen D. Distance to care and relative supply among pediatric surgical subspecialties. J Pediatr Surg. 2009;44:483–495. [DOI] [PubMed] [Google Scholar]
- 44. National ambulatory medical care survey: 2010 summary tables. Available at: http://www.cdc.gov/nchs/data/ahcd/namcs_summary/2010_namcs_web_tables.pdf. Accessed March 3, 2016.
- 45. Wakefield DS, Tracy R. Adjusting measures of physician availability to reflect importation of physician services into rural areas. J Rural Health. 1996;12:39–44. [DOI] [PubMed] [Google Scholar]
- 46. NAMCS 2010 fact sheet: Cardiovascular Diseases. Available at: http://www.cdc.gov/nchs/data/ahcd/NAMCS_2010_factsheet_cardiovascular_diseases.pdf. Accessed March 3, 2016.
- 47. Wicklund E. UVA Center for telehealth provides model for telehealth industry. HealthcareITNews.com May 1, 2013. Available at: http://www.healthcareitnews.com/news/uva-center-telehealth-provides-model-telehealth-industry. Accessed May 20, 2016.
- 48. Rheuban KS. Virginia healthcare leadership retreat. Presentation dated August 21, 2015. Available at: https://academicoutreach.virginia.edu/sites/academicoutreach.virginia.edu/files/Rheuban-NGA-August-21-2015-presentation.pdf. Accessed May 19, 2016.
- 49. Pierce C. Distance and access to health care for rural women with heart failure. Online J Rural Nurs Health Care. 2007;7:27–34. [Google Scholar]


