Abstract
Rationale
Stroke and vascular risk factors disproportionately affect minority populations, with Blacks and Hispanics experiencing a 2·5‐ and 2·0‐fold greater risk compared with whites, respectively. Patients with transient ischemic attacks and mild, nondisabling strokes tend to have short hospital stays, rapid discharges, and inaccurate perceptions of vascular risk.
Aim
The primary aim of the Discharge Educational Strategies for Reduction of Vascular Events (DESERVE) trial is to evaluate the efficacy of a novel community health worker‐based multilevel discharge intervention vs. standard discharge care on vascular risk reduction among racially/ethnically diverse transient ischemic attack/mild stroke patients at one‐year postdischarge. We hypothesize that those randomized to the discharge intervention will have reduced modifiable vascular risk factors as determined by systolic blood pressure compared with those receiving usual care.
Sample size estimates
Given 300 subjects per group and alpha of 0·05, the power to detect a 6 mmHg reduction in systolic blood pressure is 89%.
Design
DESERVE trial is a prospective, randomized, multicenter clinical trial of a novel discharge behavioral intervention. Patients with transient ischemic attack/mild stroke are randomized during hospitalization or emergency room visit to intervention or usual care. Intervention begins prior to discharge and continues postdischarge.
Study outcomes
The primary outcome is difference in systolic blood pressure reduction between groups at 12 months. Secondary outcomes include between‐group differences in change in glycated hemoglobin, smoking rates, medication adherence, and recurrent stroke/transient ischemic attack at 12 months.
Discussion
DESERVE will evaluate whether a novel discharge education strategy leads to improved risk factor control in a racially diverse population.
Keywords: discharge, health education, mild, stroke, TIA
Introduction and rationale
In the United States, stroke disproportionally affects minority populations 1, 2. Secondary prevention strategies in minority populations have been suboptimal due to cultural and behavioral factors not addressed in standard prevention modalities and poor integration into community resources 3, 4. Current practices, with decreased length of stay and rushed discharges, fail to reinforce the ‘warning nature’ of nondisabling transient ischemic attacks (TIAs)/mild strokes 5, 6. These practices reinforce the poor risk perception that many TIA/mild stroke patients associate with mild or resolved deficits 5, 7. Intensive, interactive, and culturally tailored discharge education strategies based on health promotion theory may improve accuracy of risk perception and promote behavior change.
Methods
Design
The Discharge Educational Strategies for Reduction of Vascular Events (DESERVE) study is a prospective, randomized, multicenter trial of a novel, patient‐paced discharge behavioral intervention. The interactive, culturally tailored intervention focuses on acquisition of three skills‐based areas: risk knowledge, medication adherence, and patient–physician communication. The primary aim is to evaluate the efficacy of the behavioral intervention vs. standard discharge care on vascular risk reduction among racially/ethnically diverse TIA/mild stroke patients at 12 months postdischarge. We hypothesize that those randomized to the discharge intervention will have lower follow‐up systolic blood pressure (SBP) compared with usual care.
Patient population
Study patients are prospectively identified through daily screening of potential TIA/stroke cases at four urban medical centers with a high percentage of African American and Hispanic patients. This process includes daily review of stroke admissions and consultations, participation in rounds, and an emergency department notification pager. Patients with stroke, TIA, or stroke‐like symptoms are screened by study neurologists to confirm eligibility. Eligible patients are approached to obtain written informed consent.
Inclusion criteria
- Presentation/transfer to enrolling site with one of the following diagnoses:
- TIA
- Ischemic stroke (IS) with National Institutes of Health Stroke Scale (NIHSS) <5 at enrollment
- Intracerebral hemorrhage (ICH) with NIHSS <5 at enrollment
Age >18 years
New York area resident with phone
- One or more vascular risk factors:
- Hyperlipidemia
- Hypertension
- Current smoker
- Diabetes mellitus, type 2
- Metabolic syndrome
Can participate in educational sessions in English or Spanish
Exclusion criteria
Discharged to nursing home or requiring 24‐hour in‐home care
Baseline modified Rankin score (mRS) of >2
Dementia
End‐stage disease with life expectancy less than one‐year
Randomization
Subjects are randomized, stratified for language, into intervention or usual care groups in a 1:1 ratio using a computerized permuted block randomization program (Table 1).
Table 1.
Intervention summary
| Baseline | Discharge | 72 h | One‐month | Three‐months | Six‐months | 12 months | |
|---|---|---|---|---|---|---|---|
| Intervention group |
|
|
|
|
|
|
|
| Standard care group |
|
|
|
|
|
|
|
BP, blood pressure; HbA1c, glycated hemoglobin.
Study arms
All patients receive a baseline interview including questions on demographics, social resources, health literacy, medication adherence, and validated measures of stroke knowledge/preparedness 5, 8. Baseline SBP, anthropometric measures, glycated hemoglobin (HbA1c), and lipid panel are measured. Charts are abstracted for additional history and clinical information. All participants receive a bag containing a tape measure to monitor waist circumference and a pillbox to organize medications.
All participants are followed up in‐person at 6 and 12 months postdischarge. At each in‐person assessment study, health workers conduct a brief structured interview to determine changes in stroke risk factors, risk behaviors, medication compliance, social support status, quality of life, and physical activity scale. Measurements of SBP, HbA1c, and anthropometric indices are repeated.
Intervention
Patients randomized to intervention engage in an educational session with a community health worker (CHW) and watch a culturally tailored motivational video of stroke survivorship narratives prior to discharge. Intervention patients receive a take‐home patientpaced, copy of the workbook (Figure 1) and video (Figure 2) comprised of interactive, skill‐based modules emphasizing DESERVE's three thematic areas: patient–physician communication, medical adherence, and accurate risk perception. In addition to the 6‐ and 12‐month follow‐ups for all subjects, intervention subjects receive calls scheduled at key intervals from CHWs to motivate behavior change, promote access to resources, and provide social support.
Figure 1.
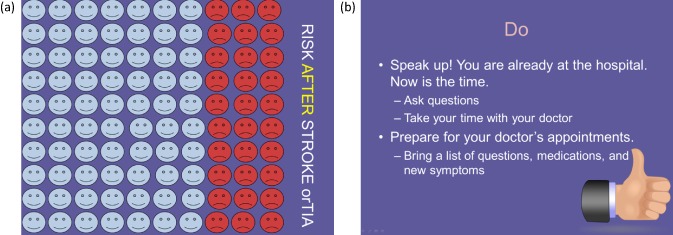
Informational and motivational presentation on stroke pathophysiology, risk factors, and lifestyle modification. (a) Graphic demonstration of increased risk after initial ischemic event; (b) graphic demonstration on empowering patients at doctors' visits.
Figure 2.
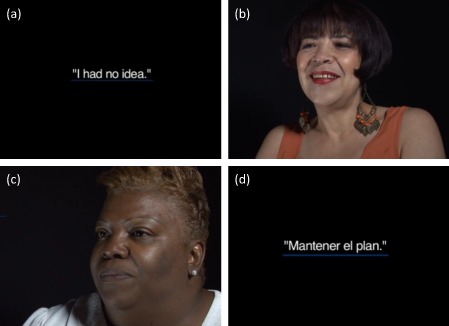
Motivational video (a) ‘I Had No Idea’: Patients describe their initial stroke and inaccurate assessment of vascular risk. (b) The Spanish version is culturally tailored to notions of faith and community. (c) ‘Don't Give Up’: Patients provide motivation in their own words: ‘Please don't give up, and above all, put in your heart that pity don't live there’. (d) ‘Keep on the Plan’: patients advise on how to be proactive at doctors' visits.
The DESERVE intervention is rooted in the Transtheoretical Model (TTM) for behavioral change. TTM emphasizes ‘stages of change’ as the pathway for sustainable behavior change. We posit the TIA/mild stroke ‘teachable moment’ propels the stroke survivor to the preparation stage for risk‐reduction strategies. Data from the Stroke Warning Information and Faster Treatment (SWIFT) trial provides evidence that patients and family members request action steps to address risk reduction 4. The DESERVE intervention utilizes the key TTM process of self‐evaluation to continue to identify realistic, rational ways to change behavior and incorporate the changes into a new self‐identity.
The DESERVE intervention also employs constructs from the Chronic Care Model (CCM), including community‐based interventions, to improve care integration 9, 10. Utilizing CCM in medically underserved communities is critical in addressing complex issues within communities. DESERVE utilizes bilingual CHWs to maximize cultural congruence in the intervention which is specifically tailored to minority TIA/mild stroke survivors.
Usual care
Usual care includes standard stroke care and treatment and distribution of standard stroke pamphlets in English or Spanish from the American Heart Association. Usual care subjects are given study contact information in case they have further questions. Any phone calls initiated by study participants will be documented.
Primary outcome
The primary outcome is difference in SBP reduction between the intervention and standard care arms in mmHg at 12‐month follow‐up.
Secondary outcomes
Secondary outcomes include between‐group differences in reduction of other vascular risk factors: HbA1c, body mass index (BMI), waist circumference, and smoking. Additionally, between‐group differences in medication adherence, appropriate self‐assessment of stroke risk, and medical appointment compliance will be assessed. We will also perform an analysis looking at the incremental cost of the intervention based on the average time spent by each health worker on each intervention patient times an expected cost per time unit. We will then compare this cost with other methods of blood pressure control.
Data and safety monitoring
While a data and safety monitoring plan was not required for this low‐risk educational intervention, protocols were established for cases where severe BP elevations or depression were detected during follow‐up.
Sample size
A randomized pilot study of 50 TIA/mild stroke patients demonstrated an 8 mmHg reduction in SBP in the intervention vs. standard care group. We then conducted power analysis using a lower 6 mmHg estimate of SBP change and an assumed variability of 23 mmHg as seen in the pilot study. Given 300 subjects per group and α = 0·05, power is 89·1%.
Statistical analysis
We will utilize two‐sample t‐tests in an intent‐to‐treat analysis for the primary outcome. We will evaluate the association between intervention assignment and change in SBP using linear regression controlling for relevant confounders including language. We will conduct repeated measures analysis using the changes in SBP at 6 and 12 months as a vector of outcome. We will fit a generalized estimating equation (GEE) model using the intervention indicator, time, and interaction between the intervention indicator and time as covariates. We will utilize multiple imputation for missing data in the intention‐to‐treat analysis.
Study organization and funding
NIH P50‐NS049060 to Dr. Boden‐Albala. The trial was registered at clinicaltrials.gov (#NCT 01836354).
Discussion
DESERVE will assess whether a novel, patient‐paced, culturally tailored education intervention can facilitate reduced vascular risk factors in survivors of mild stroke/TIA in a diverse, urban population. This intervention goes beyond typical lifestyle modification programs of diet and exercise and utilizes a theoretical construct to aid behavior change. We have made special considerations for commitment to family, communalism, religion/spirituality, fatalism, mistrust, worry about isolation, and death. Importantly, the DESERVE intervention is based on numerous pilot studies integrating input from African American and Latino stroke survivors and their family members, ethnically diverse community focus groups, community health advocates, and key community leaders. By utilizing patient‐paced workbooks and videos, we hope to make these interventions sustainable and practical in nonstudy settings with often limited resources.
Conflict of interest: None declared.
References
- 1. Kissela B, Schneider A, Kleindorfer D et al Stroke in a biracial population: the excess burden of stroke among blacks. Stroke 2004; 35:426–431. [DOI] [PubMed] [Google Scholar]
- 2. Sacco RL, Boden‐Albala B, Abel G et al Race‐ethnic disparities in the impact of stroke risk factors: the northern Manhattan stroke study. Stroke 2001; 32:1725–1731. [DOI] [PubMed] [Google Scholar]
- 3. Boden‐Albala B, Quarles LW. Education strategies for stroke prevention. Stroke 2013; 44(6 Suppl. 1):S48–51. [DOI] [PubMed] [Google Scholar]
- 4. Boden‐Albala B, Stillman J, Perez T et al A stroke preparedness RCT in a multi‐ethnic cohort: design and methods. Contemp Clin Trials 2010; 31:235–241. [DOI] [PubMed] [Google Scholar]
- 5. Boden‐Albala B, Carman H, Moran M, Doyle M, Paik MC. Perception of recurrent stroke risk among black, white and Hispanic ischemic stroke and transient ischemic attack survivors: the SWIFT study. Neuroepidemiology 2011; 37:83–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kleindorfer D, Khoury J, Broderick JP et al Temporal trends in public awareness of stroke: warning signs, risk factors, and treatment. Stroke 2009; 40:2502–2506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Boden‐Albala B, Edwards DF, Clair SS et al Methodology for a community‐based stroke preparedness intervention: the acute stroke program of interventions addressing racial and ethnic disparities study. Stroke 2014; 45:2047–2052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kumpfer KL, Alvarado R, Smith P, Bellamy N. Cultural sensitivity and adaptation in family‐based prevention interventions. Prev Sci 2002; 3:241–246. [DOI] [PubMed] [Google Scholar]
- 9. Bodenheimer T. Interventions to improve chronic illness care: evaluating their effectiveness. Dis Manag 2003; 6:63–71. [DOI] [PubMed] [Google Scholar]
- 10. Wagner EH. What will it take to improve care for chronic illness? Eff Clin Pract 1998; 1:2–4. [PubMed] [Google Scholar]


