Abstract
Objective:
Although persons who inject drugs (PWID) in the western United States–Mexico border region are known to inject both heroin and methamphetamine, little is known about the prevalence and risks associated with co-injection of this depressant–stimulant combination (also known as “goofball” and “Mexican speedball”).
Method:
Baseline data from parallel cohort studies of PWID conducted concurrently in San Diego, CA, and Tijuana, Mexico, were used to estimate the prevalence and identify correlates of heroin–methamphetamine co-injection. PWID older than 18 years of age who reported injecting illicit drugs in the past month (N = 1,311; 32.7% female) were recruited in San Diego (n = 576) and Tijuana (n = 735) and completed interviewer-administered questionnaires. Bivariate and multivariable logistic regression analyses were used to identify correlates of heroin–methamphetamine co-injection.
Results:
The prevalence of co-injection in the past 6 months was 39.9% overall and was higher in Tijuana (55.8%) than in San Diego (19.8%). In multivariable analyses adjusting for study cohort, distributive syringe sharing, purchasing syringes prefilled with drugs, finding it hard to get new syringes, reporting great or urgent need for treatment, and younger age were independently associated with co-injection. Past-6-month overdose was significantly associated with higher odds of co-injection in San Diego than in Tijuana.
Conclusions:
These findings indicate that heroin–methamphetamine co-injection is more common in Tijuana than in San Diego, yet this practice was only associated with overdose in San Diego. Heroin–methamphetamine co-injection was also independently associated with HIV-associated injection risk behaviors. Overdose-prevention interventions should address co-injection of depressants and stimulants.
Although heroin is the main illicit drug injected worldwide (United Nations Office on Drugs and Crime [UNODC], 2014), methamphetamine has emerged as a major drug of abuse by injection and smoking routes of administration, especially in western U.S. states and northwestern Mexico. Methamphetamine production has increased in Mexico (Brouwer et al., 2006; Bucardo et al., 2005; UNODC, 2014) following U.S. crackdown on laboratories and regulation of precursor chemicals in the 1990s, and Mexico has replaced Colombia as the major regional producer of heroin (Organization of American States, 2013). Tijuana, Baja California, Mexico, and San Diego, CA, are adjacent cities on the westernmost edge of the U.S.–Mexico border, connected by the busiest land border crossing in the Western Hemisphere and situated on a major drug trafficking route (Brouwer et al., 2006). Production and trafficking of heroin and methamphetamine in Mexico and trafficking to other countries, mainly the United States, has had a “spillover” effect into local consumption markets. This spillover effect is seen particularly along the U.S.–Mexico border, where higher consumption of methamphetamine in northwestern Mexico mirrors the east–west cocaine–methamphetamine gradient of use observed north of the border (Brouwer et al., 2006; Bucardo et al., 2005; Case et al., 2008).
Polydrug use, or use of multiple substances, is associated with substance use disorder diagnosis, younger age, and male gender (Hunt et al., 2003; Merikangas et al., 1998). Use of multiple substances places great strain on the respiratory and cardiac functions of the body, putting users at greater risk for overdose (Davidson, 1999). Use of heroin, a central nervous system depressant (Darke & Zador, 1996), increases risk for overdose because of lowered respiratory rate, whereas methamphetamine, a central nervous system stimulant, increases heart rate and, correspondingly, oxygen demands (Radfar & Rawson, 2014), thereby increasing the risk for cardiac arrest. The stimulant effect of methamphetamine counterbalances the depressant effects of heroin and could allow persons who inject drugs (PWID) to tolerate larger heroin doses initially, but because methamphetamine’s effects wear off sooner than heroin’s, co-injection of these two substances may increase the risk for overdose through both respiratory suppression and cardiac arrest.
Methamphetamine use has been linked to high-risk sexual behaviors, including greater number of casual partners and inconsistent condom use (Cheng et al., 2010; Degenhardt et al., 2010; Patterson et al., 2008; Rusch et al., 2009; Semple et al., 2002), which could increase the likelihood of HIV seroconversion (Kral et al., 2001; Patterson et al., 2008). It is not clear from the existing research if this increased sexual risk for HIV among methamphetamine users is also increased for heroin–methamphetamine co-injectors. In addition to increased sexual libido, motivations for methamphetamine use include increased sociability and energy and loss of inhibitions (Cheng et al., 2010; Degenhardt et al., 2010; Semple et al., 2002); this is in contrast to the analgesic, depressant, and dissociative effects of heroin. Although the majority of PWID inject heroin and other opioids, PWID who co-inject heroin and methamphetamine may engage in more unsafe injecting practices than people who inject heroin because of the added socializing and disinhibitory effects of methamphetamine.
Stimulant–heroin combinations have been reported as common among PWID in qualitative interviews in Tijuana in 2004. Participants reported that the combination of drugs was cheaper than buying heroin alone (Case et al., 2008), and that the combination is also used to intensify the effect of low-purity heroin. Specific street names for this combination in Mexico include “speedball” or “espibulazo” (which may also refer to cocaine and heroin combinations), “Mexican speedball,” as well as “coctel de muerte” (cocktail of death) (Case et al., 2008; Strathdee et al., 2005). Field staff in Tijuana have reported that this combination is also referred to as “speedys.” In the United States this combination may be referred to as “goofball” (Jenkins et al., 2011; Ochoa et al., 2005) or “Mexican speedball.”
The U.S.–Mexico border region is characterized by dramatic income disparities between the two countries and high levels of migration (Strathdee et al., 2005). Injection drug use, a large red-light district (zona roja) attracting sex tourism, and high levels of social and economic disparities have contributed to a localized HIV epidemic in Tijuana. Given the substantial bidirectional traffic of people and goods in this region, there are significant implications for cross-border spread of unsafe injecting practices that heighten the risk of blood-borne infections, including HIV and hepatitis C. Although PWID are known to inject both heroin and methamphetamine (Darke & Hall, 1995; Garfein et al., 2013; Meacham et al., 2015; Roth et al., 2015; Rusch et al., 2009), less is known about the prevalence of and risks associated with mixed or co-injection of this depressant–stimulant combination.
The present analysis examined the prevalence and correlates of heroin–methamphetamine co-injection among PWID in San Diego, California, and Tijuana, Baja California. Given the production of methamphetamine in Mexico and the limited access to healthcare and drug treatment services, we hypothesized that past-6-month prevalence of heroin–methamphetamine co-injection would be higher among PWID in Tijuana. We also hypothesized that, compared with PWID who did not co-inject, PWID who co-injected heroin and methamphetamine would be more likely to engage in HIV-associated injection and sexual risk behaviors (e.g., sharing syringes and having unprotected sex) and to have experienced a recent overdose. Examining prevalence and correlates of co-injection of these two substances may indicate that this is a high-risk behavior associated with HIV and overdose among PWID in these two adjacent border cities facing methamphetamine use epidemics.
Method
Study participants and procedures
Data for these analyses come from the baseline assessments of two parallel prospective cohort studies of PWID in Tijuana (Proyecto El Cuete Phase IV) and in San Diego (STAHR II). The studies were designed to be comparable in their methods, aims, and survey content (Robertson et al., 2014). From March 2011 to May 2012, Proyecto El Cuete IV enrolled 735 participants who completed quantitative surveys and HIV testing every 6 months for 3 years. From June 2012 to January 2014, STAHR II enrolled 576 participants who completed quantitative surveys and HIV testing every 6 months for 2 years.
Potential participants were recruited through convenience sampling using targeted street and venue-based outreach by local staff and peer referrals. These individuals were referred to storefront offices, where they were screened for eligibility and underwent informed consent procedures. Eligibility criteria included (a) injecting illicit drugs within the past month, confirmed by track marks; (b) age 18 or older; (c) speaking Spanish or English; (d) current residence in Tijuana (El Cuete) or San Diego (STAHR) with no plans to move for 2 years; and (e) not currently participating in intervention research studies.
Trained interviewers administered quantitative questionnaires in English or Spanish using computer-assisted personal interview technology on a laptop in a private room. The baseline assessment included questions about sociodemographics and lifetime and past-6-month history of drug use and related health behaviors. Participants were reimbursed for completing the baseline assessment and disease testing ($25 USD for STAHR II and $20 USD for El Cuete IV). Pre- and post-test counseling for HIV was performed according to Centers for Disease Control and Prevention guidelines, and HIV-positive individuals were given referrals for free or reduced-cost healthcare. Additional details regarding HIV testing and parallel study procedures can be found in a previously published article (Robertson et al., 2014). The University of California San Diego Human Research Protection Program approved both study protocols. The Institutional Review Board for el Colegio de la Frontera Norte (COLEF) also approved the study protocol for El Cuete IV.
Measures
Dependent variable.
Participants were asked about heroin–methamphetamine co-injection over their lifetime and in the past 6 months. Frequency of heroin–methamphetamine co-injection in the past 6 months was dichotomized into yes or no. For this analysis, we used co-injection in the past 6 months as the dependent variable, rather than lifetime use, to understand associations with behaviors over a more defined and specific time range.
Sociodemographic characteristics assessed at baseline included age, gender, education level, income, housing status, birthplace, and years living in Tijuana or San Diego. For this comparative analysis, education level was dichotomized to completion of high school in San Diego (yes/no) and to completion of preparatoria (i.e., 12 years of education) in Tijuana (yes/no). For housing status, participants were asked where they had lived or slept in the past 6 months. From an identical list of options for both studies, responses of sleeping most often in a vehicle, abandoned building, shelter, in the streets, or in a shooting gallery were classified as sleeping in places consistent with being homeless (yes/no). Participants also reported their age at first injection; the difference between age and age at first injection was calculated to provide an estimate of duration of injection behavior.
HIV-associated injection behaviors included past-6-month engagement in receptive syringe sharing; distributive syringe sharing; sharing of cookers, cotton, or rinse water; sharing unbleached syringes; dividing drugs using a syringe; and purchasing a prefilled syringe.
HIV-associated sexual behaviors included past-6-month engagement in unprotected sex with a casual partner; having two or more casual partners; exchanging sex for food, money, drugs, or shelter; and using drugs during or within 2 hours before having sex.
HIV and overdose.
A dichotomous variable was used to indicate whether participants tested positive for HIV through serologic testing. Interviewers asked participants if they had experienced an opioid overdose in their lifetime and in the past 6 months, defining overdose as a “situation where you passed out due to drug use and could not wake or your lips turned blue.”
Harm-reduction service need was assessed by two questions regarding need for help for drug use and difficulty of accessing sterile syringes. Participants were asked to state to what degree they need help for their drug use, with response options of no need, some need, great need, and urgent need, which were dichotomized into no or some need versus great or urgent need. Participants were also asked how hard it was to obtain sterile syringes, with responses dichotomized into easy or very easy versus hard or very hard.
Statistical analysis
Univariate descriptive statistics were assessed overall and by study cohort (Tijuana vs. San Diego). Chi-square tests and Wilcoxon rank sum tests were used to determine bivariate associations between co-injection and sociodemographic characteristics, HIV-associated risk behaviors, HIV status, recent overdose, harm-reduction service need, and study cohort. Covariates with a significance level of p < .10 were considered for inclusion in multivariable logistic regression analysis to determine independent associations. These covariates were then added by conceptual blocks hierarchically into a logistic regression model in a manual stepwise fashion starting with injection behaviors and followed by sexual behaviors, health outcomes, harm-reduction service need, and sociodemographic characteristics. Covariates with regression coefficients significant at p < .05 were retained in the final model.
Interaction terms with study cohort and covariates significant in the main effects model were tested to determine if associations with co-injecting behavior were different in the two cohorts. To determine if they were potential confounders, variables significant at the bivariate level but not in the final model were added to assess changes in coefficients of more than 10% for variables in the final multivariable model. We also checked for linearity on the logit scale for the continuous covariate variables (Hosmer et al., 2013).
Results
Sample characteristics and prevalence of co-injection
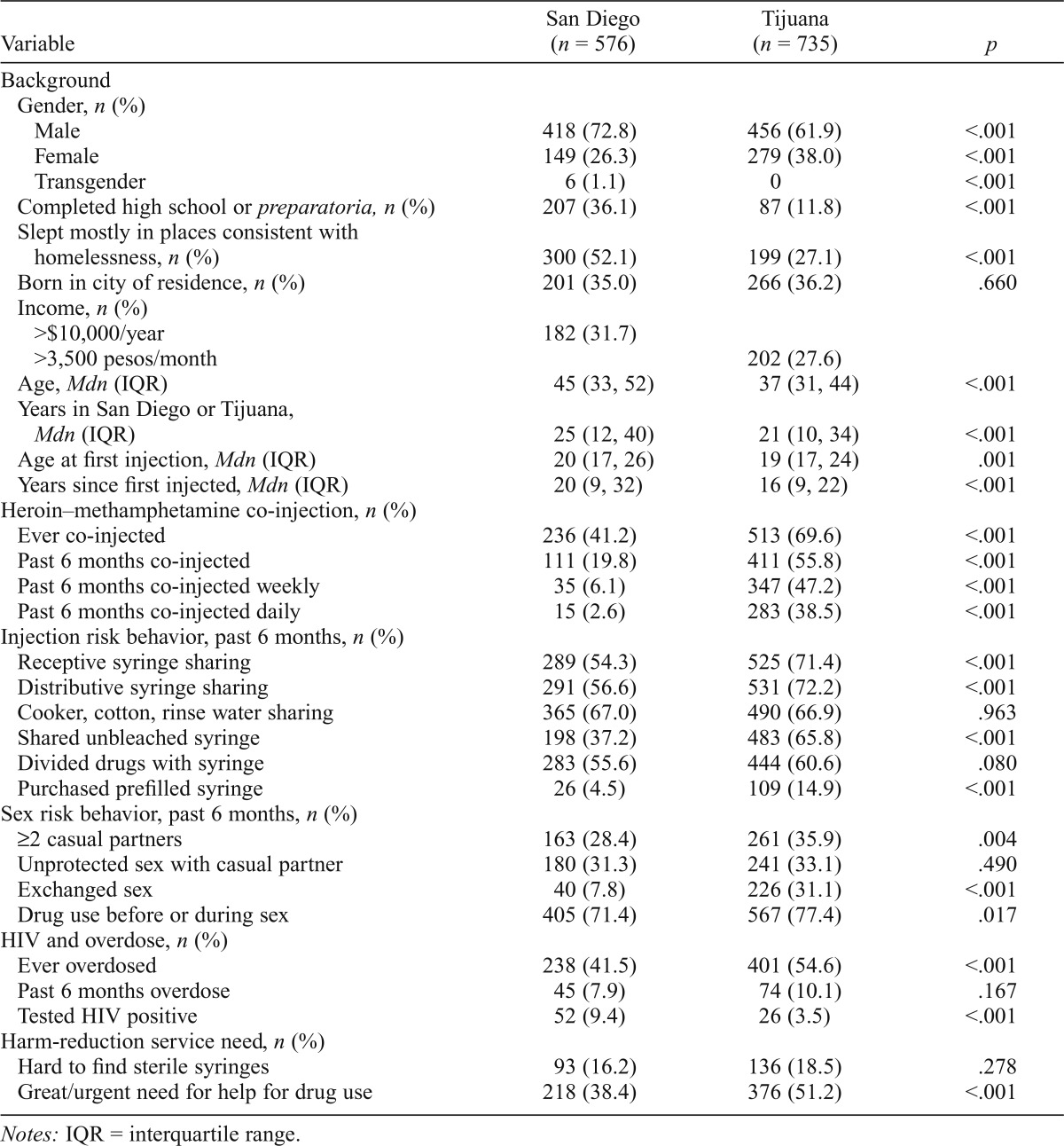
Among the 1,311 participants from both cohorts (San Diego: n = 576; Tijuana: n = 735), 32.7% were female, and the median age was 39 (range: 18–70 years). Less than one quarter (22.4%) had completed high school or preparatoria, and 42.0% slept in places consistent with being homeless in the past 6 months. About one third of participants (35.7%) were born in the city in which they were enrolled. Participants had resided in San Diego or Tijuana for a median of 24 years and had been injecting for a median of 17 years, with a median age at first injection of 20 years. There were quite a few significant differences between the two cohorts for several sociodemographic characteristics. A greater percentage of participants from Tijuana were female (38.0 vs. 26.3%, p < .001). Compared with San Diego participants, Tijuana participants were less likely to have completed preparatoria, had a younger median age, and had lived fewer years in their city of residence. San Diego participants were more likely to report sleeping most often in places consistent with homelessness (Table 1).
Table 1.
Comparison of sociodemographics, heroin–methamphetamine co-injection, HIV risk behaviors, overdose, HIV status, and service need between persons who inject drugs in San Diego and Tijuana (N = 1,311)
| Variable | San Diego (n = 576) | Tijuana (n = 735) | p |
| Background | |||
| Gender, n (%) | |||
| Male | 418 (72.8) | 456 (61.9) | <.001 |
| Female | 149 (26.3) | 279 (38.0) | <.001 |
| Transgender | 6(1.1) | 0 | <.001 |
| Completed high school or preparatoria, n (%) | 207 (36.1) | 87 (11.8) | <.001 |
| Slept mostly in places consistent with homelessness, n (%) | 300 (52.1) | 199 (27.1) | <.001 |
| Born in city of residence, n (%) | 201 (35.0) | 266 (36.2) | .660 |
| Income, n (%) | |||
| >$10,000/year | 182 (31.7) | ||
| >3,500 pesos/month | 202 (27.6) | ||
| Age, Mdn (IQR) | 45 (33, 52) | 37 (31, 44) | <.001 |
| Years in San Diego or Tijuana, Mdn (IQR) | 25 (12, 40) | 21 (10, 34) | <.001 |
| Age at first injection, Mdn (IQR) | 20 (17, 26) | 19 (17, 24) | .001 |
| Years since first injected, Mdn (IQR) | 20 (9, 32) | 16 (9, 22) | <.001 |
| Heroin–methamphetamine co-injection, n (%) | |||
| Ever co-injected | 236 (41.2) | 513 (69.6) | <.001 |
| Past 6 months co-injected | 111 (19.8) | 411 (55.8) | <.001 |
| Past 6 months co-injected weekly | 35 (6.1) | 347 (47.2) | <.001 |
| Past 6 months co-injected daily | 15 (2.6) | 283 (38.5) | <.001 |
| Injection risk behavior, past 6 months, n (%) | |||
| Receptive syringe sharing | 289 (54.3) | 525 (71.4) | <.001 |
| Distributive syringe sharing | 291 (56.6) | 531 (72.2) | <.001 |
| Cooker, cotton, rinse water sharing | 365 (67.0) | 490 (66.9) | .963 |
| Shared unbleached syringe | 198 (37.2) | 483 (65.8) | <.001 |
| Divided drugs with syringe | 283 (55.6) | 444 (60.6) | .080 |
| Purchased prefilled syringe | 26 (4.5) | 109 (14.9) | <.001 |
| Sex risk behavior, past 6 months, n (%) | |||
| ≥2 casual partners | 163 (28.4) | 261 (35.9) | .004 |
| Unprotected sex with casual partner | 180 (31.3) | 241 (33.1) | .490 |
| Exchanged sex | 40 (7.8) | 226 (31.1) | <.001 |
| Drug use before or during sex | 405 (71.4) | 567 (77.4) | .017 |
| HIV and overdose, n (%) | |||
| Ever overdosed | 238 (41.5) | 401 (54.6) | <.001 |
| Past 6 months overdose | 45 (7.9) | 74(10.1) | .167 |
| Tested HIV positive | 52 (9.4) | 26 (3.5) | <.001 |
| Harm-reduction service need, n (%) | |||
| Hard to find sterile syringes | 93 (16.2) | 136 (18.5) | .278 |
| Great/urgent need for help for drug use | 218 (38.4) | 376 (51.2) | <.001 |
Notes: IQR = interquartile range.
Overall prevalence of heroin–methamphetamine co-injection in the past 6 months was 39.9% and was significantly higher in Tijuana than in San Diego (55.8% vs. 19.8%, p < .001). HIV prevalence overall was 6.1% and was higher in San Diego than in Tijuana. Prevalence of self-reported overdose in the past 6 months was 9.1%. Nearly all HIV-associated injection behaviors, except for purchasing a prefilled syringe, were reported by a majority of participants (55.6%–69.2%). Three quarters of participants reported using drugs before or during sex. About one third reported having two or more casual sexual partners in the past 6 months and having unprotected sex with a casual sex partner. One fifth reported exchanging sex for food, money, drugs, or shelter in the past 6 months, with a greater percentage reporting this in Tijuana than in San Diego (Table 1).
Correlates of heroin–methamphetamine co-injection
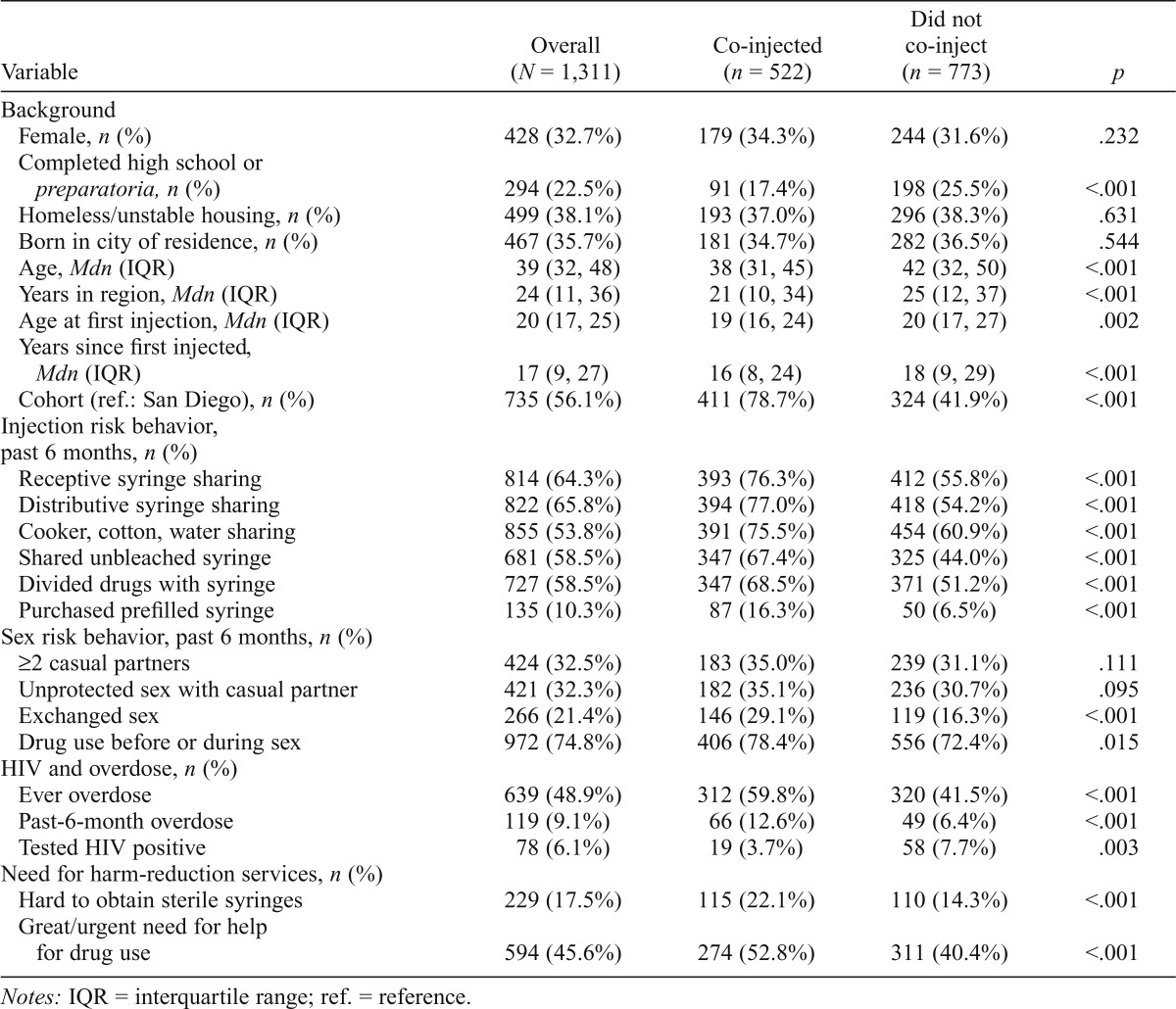
In bivariate analyses (Table 2), those who co-injected heroin and methamphetamine were more likely to be younger, to have spent less time in the region, to have injected for less time, and to have started injecting at a younger age. Consistent with our hypothesis, those who co-injected were more likely to have engaged in HIV-associated injection risk behaviors. They were also more likely to have exchanged sex for something they needed, used drugs before or during sex, and overdosed in the past 6 months. Furthermore, PWID who co-injected heroin and methamphetamine were more likely to report great or urgent need for help for their drug use and to report that it was hard or very hard to obtain sterile syringes.
Table 2.
Bivariate analysis of factors associated with heroin–methamphetamine co-injection in the past 6 months among persons who inject drugs in San Diego and Tijuana (N = 1,311)
| Variable | Overall (N = 1,311) | Co-injected (n = 522) | Did not co-inject (n = 773) | p |
| Background | ||||
| Female, n (%) | 428 (32.7%) | 179 (34.3%) | 244 (31.6%) | .232 |
| Completed high school or preparatoria, n (%) | 294 (22.5%) | 91 (17.4%) | 198 (25.5%) | <.001 |
| Homeless/unstable housing, n (%) | 499 (38.1%) | 193 (37.0%) | 296 (38.3%) | .631 |
| Born in city of residence, n (%) | 467 (35.7%) | 181 (34.7%) | 282 (36.5%) | .544 |
| Age, Mdn (IQR) | 39 (32, 48) | 38 (31, 45) | 42 (32, 50) | <.001 |
| Years in region, Mdn (IQR) | 24(11, 36) | 21 (10, 34) | 25 (12, 37) | <.001 |
| Age at first injection, Mdn (IQR) | 20(17, 25) | 19(16, 24) | 20(17, 27) | .002 |
| Years since first injected, Mdn (IQR) | 17 (9, 27) | 16(8, 24) | 18(9, 29) | <.001 |
| Cohort (ref.: San Diego), n (%) | 735 (56.1%) | 411 (78.7%) | 324 (41.9%) | <.001 |
| Injection risk behavior, past 6 months, n (%) | ||||
| Receptive syringe sharing | 814(64.3%) | 393 (76.3%) | 412 (55.8%) | <.001 |
| Distributive syringe sharing | 822 (65.8%) | 394 (77.0%) | 418 (54.2%) | <.001 |
| Cooker, cotton, water sharing | 855 (53.8%) | 391 (75.5%) | 454 (60.9%) | <.001 |
| Shared unbleached syringe | 681 (58.5%) | 347 (67.4%) | 325 (44.0%) | <.001 |
| Divided drugs with syringe | 727 (58.5%) | 347 (68.5%) | 371 (51.2%) | <.001 |
| Purchased prefilled syringe | 135 (10.3%) | 87(16.3%) | 50 (6.5%) | <.001 |
| Sex risk behavior, past 6 months, n (%) | ||||
| ≥2 casual partners | 424 (32.5%) | 183 (35.0%) | 239 (31.1%) | .111 |
| Unprotected sex with casual partner | 421 (32.3%) | 182 (35.1%) | 236 (30.7%) | .095 |
| Exchanged sex | 266(21.4%) | 146 (29.1%) | 119(16.3%) | <.001 |
| Drug use before or during sex | 972 (74.8%) | 406 (78.4%) | 556 (72.4%) | .015 |
| HIV and overdose, n (%) | ||||
| Ever overdose | 639 (48.9%) | 312(59.8%) | 320 (41.5%) | <.001 |
| Past-6-month overdose | 119(9.1%) | 66 (12.6%) | 49 (6.4%) | <.001 |
| Tested HIV positive | 78(6.1%) | 19 (3.7%) | 58 (7.7%) | .003 |
| Need for harm-reduction services, n (%) | ||||
| Hard to obtain sterile syringes | 229(17.5%) | 115 (22.1%) | 110(14.3%) | <.001 |
| Great/urgent need for help for drug use | 594 (45.6%) | 274 (52.8%) | 311 (40.4%) | <.001 |
Notes: IQR = interquartile range; ref. = reference.
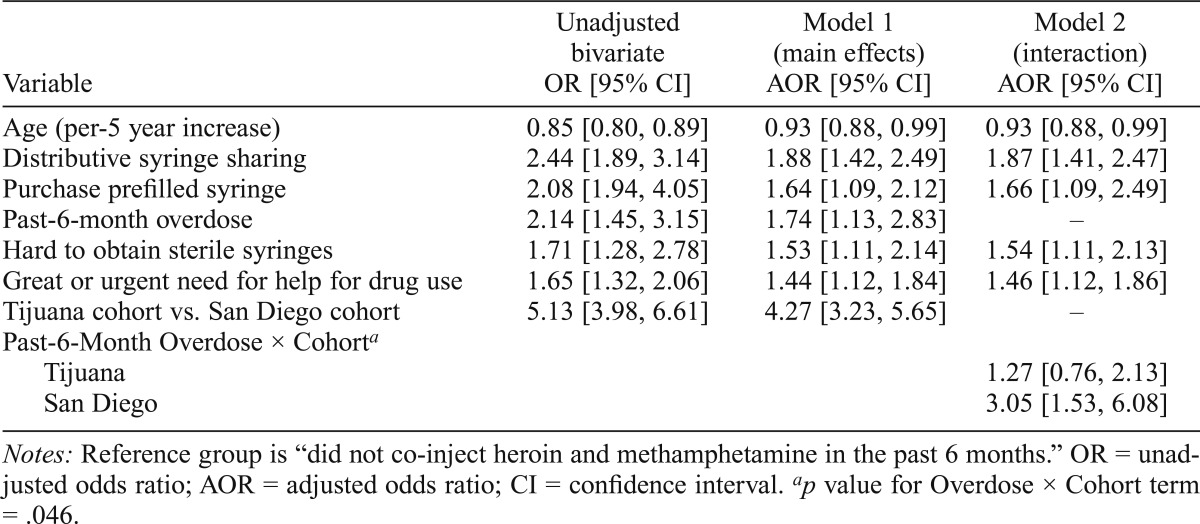
Independent associations with co-injection
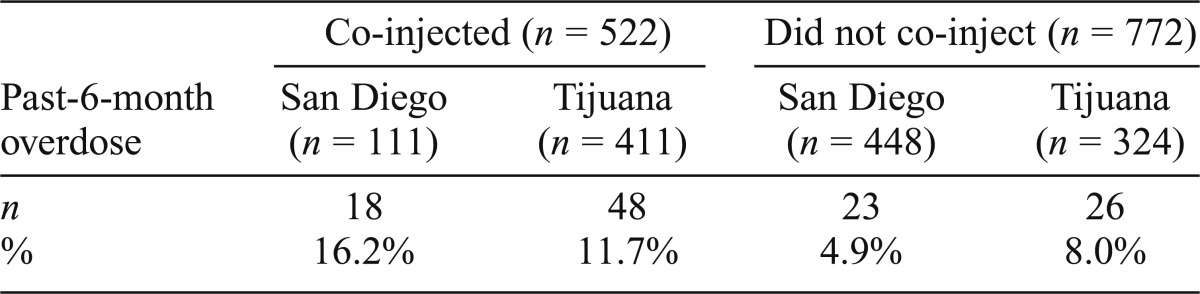
In multivariable logistic regression analyses adjusting for study site (Table 3, Model 2), heroin–methamphetamine co-injection was independently and positively associated with distributive syringe sharing (adjusted odds ratio [AOR] = 1.87, 95% CI [1.41, 2.47]), purchasing a prefilled syringe (AOR = 1.66, 95% CI [1.09, 2.49]), finding it hard to obtain sterile syringes (AOR = 1.54, 95% CI [1.11, 2.13]), reporting great or urgent need for help for drug use (AOR = 1.46, 95% CI [1.12, 1.86]), and younger age (AOR = 0.93 per 5 years, 95% CI [0.88, 0.99]). A statistically significant interaction (p = .046) between overdose and study cohort showed that the odds of co-injection were higher for those with a recent overdose compared with those without a recent overdose in San Diego (AOR = 3.05, 95% CI [1.53, 6.08]) and Tijuana (AOR = 1.27, 95% CI [0.76, 2.13]), although the 95% CI for the AOR overlapped with 1 in Tijuana. To further demonstratethis interaction, the conditional prevalence of overdose in the past 6 months by co-injection and study cohort is presented in Table 4.
Table 3.
Multivariable analysis of factors associated with heroin–methamphetamine co-injection in the past 6 months among persons who inject drugs in San Diego and Tijuana (n = 1,224)
| Variable | Unadjusted bivariate OR [95% CI] | Model 1 (main effects) AOR [95% CI] | Model 2 (interaction) AOR [95% CI] |
| Age (per-5 year increase) | 0.85 [0.80, 0.89] | 0.93 [0.88, 0.99] | 0.93 [0.88, 0.99] |
| Distributive syringe sharing | 2.44 [1.89, 3.14] | 1.88 [1.42, 2.49] | 1.87 [1.41, 2.47] |
| Purchase prefilled syringe | 2.08 [1.94, 4.05] | 1.64 [1.09, 2.12] | 1.66 [1.09, 2.49] |
| Past-6-month overdose | 2.14 [1.45, 3.15] | 1.74 [1.13, 2.83] | – |
| Hard to obtain sterile syringes | 1.71 [1.28, 2.78] | 1.53 [1.11, 2.14] | 1.54 [1.11, 2.13] |
| Great or urgent need for help for drug use | 1.65 [1.32, 2.06] | 1.44 [1.12, 1.84] | 1.46 [1.12, 1.86] |
| Tijuana cohort vs. San Diego cohort | 5.13 [3.98, 6.61] | 4.27 [3.23, 5.65] | – |
| Past-6-Month Overdose × Cohorta | |||
| Tijuana | 1.27 [0.76, 2.13] | ||
| San Diego | 3.05 [1.53, 6.08] |
Notes: Reference group is “did not co-inject heroin and methamphetamine in the past 6 months.” OR = unadjusted odds ratio; AOR = adjusted odds ratio; CI = confidence interval.
p value for Overdose × Cohort term = .046.
Table 4.
Conditional prevalence of past-6-month overdose by heroin–methamphetamine co-injection use and study cohort (n = 1,294)
| Co-injected (n = 522) |
Did not co-inject (n = 772) |
|||
| Past-6-month overdose | San Diego (n = 111) | Tijuana (n = 411) | San Diego (n = 448) | Tijuana (n = 324) |
| n | 18 | 48 | 23 | 26 |
| % | 16.2% | 11.7% | 4.9% | 8.0% |
Discussion
Findings indicate that heroin–methamphetamine co-injection among PWID is more common in Tijuana than in San Diego, yet this practice had a positive independent association with overdose in San Diego and a lower and positive although not significant independent association in Tijuana. Heroin–methamphetamine co-injection was also independently associated with injection risk behaviors but not independently associated with sexual risk behaviors. PWID who co-injected these two drugs were younger and reported more difficulty finding sterile syringes and being in greater need of help for their drug use.
The prevalence of heroin–methamphetamine co-injection in the past 6 months in Tijuana PWID appeared stable, yet high, when results from the present study were compared with results from an earlier cohort study conducted in 2006–2007 (55.8% vs. 53.3%, respectively) (Meacham et al., 2015). Although the prevalence was lower among San Diego PWID compared with Tijuana PWID in the present study (19.8%), prevalence appears to have increased compared with results of an earlier study conducted in 2009–2010 (7.2%) (Garfein et al., 2013). This increase among PWID in San Diego should be interpreted cautiously, however, because the earlier cohort was restricted to PWID ages 18–40 years but open to PWID who had injected in the past 6 months (compared with in the previous month for the present study).
Few other epidemiologic studies have reported on heroin–methamphetamine co-injection. Other reports of heroin–methamphetamine co-injection in the United States include 11.0% of Seattle syringe exchange program participants reporting use in the past year in 2009 (Jenkins et al., 2011) and 23.0% of young PWID in San Francisco reporting use in the past 3 months in 2000–2001 (Ochoa et al., 2005). These studies also found that this behavior was associated with past-year nonfatal overdose.
Another stimulant–depressant combination—heroin and cocaine co-injection—known as “speedball,” has been reported as more common in the east coast of United States (Garfein et al., 2004), where cocaine is more commonly used than methamphetamine. PWID on the west coast may be co-injecting heroin and methamphetamine for similar reasons as those injecting speedballs on the east coast but using the more locally available methamphetamine instead of cocaine. Studies in Vancouver and San Francisco have also found that co-injection of heroin and cocaine was associated with overdose (Kerr et al., 2007; Ochoa et al., 2005).
Although all of these independent associations with HIV injection behaviors, service need, and age were of similar magnitude in both cohorts, we only observed a significant association between co-injection and overdose in San Diego. Given the lower prevalence of heroin–methamphetamine co-injection in San Diego, this finding may reflect that it is engaged in by higher risk-taking PWID in San Diego, whereas it may be more common and normalized among PWID in Tijuana. Nevertheless, overdose prevention efforts in both cities should address co-injection of heroin and methamphetamine.
Although it was hypothesized that sexual risk behavior would be greater among PWID who co-injected heroin and methamphetamine, this was not supported in multivariable analyses, perhaps because the independent association with HIV drug injection behaviors overshadowed the smaller bivariate association with sex exchange and using drugs before sex. Independent associations with distributive syringe sharing and prefilled syringe purchase may be indicative of the social circumstances surrounding injection, such as reciprocal sharing of drugs and minimizing other risks. This finding is consistent with the higher energy and greater sociability reported by methamphetamine users yet also suggests that this co-injection behavior may increase the chances of transmitting HIV through sharing of injection equipment.
The positive association between co-injection and the need for harm-reduction services (e.g., drug treatment and sterile syringe access) in both cities emphasizes and rein-forces the need for improved access to noncoercive treatment and syringe exchange programs. Existing treatment programs that focus on opioid substitution therapy for heroin users might not be as effective in reducing injection use for PWID who are also co-injecting methamphetamine. This association of need for help for drug use and co-injection also aligns with previous research that polydrug users may be more drug dependent (Merikangas et al., 1998).
There are limitations to this analysis that must be considered. Self-report of drug-using behavior and possible recall bias may raise questions about underreporting of substance use; however, many studies have demonstrated the general validity of PWID self-reports (Darke, 1998), and participants had already disclosed their injection behavior as an eligibility criterion for enrolling in these studies. Although the two studies were conducted concurrently and were designed to be comparable, these two populations of PWID and the environment in which they live are quite different. Given that this analysis used cross-sectional data, we are unable to determine temporal sequence between heroin–methamphetamine co-injection and overdose occurrence. Future studies should obtain greater specificity regarding the proximity of these events. In addition, overdose was self-reported and might not reflect true overdose prevalence in these samples. Generalizability of these findings may also be limited to regions in which heroin and methamphetamine use is common, although global drug use statistics indicate that co-occurrence of heroin use, methamphetamine use, and injection behaviors may be growing in several regions (UNODC, 2014).
As drug production regions and trans-shipment routes shift in response to environmental, economic, and policy changes, there is a need to pay attention to spillover effects into local drug consumption markets, particularly in less-developed regions with growing numbers of urban migrants (Singer, 2008). This is one of the first studies to specifically examine the association between heroin–methamphetamine co-injection and health risk behaviors in a large of sample of PWID in a dynamic bi-national border setting. Findings indicate the need to consider use of multiple substances as a correlate of HIV-associated risk behaviors and overdose occurrence, as well as a potential indicator in global drug use surveillance efforts (Degenhardt & Hall, 2012). Future research on specific drug combinations and routes of administration, as well as event-level motivations and contextual drug market factors, will further contribute to effective and appropriate responses and interventions to prevent HIV transmission and overdose.
Acknowledgments
The authors gratefully acknowledge the contributions to this research by the study participants and staff.
Footnotes
This research is funded by the National Institutes of Health Grants R01 DA031074 and R37 DA019829. Meredith C. Meacham was supported by Grant T32 DA023356, and Tommi L. Gaines was supported by Grant K01 DA034523.
References
- Brouwer K. C., Case P., Ramos R., Magis-Rodríguez C., Bucardo J., Patterson T. L., Strathdee S. A. Trends in production, trafficking, and consumption of methamphetamine and cocaine in Mexico. Substance Use & Misuse. 2006;41:707–727. doi: 10.1080/10826080500411478. doi:10.1080/10826080500411478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucardo J., Brouwer K. C., Magis-Rodríguez C., Ramos R., Fraga M., Perez S. G., Strathdee S. A. Historical trends in the production and consumption of illicit drugs in Mexico: Implications for the prevention of blood borne infections. Drug and Alcohol Dependence. 2005;79:281–293. doi: 10.1016/j.drugalcdep.2005.02.003. doi:10.1016/j.drugalcdep.2005.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case P., Ramos R., Brouwer K. C., Firestone-Cruz M., Pollini R. A., Strathdee S. A., Patterson T. L. At the borders, on the edge: Use of injected methamphetamine in Tijuana and Ciudad Juarez, Mexico. Journal of Immigrant and Minority Health. 2008;10:23–33. doi: 10.1007/s10903-007-9051-0. doi:10.1007%2Fs10903-007-9051-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng W. S., Garfein R. S., Semple S. J., Strathdee S. A., Zians J. K., Patterson T. L. Increased drug use and STI risk with injection drug use among HIV-seronegative heterosexual methamphetamine users. Journal of Psychoactive Drugs. 2010;42:11–18. doi: 10.1080/02791072.2010.10399781. doi:10.1080/02791072.2010.10399781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darke S. Self-report among injecting drug users: A review. Drug and Alcohol Dependence. 1998;51:253–263. doi: 10.1016/s0376-8716(98)00028-3. discussion 267–268. doi:10.1016/S0376-8716(98)00028-3. [DOI] [PubMed] [Google Scholar]
- Darke S., Hall W. Levels and correlates of polydrug use among heroin users and regular amphetamine users. Drug and Alcohol Dependence. 1995;39:231–235. doi: 10.1016/0376-8716(95)01171-9. doi:10.1016/0376-8716(95)01171-9. [DOI] [PubMed] [Google Scholar]
- Darke S., Zador D. Fatal heroin ‘overdose’: A review. Addiction. 1996;91:1765–1772. doi: 10.1046/j.1360-0443.1996.911217652.x. doi:10.1111/j.1360-0443.1996.tb03800.x. [DOI] [PubMed] [Google Scholar]
- Davidson P. Circumstances of death: An assessment of the viability of using non-toxicological coronial data to investigate opiate overdose risk factors. Perth, Australia: National Centre for Research into the Prevention of Drug Abuse; 1999. [Google Scholar]
- Degenhardt L., Hall W. Extent of illicit drug use and dependence, and their contribution to the global burden of disease. The Lancet. 2012;379:55–70. doi: 10.1016/S0140-6736(11)61138-0. doi:10.1016/S0140-6736(11)61138-0. [DOI] [PubMed] [Google Scholar]
- Degenhardt L., Mathers B., Guarinieri M., Panda S., Phillips B., Strathdee S. A., Howard J. the Reference Group to the United Nations on HIV and injecting drug use. Meth/amphetamine use and associated HIV: Implications for global policy and public health. International Journal of Drug Policy. 2010;21:347–358. doi: 10.1016/j.drugpo.2009.11.007. doi:10.1016/j.drugpo.2009.11.007. [DOI] [PubMed] [Google Scholar]
- Garfein R. S., Monterroso E. R., Tong T. C., Vlahov D., Des Jarlais D. C., Selwyn P., Holmberg S. D. Comparison of HIV infection risk behaviors among injection drug users from East and West Coast US cities. Journal of Urban Health. 2004;81:260–267. doi: 10.1093/jurban/jth112. doi:10.1093/jurban/jth112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garfein R. S., Rondinelli A., Barnes R. F. W., Cuevas J., Metzner M., Velasquez M., Teshale E. H. HCV infection prevalence lower than expected among 18–40-year-old injection drug users in San Diego, CA. Journal of Urban Health. 2013;90:516–528. doi: 10.1007/s11524-012-9728-0. doi:10.1007/s11524-012-9728-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosmer D. W., Lemeshow S., Sturdivant R. X. Applied logistic regression. Vol. 398. Hoboken, NJ: John Wiley & Sons; 2013. [Google Scholar]
- Hunt N., Trace M., Bewley-Taylor M. Reducing drug related harms to health: An overview of the global evidence. Oxford, England: The Beckley Foundation Drug Policy Programme; 2003. [Google Scholar]
- Jenkins L. M., Banta-Green C. J., Maynard C., Kingston S., Hanrahan M., Merrill J. O., Coffin P. O. Risk factors for nonfatal overdose at Seattle-area syringe exchanges. Journal of Urban Health. 2011;88:118–128. doi: 10.1007/s11524-010-9525-6. doi:10.1007/s11524-010-9525-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr T., Fairbairn N., Tyndall M., Marsh D., Li K., Montaner J., Wood E. Predictors of non-fatal overdose among a cohort of polysubstance-using injection drug users. Drug and Alcohol Dependence. 2007;87:39–45. doi: 10.1016/j.drugalcdep.2006.07.009. doi:10.1016/j.drugalcdep.2006.07.009. [DOI] [PubMed] [Google Scholar]
- Kral A. H., Bluthenthal R. N., Lorvick J., Gee L., Bacchetti P., Edlin B. R. Sexual transmission of HIV-1 among injection drug users in San Francisco, USA: Risk-factor analysis. The Lancet. 2001;357:1397–1401. doi: 10.1016/S0140-6736(00)04562-1. doi:10.1016/S0140-6736(00)04562-1. [DOI] [PubMed] [Google Scholar]
- Meacham M. C., Rudolph A. E., Strathdee S. A., Rusch M. L., Brouwer K. C., Patterson T. L., Roesch S. C. Polydrug use and HIV risk among people who inject heroin in Tijuana, Mexico: A latent class analysis. Substance Use & Misuse. 2015;50:1351–1359. doi: 10.3109/10826084.2015.1013132. doi:10.3109/10826084.2015.1013132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Merikangas K. R., Mehta R. L., Molnar B. E., Walters E. E., Swendsen J. D., Aguilar-Gaziola S., Kessler R. C. Comorbidity of substance use disorders with mood and anxiety disorders: Results of the International Consortium in Psychiatric Epidemiology. Addictive Behaviors. 1998;23:893–907. doi: 10.1016/s0306-4603(98)00076-8. doi:10.1016/S0306-4603(98)00076-8. [DOI] [PubMed] [Google Scholar]
- Ochoa K. C., Davidson P. J., Evans J. L., Hahn J. A., Page-Shafer K., Moss A. R. Heroin overdose among young injection drug users in San Francisco. Drug and Alcohol Dependence. 2005;80:297–302. doi: 10.1016/j.drugalcdep.2005.04.012. doi:10.1016/j.drugalcdep.2005.04.012. [DOI] [PubMed] [Google Scholar]
- Organization of American States. The Drug Problem in the Americas: Studies. Production and supply of drugs, pharmaceuticals, and chemical precursors. 2013. Retrieved from http://www.cicad.oas.org/drogas/elinforme/informeDrogas2013/produccionDrogas_ENG.pdf. [Google Scholar]
- Patterson T. L., Semple S. J., Staines H., Lozada R., Orozovich P., Bucardo J., Strathdee S. A. Prevalence and correlates of HIV infection among female sex workers in 2 Mexico-US border cities. Journal of Infectious Diseases. 2008;197:728–732. doi: 10.1086/527379. doi:10.1086/527379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radfar S. R., Rawson R. A. Current research on methamphetamine: Epidemiology, medical and psychiatric effects, treatment, and harm reduction efforts. Addiction & Health. 2014;6:146–154. [PMC free article] [PubMed] [Google Scholar]
- Robertson A. M., Garfein R. S., Wagner K. D., Mehta S. R., Magis-Rodriguez C., Cuevas-Mota J., Strathdee S. A. the Proyecto El Cuete IV and STAHR II. Evaluating the impact of Mexico’s drug policy reforms on people who inject drugs in Tijuana, B.C., Mexico, and San Diego, CA, United States: A binational mixed methods research agenda. Harm Reduction Journal. 2014;11:4. doi: 10.1186/1477-7517-11-4. doi:10.1186/1477-7517-11-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth A. M., Armenta R. A., Wagner K. D., Roesch S. C., Bluthenthal R. N., Cuevas-Mota J., Garfein R. S. Patterns of drug use, risky behavior, and health status among persons who inject drugs living in San Diego, California: A latent class analysis. Substance Use & Misuse. 2015;50:205–214. doi: 10.3109/10826084.2014.962661. doi:10.3109/10826084.2014.962661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rusch M. L., Lozada R., Pollini R. A., Vera A., Patterson T. L., Case P., Strathdee S. A. Polydrug use among IDUs in Tijuana, Mexico: Correlates of methamphetamine use and route of administration by gender. Journal of Urban Health. 2009;86:760–775. doi: 10.1007/s11524-009-9377-0. doi:10.1007/s11524-009-9377-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Semple S. J., Patterson T. L., Grant I. Motivations associated with methamphetamine use among HIV+ men who have sex with men. Journal of Substance Abuse Treatment. 2002;22:149–156. doi: 10.1016/s0740-5472(02)00223-4. doi: 10.1016/S0740-5472(02)00223-4. [DOI] [PubMed] [Google Scholar]
- Singer M. Drugs and development: The global impact of drug use and trafficking on social and economic development. International Journal on Drug Policy. 2008;19:467–478. doi: 10.1016/j.drugpo.2006.12.007. doi:10.1016/j.drugpo.2006.12.007. [DOI] [PubMed] [Google Scholar]
- Strathdee S. A., Fraga W. D., Case P., Firestone M., Brouwer K. C., Perez S. G., Fraga M. A. “Vivo para consumirla y la consumo para vivir” [“I live to inject and inject to live”]: High-risk injection behaviors in Tijuana, Mexico. Journal of Urban Health. 2005;82(Supplement 4):iv58–iv73. doi: 10.1093/jurban/jti108. doi:10.1093/jurban/jti108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United Nations Office on Drugs and Crime. World drug report 2014. Vienna, Austria: Author; 2014. Retrieved from http://www.unodc.org/documents/wdr2014/World_Drug_Report_2014_web.pdf. [Google Scholar]