Abstract
Purpose:
Recent studies have demonstrated increasing rates of financial toxicities and emotional distress related to cancer treatment. This study assessed and characterized the relationships among financial distress, emotional symptoms, and overall distress in patients with cancer.
Methods:
A cross-sectional sample of patients with cancer who visited our outpatient medical oncology and psychiatry clinics completed a pen-and-paper survey. The survey assessed demographics; cost concerns; and financial, emotional, and overall distress.
Results:
One hundred twenty insured patients completed the survey. Sixty-five percent reported clinically significant overall distress scores, with the same percentage reporting at least one emotional problem (worry, anxiety, depression, etc). Twenty-nine percent scored in the range of high to overwhelming financial distress. By using structural equation modeling, we found that financial distress was associated with overall distress. This association was both direct (accounting for 76% of the effect) and indirect (accounting for 24% of the effect) via mediation by emotional distress.
Conclusion:
This cohort of patients with cancer reported significant levels of emotional distress, financial distress, and overall distress. These factors were interrelated, with both financial and emotional distress contributing to overall distress. Interventions targeted at alleviating financial distress may help to decrease levels of overall distress.
INTRODUCTION
All patients with cancer experience some level of distress. The National Comprehensive Cancer Network (NCCN) has defined distress in clinical practice as a “multifactorial unpleasant emotional experience of a psychological (ie, cognitive, behavioral, emotional), social, and/or spiritual nature that may interfere with the ability to cope effectively with cancer, its physical symptoms, and its treatment.”1(pDIS-2) Distress is now considered the sixth vital sign,2 and the American College of Surgeons Commission on Cancer now mandates that its accredited hospitals implement distress screening and refer patients for psychosocial health care services when needed. If a patient’s distress is left unaddressed, it can lead to impaired decision making and poor care self-management.3-5
The rising costs of cancer treatment are increasingly shifted to the patient, which can contribute to financial distress.6,7 One study found that patients with cancer who experienced unexpected medical costs had increased anxiety and depression and worse quality-of-life (QOL) outcomes over time.8 The financial burden that patients face in the form of rising out-of-pocket costs can negatively affect QOL and can affect the quality of care received.6 Furthermore, these rising costs may affect patients who already struggle to meet their normal monthly living expenses. These patients who may already be faced with a heat-or-eat dilemma are now faced with the more-troubling decision of heat, eat, or treat. Financial burden, financial concern, and financial distress often are used interchangeably in oncologic practice and the scientific literature, each of which can contribute to the more clinically meaningful term financial toxicity, which was first introduced by Ratain9 in 2009. Zafar and Abernethy6 further recommended that the financial toxicities of cancer be viewed and considered similarly to the physical toxicities that are strategically monitored and addressed.
Like financial distress, emotional distress may be a component of overall distress. Psychiatric disorders, including anxiety and depression, are common among patients with cancer, with rates varying from 16% reported in unresectable non–small-cell lung carcinoma10 and newly diagnosed head and neck cancer,11 24% in Hodgkin lymphoma,12 as high as 42% in breast cancer after the first recurrence,13 and 47% in new admissions to a cancer center.14 A meta-analysis reported the prevalence of depression in oncologic outpatients to be 16.2%,15 and depression is known to cause distress, diminish the patient’s ability or willingness to participate in their care, affect QOL measures, and affect survival.16
In oncologic research, a great chasm exists in quantifying financial burden and in understanding how financial distress affects QOL.7,17-21 A study of 149 patients with advanced cancer found that 37% reported more financial distress than emotional distress, and 30% reported their financial distress as more severe than other types of distress.21 In a national sample of cancer survivors, financial burden had a significant impact on levels of depressed mood, psychologic distress, and worry.22 Patients who reported cancer-related financial stress had a three to four times increase in the risk of adverse psychologic outcomes (ie, anxiety, depression).23 To further advance this work, we sought to characterize the relationship among these various forms of distress in patients with cancer. By using assessments of financial distress, overall distress, and emotional distress, we tested the hypothesis that these constructs are interrelated. We also sought to understand some of the financial concerns and assistance needs patients expressed.
METHODS
This study was conducted at Fox Chase Cancer Center, a National Cancer Institute–designated comprehensive cancer center. A convenience sample of patients with cancer older than 18 years was recruited from medical oncology and psychiatry clinics. All eligible patients were taking, had taken, or were consulting with their physician to begin taking anticancer medications. Recruitment of patients occurred in two phases that spanned September 2013 to April 2014. A clinical care provider (eg, physician, nurse) consulted with eligible patients about the study during their visit and gave the research assistant permission to approach specific patients either before or after their appointment.
We received a waiver of documentation of informed consent. Patients could refuse to answer any question. As such, patients were not prompted to complete missing questions or sections. Because we did not collect participants’ names or medical record numbers, we did not abstract missing demographic data from medical charts.
The study involved one questionnaire that patients completed in clinic. The questionnaire included demographics along with the validated measurements outlined next. The survey was amended before the second phase to add questions, so the first and second phase questionnaires and specific question sample sizes differed slightly.
Patient Characteristics
In addition to the usual sociodemographic data, patients reported their health insurance status, original cancer site, disease and treatment history, and sources of financial support.
Overall Distress
We measured overall distress by using the NCCN Distress Thermometer (DT) and Problem List.1 This instrument asks patients to rate their overall distress from 0 to 10 (highest level of distress) in the past week. Self-reported distress scores of ≥ 4 are considered clinically meaningful.25 Participants were also asked to specify whether the source of their distress was related to specific issues on the Problem List as follows: practical problems (six items [eg, insurance/financial]), family problems (four items [eg, dealing with children]), emotional problems (six items [depression, fears, nervousness, sadness, worry, loss of interest in usual activity]), spiritual/religious concerns, and physical problems (21 items [eg, appearance, pain]).
Emotional Distress
We considered patients to have emotional distress if they answered yes to experiencing any of the six emotions in the Problem List. The number of responses was summed. The emotional domain of the Problem List is correlated strongly with the single DT measure, and positive responses on the Problem List help to qualify a clinically significant distress score on the DT.26
Financial Distress
Financial distress was measured by using the InCharge Financial Distress/Financial Well-Being Scale (InCharge) because no other financial distress measure had been validated in patients with cancer at the time of recruitment. InCharge measures a latent construct that represents responses to one’s financial state on a continuum of overwhelming financial distress to highest level of financial well-being.27 Scores < 5.0 represent financial distress.
Financial Concerns
Patients were also asked to indicate whether they felt the need to continue working during treatment to meet their financial needs as well as about concerns with various normal expenses. A subset of 34 patients recruited in the second phase responded to the prompt, “Please identify any areas that you may need assistance with.” Response options included “understanding my insurance policy and coverage,” “knowing whom to ask for help,” and “identifying sources of financial assistance.”
Statistical Analyses
To investigate mediational pathways in the association among financial distress, emotional distress, and overall distress, we used a structural equation approach.28 We used bootstrap standard errors for the assessment of the mediated effect.29 A mediating variable explains the association between an independent and a dependent variable. Mediation models have been used in the health psychology literature to explain health behaviors and to develop interventions to improve them. For example, findings from a study of women with diabetes mellitus found that healthy lifestyle changes in diet and physical activity were mediated by social support through neighbors and family, suggesting that improving social support might improve clinical outcomes.30 We controlled for sex, education, age, marital status, children, employment status, income, and race in the models. Numerical variables were sums along with the sample median and range. Categorical variables were summarized as frequencies and percentages.
RESULTS
Participant Characteristics
One hundred twenty patients completed the survey, with 60 patients in each phase. Fifty-eight percent were younger than 65 years of age, and 66% were married or had a domestic partner. Fifty-two percent were female, and 84% were white. All patients had health insurance, and 56% reported household incomes of ≥ $50,000. The remainder of patient characteristics are shown in Table 1.
Table 1.
Patient Characteristics
| Characteristic | No. (%) |
|---|---|
| No. of patients | 120 |
| Median (range) age, years | 62 (22-87) |
| < 40 | 7 (6) |
| 40-50 | 18 (15) |
| 51-60 | 26 (21) |
| 61-70 | 43 (36) |
| > 70 | 25 (21) |
| Missing | 1 (1) |
| Sex | |
| Female | 62 (52) |
| Male | 58 (48) |
| Ethnicity | |
| White (non-Hispanic) | 101 (84) |
| Black | 13 (11) |
| Asian | 3 (3) |
| Hispanic | 1 (1) |
| Other | 2 (1) |
| Marital status | |
| Married/domestic partnership | 79 (66) |
| Never married | 18 (15) |
| Divorced/separated | 17 (14) |
| Widowed | 6 (5) |
| Have children | 93 (78) |
| Homeowners | 92 (77) |
| Education | |
| High school diploma | 39 (33) |
| Some college/trade school | 33 (27) |
| Bachelor’s degree | 25 (21) |
| Advanced degree | 13 (11) |
| Less than high school | 9 (7) |
| Missing | 1 (1) |
| Employment | |
| Retired | 49 (41) |
| Used for wages | 31 (26) |
| Unable to work | 23 (19) |
| Out of work | 6 (5) |
| Other | 7 (6) |
| Missing | 4 (3) |
| Has health insurance | 120 (100) |
| Income (annual) | |
| > $100,000 | 27 (23) |
| $75,000-$100,000 | 16 (13) |
| $50,000-$74,999 | 24 (20) |
| $25,000-$49,999 | 24 (20) |
| < $25,000 | 19 (16) |
| Missing | 10 (8) |
| Sources of income | |
| Spouse or self-support | 109 (91) |
| Parents | 5 (4) |
| Friends | 5 (4) |
| Children | 1 (1) |
| Cancer site | |
| Genitourinary | 46 (38) |
| Gastrointestinal | 29 (24) |
| Gynecologic | 16 (13) |
| Sarcoma | 9 (8) |
| Other | 20 (17) |
| Treatment history | |
| Surgery | 82 (68) |
| Chemotherapy | 80 (67) |
| Radiation | 47 (39) |
| Targeted therapy | 19 (16) |
| Hormone | 18 (15) |
| Time since diagnosis (n = 60*), years | |
| < 1 | 22 (37) |
| 1-3 | 13 (22) |
| 3-5 | 10 (17) |
| > 5 | 15 (25) |
| Metastatic disease present (n = 60*) | 38 (63) |
Added to the demographics section for the second phase of the study.
Overall Distress
One hundred nine patients completed the DT portion of the questionnaire. Sixty-five percent reported clinically significant distress scores (≥ 4), with 28% identifying that their distress level was in the highest range (8 to 10).
Emotional Distress
One hundred eighteen patients responded to the Problem List portion of the DT. Sixty-six percent indicated that they had a problem with at least one emotional symptom. Worry was the most common problem identified in almost one half of the participants (49%), followed by nervousness (38%), fears (37%), sadness (30%), depression (29%), and loss of interest in usual activities (26%).
Financial Distress
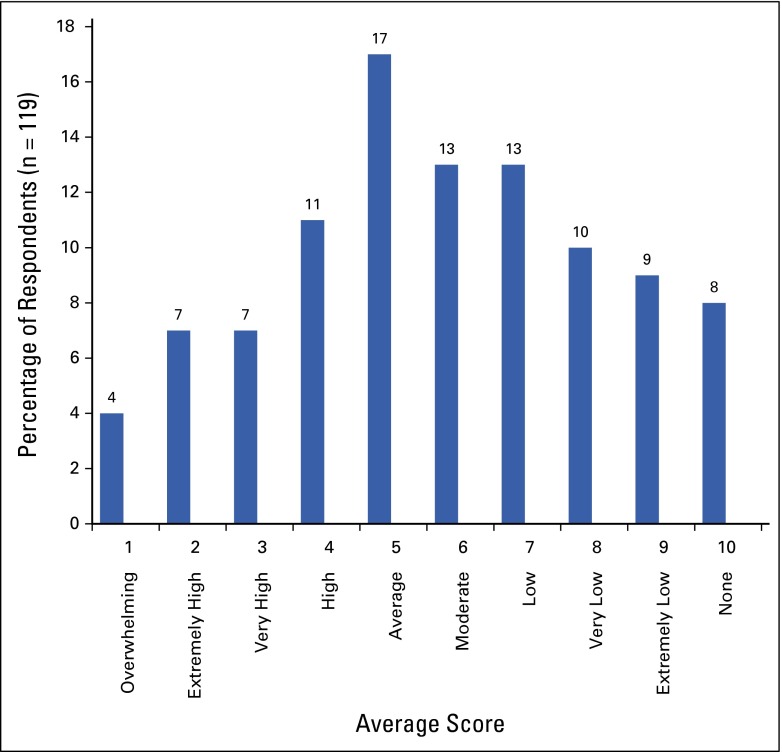
All 120 patients responded to InCharge. Figure 1 shows the distribution of financial distress scores by deciles. Lower scores indicate greater financial distress. Twenty-nine percent had an overall score in the range of high to overwhelming financial distress.
FIG 1.
InCharge Financial Distress/Financial Well-being average scores. Scores represent the full decile (ie, 1 = all possible scores from 1.0 to 1.99), with the exception of 10, which represents an average score of exactly 10.0. Normative descriptive terminology for interpreting InCharge scores includes modifiers related to both financial distress and financial well-being (ie, overwhelming financial distress/lowest financial well-being); terminology has been truncated to include only financial distress modifiers.
Financial Concerns
We collected additional data on subjective concerns (Appendix Table A1, online only). Concerns included need to continue to work to pay for treatment (40%), paying for treatment (43%), and paying other bills (41%). The most frequently reported assistance needs were knowing whom to ask for help (29%), identifying sources of financial assistance (26%), understanding the insurance policy (24%), and accessing community resources that may help (21%).
Relationships Among Financial Distress, Emotional Symptoms, and Overall Distress
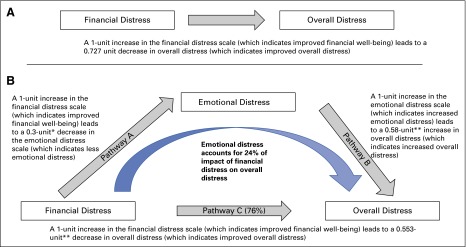
We found that financial distress was associated with overall distress and that emotional distress also mediated this association (Figs 2A and 2B). In this model, higher scores on the financial distress scale represented improved financial well-being. However, lower scores on the emotional distress and overall distress scales indicated better outcomes. By controlling for demographic variables, the total effect of financial distress on overall distress was −0.727 (Fig 2A). That is, for each 1-unit increase in the financial distress scale (which demonstrated improved financial well-being), the overall DT fell by 0.727 points, which suggests that improved financial well-being is associated with lower overall distress.
FIG 2.
(A) Association between financial distress and overall distress. (B) Emotional distress mediates the association between financial distress and overall distress (P = .005). Financial distress was measured using the InCharge Financial Distress/Financial Well-being scale, where scores range from 1.0 to 10.0 and a lower score indicates greater financial distress. Overall distress was measured using the National Comprehensive Cancer Center Distress Thermometer, which is a screening tool for distress with scores that range from 0 (no distress) to 10 (most distress). Emotional distress was measured by summing the number of emotional problems indicated by each participant on the Problem List portion of the Distress Thermometer. *P = .008; **P < .001.
The total effect can be divided into two routes: pathways A and B (emotional distress mediates the association between financial distress and overall distress) and pathway C (financial distress directly increases overall distress). A 1-unit increase in the financial distress scale (which indicates improved financial well-being) reduced emotional distress by 0.3 (P = .008, pathway A), and a 1-unit increase in emotional distress increased the overall DT by 0.58 units (P < .001, pathway B). After accounting for emotional distress, the direct effect of financial distress on overall distress decreased to −0.553 (compared with −0.727 when not accounting for emotional distress; P < .001, pathway C). This means that for each 1-point increase in financial distress, −0.727 − (−0.553) = −0.174 of its effect on the DT is through the mediated pathway (pathways A and B), which suggests that the mediational pathway of emotional distress accounts for 24% of the impact [(0.174 / 0.727) × 100] of financial distress on the overall distress score. This mediational pathway is statistically significant (P = .005 for the attenuation of the financial distress coefficient when emotional distress is added to the model).
DISCUSSION
In this study of relatively affluent, insured, and well-educated patients seen at a National Cancer Institute–designated comprehensive cancer center, 29% reported high levels of financial distress. Two thirds (65%) reported clinically significant levels of overall distress measured with the NCCN DT, with a similar percentage (66%) also reporting at least one symptom of emotional distress. We also found a strong association between financial distress and overall distress (Fig 2). This association was both direct and mediated through emotional distress, which suggests that financial distress can cause overall distress directly and be associated with emotional distress, which in turn can affect overall distress.
The practical implications of the results of this pilot study are to encourage health care institutions to recognize and manage distress. In the subset of patients who answered questions about informational needs, 29% identified knowing whom to ask for help as a need, whereas 24% stated that they needed assistance with understanding their insurance policy and coverage. Interventions aimed at helping to reduce overall distress in patients with cancer should include efforts focused on ameliorating financial distress in patients who identify this as a concern. Efforts to help patients to understand and manage their insurance coverage and financial obligations and to develop financial literacy skills would be useful. In addition, financial counselors should be cross-trained to recognize emotional distress because emotional distress can exacerbate financial distress. Rigorous programs to recognize and manage emotional distress, such as anxiety and depression, may help to reduce the impact of financial distress on overall distress, and future research could include baseline and follow-up measures of financial distress to help to measure potential resultant effects.21
The current findings are important given the increased focus on shared decision making and patient-centered care.31 ASCO developed a conceptual framework to present benefits, toxicities, overall costs, and out-of-pocket costs to help patients to make treatment decisions.32 However, physicians may not be comfortable with these cost conversations.33 The balance of the survival benefits from treatment with out-of-pocket costs is a challenge. It has been argued that the conversation should focus on value versus outright cost and must include the financial toxicities of treatment.34 Unfortunately, the Affordable Care Act may not bring the financial relief that many hoped for. It has been projected that given the high cost of most oral anticancer medications, even with the closing of the Medicare donut hole by the year 2020, as part of the Affordable Care Act, patients still will face very-high out-of-pocket costs.35 Therefore, issues about the cost and value of cancer care and financial distress in patients will remain important issues because distressed patients may have a diminished ability to self-manage their care.36
The current findings should be interpreted within the context of the limitations of a pilot study. This was a cross-sectional study at a tertiary referral center, and patients were only approached after approval from their clinician. This was a convenience sample. We recruited some patients from our psychiatry clinics, which may have led to an overestimation of distress in the group. However, we did not approach patients who were viewed by their clinician to be too distressed to complete the survey. Therefore, true population rates of financial, emotional, and overall distress may be higher than reported in this study. In addition, the group was relatively affluent, educated, and predominantly white. The results may be different if the study was conducted within a community practice or capitated health system. Future work should address these issues in a minority or underserved population. Because patients could consult with their family while completing the survey, it is possible that family member input may have introduced bias to the patients’ responses. In addition, we did not collect data on patients’ out-of-pocket expenses or on insurance structure, such as the extent of copayments and deductibles. However, unlike these objective variables, patients’ self-report of financial concerns, emotional concerns, and overall distress is highly subjective and likely varies as they progress through their disease and treatment trajectory. Patients possibly have different needs and concerns in the curative and palliative settings. In addition, the financial distress/well-being cutoffs analyzed from InCharge have not been prospectively validated, and future studies may use newer measures, such as the validated COST (comprehensive score for financial toxicity) measure.37 We did not track decliners; therefore, an overall response rate was not calculated.
The self-report of emotional symptoms (worry, depression, etc) was completed on the NCCN DT, which is a screening tool, and may not reflect the true prevalence of these symptoms in this population. The NCCN-endorsed single-item DT is a widely accepted and routinely used tool for distress screening, especially among NCCN member institutions.38 Although the DT has been successfully validated against the Hospital Anxiety and Depression Scale in a variety of cancer-related patient and caregiver populations,39 research has shown that the single-item measure is not as successful at identifying all cases of psychologic distress compared with more-robust tools (eg, Brief Symptom Inventory-18), although it is an efficient method for ruling out symptoms of depression and anxiety.36,40 Therefore, the true level of overall distress in this population of 120 insured patients with cancer may be even higher than the 65% rate determined by this research. Finally, we measured emotional distress by summing the responses on the Problem List. Formal measures of anxiety and depression may produce different results.
Despite these limitations, the current results provide important insight into patients’ financial concerns that should be explored in future work. As providers screen for distress, they need to recognize that financial distress may be an important source of overall distress. Our previous work demonstrated that financial concerns are present among all sociodemographic groups and that higher income or education was not protective against financial concerns.41,42 The importance of addressing patients’ financial concerns is underscored by the Institute of Medicine, which defined health literate organizations as those that assist patients in navigating, understanding, and using health care services. Such an organization communicates clearly what health plans cover and what individuals will have to pay for services.31 However, the addressing of these concerns can be a challenge. A study of cancer center social workers and financial counselors cited a lack of financial resources, process inefficiencies, limited resources to identify at-risk individuals, and inadequate insurance coverage as barriers to addressing financial distress in patients with cancer.43 Hospital initiatives to provide clearer information about out-of-pocket costs, reduce medical billing errors, and improve transparency may be helpful in reducing distress.
In summary, even among insured patients treated at a comprehensive cancer center, financial distress may be an important component of overall distress. Educational interventions to address financial concerns alongside emotional symptoms may reduce overall distress.
Supplementary Material
Acknowledgment
Presented at the 2014 ASCO Annual Meeting, Chicago, IL, May 30-June 3, 2014. Supported by Core Grant No. P30CA06927.
Appendix
Table A1.
Assistance Needs and Financial Concerns
| No. (%) | |
|---|---|
| Assistance needs (n = 34) | |
| Knowing whom to ask for help | 10 (29) |
| Identifying sources of financial assistance | 9 (26) |
| Understanding my insurance policy and coverage | 8 (24) |
| Accessing community resources that may help me with my cancer | 7 (21) |
| Knowing what my copayment will be | 6 (18) |
| Understanding paperwork, bills, and statements that I receive from my insurance company and my health care providers | 6 (18) |
| Understanding my diagnosis, treatment options, follow-up instructions, and/or survivorship plan | 4 (12) |
| Filling out medical forms | 1 (3) |
| Communicating with my health care team | 0 (0) |
| Need to keep working to pay for my treatment (N = 120*) | |
| No | 69 (58) |
| Yes | 21 (18) |
| Yes, and I am still working | 15 (13) |
| Yes, but I am unable to work | 10 (8) |
| Missing | 5 (4) |
| Concerns about expenses (N = 120) | |
| I have no concerns about my expenses | 53 (44) |
| Paying other bills | 30 (25) |
| Clothing | 30 (25) |
| Medical expenses | 28 (23) |
| Rent/mortgage | 24 (20) |
| Child care | 22 (18) |
| Holidays | 20 (17) |
| Recreational activities | 18 (15) |
| Buying food | 12 (10) |
| Student loan debt | 12 (10) |
The response options were expanded from no/yes in the first phase to no/yes, and I am still working/yes, but I am unable to work in the second phase of the questionnaire based on participant feedback.
AUTHOR CONTRIBUTIONS
Conception and design: Brian L. Egleston, Michael J. Hall, Karen Y. Mechanic, Yu-Ning Wong
Provision of study materials or patients: Michael J. Hall, Marijo Bilusic, Elizabeth R. Plimack, Lainie P. Martin, Karen Y. Mechanic, Margaret von Mehren
Collection and assembly of data: Caitlin R. Meeker, Daniel M. Geynisman, Bianca Lewis, Yu-Ning Wong
Data analysis and interpretation: Caitlin R. Meeker, Daniel M. Geynisman, Brian L. Egleston, Marijo Bilusic, Elizabeth R. Plimack, Lainie P. Martin, Margaret von Mehren, Yu-Ning Wong
Manuscript writing: All authors
Final approval of manuscript: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Relationships Among Financial Distress, Emotional Distress, and Overall Distress in Insured Patients With Cancer
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or jop.ascopubs.org/site/misc/ifc.xhtml.
Caitlin R. Meeker
No relationship to disclose
Daniel M. Geynisman
Consulting or Advisory Role: Pfizer, Novartis, Prometheus Labs
Research Funding: Pfizer
Brian L. Egleston
Research Funding: Verilogue (Inst)
Michael J. Hall
Research Funding: Myriad Genetics (Inst)
Patents, Royalties, Other Intellectual Property: Patent with several Fox Chase investigators for a novel method to investigate hereditary colorectal cancer genes (Inst)
Travel, Accommodations, Expenses: PAREXEL International
Other Relationship: Myriad Genetics, Foundation Medicine, Invitae
Karen Y. Mechanic
No relationship to disclose
Marijo Bilusic
Consulting or Advisory Role: Dendreon, Genomic Health, Astellas Pharma, Bayer AG
Speakers’ Bureau: Dendreon
Research Funding: Ambry Genetics (Inst), Bavarian Nordic (Inst), Johnson & Johnson (Inst), Sotio (Inst), Advaxis (Inst)
Elizabeth R. Plimack
Consulting or Advisory Role: Acceleron Pharma, Bristol-Myers Squibb, Genentech, Eli Lilly, Novartis, Pfizer, Synergene, Merck, Dendreon
Research Funding: Acceleron Pharma (Inst), AstraZeneca (Inst), Bristol-Myers Squibb (Inst), Dendreon (Inst), GlaxoSmithKline (Inst), Eli Lilly (Inst), Merck (Inst), Peloton (Inst), Pfizer (Inst)
Patents, Royalties, Other Intellectual Property: US Patent No. 14/588,503 filed January 2, 2015 (Inst)
Lainie P. Martin
Consulting or Advisory Role: ImmunoGen
Research Funding: AbbVie (Inst), Clovis Oncology (Inst), Merck (Inst), Millennium Pharmaceuticals (Inst), Regeneron Pharmaceuticals (Inst), Sanofi (Inst), TetraLogic Pharmaceuticals (Inst), TEVA Pharmaceuticals Industries (Inst), Novartis (Inst)
Margaret von Mehren
Consulting or Advisory Role: Eisai, CytRx, Blueprint Medicines, Janssen Pharmaceuticals (a Johnson & Johnson co.)
Research Funding: ArQule
Travel, Accommodations, Expenses: Janssen Pharmaceuticals (a Johnson & Johnson co.), Blueprint Medicines, ARIAD Pharmaceuticals, Eisai, Novartis
Bianca Lewis
No relationship to disclose
Yu-Ning Wong
Research Funding: Pfizer (Inst), Bayer AG (Inst), Tokai Pharmaceuticals (Inst), PhRMA Foundation
Travel, Accommodations, Expenses: Tokai Pharmaceuticals
References
- 1. Holland JC, Anderson B, Breitbart WS, et al: NCCN Clinical Practice Guidelines in Oncology: Distress Management. Version 2.2012. Ft Washington, PA, National Comprehensive Cancer Network, 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lazenby M. The international endorsement of US distress screening and psychosocial guidelines in oncology: A model for dissemination. J Natl Compr Canc Netw. 2014;12:221–227. doi: 10.6004/jnccn.2014.0023. [DOI] [PubMed] [Google Scholar]
- 3.Holland JC, Bultz BD. The NCCN guideline for distress management: A case for making distress the sixth vital sign. J Natl Compr Canc Netw. 2007;5:3–7. [PubMed] [Google Scholar]
- 4. Adler NE, Page AEK (eds): Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs. Washington, DC, National Academy of Sciences, 2008. [PubMed] [Google Scholar]
- 5. doi: 10.1200/JCO.2015.63.2463. Wong YN, Schluchter MD, Albrecht TL, et al: Financial Concerns about participation in clinical trials among patients with cancer. J Clin Oncol 34:479-487, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zafar SY, Abernethy AP. Financial toxicity, part I: A new name for a growing problem. Oncology (Williston Park) 2013;27:80–81, 149. [PMC free article] [PubMed] [Google Scholar]
- 7. Zafar SY, Peppercorn JM, Schrag D, et al: The financial toxicity of cancer treatment: A pilot study assessing out-of-pocket expenses and the insured cancer patient’s experience. Oncologist 18:381-390, 2013. [DOI] [PMC free article] [PubMed]
- 8. Hlubocky FJ, Cella D, Sher TG, et al: Financial burdens (FB), quality of life, and psychological distress among advanced cancer patients (ACP) in phase I trials and their spousal caregivers (SC). J Clin Oncol 30, 2012 (suppl; abstr 6117)
- 9. Ratain MJ: Biomarkers and clinical care. Presented at the AAAS/FDLI Colloquium, Personalized Medicine in an Era of Health Care Reform, Washington, DC, October 27, 2009. [Google Scholar]
- 10.Akechi T, Okamura H, Nishiwaki Y, et al. Psychiatric disorders and associated and predictive factors in patients with unresectable nonsmall cell lung carcinoma: A longitudinal study. Cancer. 2001;92:2609–2622. doi: 10.1002/1097-0142(20011115)92:10<2609::aid-cncr1614>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 11.Kugaya A, Akechi T, Okuyama T, et al. Prevalence, predictive factors, and screening for psychologic distress in patients with newly diagnosed head and neck cancer. Cancer. 2000;88:2817–2823. doi: 10.1002/1097-0142(20000615)88:12<2817::aid-cncr22>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- 12.Oerlemans S, Mols F, Nijziel MR, et al. The course of anxiety and depression for patients with Hodgkin’s lymphoma or diffuse large B cell lymphoma: A longitudinal study of the PROFILES registry. J Cancer Surviv. 2014;8:555–564. doi: 10.1007/s11764-014-0367-1. [DOI] [PubMed] [Google Scholar]
- 13.Okamura H, Watanabe T, Narabayashi M, et al. Psychological distress following first recurrence of disease in patients with breast cancer: Prevalence and risk factors. Breast Cancer Res Treat. 2000;61:131–137. doi: 10.1023/a:1006491417791. [DOI] [PubMed] [Google Scholar]
- 14.Derogatis LR, Morrow GR, Fetting J, et al. The prevalence of psychiatric disorders among cancer patients. JAMA. 1983;249:751–757. doi: 10.1001/jama.249.6.751. [DOI] [PubMed] [Google Scholar]
- 15.Mitchell AJ, Chan M, Bhatti H, et al. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: A meta-analysis of 94 interview-based studies. Lancet Oncol. 2011;12:160–174. doi: 10.1016/S1470-2045(11)70002-X. [DOI] [PubMed] [Google Scholar]
- 16.Linden W, Vodermaier A, Mackenzie R, et al. Anxiety and depression after cancer diagnosis: Prevalence rates by cancer type, gender, and age. J Affect Disord. 2012;141:343–351. doi: 10.1016/j.jad.2012.03.025. [DOI] [PubMed] [Google Scholar]
- 17. Starkey AJ, Keane CR, Terry MA, et al: Financial distress and depressive symptoms among African American women: Identifying financial priorities and needs and why it matters for mental health. J Urban Health 90:83-100, 2013. [DOI] [PMC free article] [PubMed]
- 18. Timmons A, Gooberman-Hill R, Sharp L: “It’s at a time in your life when you are most vulnerable”: A qualitative exploration of the financial impact of a cancer diagnosis and implications for financial protection in health. PLoS One 8:e77549, 2013. [DOI] [PMC free article] [PubMed]
- 19. Ramsey S, Blough D, Kirchhoff A, et al: Washington State cancer patients found to be at greater risk for bankruptcy than people without a cancer diagnosis. Health Aff (Millwood) 32:1143-1152, 2013. [DOI] [PMC free article] [PubMed]
- 20. Zafar SY, McNeil RB, Thomas CM, et al: Population-based assessment of cancer survivors’ financial burden and quality of life: A prospective cohort study. J Oncol Pract 11:145-150, 2015. [DOI] [PMC free article] [PubMed]
- 21.Delgado-Guay M, Ferrer J, Rieber AG, et al. Financial distress and its associations with physical and emotional symptoms and quality of life among advanced cancer patients. Oncologist. 2015;20:1092–1098. doi: 10.1634/theoncologist.2015-0026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kale HP, Carroll NV. Self-reported financial burden of cancer care and its effect on physical and mental health-related quality of life among US cancer survivors. Cancer. 2016;122:283–289. doi: 10.1002/cncr.29808. [DOI] [PubMed] [Google Scholar]
- 23.Sharp L, Carsin AE, Timmons A. Associations between cancer-related financial stress and strain and psychological well-being among individuals living with cancer. Psychooncology. 2013;22:745–755. doi: 10.1002/pon.3055. [DOI] [PubMed] [Google Scholar]
- 24. Reference deleted.
- 25.Jacobsen PB, Donovan KA, Trask PC, et al. Screening for psychologic distress in ambulatory cancer patients. Cancer. 2005;103:1494–1502. doi: 10.1002/cncr.20940. [DOI] [PubMed] [Google Scholar]
- 26.Tuinman MA, Gazendam-Donofrio SM, Hoekstra-Weebers JE. Screening and referral for psychosocial distress in oncologic practice: Use of the Distress Thermometer. Cancer. 2008;113:870–878. doi: 10.1002/cncr.23622. [DOI] [PubMed] [Google Scholar]
- 27.Prawitz AD, Garman ET, Sorhaindo B, et al. InCharge Financial Distress/Financial Well-Being Scale: Development, administration, and score interpretation. J Financial Counseling Plann. 2006;17 [Google Scholar]
- 28. Imai K, Keele L, Yamamoto T. Identification, inference and sensitivity analysis for causal mediation effects. Stat Sci 25:51-71, 2010 . [Google Scholar]
- 29.Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: New procedures and recommendations. Psychol Methods. 2002;7:422–445. [PubMed] [Google Scholar]
- 30. doi: 10.1037/0278-6133.27.2(Suppl.).S118. Barrera M, Strycker LA, Mackinnon DP, et al: Social-ecological resources as mediators of two-year diet and physical activity outcomes in type 2 diabetes patients. Health Psychol 27:S118-S125, 2008 (suppl 2) [DOI] [PubMed] [Google Scholar]
- 31. Alston C, Berger ZD, Brownlee S, et al: Shared Decision-Making Strategies for Best Care: Patient Decision Aids. Washington, DC, National Academy of Medicine, 2014. [Google Scholar]
- 32.Schnipper LE, Davidson NE, Wollins DS, et al. American Society of Clinical Oncology statement: A conceptual framework to assess the value of cancer treatment options. J Clin Oncol. 2015;33:2563–2577. doi: 10.1200/JCO.2015.61.6706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bestvina CM, Zullig LL, Rushing C, et al. Patient-oncologist cost communication, financial distress, and medication adherence. J Oncol Pract. 2014;10:162–167. doi: 10.1200/JOP.2014.001406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. doi: 10.1200/JCO.2015.64.7867. Saltz LB: The value of considering cost, and the cost of not considering value. J Clin Oncol 34:659-660, 2016 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. doi: 10.1200/JCO.2015.63.7736. Dusetzina SB, Keating NL: Mind the gap: Why closing the doughnut hole is insufficient for increasing Medicare beneficiary access to oral chemotherapy. J Clin Oncol 34:375-380, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mitchell AJ. Pooled results from 38 analyses of the accuracy of distress thermometer and other ultra-short methods of detecting cancer-related mood disorders. J Clin Oncol. 2007;25:4670–4681. doi: 10.1200/JCO.2006.10.0438. [DOI] [PubMed] [Google Scholar]
- 37.de Souza JA, Yap BJ, Hlubocky FJ, et al. The development of a financial toxicity patient-reported outcome in cancer: The COST measure. Cancer. 2014;120:3245–3253. doi: 10.1002/cncr.28814. [DOI] [PubMed] [Google Scholar]
- 38.Donovan KA, Jacobsen PB. Progress in the implementation of NCCN guidelines for distress management by member institutions. J Natl Compr Canc Netw. 2013;11:223–226. doi: 10.6004/jnccn.2013.0029. [DOI] [PubMed] [Google Scholar]
- 39. doi: 10.1188/14.CJON.S1.26-30. Tavernier SS: Translating research on the distress thermometer into practice. Clin J Oncol Nurs 18:26-30, 2014 (suppl) [DOI] [PubMed] [Google Scholar]
- 40.Merport A, Bober SL, Grose A, et al. Can the distress thermometer (DT) identify significant psychological distress in long-term cancer survivors? A comparison with the Brief Symptom Inventory-18 (BSI-18) Support Care Cancer. 2012;20:195–198. doi: 10.1007/s00520-011-1269-7. [DOI] [PubMed] [Google Scholar]
- 41. Wong YN, Egleston BL, Sachdeva K, et al: Cancer patients’ trade-offs among efficacy, toxicity, and out-of-pocket cost in the curative and noncurative setting. Med Care 51:838-845, 2013. [DOI] [PMC free article] [PubMed]
- 42.Stump TK, Eghan N, Egleston BL, et al. Cost concerns of patients with cancer. J Oncol Pract. 2013;9:251–257. doi: 10.1200/JOP.2013.000929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Smith SK, Nicolla J, Zafar SY. Bridging the gap between financial distress and available resources for patients with cancer: A qualitative study. J Oncol Pract. 2014;10:e368–e372. doi: 10.1200/JOP.2013.001342. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.