Abstract
Focal gingival enlargements are a diverse group of lesions with almost similar clinical presentation but varied etiology and histopathology. The actual cause of peripheral ossifying fibroma (POF) has been debated over many years. POFs are usually seen in childhood and younger ages. There is a slight female predilection. It is usually localized, rarely generalized. Usually, the treatment option is only surgical excision with minimal chances of recurrence. Here, we report a case of POF of the right maxillary posterior region with a review of literature.
Key words: Epulis, focal overgrowths, gingival enlargements, ossification, peripheral ossifying fibroma
INTRODUCTION
Focal gingival enlargements are quite frequent lesions in the oral cavity amounting to almost 3.1% of all oral tumors and for 9.6% of gingival lesions.[1] In 1992, the World Health Organization classification about this kind of focal overgrowth had tapered toward one universal term “Peripheral Cemento-Ossifying Fibroma.” These lesions histopathologically have fibrous stroma with varying amounts of mineralized materials.[2] We, in our case report prefer to call it as peripheral ossifying fibroma (POF). POFs are more frequent in younger ages, peak being in the second decade, although there are cases occurring in older age groups also. There could be a hormonal influence for such a finding.[3] There is a strong female predilection.[4,5] There is uncertainty for diagnosing focal reactive overgrowths of the gingiva because of their nearly same clinical presentation. The typical appearance of POF is small gingival growth (Epulis) initially which can attain large sizes so as to cause facial disfigurement. They do not have radiological changes generally. If the lesions grow to larger sizes, there can be a mild erosion of bone. The treatment of POF is straight forward with surgical excision with blade and scalpel commonly followed. A newer approach is the use of diode lasers for its removal, probably having an advantage of lesser bleeding and predicted results. Whatever may be the method of removal, it should be sent for histopathological diagnosis. Here, we report a rare case of POF affecting the right maxillary region.
CASE REPORT
A 60 year old female presented to us with a chief complaint of swelling on the right maxillary posterior region of jaw since 3-4 years. It was sometimes associated with draining yellow color fluid which was salty in taste. She also gave a history of the slow growth of the mass since last 3-years to reach the present size. There were no other symptoms and no history of pain. Her medical history was noncontributory.
The oral examination showed the presence of a solitary pedunculated mass of size 4 cm × 2 cm × 3 cm which was red in color with lobulated surface on the right maxillary posterior alveolar ridge. The overlying and surrounding gingiva was inflamed [Figure 1]. She was partially edentulous with only four teeth remaining in the oral cavity. On palpation, the mass was firm, nontender, and not fixed to underlying structure. Orthopantomogram (OPG) evaluation showed the presence of a unilocular radiolucent area extending superiorly into the corresponding maxillary sinus, posteriorly to maxillary tuberosity, and anteriorly until the distal end of canine. Few areas of radio-opacities were also seen [Figure 2a]. Dento-alveolar scan did not show the extension of mass into maxillary sinus, rather showed the inflamed lining of the sinus. The floor of the maxillary sinus was intact [Figure 2b]. A three dimensional construction image done after dento-alveolar scan confirmed the calcifications [Figure 2c] within the mass which was seen as radio-opaque areas in OPG. After clinical and radiographic investigations POF, peripheral giant cell granuloma (PGCG) and pyogenic granuloma (PG) (longstanding) were considered in differential diagnosis.
Figure 1.

The clinical presentation of intraoral mass
Figure 2.
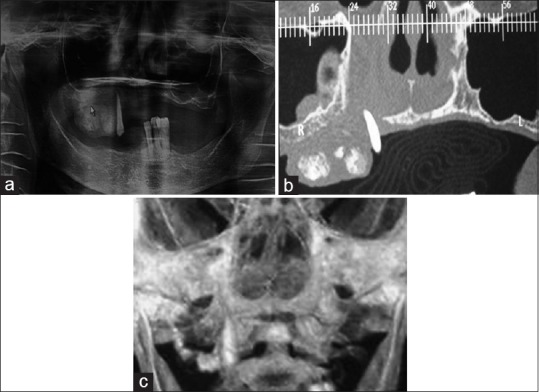
(a) Orthopantomogram showing the extension of mass. (b) Dento-alveolar scan showing the extension of lesion and inflamed maxillary sinus lining. (c) Three-dimensional construction showing calcifications within the mass
A comprehensive explanation was given to the patient and sign was taken on the consent form. Excisional biopsy was carried out, and the tissue was sent for histopathological examination for confirmatory diagnosis. Macroscopically, the gross specimen was measuring 3.5 cm × 2 cm × 1 cm, creamish brown in color, firm to hard in consistency with lobulated, and pebbly surface. The specimen was cut into two halves, and most representative areas were taken for processing [Figure 3].
Figure 3.

The complete gross specimen
The specimen was fixed in phosphate-buffered neutral formalin for 1 day, subsequently, five-micron paraffin sections were obtained and stained with hematoxylin and eosin (H and E). Microscopic analysis of the H and E section showed parakeratinized stratified squamous epithelium covering loosely arranged highly cellular connective tissue stroma [Figure 4a]. Connective tissue stroma shows few areas of ossification [Figure 4b]. Few vascular spaces of varied sizes and inflammatory infiltrate were also seen in underlying connective tissue. Based on these histologic features, the final diagnosis was given as POF.
Figure 4.

(a) Photomicrography showing parakeratinized stratified squamous epithelium covering loosely arranged highly cellular connective tissue stroma. (b) Photomicrography showing ossification in connective tissue stroma
DISCUSSION
Gingival overgrowths are one of the common lesions encountered in day to day practice. POF is a gingival lesion. Although Menzel described it first in 1872, Montgomery coined the term ossifying fibroma.[6] There are two types of ossifying fibroma, central, and peripheral. POF is clinically present as a soft nodular mass which may be either pedunculated or sessile present near the interdental papilla.[7] There are not any radiographic changes. Clinically, it is indistinguishable from PGCG, irritational fibroma, PG.
POF histopathologically is described as a lesion which has a fibrous stroma in which there is presence of mineralized tissues such as bone and/or cementum-like. The one which predominates gives the term as either “Ossifying or Cementifying.” There can be a mixture of both “Cemento-Ossifying.” However, this term is discarded as clinical and histopathological presentation is the same in those cases where there is no cementum.[8] The mineralized material may be lamellar or woven bone. These can be in any combination with cementum. There are no giant cells reported. Some authors have reported the presence of odontogenic epithelium and also that the proliferating cells may be of myofibroblastic origin.[9]
It is most commonly seen in the mandibular region anterior to the molar. It is very rare to see POF in the maxillary arch. It is seen to affect females and in the second decade of life.
Its etiopathogenesis is still debated. Some researchers feel that it represents that some kind of chronic irritation is responsible for stimulation of cells in the periodontal ligament. These cells ultimately lead to the formation of bone by metaplasia. Others believe that POF is just a continuation or extension of PG. It merely represents a matured form of PG.[10]
The treatment of choice remains surgical excision. There are very few cases to be reported as having a recurrence.[11] The purpose of reporting this case was to give a brief review to the surgeon that there can be a number of lesions presenting with the same picture but have varying histopathological presentation. It is always better to be aware of the fact and plan the surgery accordingly.
CONCLUSION
POFs are lesions with a common clinical presentation but distinct histopathological picture. POFs are common in the mandibular region and in the second decade of life usually. Irrespective of the type of mineralized component, the treatment of choice is surgical excision and there are very few cases of recurrence reported.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Barot VJ, Chandran S, Vishnoi SL. Peripheral ossifying fibroma: A case report. J Indian Soc Periodontol. 2013;17:819–22. doi: 10.4103/0972-124X.124533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mishra AK, Maru R, Dhodapkar SV, Jaiswal G, Kumar R, Punjabi H. Peripheral cemento-ossifying fibroma: A case report with review of literature. World J Clin Cases. 2013;1:128–33. doi: 10.12998/wjcc.v1.i3.128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Akkara F, Chalakkal P, Boyapati CM, Pavaskar R. Peripheral ossifying fibroma secondary to pulpo-periodontal irritation. J Clin Diagn Res. 2013;7:2076–7. doi: 10.7860/JCDR/2013/6009.3410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eversole LR, Leider AS, Nelson K. Ossifying fibroma: A clinicopathologic study of sixty-four cases. Oral Surg Oral Med Oral Pathol. 1985;60:505–11. doi: 10.1016/0030-4220(85)90239-7. [DOI] [PubMed] [Google Scholar]
- 5.Jung SL, Choi KH, Park YH, Song HC, Kwon MS. Cemento-ossifying fibroma presenting as a mass of the parapharyngeal and masticator space. AJNR Am J Neuroradiol. 1999;20:1744–6. [PMC free article] [PubMed] [Google Scholar]
- 6.Sujatha G, Sivakumar G, Muruganandhan J, Selvakumar J, Ramasamy M. Peripheral ossifying fibroma – Report of a case. Indian J Multidiscip Dent. 2012;2:415–8. [Google Scholar]
- 7.Bhasin M, Bhasin V, Bhasin A. Peripheral ossifying fibroma. Case Rep Dent. 2013;2013:497234. doi: 10.1155/2013/497234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Verma E, Chakki AB, Nagaral SC, Ganji KK. Peripheral cemento-ossifying fibroma: Case series literature review. Case Rep Dent. 2013;2013:930870. doi: 10.1155/2013/930870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.García de Marcos JA, García de Marcos MJ, Arroyo Rodríguez S, Chiarri Rodrigo J, Poblet E. Peripheral ossifying fibroma: A clinical and immunohistochemical study of four cases. J Oral Sci. 2010;52:95–9. doi: 10.2334/josnusd.52.95. [DOI] [PubMed] [Google Scholar]
- 10.Dahiya P, Kamal R, Saini G, Agarwal S. Peripheral ossifying fibroma. J Nat Sci Biol Med. 2012;3:94–6. doi: 10.4103/0976-9668.95983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sah K, Kale AD, Hallikerimath S, Chandra S. Peripheral cemento-ossifying fibroma: Report of a recurrence case. Contemp Clin Dent. 2012;3(Suppl 1):S23–5. doi: 10.4103/0976-237X.95098. [DOI] [PMC free article] [PubMed] [Google Scholar]


