Abstract
Purpose
We used a clinical next-generation sequencing hotspot mutation panel to investigate clonal evolution in paired primary and metastatic tumors.
Experimental Design
A total of 265 primary and metastatic tumor pairs were sequenced using a 46-gene cancer mutation panel capable of detecting one or more single nucleotide variants as well as small insertions/deletions. Mutations were tabulated together with tumor type and percentage, mutational variant frequency, time interval between onset of primary tumor and metastasis, and neoadjuvant therapy status.
Results
227 of 265 (85.7%) tumor-metastasis pairs showed identical mutation calls. Of the tumor pairs with identical mutation calls, 160 (60.4%) possessed defining somatic mutation signatures and 67 (25.3%) did not exhibit any somatic mutations. There were 38 (14.3%) cases that showed at least one novel mutation call between the primary and metastasis. Metastases were almost two times more likely to show novel mutations (n=20, 7.5%) than primary tumors (n=12, 4.5%). TP53 was the most common additionally mutated gene in metastatic lesions, followed by PIK3CA and SMAD4. PIK3CA mutations were more often associated with metastasis in colon carcinoma samples.
Conclusions
Clinical next-generation sequencing hotspot panels can be useful in analyzing clonal evolution within tumors as well as in determining subclonal mutations that can expand in future metastases. PIK3CA, SMAD4 and TP53 are most often involved in clonal divergence, providing potential targets that may help guide the clinical management of tumor progression or metastases.
Keywords: Next-generation sequencing, hotspot mutation panel, primary, metastasis, clonal evolution
Introduction
Cancer is a disease caused by the accumulation of genetic alterations that facilitate dysregulated cell growth and the evasion of cell death (1, 2). It is also believed that genomic alterations allow for the development of clones that acquire the potential to metastasize. Studies employing genomic techniques such as array comparative genomic hybridization, loss of heterozygosity studies, and traditional Sanger sequencing have shown that mutations accumulate over the lifetime of a tumor, that tumors can exhibit intra-tumoral heterogeneity, and that heterogeneity may allow for the selection of tumor subclones that facilitate growth and metastasis (2–13).
Although much information has been gathered through the use of traditional genomic techniques, next-generation sequencing (NGS) approaches have the potential to facilitate identification of or tracking of clonal evolution within tumors. Advantages of NGS methods that can be leveraged to determine intratumoral heterogeneity and concordances between a primary tumor and its metastasis include: the ability to successfully sequence genetic material from nanogram quantities of DNA (including poorer quality DNA), and the ability of NGS to sequence DNA at a much higher sensitivity than Sanger sequencing, allowing for the examination of rare and uncommon subclones within a tumor. To date, studies on clonal evolution using NGS techniques have looked at relatively small numbers of patients with a high depth of sequencing (14, 15).
In this study, we collected 265 tumor primary and metastasis pairs and analyzed these cases for hotspot mutations in 46 well-known cancer-related genes using a targeted NGS assay in routine clinical usage. This study had two goals: 1) to determine the concordance rate of mutations between primary tumors and their paired metastases; and 2) to characterize the types of mutations found in concordant versus clonally divergent/evolved primary and metastatic tumor pairs.
Materials and Methods
All samples included in this study were obtained in accordance with the Declaration of Helsinki from patients with appropriate informed consent and with approval from the institutional review board. A total of 265 primary tumor and metastasis pairs were analyzed using the AmpliSeq™ Cancer Panel, version 1 run on the Ion Torrent Personal Genome Machine™ for NGS (Life Technologies, Guilford, CT). All of the tumors in this study were solid tumors, mainly carcinomas, but also melanomas and sarcomas. Our laboratory has had extensive experience with this form of high-throughput sequencing (16), and has been using this technique to obtain NGS data for clinical samples for over a year.
Briefly, 4 μm sections were obtained from each tumor block. One hematoxylin and eosin-stained slide was examined by a pathologist to estimate tumor percentage and to outline the areas of the slide for microdissection. Only tumors with >20% tumor in the identified area were qualified for sequencing. DNA was extracted and purified after microdissection using the AMPure kit (Agencourt Biosciences, Beverly, MA). DNA was then fragmented, ligated to adapters, barcoded, and clonally amplified onto beads to create a sequencing library (17), using the Ion Torrent AmpliSeq kit 2.0, the Ion Xpress Barcode Adapters Kits, and the AmpliSeq Cancer Panel primer pool (Life Technologies), following the manufacturer’s instructions. Libraries were pooled and amplified onto IonSpheres using emulsion polymerase chain reaction through the Ion Torrent OneTouch template kit, and enriched on the Ion Torrent OneTouch System following the manufacturer’s protocol. The enriched IonSpheres were collected onto a 318 IonChip to sequence the pooled libraries from 8 samples and the cell line control. Sequencing success was characterized by the presence of at least 300,000 reads per sample and less than one misaligned base per 100 bases (16).
Signal processing, base calling, alignment, and variant calling was carried out using TorrentSuite version 2.0 (Life Technologies). Manual review of alignments was performed using the Integrative Genomics Viewer (Broad Institute, Boston, MA) (16). A minimum coverage depth of 250 reads and a minimal variant frequency of 5% were designated as mutations. Minimal variant frequencies of ≥2% were considered to be mutations if the same mutation was seen at ≥5% in the corresponding paired tumor. In addition, custom-built software previously described was used to review the variant call data files in order to inspect the alignments and mutations detected, to filter errors generated in sequencing homopolymer repeat regions, and to annotate the results (16). Paired primary and metastatic tumors were analyzed using the Comparison Viewer mode of this software to examine concordant and discordant mutations for each tumor-metastasis pair. Mutations for each pair were tabulated together with tumor percentage, mutational allelic frequency, time interval between onset of primary tumor and metastasis, and the presence or absence of neoadjuvant therapy. Calls were considered fully concordant if all mutations found in the paired primary and metastatic tumors were identical. The remaining cases were classified as clonally divergent/evolved. Single nucleotide polymorphism analysis was used to confirm that samples from primary and metastatic lesions originated from the same germline material (Supplemental Table 1).
Statistical analysis was performed on the breast and colon carcinomas (the most common tumor types) within this subset to determine if mutations were more common in certain genes between primaries and their paired metastases. Fisher’s exact test was used to test the null hypothesis of no difference in the mutation frequencies of genes in primary versus metastatic tumor. Holm’s method was used to correct for multiple gene comparisons.
Results
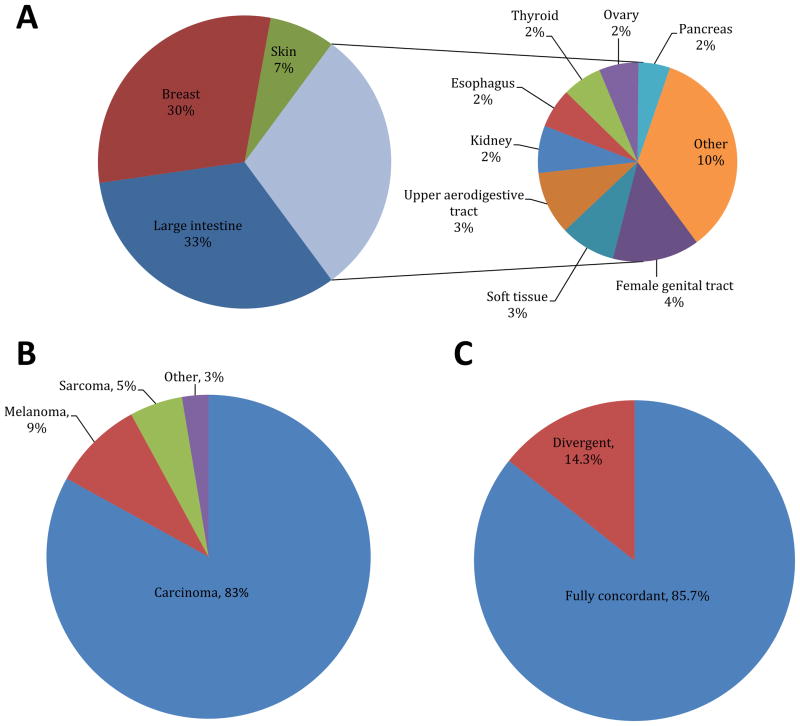
Two hundred and sixty-five primary-metastasis tumor pairs were analyzed including 86 (32.5%) colorectal carcinomas, 79 (29.8%) breast carcinomas, 20 (7.5%) melanomas, and 80 (30.2%) various other tumor sites (Figure 1A). Accordingly, most tumors were carcinomas (83%), followed by melanomas (9%) and sarcomas (5.3%) (Figure 1B). Of the 265 tumor primary-metastasis pairs studied, 227 (85.7%) pairs showed identical mutation calls, including 160 (60.4%) with defining mutation signatures, and 67 (25.3%) without any somatic mutations identified (Figure 1C; subset of identical mutation call cases are detailed in Supplemental Table 2). The remaining 38 (14.3%) tumor primary-metastasis pairs had discordant mutation calls, and were considered to be clonally divergent/evolved tumors (Figure 1C; Table 1). The time interval between primary tumor sampling and paired metastatic tumor sampling was highly variable, but not significantly different between the concordant and divergent groups (concordant group 25±30 months, divergent 22±32 months). The percentage of neoplastic cells was indistinguishable between primary (61.3%±20%) and metastatic tumor samples (62.3%±20.5%), and showed a similar range in the samples that showed no mutations (60.7%±22.3%). The most common tumors with no mutations were carcinomas (76.5%), sarcomas (11.8%), and melanomas (4.4%), which represents a relative enrichment in sarcomas compared to the overall distribution of histologies. No identifiable trend between tumor histology and concordance rate was noted.
Figure 1.
Summary of initial tumor sites (A) and histologies (B) for primary/metastatic tumor pairs analyzed. (C) Summary of the frequencies of concordant and divergent mutations between paired primary and metastasis samples within our cohort of 265 cases.
Table 1.
List of divergent mutations between primary and metastatic tumors indicating possible clonal evolution. Novel mutations between tumor pairs are highlighted in bold.
| Site of novel mutations | Primary site | Mutations in primary | Mutations in metastasis |
|---|---|---|---|
| Metastasis | Breast | PIK3CA:c.1633G>A p.E545K |
PIK3CA:c.1633G>A p.E545K TP53:c.853G>A p.E285K |
| Breast | PTEN:c.733C>T p.Q245* | ||
| Breast | HRAS:c.34G>A p.G12S |
HRAS:c.34G>Ap.G12S SMAD4:c.1553T>C p.I518T |
|
| Breast | PIK3CA:c.1633G>A p.E545K |
PIK3CA:c.1633G>A p.E545K PTPN11:c.173A>G p.N58S |
|
| Breast | TP53:c.839G>T p.R280I | ||
| Breast | KRAS:c.34G>C p.G12R | ||
| Breast | KRAS:c.35G>T p.G12V | ||
| Breast | PIK3CA:c.278G>C p.R93P | ||
| Colon |
PIK3CA:c.1624G>A p.E542K KRAS:c.35G>T p.G12V |
PIK3CA:c.1624G>A p.E542K KRAS:c.35G>T p.G12V SMAD4:c.1081C>A p.R361S |
|
| Colon | PIK3CA:c.1624G>A p.E542K | ||
| Colon |
APC:c.3340C>T p.R1114* TP53:c.742C>T p.R248W PIK3CA:c.3140A>Gp.H1047R KRAS:c.436G>A p.A146T |
APC:c.3340C>T p.R1114* TP53:c.742C>T p.R248W PIK3CA:c.3140A>G p.H1047R KRAS:c.436G>A p.A146T PIK3CA:c.1030G>A p.V344M APC:c.4348C>T p.R1450* |
|
| Colon |
TP53:c.818G>A p.R273H KRAS:c.38G>A p.G13D |
TP53:c.818G>A p.R273H KRAS:c.38G>A p.G13D PIK3CA:c.1638G>T p.Q546H |
|
| Colon | KRAS:c.35G>A p.G12D |
KRAS:c.35G>A p.G12D TP53:c.844C>T p.R282W PIK3CA:c.1633G>A p.E545K |
|
| Colon | TP53:c.809T>C p.F270S |
TP53:c.809T>C p.F270S NRAS:c.183A>C p.Q61H |
|
| Gastric | APC:c.4396G>T p.G1466* | ||
| Lung | FBXW7:c.1436G>A p.R479Q | ||
| Melanoma |
CDKN2A:c.158_159delp.M53fs NRAS:c.181C>A p.Q61K |
CDKN2A:c.158_159del p.M53fs NRAS:c.181C>A p.Q61K CTNNB1:c.133T>C p.S45P |
|
| Renal cell | TP53:c.742C>T p.R248W | ||
| Renal cell | TP53:c.581T>G p.L194R | ||
| Sarcoma | FBXW7:c.1698G>A p.W566* | ||
| Primary | Breast | TP53:c.602T>A p.L201* | |
| Breast |
TP53:c.526T>Ap.C176S TP53:c.581T>G p.L194R |
TP53:c.526T>A p.C176S | |
| Breast | PIK3CA:c.1624G>A p.E542K | ||
| Breast |
TP53:c.722C>A p.S241Y ABL1:c.844G>C p.E282Q PIK3CA:c.1633G>A p.E545K PTEN:c.511C>T p.Q171* |
TP53:c.722C>A p.S241Y ABL1:c.844G>C p.E282Q PIK3CA:c.1633G>A p.E545K |
|
| Colon |
KRAS:c.35G>A p.G12D FBXW7:c.1375G>A p.G459R APC:c.2626C>T p.R876* |
KRAS:c.35G>A p.G12D FBXW7:c.1375G>A p.G459R |
|
| Colon |
APC:c.4495G>T p.G1499* NRAS:c.35G>T p.G12V PIK3CA:c.1637A>G p.Q546R TP53:c.581T>A p.L194H |
APC:c.4495G>T p.G1499* NRAS:c.35G>T p.G12V PIK3CA:c.1637A>G p.Q546R |
|
| Colon |
APC:c.3883G>T p.E1295* TP53:c.817C>T p.R273C SMAD4:c.1082G>A p.R361H |
APC:c.3883G>T p.E1295* TP53:c.817C>T p.R273C |
|
| Colon |
TP53:c.527G>A p.C176Y KRAS:c.38G>A p.G13D SMAD4:c.1529G>T p.G510V |
TP53:c.527G>A p.C176Y KRAS:c.38G>A p.G13D |
|
| Melanoma |
MLH1:c.1151T>A p.V384D NRAS:c.182A>G p.Q61R KIT:c.1621A>C p.M541L |
MLH1:c.1151T>A p.V384D NRAS:c.182A>G p.Q61R |
|
| Melanoma |
BRAF:c.1406G>A p.G469E KRAS:c.40G>A p.V14I |
BRAF:c.1406G>A p.G469E | |
| Sarcoma | TP53:c.535C>A p.H179N | ||
| Thyroid |
BRAF:c.1799T>A p.V600E AKT1:c.49G>A p.E17K |
BRAF:c.1799T>A p.V600E | |
| Both | Small intestine |
TP53:c.856G>A p.E286K ERBB2:c.2524G>A p.V842I |
TP53:c.856G>A p.E286K ERBB4:c.2817G>T p.L939F SMAD4:c.380G>T p.C127F KRAS:c.35G>A p.G12D |
| Breast | TP53:c.626_627del p.R209fs | TP53:c.524G>A p.R175H | |
| Colon |
KRAS:c.35G>T p.G12V TP53:c.273G>A p.W91* |
KRAS:c.35G>T p.G12V TP53:c.725G>A p.C242Y PIK3CA:c.3140A>G p.H1047R |
|
| Colon |
PIK3CA:c.263G>A p.R88Q KRAS:c.38G>A p.G13D |
PIK3CA:c.263G>A p.R88Q GNAS:c.602G>A p.R201H |
|
| Colon |
APC:c.3927_3931delp.E1309fs KRAS:c.35G>T p.G12V |
APC:c.3927_3931delp.E1309fs PIK3CA:c.263G>A p.R88Q |
|
| Sarcoma |
TP53:c.818G>A p.R273H CSF1R:c.950A>G p.E317G |
TP53:c.844C>T p.R282W TP53:c.871A>G p.K291E CSF1R:c.923A>G p.N308S |
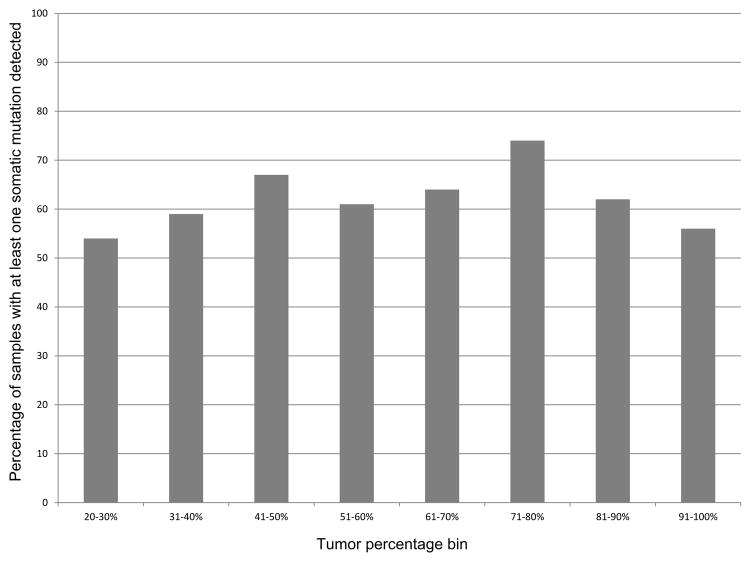
A subset of primary and paired metastatic tumor cases that were concordant showed no identifiable somatic mutations, which could potentially represent true negatives (no mutations present in the assessed genes/codons) or false negative findings due to preanalytic factors such as a low tumor percentage. If low tumor percentage in samples resulted in false negative mutation findings, a lower mutation detection rate would be expected at lower tumor percentages. However, no significant relationship between mutation detection rate and tumor percentage was identified (Figure 2).
Figure 2.
Independence of sample tumor percentage and mutation detection rate. Tumors were defined into bins based on estimated tumor percentage (all tumors had a minimum tumor percentage of 20%). Mutation detection was treated as a binary variable with positivity defined by the presence of at least one presumed somatic mutation in the sample. No statistically significant difference between any tumor percentage bins was identified (Student’s t-test).
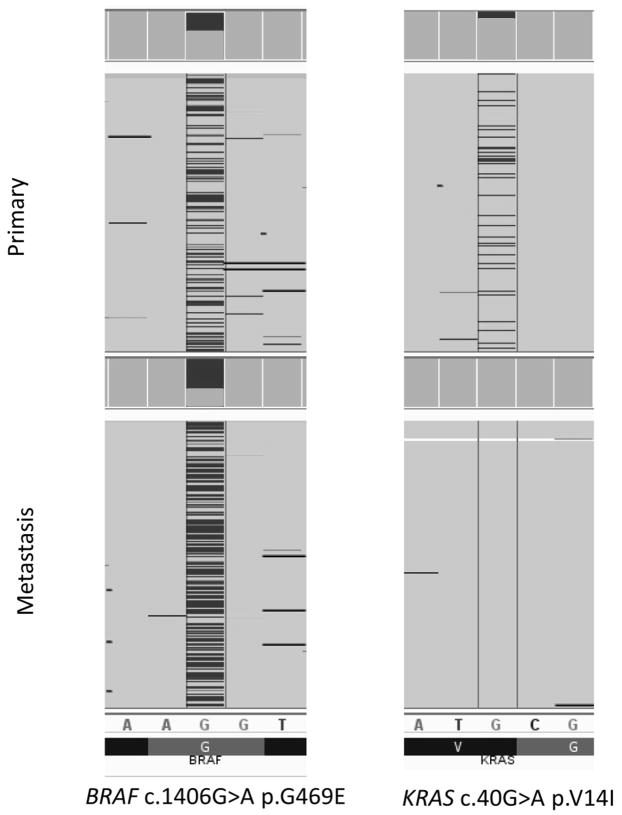
Clonal Evolution
An example of clonal evolution is shown in Figure 3, and all novel mutations associated with primary/metastasis discordance are detailed in Table 1. As might be predicted, metastases more commonly showed novel mutations than primary tumors within the paired samples. Within the 38 primary-metastasis pairs demonstrating novel calls between the primary and the metastatic tumor, in 20 (7.5%) primary-metastasis pairs the metastasis had novel mutations not found in the primary tumor. In contrast, in 12 (4.5%) primary-metastasis pairs the primary tumors had novel mutations not identified in the metastatic tumor. The time interval between obtaining biopsy specimens from the primary and metastatic tumor was widely divergent, ranging from 0 to 79.1 months. Five primary-metastasis pairs showed novel mutations in both the primary tumor and the metastatic lesion, most commonly distinct TP53 mutations (3 of 5 pairs). The time interval between obtaining biopsy specimens from the primary and metastatic tumors in these 3 patients ranged from 12.3 to 79.1 months. These findings are at least partly in keeping with the paradigm that mutations accumulate within a tumor over time and that metastatic clones diverge from the primary tumor. Because this study focused on primary-metastasis pairs and not on multiple sites within a contiguous primary tumor, we cannot differentiate clonal evolution as a function of metastasis from intratumoral clonal evolution or intratumoral heterogeneity. Nonetheless, the presence of mutations found in the primary tumor but not seen in the metastatic tumor suggest that there may be clonal divergence within the tumor, with the metastasis branching off from the primary tumor, at an earlier point in time prior to the accumulation of new mutations within the primary tumor.
Figure 3.
Clonal evolution in solid tumors. Here, the primary and metastasis both share the same BRAF mutation, but vary in their mutational status at the KRAS locus. The presence of the KRAS mutation in the primary but not in the paired metastasis, suggests that the primary and metastasis both evolved from a common progenitor that possessed the BRAF mutation shared by both tumors, but that the metastasis and primary branched off from one another prior to the primary acquiring a KRAS mutation. This case provides evidence for branched evolution in carcinogenesis.
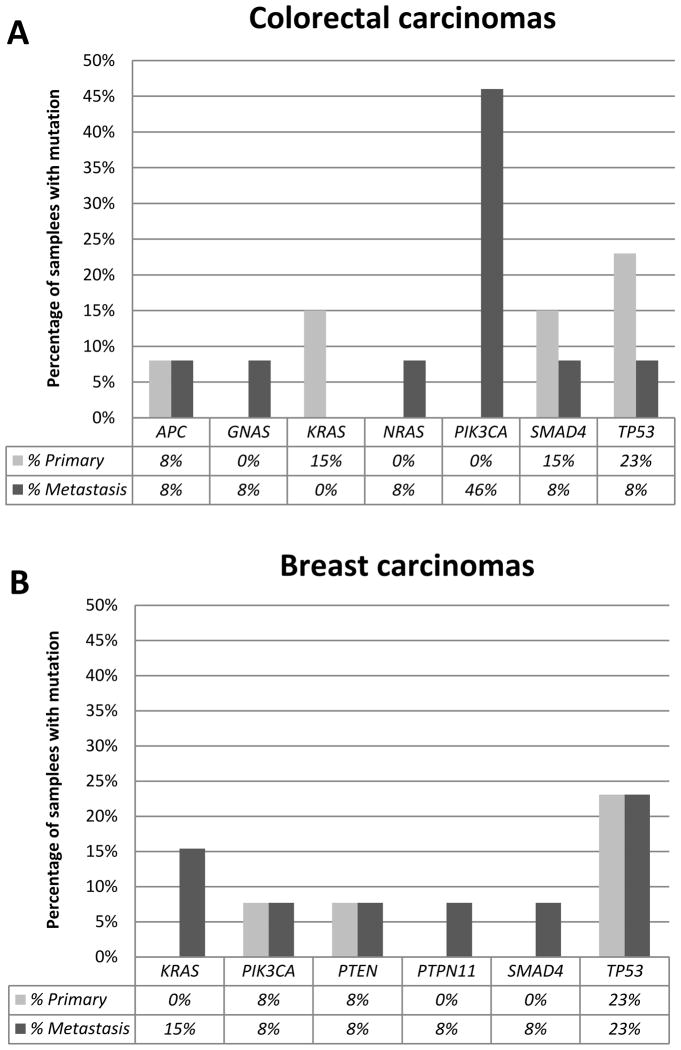
Mutations associated with clonal divergence were found more commonly in certain genes within the hotspot mutation panel. Novel mutations between the primary and metastatic tumor were found in 16 of 46 genes on the panel including AKT1, APC, CSF1R, CTNNB1, ERBB2, ERBB4, FBXW7, GNAS, KIT, KRAS, NRAS, PIK3CA, PTEN, PTPN11, SMAD4, and TP53. TP53 was the most commonly additionally mutated gene (15 mutations), followed by PIK3CA (8 mutations), and SMAD4 (5 mutations). In this tumor set, PIK3CA mutations showed a trend toward association with metastasis in colon carcinoma samples: almost half of colorectal carcinoma pairs with clonal divergence showed a PIK3CA mutation in the metastasis, but not in the primary neoplasm. In contrast, PIK3CA mutations in breast carcinomas were almost equally identified in primary and metastatic tumors (Figure 4). Although our overall numbers in this subgroup are small and did not reach statistical significance (p=0.011 before Holm’s correction, p=0.1 after correction), the trend toward predominance of PIK3CA mutations in metastatic colorectal carcinoma suggests that these mutations may lend a selection or growth advantage to subclones within the tumor leading to metastasis. This finding may have clinical implications should PIK3CA inhibitors have an impact on progression-free or overall survival in colorectal carcinoma patients. The use of aspirin within our colorectal carcinoma group could not be obtained and may be an avenue of further study as aspirin has shown to have survival benefits in patients with PIK3CA-mutated colorectal carcinoma (18).
Figure 4.
Frequency of mutations by gene in the subset of paired primary and metastatic tumors exhibiting clonal divergence. A) Colorectal carcinomas (n=13) B) Breast carcinomas (n=13).
Discussion
The traditional concept of tumor metastasis is that tumor cells undergo clonal evolution by acquiring a number of genetic and epigenetic events that facilitate a sequence of steps that further lymphovascular invasion and colonization at metastatic sites (19–21). This view suggests that metastases may possess mutations differing from the primary tumor since these mutations confer selective growth or invasion advantage to the metastatic tumor cells that are not necessary for primary tumor survival (14, 21). Recent genomic studies are demonstrating that this view of metastasis may need to be amended as it appears that the pattern of mutations between primary and metastatic tumors, and within multiple areas of a single primary lesion, is that of branched evolution – where both divergence and independent convergence may happen synchronously in multiple subclonal populations (15). With the advent of more efficient and sensitive sequencing methods, such as NGS, subclonal analysis of primary and metastatic tumors suggest that that several clones of similar genetic fitness can develop simultaneously (15, 22).
Our findings are in keeping with earlier studies indicating that most mutations between paired primary and metastatic tumor are predominantly concordant (14). In this study, almost 86% of primary-metastasis pairs were concordant between the primary and metastatic components, including almost two-thirds of cases with at least one mutation. Our results also show that mutations accumulate over time and are more common in the metastatic tumor, with 21 novel mutations seen in metastases compared with paired primary tumors. However, a subset of paired primary-metastatic tumors in this study had novel mutations only in the primary tumor (n=12) or novel mutations in both the paired primary and metastatic tumors (n=6) suggesting that branched clonal evolution occurs within a variety of tumors. In this cohort of cases, novel mutations identified in the primary rather than the paired metastatic tumor were observed in breast, colon, and thyroid carcinomas, melanoma, and sarcoma. Novel mutations present only in the primary tumor suggest that the metastases branched off prior to the acquisition of novel mutations within the primary tumor. It is important to note that a formal alternative explanation for these findings includes the presence or development of intratumoral heterogeneity. Such heterogeneity as a cause of the branched evolution seen in this study between primary and metastatic lesions cannot be entirely excluded without a more extensive analysis involving sequencing of multiple physical locations within primary and metastatic lesions, or single cell sequencing studies. Such studies are particularly challenging to contemplate in human metastatic tumor material, as it is rare that anything other than narrow gauge core biopsy material would be available for clinical testing.
Our study also highlights certain mutations that are often associated with clonal divergence. In agreement with other studies (23), TP53 mutations were common in this sample cohort, and frequently seen as a divergence between primary and metastatic lesions. Loss of a TP53 mutation in a metastasis – or a mutation in any tumor suppressor gene – may reflect loss of heterozygosity or copy number loss as an alternative inactivating mechanism. TP53 is a known tumor suppressor gene with roles in maintenance of genomic stability and regulation of apoptosis. Mutations in TP53 can disrupt metabolic functions leading to metastasis by enhancing anchorage-independent growth (24). In addition, recruitment of mutant TP53 to sites of DNA damage can lead to expression of genes that participate in regulation of proliferation and chemoresistance (24). Mutant TP53 has also been shown to deregulate expression of SHARP1, CCNG2, DICER and DEPDC1 which all play roles in invasion and metastasis (24). Given the involvement of mutant TP53 in proliferation, resistance mechanisms and metastasis, it is understandable that TP53 mutations are most often associated with clonal divergence.
Other common mutations involved in clonal divergence in this study included PIK3CA and SMAD4 (25). PIK3CA encodes for a cell signaling lipid kinase within a group of lipid kinases involved in cell proliferation, cellular adhesion, survival and motility (26). Activating PIK3CA mutations have been discovered in a variety of tumors and have been found to promote growth-factor-independent growth, cell invasion and metastasis through activation of AKT signaling (26). These cases could potentially be targeted by PIK3CA inhibitors, thus justifying the use of NGS for identification of relevant mutations. Recent studies have shown that aspirin may have survival benefits in PIK3CA-mutated colorectal carcinoma (18, 27). Since these survival benefits are not seen with specific COX-2 inhibitors, these data may highlight the importance of a COX-independent effect of aspirin in the prevention of cancer spread (27, 28). It is unclear what effect aspirin will have on patients that develop PIK3CA mutations within their metastases. In addition, we were not able to obtain the presence and/or duration of aspirin use in our patient population. A further large-scale study on this subset of patients may be warranted.
Loss of SMAD4 activity has been associated with lymph node metastases, advanced stage disease and shortened overall survival in patients with colorectal cancer (29, 30). Murine in vivo studies have shown that SMAD4 loss increases the metastatic potential of colorectal cancer through TGF-β signaling (29, 31).
In summary, this study is the largest comparison of paired primary and metastatic tumors assessed by NGS mutational hotspot analysis. We show that there is a high rate of concordance for mutation profiling between paired primary and metastatic tumors. Although our study did not involve whole genome or whole exome sequencing, the hotspot mutation panel we used was able to demonstrate clonal evolution between paired primary and metastatic tumors, including the presence of branched clonal evolution in a small subset (6%) of paired primary-metastatic tumors. As hotspot based mutation panels are rapidly converging on clinical standard of care testing for neoplasms such as lung and colorectal carcinoma and melanoma, we believe that the finding of heterogeneity in a subset of primary/metastasis pairs using these methods represents an important take-home message for clinical testing and consideration of targeted therapies. The trend toward secondary, divergent PIK3CA mutations in colorectal carcinoma metastases may warrant additional study with a larger cohort focused on colorectal adenocarcinomas. Overall, TP53, PIK3CA, and SMAD4 mutations were most often involved in clonal divergence, providing potential targets for directed therapies in progressive disease.
Supplementary Material
Statement of Translational Relevance.
It is believed that cancer evades our attempts to halt its growth through acquisition of genetic and epigenetic events, a concept known as clonal evolution, that facilitates lymphovascular invasion and colonization at metastatic sites. The advent of next-generation sequencing (NGS) technologies allows us to examine this phenomenon at the mutational level. This study is the largest clinical study to date, using an NGS hotspot mutation panel to examine clonal evolution in paired primary and metastatic solid tumor tissues. Similar to whole exome sequencing studies, the data demonstrate that a high percentage (86%) of paired tumors share the same mutational profile. However, there is still a sizeable proportion of samples (14%) with divergent mutational profiles, suggesting that sequencing of both primary and metastatic tumors is warranted. Of note, divergent PIK3CA mutations were most often found in colon carcinomas, implicating them in the metastatic process and advocating future avenues of study.
Acknowledgments
FINANCIAL SUPPORT: This work was supported in part by the Sheikh Khalifa Al Nahyan Ben Zayed Institute for Personalized Cancer Therapy, NCATS grant UL1 TR000371 (Center for Clinical and Translational Sciences), and the MD Anderson Cancer Center Support grant (P30 CA016672). RSG is supported by a Post-Doctoral Fellowship Award through the Canadian Institutes of Health Research (www.cihr-irsc.gc.ca).
Footnotes
PRIOR PRESENTATIONS AND CONFLICTS: Aspects of this study have previously been presented in abstract form at the United States & Canadian Association of Pathology Annual Meeting 2014. This manuscript describes original work and is not under consideration by any other journal. All authors approved the manuscript and this submission, and have no conflicts of interest.
References
- 1.Fearon ER, Vogelstein B. A genetic model for colorectal tumorigenesis. Cell. 1990;61:759–67. doi: 10.1016/0092-8674(90)90186-i. [DOI] [PubMed] [Google Scholar]
- 2.Brosnan JA, Iacobuzio-Donahue CA. A new branch on the tree: next-generation sequencing in the study of cancer evolution. Semin Cell Dev Biol. 2012;23:237–42. doi: 10.1016/j.semcdb.2011.12.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Poste G, Tzeng J, Doll J, Greig R, Rieman D, Zeidman I. Evolution of tumor cell heterogeneity during progressive growth of individual lung metastases. Proc Natl Acad Sci U S A. 1982;79:6574–8. doi: 10.1073/pnas.79.21.6574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Talmadge JE, Wolman SR, Fidler IJ. Evidence for the clonal origin of spontaneous metastases. Science. 1982;217:361–3. doi: 10.1126/science.6953592. [DOI] [PubMed] [Google Scholar]
- 5.Armengol G, Capella G, Farre L, Peinado MA, Miro R, Caballin MR. Genetic evolution in the metastatic progression of human pancreatic cancer studied by CGH. Lab Invest. 2001;81:1703–7. doi: 10.1038/labinvest.3780383. [DOI] [PubMed] [Google Scholar]
- 6.Jiang JK, Chen YJ, Lin CH, Yu IT, Lin JK. Genetic changes and clonality relationship between primary colorectal cancers and their pulmonary metastases--an analysis by comparative genomic hybridization. Genes Chromosomes Cancer. 2005;43:25–36. doi: 10.1002/gcc.20167. [DOI] [PubMed] [Google Scholar]
- 7.Schmidt-Kittler O, Ragg T, Daskalakis A, Granzow M, Ahr A, Blankenstein TJ, et al. From latent disseminated cells to overt metastasis: genetic analysis of systemic breast cancer progression. Proc Natl Acad Sci U S A. 2003;100:7737–42. doi: 10.1073/pnas.1331931100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Micci F, Haugom L, Ahlquist T, Abeler VM, Trope CG, Lothe RA, et al. Tumor spreading to the contralateral ovary in bilateral ovarian carcinoma is a late event in clonal evolution. J Oncol. 2010;2010:646340. doi: 10.1155/2010/646340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Harbst K, Staaf J, Masback A, Olsson H, Ingvar C, Vallon-Christersson J, et al. Multiple metastases from cutaneous malignant melanoma patients may display heterogeneous genomic and epigenomic patterns. Melanoma Res. 2010;20:381–91. [PubMed] [Google Scholar]
- 10.Jones TD, Carr MD, Eble JN, Wang M, Lopez-Beltran A, Cheng L. Clonal origin of lymph node metastases in bladder carcinoma. Cancer. 2005;104:1901–10. doi: 10.1002/cncr.21466. [DOI] [PubMed] [Google Scholar]
- 11.Losi L, Baisse B, Bouzourene H, Benhattar J. Evolution of intratumoral genetic heterogeneity during colorectal cancer progression. Carcinogenesis. 2005;26:916–22. doi: 10.1093/carcin/bgi044. [DOI] [PubMed] [Google Scholar]
- 12.Jones S, Chen WD, Parmigiani G, Diehl F, Beerenwinkel N, Antal T, et al. Comparative lesion sequencing provides insights into tumor evolution. Proc Natl Acad Sci U S A. 2008;105:4283–8. doi: 10.1073/pnas.0712345105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yachida S, Jones S, Bozic I, Antal T, Leary R, Fu B, et al. Distant metastasis occurs late during the genetic evolution of pancreatic cancer. Nature. 2010;467:1114–7. doi: 10.1038/nature09515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vignot S, Frampton GM, Soria JC, Yelensky R, Commo F, Brambilla C, et al. Next-generation sequencing reveals high concordance of recurrent somatic alterations between primary tumor and metastases from patients with non-small-cell lung cancer. J Clin Oncol. 2013;31:2167–72. doi: 10.1200/JCO.2012.47.7737. [DOI] [PubMed] [Google Scholar]
- 15.Gerlinger M, Rowan AJ, Horswell S, Larkin J, Endesfelder D, Gronroos E, et al. Intratumor heterogeneity and branched evolution revealed by multiregion sequencing. N Engl J Med. 2012;366:883–92. doi: 10.1056/NEJMoa1113205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Singh RR, Patel KP, Routbort MJ, Reddy NG, Barkoh BA, Handal B, et al. Clinical validation of a next-generation sequencing screen for mutational hotspots in 46 cancer-related genes. J Mol Diagn. 2013;15:607–22. doi: 10.1016/j.jmoldx.2013.05.003. [DOI] [PubMed] [Google Scholar]
- 17.Rothberg JM, Hinz W, Rearick TM, Schultz J, Mileski W, Davey M, et al. An integrated semiconductor device enabling non-optical genome sequencing. Nature. 2011;475:348–52. doi: 10.1038/nature10242. [DOI] [PubMed] [Google Scholar]
- 18.Liao X, Lochhead P, Nishihara R, Morikawa T, Kuchiba A, Yamauchi M, et al. Aspirin use, tumor PIK3CA mutation, and colorectal-cancer survival. N Engl J Med. 2012;367:1596–606. doi: 10.1056/NEJMoa1207756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Nowell PC. The clonal evolution of tumor cell populations. Science. 1976;194:23–8. doi: 10.1126/science.959840. [DOI] [PubMed] [Google Scholar]
- 20.Ding L, Raphael BJ, Chen F, Wendl MC. Advances for studying clonal evolution in cancer. Cancer Lett. 2013;340:212–9. doi: 10.1016/j.canlet.2012.12.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vignot S, Besse B, Andre F, Spano JP, Soria JC. Discrepancies between primary tumor and metastasis: a literature review on clinically established biomarkers. Crit Rev Oncol Hematol. 2012;84:301–13. doi: 10.1016/j.critrevonc.2012.05.002. [DOI] [PubMed] [Google Scholar]
- 22.Snuderl M, Fazlollahi L, Le LP, Nitta M, Zhelyazkova BH, Davidson CJ, et al. Mosaic amplification of multiple receptor tyrosine kinase genes in glioblastoma. Cancer Cell. 2011;20:810–7. doi: 10.1016/j.ccr.2011.11.005. [DOI] [PubMed] [Google Scholar]
- 23.Vakiani E, Janakiraman M, Shen R, Sinha R, Zeng Z, Shia J, et al. Comparative genomic analysis of primary versus metastatic colorectal carcinomas. J Clin Oncol. 2012;30:2956–62. doi: 10.1200/JCO.2011.38.2994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Muller PA, Vousden KH. p53 mutations in cancer. Nature Cell Biol. 2013;15:2–8. doi: 10.1038/ncb2641. [DOI] [PubMed] [Google Scholar]
- 25.Shah SP, Roth A, Goya R, Oloumi A, Ha G, Zhao Y, et al. The clonal and mutational evolution spectrum of primary triple-negative breast cancers. Nature. 2012;486:395–9. doi: 10.1038/nature10933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ligresti G, Militello L, Steelman LS, Cavallaro A, Basile F, Nicoletti F, et al. PIK3CA mutations in human solid tumors: role in sensitivity to various therapeutic approaches. Cell Cycle. 2009;8:1352–8. doi: 10.4161/cc.8.9.8255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Domingo E, Church DN, Sieber O, Ramamoorthy R, Yanagisawa Y, Johnstone E, et al. Evaluation of PIK3CA mutation as a predictor of benefit from nonsteroidal anti-inflammatory drug therapy in colorectal cancer. J Clin Oncol. 2013;31:4297–305. doi: 10.1200/JCO.2013.50.0322. [DOI] [PubMed] [Google Scholar]
- 28.Cathomas G. PIK3CA in Colorectal Cancer. Front Oncol. 2014;4:35. doi: 10.3389/fonc.2014.00035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kin C, Kidess E, Poultsides GA, Visser BC, Jeffrey SS. Colorectal cancer diagnostics: biomarkers, cell-free DNA, circulating tumor cells and defining heterogeneous populations by single-cell analysis. Expert Rev Mol Diagn. 2013;13:581–99. doi: 10.1586/14737159.2013.811896. [DOI] [PubMed] [Google Scholar]
- 30.Xie W, Rimm DL, Lin Y, Shih WJ, Reiss M. Loss of Smad signaling in human colorectal cancer is associated with advanced disease and poor prognosis. Cancer J. 2003;9:302–12. doi: 10.1097/00130404-200307000-00013. [DOI] [PubMed] [Google Scholar]
- 31.Zhang B, Halder SK, Kashikar ND, Cho YJ, Datta A, Gorden DL, et al. Antimetastatic role of Smad4 signaling in colorectal cancer. Gastroenterology. 2010;138:969–80. e1–3. doi: 10.1053/j.gastro.2009.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.