Abstract
This research investigated baseline impulsivity, rejection sensitivity, and reactions to stressors in individuals with borderline personality disorder compared to healthy individuals and those with avoidant personality disorder. The borderline group showed greater impulsivity than the avoidant and healthy groups both in a delay-discounting task with real monetary rewards and in self-reported reactions to stressors; moreover, these findings could not be explained by co-occurring substance use disorders. Distress reactions to stressors were equally elevated in both personality disorder groups (relative to the healthy group). The borderline and avoidant groups also reported more maladaptive reactions to a stressor of an interpersonal vs. non-interpersonal nature, whereas the healthy group did not. Finally, self-reported impulsive reactions to stressors were associated with baseline impulsivity in the delay-discounting task, and greater self-reported reactivity to interpersonal than non-interpersonal stressors was associated with rejection sensitivity. This research highlights distinct vulnerabilities contributing to impulsive behavior in borderline personality disorder.
Borderline personality disorder (BPD) is characterized diagnostically by an enduring pattern of instability in multiple facets of an individual’s life including the self-concept, interpersonal relationships, and affect. In addition, individuals with BPD often show marked impulsivity, manifesting itself in high-risk behavior, self-injurious and suicidal behavior, and temper outbursts (American Psychiatric Association, 2013). These are especially devastating BPD symptoms because they may involve risk of death, serious health problems, or legal problems. Even the least risky of these symptoms take a high toll, as they undermine relationships, occupational functioning, and overall stability. Impulsivity in BPD has been found to be stable over time, and to be a long-term predictor of BPD symptom severity (Links, Heslegrave, & van Reekum, 1999). The trait impulsivity associated with BPD has been documented using self-report measures (e.g., Gagnon, Daelman, & McDuff, 2013), as well as tasks that assess impulsive decision-making in laboratory settings (e.g., Svaldi, Philipsen, & Matthies, 2014).
Given that self-report measures of impulsive traits and retrospective reports of impulsive behaviors can be highly influenced by response biases and recall biases, a delay-discounting task with monetary rewards has the advantage of being a real-time behavioral measure with high external validity. Delay-discounting procedures require participants to choose between small immediate monetary rewards and larger delayed monetary rewards. Impulsivity is measured by the tendency to choose the immediate rewards, suggesting that the perceived value of the future reward is diminished or discounted as a result of the delay (Rachlin, 1974; see also Kirby, Petry & Bickel, 1999; Reynolds & Schiffbauer, 2005). Developed for studies of substance use disorders, delay-discounting tasks have also shown utility in assessing baseline impulsivity in BPD samples (Crean, de Wit, & Richards, 2000; Lawrence, Allen, & Chanen, 2010). Nonetheless, it remains unclear whether the association of BPD with higher discounting rates may be explained by the presence of co-occurring substance use disorders. Coffey, Schumacher, Baschnagel, Hawk, and Holloman (2010) found that participants with both BPD and substance use disorder showed significantly more impulsive responding on the delay-discounting task than a healthy comparison group, whereas the small sub-sample of BPD participants without a substance use disorder did not.
In addition to a higher baseline level of impulsivity, BPD also involves a heightened vulnerability to maladaptive impulsive behaviors in the context of perceived rejection/abandonment and interpersonal stressors (Berenson, Downey, Rafaeli, Coifman, & Leventhal Paquin, 2011; Brodsky, Groves, Oquendo, Mann, & Stanley, 2006; Coifman, Berenson, Rafaeli, & Downey, 2013; Welch & Linehan, 2002; Yen et al., 2006). Exposure to pictures depicting negative interpersonal experiences elicits heightened emotional and physiological arousal in BPD relative to comparison groups (Limberg, Barnow, Freyberger & Hamm, 2011; Sauer, Arens, Stopsack, Spitzer, & Barnow, 2014), and in turn, interpersonally-triggered distress has been found to put people with BPD at greater risk for impulsive behavior (Chapman, Dixon-Gordon, Layden, and Walters, 2010). Consistent with this idea, more numerous stressful interpersonal life events are associated with greater impulsivity among individuals with BPD (Powers, Gleason, & Oltmanns, 2013).
Vulnerability to maladaptive behavior in the context of interpersonal stressors has been previously conceptualized and examined in terms of individual differences in rejection sensitivity, the tendency to anxiously expect, readily perceive and strongly react to the mere possibility of rejection in interpersonal situations (Downey & Feldman, 1996). Even among non-clinical samples, heightened rejection sensitivity is associated with a greater risk for hostile and aggressive reactions (Romero-Canyas, Downey, Berenson, Ayduk, & Kang, 2010). Moreover, among adults who had shown poor ability to delay gratification when assessed during childhood, rejection sensitivity is associated with increased substance use (Ayduk, et al., 2000) and self-reported BPD features (Ayduk et al., 2008). In short, impulsivity and rejection sensitivity are two distinct vulnerabilities both likely to contribute to the maladaptive impulsive behavior characteristic of BPD.
The Present Study
Baseline impulsivity
The present study examines delay discounting as an index of baseline impulsivity in BPD, using the task developed by Kirby et al. (1999) with both real and hypothetical monetary rewards. Although some studies suggest that these two procedures yield equivalent results (Johnson & Bickel, 2002; Lagorio & Madden, 2005; Lawyer, Schoepflin, Green, & Jenks, 2011; Madden, Begotka, Raiff, & Kastern, 2003; Matusiewicz, Carter, Landes, & Yi, 2013), these studies were not conducted in personality disorder samples. This study also aims to clarify some ambiguities in previous research regarding the role of co-occurring substance use disorders, testing the hypothesis that heightened impulsivity will be associated with BPD even when individuals with substance use diagnoses are excluded from the analyses. We also extend previous work by examining the specificity of impulsive responding in the delay-discounting task in BPD relative to a clinical comparison group with avoidant personality disorder (APD). Finally, we examine relationships between delay-discounting and specific BPD criteria, predicting that these relationships will be specific to symptoms involving impulsive behavior.
Stress reactions
In the present research, we examine the self-reported likelihood of impulsive behavior and distress in reaction to hypothetical interpersonal and non-interpersonal stressors, extending previous research in this area by comparing the pattern of stress reactions in BPD to those in another disorder characterized by high sensitivity to interpersonal rejection (APD). We predicted that impulsive reactions would be significantly more characteristic of BPD than APD, and that this impulsivity would not be explained by co-occurring substance use disorders. In contrast, we expected that relative to a healthy comparison group, distress reactions would be equally elevated in BPD and APD, and that both would report more maladaptive reactions to interpersonal than non-interpersonal stressors. Finally, we predicted that self-reported impulsive reactions to stressors would be associated with the index of baseline impulsivity obtained in the delay-discounting task, and that greater self-reported reactivity to interpersonal than non-interpersonal stressors would be associated with rejection sensitivity.
APD as a clinical comparison group
We selected APD as a clinical comparison group because it is similar to BPD in terms of prevalence, chronicity, and psychosocial impairment (Torgersen, Kringlen, & Cramer, 2001; Wilberg, Karterud, Pedersen, & Umes, 2009). Moreover, like BPD, APD is associated with especially maladaptive reactions to interpersonal stressors (Gadassi et al., 2014; Meyer, Ajchenbrenner, & Bowles, 2005). Consistent with this shared vulnerability, the two disorders show substantial comorbidity (American Psychiatric Association, 2013). Nevertheless, they present with diverging behavioral profiles. Whereas BPD is associated with difficulty resisting behaviors that bring immediate reward or relief, APD is associated with high levels of inhibition. This research is designed to highlight both the ways in which BPD and APD are expected to differ (baseline impulsivity) and the ways they are expected to be similar (sensitivity to rejection).
Method
Participants and Recruitment
Adult participants from a metropolitan area were recruited for a larger study on personality and mood in daily life. Advertisements published in newspapers and posted on Internet forums were designed to reach people with BPD or APD by describing symptoms of the disorders (e.g., mood swings, shyness). Flyers were also posted at treatment clinics, and disorder-specific support groups. Interested individuals completed a telephone screening based on the Structured Clinical Interview for DSM-IV Personality Disorders (SCID-II-Q; First, Gibbon, Spitzer, Williams, & Benjamin, 1997). Those likely to meet criteria for one of the study groups were invited to the lab for a diagnostic interview, which included the Structured Interview for the Diagnosis of Personality Disorders (SID-P-IV; Pfohl, Blum & Zimmerman, 1997) and the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I; First, Gibbon, Spitzer, & Williams, 1996). Conducted or supervised by doctoral-level clinical psychologists, the interviews demonstrated good inter-rater reliability at the criterion and diagnostic level for personality disorders (kappa = .83) and at the diagnostic level for Axis-I disorders (kappa =.86). Reliability was established by comparing ratings of five videotaped interviews with those of an expert diagnostic interviewer.
Participants who met criteria for BPD were included in the BPD group. To be eligible for the APD group, participants were required to meet criteria for APD and to not meet criteria for diagnosis with any cluster B personality disorder. Those meeting criteria for both BPD and APD were included in the BPD group because when they occur together, BPD is the more salient of the two disorders and more likely to be the direct focus of treatment (McGlashan et al., 2000). Dividing the groups this way may have made it more difficult for us to detect the differences we predicted between the BPD and APD groups. Yet, as both diagnosable and subclinical levels of comorbidity are the rule rather than the exception for personality disorders, it is impossible to select truly non-overlapping BPD and APD groups without a substantial cost to external validity.
Participants eligible for the healthy comparison (HC) group met no more than two criteria for a specific personality disorder and no more than 10 criteria in total; they had no psychiatric diagnoses nor use of psychotropic medication in the previous year, and had a Global Assessment of Functioning score of at least 80. Primary psychotic disorder, current substance intoxication or withdrawal, and cognitive impairment or illiteracy were exclusion criteria for all three groups.
The measures that are the focus of this investigation were added to the study procedures midway through data collection for a large project; hence the sample is smaller than the sample completing other portions of the study (e.g., MASKED REFERENCE). All participants who completed both versions of the delay-discounting task and the reactions to stressors questionnaire are included in these analyses. The current study sample (N=104) includes 35 (30 female) meeting DSM-IV-TR criteria for BPD (9 of them meeting criteria for APD as well), 24 (13 female) who met DSM-IV-TR criteria for APD (without BPD), and 45 (31 females) meeting eligibility criteria for our HC group. The significant difference in the proportion of females in the BPD vs. APD groups, χ2 = 7.17, p = .007, is consistent with gender differences in the prevalence of these disorders (American Psychiatric Association, 2013).
Participants were 18–64 years old, M = 30.69, SD = 9.63, with no significant age differences in the three groups, F < 1, ns. They identified their racial/ethnic backgrounds as White (48.1%) Black (22.1%) Latino/a (12.5%) Asian (12.5%) Native American (1%) and multiracial (3.8%), and the three groups did not differ in race/ethnicity. They had completed between 10 and 20 years of education M = 16.10, SD = 2.58. The HC group had significantly more education M = 16.89, SD = 2.54 than the BPD group, M = 15.54, SD = 2.38; t (78) = 2.42, p =.02, and the APD group M = 15.42, SD = 2.60; t (67) = 2.27, p =.03. The BPD and APD groups did not differ from one another in education level t < 1, ns.
Fourteen participants in the BPD group and six in the APD group were currently taking medication for a psychiatric condition, χ 2 = 1.43, ns. Seventeen in the BPD group, nine in the APD group, and two in the HC group were currently receiving psychotherapy or counseling (not significantly different for the BPD vs. APD groups, χ2 = 0.71, ns.). Table 1 presents Axis I diagnoses for the BPD and APD groups.
Table 1.
Current DSM-IV Axis I diagnoses.
| BPD (35) | APD (24) | χ2 | p | |
|---|---|---|---|---|
| Major depressive disorder | 18 | 5 | 5.60 | <.05 |
| Bipolar disorder | 3 | 0 | 2.17 | ns |
| Dysthymic disorder | 8 | 7 | 0.30 | ns |
| Social anxiety disorder | 16 | 25 | 19.22 | <.001 |
| Post-Traumatic stress disorder | 13 | 1 | 8.55 | <.01 |
| Panic disorder | 3 | 1 | 0.44 | ns |
| Agoraphobia without history of panic | 2 | 1 | 0.07 | ns |
| Obsessive-compulsive disorder disorder | 1 | 1 | 0.08 | ns |
| Generalized anxiety disorder | 14 | 7 | 2.22 | ns |
| Bulimia | 1 | 0 | 0.70 | ns |
| Binge eating disorder | 0 | 2 | 3.02 | ns |
| Substance dependence | 9 | 0 | 7.28 | <.01 |
| Substance abuse | 5 | 0 | 3.75 | ns |
Procedure
Following the diagnostic interview, eligible participants returned for a second lab visit in which they completed a battery of social-cognitive tasks and questionnaires, including the hypothetical delay-discounting task and the questionnaire assessing reactions to an interpersonal stressor. After at least three weeks, participants returned to the lab for a third visit, where they completed the delay-discounting task with the possibility of a real monetary reward, and completed the questionnaire about reactions to a non-interpersonal stressor. During each lab session participants also took part in other tasks and in the weeks between them completed an experience-sampling diary; these are all beyond the scope of this paper but have been reported elsewhere (MASKED REFERENCES). Participants provided written informed consent and were compensated for their time. All study procedures were approved by applicable Institutional Review Boards.
Delay-discounting task – Hypothetical reward version
Once participants arrived for their second lab visit, a trained research assistant escorted them into a soundproof room, and instructed them to sit directly in front of a computer and response box. Participants read the following instructions on the computer screen: “You will see a pair of options. For each pair, please indicate which of the two options you’d prefer by pressing the button that corresponds to it (either “1” or “2”)” (Kirby et al., 1999). Participants were told that they should make their selections at a pace that was comfortable for them and should not rush.
During the task, participants were presented with 27 hypothetical pairs of smaller immediate and larger delayed monetary rewards, for example: 1) $11 today or 2) $30 in 7 days (Kirby et al., 1999). The 27 reward pairs were presented in the same order for each participant. At the beginning of each trial the top of the computer screen read: “Which of the following options would you prefer?” Beneath this question, the two reward options were centered on the computer screen, with the smaller immediate reward displayed above the larger delayed reward, separated by the word “or.” The computer recorded participants’ responses.
Delay-discounting task – Real reward version
During their third lab visit, participants completed the same task again but with an important difference: as in Kirby et al. (1999) they were told that they had a one-in-six chance of actually receiving one of the reward options that they chose. Specifically, participants were told that after they selected their preferences, the experimenter would roll a six-sided die to determine whether or not they would receive a reward. If they were to receive a reward, the experimenter would roll a 30-sided die to determine which of the 27 selected reward options they would receive. If they selected the immediate reward they would receive cash before leaving the session. If they selected the delayed reward, it would be mailed to them on the specified date or they could arrange to pick it up in person on or after that date. The choices were presented on paper, in the same order as they had been presented during the hypothetical version of the task, and participants were asked to circle their preferred options. They were told: “Remember, one of these may turn out to be a real monetary reward, so you should answer every question as if it were going to be the one you will win.”
Reactions to interpersonal and non-interpersonal stressors
Participants completed questionnaires regarding the self-reported likelihood of particular reactions to an interpersonal and non-interpersonal stressor, administered at least 3 weeks apart. These questionnaires were developed by the authors specifically for the purpose of this paper.
The interpersonal condition began with instructions to identify by name a person who is important to them: “For this questionnaire, we would like you to think about a specific person who is very important to you and close to you, preferably your romantic partner or closest friend.” Participants were then instructed to visualize and answer questions about a hypothetical scenario involving the identified individual: “Imagine if you thought that [important person] might be losing interest in you, or be about to let you down. What thoughts, feelings, and behaviors would you be likely to have? Please indicate how likely you would be to react in the ways listed below.” The questionnaire then proposed a series of possible reactions and the participant was asked to rate the likelihood of engaging in each one. Participants responded on a Likert scale ranging from 1 – 6, with 1 being very unlikely and 6 being very likely.
For the non-interpersonal condition, participants were asked to identify some expensive equipment that is particularly important to them: “Imagine if you thought that your important piece of equipment might be malfunctioning or about to stop working at all. What thoughts, feelings, and behaviors would you be likely to have? Please indicate how likely you would be to react in the ways listed below.” Participants rated the likelihood of responding various ways from 1 – 6, with 1 being very unlikely and 6 being very likely.
Impulsive reactions were assessed using five items (interpersonal impulsivity, α=89, non-interpersonal impulsivity, α=85). The items were: “do something that could be harmful to me e.g., binge eating getting drunk or high, risky sex, shoplifting, etc”; “impulsively do or say something I shouldn’t “; “do or say something without considering the consequences”; “smash or otherwise destroy something important to me”; “be unable to keep my temper from exploding”.
Distress reactions included unpleasant cognitive/affective responses without any explicitly impulsive components (interpersonal distress, α=92, non-interpersonal distress, α=85). The five items on this scale were: “feel helpless”; “feel worthless”; “experience intense despair or panic”; “think about how much worse the situation could become”; “believe there is nothing I can do to help myself feel better”.
Rejection sensitivity
To examine predicted group differences in reactions to interpersonal versus non-interpersonal stressors, we assessed anxious expectations for rejection by people who are important to the self, using the Adult Rejection Sensitivity Questionnaire (ARSQ). Similar in structure and scoring to the college student RSQ from which it was adapted (Downey & Feldman, 1996), the adult version presents nine hypothetical interpersonal situations involving possible acceptance or rejection by important others. For each situation, respondents rate the anxiety/concern they would feel about the outcome, as well as the likelihood that the other would respond with rejection. Scores are calculated by first multiplying the expected likelihood of rejection for each situation by the degree of anxiety/concern, and then averaging these weighted scores across the nine situations (see Berenson et al., 2009). Participants completed this measure during their first lab visit; its internal consistency in this sample was .91.
Covariates
Social desirability, sex, and age (in years) were assessed via questionnaires during participants’ initial lab visit for inclusion as covariates in all our analyses. We assessed the tendency to answer questions in a socially acceptable way using the Social Desirability Scale (Crowne & Marlowe, 1960). The scale consists of 33 yes-no questions about desirable uncommon behaviors and undesirable common behaviors; its internal consistency in this sample was .86. Measures of social desirability are frequently used as covariates when the desirability or undesirability of response options may be an important influence on the data, as was the case in our study. Sex was included as a covariate because the proportion of females varied with group and there are likely to be different gender norms for reactions to stress. Age was included as a covariate to eliminate variance attributable to the inverse correlation between impulsivity and age from adolescence to retirement (Reimers, Maylor, Stewart, & Chater, 2009).
Because they were testing specific comparisons based on apriori hypotheses, our analyses did not utilize any corrections for type II error.
Results
Estimating Discounting Rates (k values)
A preference for immediate rewards over delayed ones can be thought of as a discounting of future rewards because of the delay. The higher the discounting rate k is, the more intensely the value of a future reward is discounted relative to the value of a reward received today. This rate therefore reflects impulsivity, the tendency to discount and forgo greater future rewards in favor of smaller, more proximal ones. The discounting rate is defined by the following equation, where V is the present value of the delayed reward A, D is the length of delay (days, in this case) and k is the discounting rate:
We followed the procedures used by Kirby et al. (1999) to estimate the value of each individual’s discounting rate (denoted by ksubj) from the 27 choices they made during the task. Each of these choices specifies a smaller immediate reward (SIR), a larger delayed reward (LDR) and a number of days of delay (D). The 27 choices involve a combination of nine levels of discounting rate and three levels of reward size (small, medium, large). Each trial has its own discounting rate, denoted by ktrial and defined as:
The estimation procedure for ksubj is based on the logic that if the participant chooses the LDR, then his/her actual discounting rate must be lower than the discounting rate of the trial, whereas if the participant chooses the SIR, his/her discounting rate must be higher than ktrial. The upper and lower bounds of ksubj can be estimated by examining each participant’s 27 choices. For example, if a person chooses the SIR in the first four levels of discounting rate (which means ksubj > 0.0025) and chooses the LDR for the remaining five levels (which means ksubj< 0.006), we could estimate that ksubj is within the range of [0.0025, 0.006]. As in Kirby et al. (1999), we would estimate this individual’s discounting rate by taking the geometric mean of 0.0025 and 0.006 (since the discounting rates were designed to have approximately equal intervals after a logarithmic transform). Therefore, the nine levels of discounting rate form ten ranges, each having two consecutive levels of discounting rate as its upper or lower bounds except for the first and last range. The estimated discounting rate of the middle eight ranges is the geometric mean of their upper and lower bounds. The lowest range has a discounting rate of 0.00016 and the highest range has a discounting rate of 0.25.
Of course, participants are not always perfectly consistent in their choices. For example, a participant may choose SIR on the first four levels, LDR on level five; SIR on level six, and LDR on levels seven though nine. As in Kirby et al. (1999), we identified the range for as the one selected most frequently. When two or more ranges were selected with equal frequency, ksubj was estimated as the geometric mean of these ranges. The distribution of ksubj values for our sample was positively skewed, but it became normal after applying a natural log transform.
Diagnostic Group Differences in Hypothetical and Real Discounting Rates
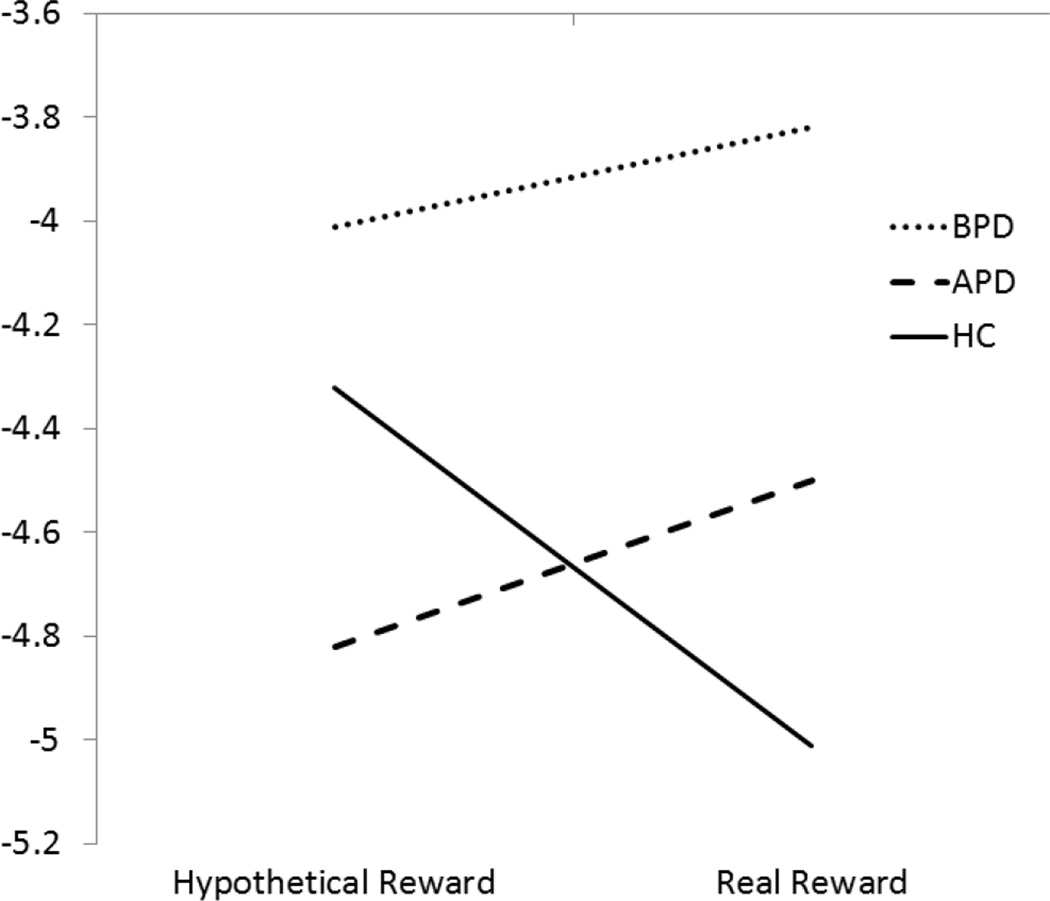
Discounting rates were analyzed in a series of repeated measures General Linear Models (GLM) with task type (hypothetical, real) as a within-subject variable and diagnostic group (BPD, APD, HC) as the between subjects variable. Sex, age, and social desirability scores were included as covariates. There was no main effect of task type, F(1,98) < 1, ns, ηp2 = .01, and no main effect of group F(2,98) = 2.31, ns, ηp2 = .05, but results revealed a significant task type by diagnostic group interaction F(2,98) = 3.09, p < .05, ηp2 = .06, depicted in Figure 1.
Figure 1.
Discount rates (log transformed) by diagnostic group, adjusting for sex, age, and social desirability scores.
In the real reward condition, the BPD group showed a significantly higher discounting rate M(SE) = −3.82 (.26) than the HC group, M (SE) = −5.01 (.23), t (98) = 3.08, p < .01 ηp2 = .09, and a marginally higher discounting rate than the APD group, M(SE) = −4.50 (.29), t(98) = 1.78 p < .08, ηp2 = .03. There was no significant difference between the APD and the HC groups t(98) = 1.35 ns, ηp2 = .02. Parallel analyses in the hypothetical task condition did not reveal any statistically significant differences. The BPD group M (SE) = −4.01 (.34) did not differ from HC M (SE) = −4.32 (.29) t < 1, ns, ηp2 = .00, or from APD M (SE) = −4.72 (.36) t(98) = 1.46, ns, ηp2 = .02. Additionally, the APD group did not differ from the HC group, t < 1, ns, ηp2 = .01.
Because the role of co-occurring substance use disorders in the discounting rates associated with BPD has been an unresolved issue in prior research (e.g., Coffey et al, 2010) we repeated our analyses excluding the 11 individuals diagnosed with concurrent substance dependence and/or abuse. Just as before, there was no main effect of task type, F(1,87) = 1.24, ns, ηp2 = .01, and no main effect of group F(2,87) = 1.59, ns, ηp2 = .04, but the task type by diagnostic group interaction was significant F(2,87) = 3.64, p < .05, ηp2 = .08. In the real reward condition, the BPD group showed a significantly higher discounting rate M (SE) = −3.685 (.33) than the HC group, M (SE) = −4.98 (.23), t (87) = 2.98, p < .01 ηp2 = .09, and a marginally higher discounting rate than the APD group, M(SE) = −4.45 (.30), t(87) = 1.78 p < .08, ηp2 = .04. The difference between the APD and the HC groups was not statistically significant, t (98) = 1.34 ns, ηp2 = .02. Again, there no between-group differences in impulsivity in the hypothetical reward condition. The BPD group M (SE) = −4.15 (.41) did not differ from HC M (SE) = −4.30 (.30) t < 1, ns, ηp2 = .00, or from APD M (SE) = −4.69 (.38) t(87) = 1.00, ns, ηp2 = .01. The APD group also did not differ from the HC group, t < 1, ns, ηp2 = .01. Diagnostic group differences in delay discounting were unchanged after excluding participants with co-occurring substance use disorders, ruling out these disorders as an explanation for the elevated discounting rate associated with BPD.
Discounting Rates and Symptom Profiles
We examined the association of discounting rates in the real monetary reward task with each BPD criterion separately, expecting the largest associations to emerge for criteria that are characterized by impulsivity. These analyses are shown in Table 2. As expected, the largest effect was found for criterion 4 of BPD (impulsive behavior problems), and significant effects were also found for the criteria involving self-injury/suicidality (criterion 5) and rage (criterion 8). Significant associations also emerged for the interpersonal criteria involving unstable relationships (criterion 2), and frantic responses to perceived abandonment (criterion 1), highlighting the role of impulsivity in the extent to which perceived interpersonal stress would trigger extreme behavioral reactions. Finally, a significant association was also found with emptiness (criterion 7), a symptom often described as preceding and potentially motivating problematic impulsive behaviors such as self-injury or pursuit of intense stimulation (e.g., Klonsky, 2008; Rallis, Deming, Glenn, & Nock, 2012). The BPD criteria involving identity disturbance, affective instability, and paranoia/dissociation were not significantly related to discounting rates. No APD criteria were significantly related to discounting rates, and no criteria for either disorder were significantly related to the discounting rate for hypothetical rewards.
Table 2.
Means and standard deviations of discounting rates (log transformed k) in the real reward condition by DSM-IV-TR criteria for BPD, adjusting for sex, age, and social desirability scores.
| Met criterion | |||||
|---|---|---|---|---|---|
| Criterion | No | Yes | |||
| M (SE) | M (SE) | F (1, 99) | ηp2 | p | |
| 1. Abandonment reactions | − 4.69 (.16) | − 3.90 (.30) | 4.96 | .05 | <.05 |
| 2. Interpersonal instability | − 4.85 (.17) | − 3.71 (.26) | 11.67 | .11 | <.001 |
| 3. Identity disturbance | − 4.46 (.16) | − 4.63 (.36) | < 1 | .00 | ns |
| 4. Impulsive behavior problems | − 4.90 (.17) | − 3.62 (.27) | 13.64 | .12 | <.001 |
| 5. Suicidality or self-injury | − 4.72 (.17) | − 3.93 (.29) | 4.79 | .05 | <.05 |
| 6. Affective instability | − 4.70 (.19) | − 4.07 (.29) | 2.68 | .03 | ns |
| 7. Emptiness | − 4.74 (.18) | − 4.09 (.23) | 4.68 | .05 | <.05 |
| 8. Rage | − 4.70 (.17) | − 3.97 (.28) | 4.43 | .04 | <.05 |
| 9. Transient dissociation or paranoia | − 4.62 (.16) | − 4.12 (.29) | 2.24 | .02 | ns |
Reactions to Stressors
Self-reported responses to the interpersonal and non-interpersonal stressor were analyzed in a series of repeated measures General Linear Models (GLMs) with stressor type (non-interpersonal, interpersonal) as a within-subject variable and diagnostic group (HC, BPD, APD) as a between subjects variable. Sex, age, and social desirability were included as covariates.
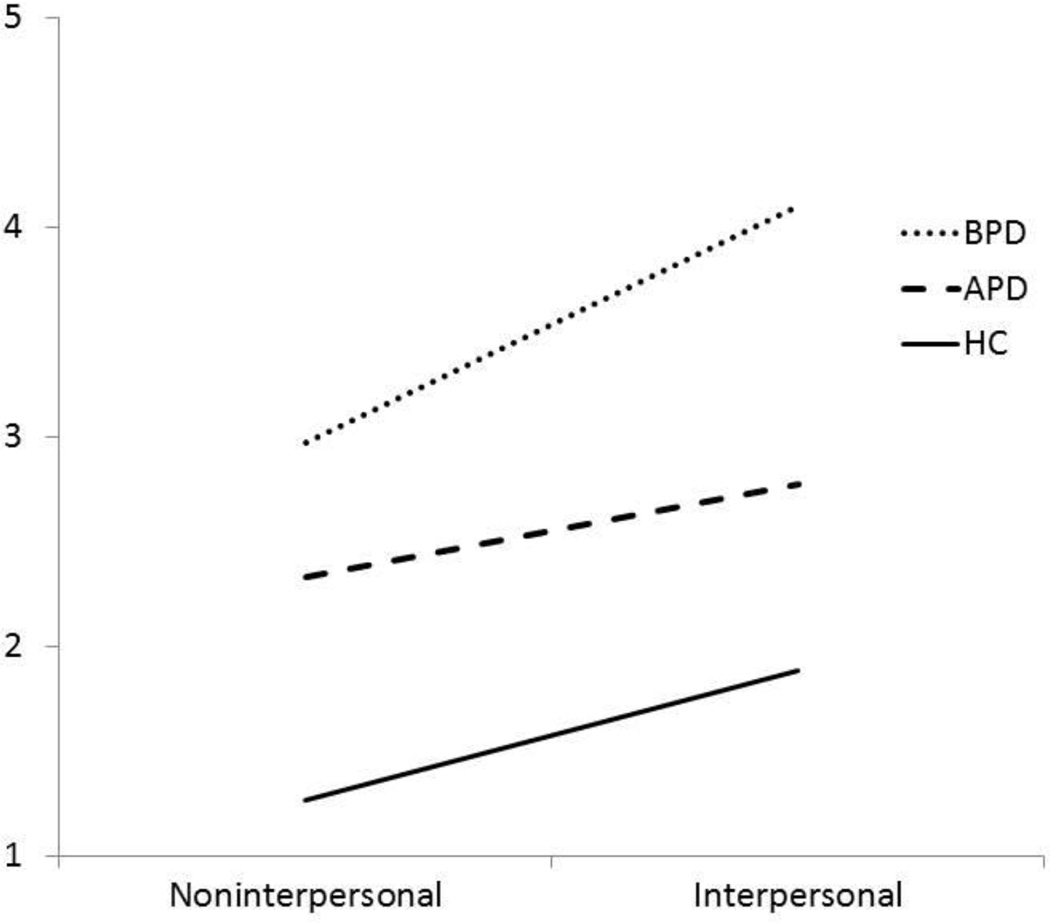
Self-reported impulsive reactions
The group means from our analysis are depicted in Figure 2. A significant main effect of stressor type, F(1,98) = 6.85, p < .05, ηp2 = .07, indicated that on average the interpersonal stressor elicited more impulsive reactions M (SE) = 2.91 (.10) than the non-interpersonal stressor, M (SE) = 2.19 (.09). There was also a main effect of diagnostic group F(2,98) = 37.89, p < .001, ηp2 = .44, such that the BPD group reported more impulsive reactions M (SE) = 3.54 (.15) than the APD group M (SE) = 2.55 (.17) and both reported more impulsive reactions than the HC group M (SE) = 1.57 (.13). However, these main effects were somewhat qualified by the stressor by diagnostic group interaction, which approached statistical significance F(2,98) = 3.04, p = .052, ηp2 = .06.
Figure 2.
Self-reported impulsive reactions to stressors by diagnostic group, adjusting for sex, age, and social desirability scores.
In the interpersonal stressor condition, the BPD group reported significantly higher impulsive reactions M (SE) = 4.10 (.19) compared to the HC group, M (SE) = 1.89 (.16), t(98) = 8.13, p < .001 ηp2 = .40. The APD group M (SE) = 2.78 (.20), also reported more impulsive reactions than the HC group t(98) = 3.37, p < .001, ηp2 = .10. The BPD group also reported significantly more impulsive reactions than the APD group, t(98) = 4.88, p < .001, ηp2 = .20. The same pattern of results also emerged in the non-interpersonal stressor condition. That is, the BPD group reported significantly higher impulsivity 2.97 (.18) than the HC group, M (SE) = 1.26 (.16) , t (98) = 6.52, p < .001 ηp2 = .40. The APD group, M (SE) = 2.33 (.19), likewise reported more impulsivity than the HC group t(98) = 4.21 p < .001, ηp2 = . 15. Finally, the BPD group reported significantly more impulsive reactions than the APD group, t (98) = 2.45, p < .05, ηp2 = .06.
To rule out the possibility that the elevated impulsive reactions to stressors reported by the BPD group may be explained by co-occurring substance use disorders in this group, we repeated our analyses excluding participants diagnosed with current substance dependence and/or abuse. Again there were significant main effects of stressor type, F(1,87) = 9.17, p < .01, ηp2 = . 10, and diagnostic group F(2,87) = 33.76, p < .001, ηp2 = .44, but both main effects were qualified by a significant stressor type by diagnostic group interaction F(2,87) = 8.17, p = .001, ηp2 = .16. In the interpersonal stressor condition, the BPD group reported significantly higher impulsive reactions M (SE) = 4.28 (.22) compared to the HC group, M (SE) = 1.86 (.16), t(87) = 8.21, p < .001 ηp2 = .44. The APD group M (SE) = 2.78 (.20), also reported more impulsive reactions than the HC group t(87) = 3.42, p < .001, ηp2 = .12. The BPD group also reported significantly more impulsive reactions than the APD group, t(87) = 5.13, p < .001, ηp2 = .23. In the non-interpersonal stressor condition the BPD group reported significantly higher impulsivity 2.78 (.20) than the HC group, M (SE) = 1.27 (.14), t(87) = 5.80, p < .001 ηp2 = .28, and the APD group, M (SE) = 2.34 (.18), likewise reported more impulsivity than the HC group t(87) =4.56 p < .001, ηp2 = .19. The BPD group also reported marginally more impulsive reactions than the APD group, t (87) = 1.68, p = .096, ηp2 = .03. The BPD group continues to show an elevation in impulsive stress reactions and a greater increase in impulsive reactions to interpersonal (vs. non-interpersonal) stressors when participants with substance use disorders have been removed from the analysis.
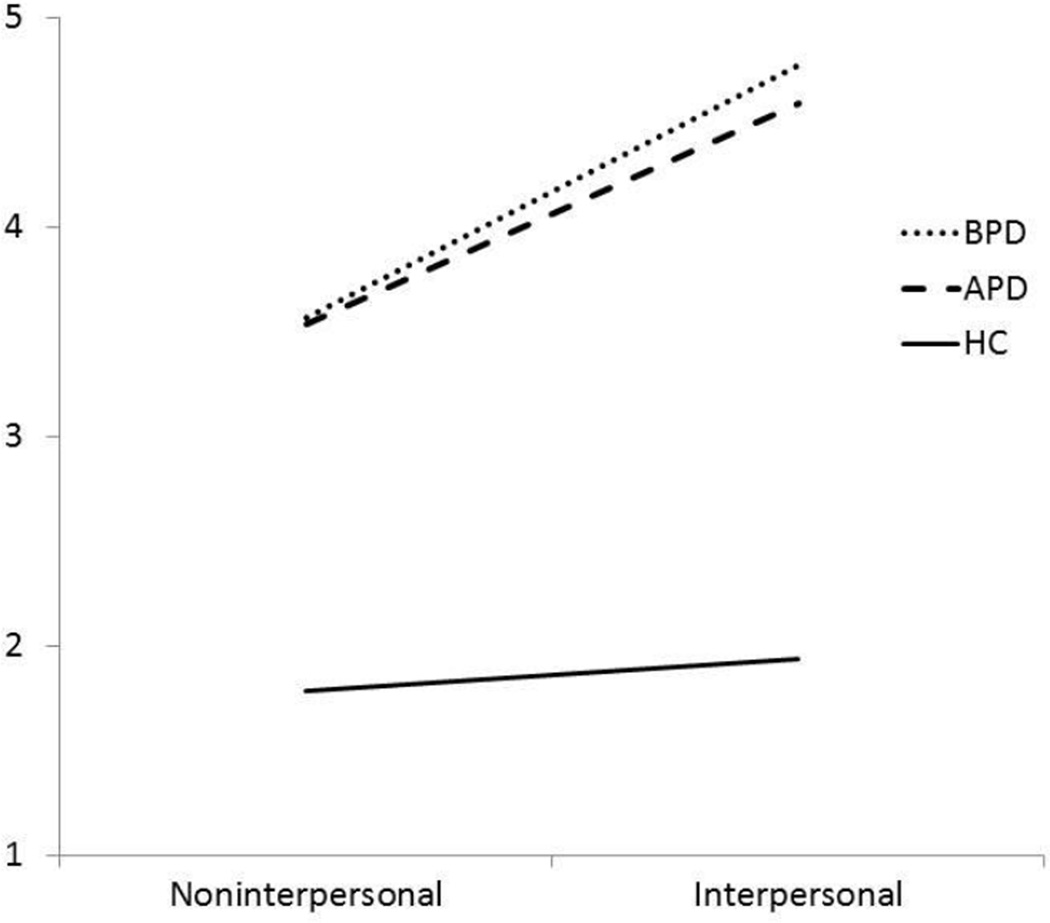
Self-reported distress reactions
The group means from our analysis of the distress scale are depicted in Figure 3. A significant main effect of stressor type, F(1,98) = 4.27, p < .05, ηp2 = .04, indicated that on average the interpersonal stressor elicited more distress than the non-interpersonal stressor. There was also a main effect of diagnostic group F(2,98) = 67.82, p < .001, ηp2 = .58. These effects were both qualified, however, by a significant stressor by diagnostic group interaction F(2,98) = 5.55, p < .01, ηp2 = .10.
Figure 3.
Self-reported distress reactions to stressors by diagnostic group, adjusting for sex, age, and social desirability scores.
In the interpersonal stressor condition, the BPD group reported significantly higher distress M (SE) = 4.77 (.18) compared to the HC group, M (SE) = 1.94 (.16), t(98) = 10.84, p < .001 ηp2 = .55. The APD group M (SE) = 4.59 (.19), also reported more distress than the HC group t (98) = 10.46, p < .001, ηp2 = .53. The BPD and APD groups, however, did not significantly differ from one another t (98) < 1 ns, ηp2 = .01. In the non-interpersonal stressor condition the BPD group reported significantly higher distress M (SE) = 3.57 (.21) than the HC group, M (SE) = 1.78 (.19), t (98) = 5.76, p < .001 ηp2 = .25. The APD group, M (SE) = 3.53 (.23), also reported more distress than the HC group t (98) = 5.84 p < .001, ηp2 = .26. The BPD and APD groups did not differ in their level of self-reported distress reactions to the non-interpersonal stressor t < 1, ns, ηp2 = .00.
Association of Impulsive Reactions to Stressors with Discounting Rates
To test the prediction that discounting rates would be associated with self-reported impulsive reactions (but not distress reactions) to stressors, we computed the partial correlation between the log-transformed k value for the real discounting task with the impulsivity and distress reactions scales (averaged across the interpersonal and non-interpersonal conditions), adjusting for sex, age, and social desirability. As expected, discounting rates were significantly correlated with self-reports of impulsive reactions to stress, r (99) = .26, p <.01, but were not significantly correlated with self-reported distress reactions, r (99) = .14, ns.
Association of Heightened Reactions to the Interpersonal Stressor with Rejection Sensitivity
As expected, rejection sensitivity scores were significantly higher in the BPD group M = 15.84 SD = 6.74 than the HC group M = 6.47 SD = 2.77, t = 7.52, p < .001; scores were also significantly higher in the APD group M = 17.35 SD = 7.25, than in the HC group, t = 7.78, p < .001. The BPD and APD groups did not significantly differ from one another t = −1.03, ns.
We predicted that rejection sensitivity should be associated with more intense self-reported impulsive and distress reactions to the interpersonal than the non-interpersonal stressor. To test this hypothesis, we examined the partial correlations of rejection sensitivity with the difference between reactions to the two stressors (interpersonal minus non-interpersonal) adjusting for the corresponding reactions to the non-interpersonal stressor as well as sex, age, and social desirability. As predicted, rejection sensitivity was significantly associated with stronger self-reported reactions to the interpersonal stressor than the non-interpersonal stressor, for both types of reactions (impulsivity r(98) = .23, p < .05; distress r(98) =.46, p < .001).
Discussion
As predicted, individuals with BPD showed greater impulsivity than those with APD and an HC group, both in a delay-discounting task and in a self-report measure of impulsive reactions to stressors. Moreover, the delay-discounting measure of impulsivity was related to both self-reported impulsive reactions to stressors and diagnostic criteria involving impulsivity as assessed by clinical interview. Whereas impulsive reactions to stressors were significantly elevated in the BPD group relative to the other groups, distress reactions were equally intense in both the BPD and APD groups. Notably, the maladaptive reactions to stressors characteristic of each disorder (impulsivity in BPD and distress in both disorders) were stronger for a hypothetical interpersonal stressor (unresponsiveness of an important other) than for a hypothetical non-interpersonal stressor (failure of important equipment). As predicted, the heightening of maladaptive reactions to interpersonal compared to non-interpersonal stressors was associated with rejection sensitivity, a vulnerability common to both BPD and APD. Our study is unique in combining performance-based and self-report measures to examine different forms of impulsivity and reactions to stressors under different contexts. Our study also extends previous research by ruling out concurrent substance use disorders as an alternative explanation for elevated indexes of impulsivity in BPD, examining associations of discount rates with specific BPD criteria, and including a clinical comparison group with APD.
Clinical Implications
The present study adds to the existing evidence for elevated impulsivity in BPD, showing that it is present both when individuals make monetary choices in a relatively emotion-free laboratory context, and in their self-reported responses to hypothetical stressors. These findings suggest that interventions designed to help individuals with BPD to delay reacting until after they have evaluated the long-term positive and negative consequences of potential reactions may be a particularly important component of effective treatment. This study also highlights the role of rejection sensitivity in the distress experienced by both those with BPD and APD, and suggests that individuals with these disorders may especially benefit from interventions focusing on the role of maladaptive interpretations of interpersonal cues in triggering their symptoms, as well as interventions to improve the quality of their close relationships.
As predicted, participants in the BPD group reported significantly higher likelihood of impulsive reactions to hypothetical stressors than did those in the APD or HC groups. However, the APD group also reported significantly higher likelihood of these impulsive reactions than did the HC group. We had not predicted this result because APD (unlike BPD) does not include impulsivity among its defining criteria. Nonetheless, the finding of somewhat elevated impulsive reactions to stressors in APD is not entirely surprising. For example, APD is significantly tied non-suicidal self-injury (Cawood & Huprich, 2011). Moreover, although the participants in the present APD sample showed no current substance use disorders, problematic alcohol use is significantly associated with APD (Olsson & Dahl, 2012) as well as generalized social phobia (Morris, Stewart & Ham, 2005). The elevated likelihood of impulsive reactions to stressors found in the APD group in this study highlights the extent to which impulsive behavior problems may be an under-recognized aspect of APD worthy of greater clinical attention.
Although participants in the BPD group reported greater reactivity to interpersonal than non-interpersonal stressors, as predicted, they also both reported greater reactivity to the non-interpersonal stressor than HC participants. This finding suggests that even if interpersonal triggers are most problematic for people with BPD, there is also a more general difficulty coping with stress. The emotion dysregulation associated with BPD (e.g., Bijttebier & Vertommen, 1999; Chapman, Leung, & Lynch, 2008) is likely to intensify reactions to non-interpersonal (as well as interpersonal) stressors. Interventions that build distress tolerance, reduce physiological arousal, and counter automatic negative thoughts about stressors may be beneficial.
Interestingly, reactivity in the non-interpersonal stress condition was similarly elevated (relative to HC participants) in those with APD, a disorder that is not commonly noted for emotion dysregulation issues. It is possible that people with this disorder also experience emotion dysregulation, but in a more hidden way than do those with BPD. Coping with stressors may also be hindered in APD by difficulties accessing and/or benefitting from social support.
Limitations and Directions for Future Research
The small size of our APD group restricted power for detecting how this group differed from the BPD and HC groups. Although our results suggest that levels of impulsivity in APD fell in between the levels found in the other two groups, it will be important for future studies to examine this phenomenon in a larger sample.
Although both the delay-discounting and reactions to stressors tasks involved two within-person conditions, condition order was not randomized. Responses to the real reward delay-discounting task are unlikely to have been influenced by having previously completed the hypothetical reward task, because each question involves a specific monetary amount and delay time that would be difficult to recall and unlikely to have been associated with affective responses that would be evoked by seeing the question again. However, it is possible that when reporting on their reactions to the non-interpersonal stress scenario, having previously answered the same questions while imagining the interpersonal stress scenario may have influenced their responses. Though reduced by separation of the conditions by at least three weeks, such potential order effects cannot be ruled out.
Interestingly, results were only found for the delay-discounting task when the monetary rewards were real; the hypothetical delay-discounting task yielded no meaningful group differences or associations. These results contrast with several prior studies that found no significant difference between hypothetical and real rewards in the delay-discounting task (Johnson & Bickel, 2002; Lagorio & Madden, 2005; Lawyer, et al., 2011; Madden, et al., 2003; Matusiewicz, et al., 2013). However, like the present study, Hinvest and Anderson (2010) found that healthy participants were significantly less impulsive in a real (versus hypothetical) reward condition. One possible reason for such a pattern is if the ability to regulate impulsive behaviors does not necessarily emerge uniformly in all situations but specifically when an impulsive response has the potential to result in a real loss. Hence, healthy individuals were significantly less impulsive or careless when selecting real rewards than when selecting hypothetical fantasy rewards, whereas the equivalence of real and hypothetical discounting rates in the two PD groups may indicate poor calibration of behavioral responses to situational demands.
Our research studied stress reactions using self-reported responses to hypothetical situations, a procedure with far less ecological validity than procedures that induce feelings of interpersonal rejection or other upsetting experiences in the laboratory. The advantage to using a hypothetical stress scenario is that it does not expose participants to procedures involving deception by the researchers nor the deliberate triggering of intense distress. We felt this was an especially important consideration for our research, given that it was conducted with a BPD sample recruited from the community and not necessarily engaged in treatment. Nevertheless, the hypothetical nature of our stress-reactions measure remains a significant limitation because there are likely to be individual differences in the extent to which participants will vividly imagine the hypothetical stressful situation and accurately report how they would react to it.
A related limitation involves the fact that while we measured delay discounting and hypothetical stress reactions in the same sample, we did not examine delay discounting under different stress conditions. Although a prior study (Lawrence et al., 2010) did not find any effects of an interpersonal rejection induction on impulsive responding in the delay-discounting task in BPD, they did find that those with BPD failed to reduce impulsive responding after rejection (as the HC group did). Future work should consider this approach further.
The nature of the non-interpersonal stressor that we chose may not have been ideal for unexpected reasons. Having noticed during the experience-sampling portion of our research that participants with BPD expressed attachment to their palm-pilot diaries, we began to administer an adaptation of the Parasocial Interaction Questionnaire (Rubin, Perse, & Powell, 1985) and confirmed that indeed, those with BPD reported significantly stronger parasocial bonds to their palm-pilot diaries than did members of the HC group (MASKED REFERENCE). This finding raises the possibility that equipment failure may not be experienced by all individuals as equally “non-interpersonal,” because for some it may involve disruption of a parasocial attachment bond. Future research on reactions to non-interpersonal stressors may want to consider scenarios with less potential for a parasocial component.
Finally, future studies that involve asking participants to imagine interpersonal stressors in their own lives ought to further examine the nature of the relationships with the significant others that participants were envisioning. For example, it is possible that different types of relationships (e.g., romantic partner, close friend, or family member) are more strongly associated with maladaptive reactions to signs of disengagement and that the types of significant others selected may have differed across diagnostic groups. Further, the quality of the relationship with the significant other may also play a role in how that individual’s disengagement is interpreted and reacted to, and relationship quality may also vary with diagnostic group. Indeed, research on rejection sensitivity in nonclinical samples suggests that maladaptive reactions to potential rejection cues and poor relationship quality may each contribute to one another in a cyclical process (Downey, Freitas, Michaelis, & Khouri, 1998). It would be important to consider the extent to which individuals with BPD and APD may have more maladaptive reactions to interpersonal stressors, in part, because the relationships in which they experience these stressors may provide less support and more reasons for concern.
Acknowledgments
Compliance with Ethical Standards
This research was supported by National Institutes of Mental Health Grant (MASKED INFO.)
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Written informed consent was obtained from all individual participants included in this study.
This research was supported by National Institutes of Mental Health Grant R01 MH081948 to authors Downey, Rafaeli, and Berenson.
Footnotes
Conflict of interest disclosure form
Authors Gregory, Glaser, Romirowsky, and Yang declare that they have no conflict of interest.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th. Washington, DC: Author; 2013. [Google Scholar]
- Ayduk O, Mendoza-Denton R, Mischel W, Downey G, Peake P, Rodriguez M. Regulating the interpersonal self: Strategic self-regulation for coping with rejection sensitivity. Journal of Personality and Social Psychology. 2000;79:776–792. doi: 10.1037//0022-3514.79.5.776. [DOI] [PubMed] [Google Scholar]
- Ayduk OZayas V, Downey G, Cole AB, Shoda Y, Mischel W. Rejection sensitivity and executive control: Joint predictors of borderline personality features. Journal of Research in Personality. 2008;42:151–168. doi: 10.1016/j.jrp.2007.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berenson KR, Downey G, Rafaeli E, Coifman KG, Leventhal Paquin N. The rejection-rage contingency in borderline personality disorder. Journal of Abnormal Psychology. 2011;120:681–690. doi: 10.1037/a0023335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berenson KR, Gyurak A, Ayduk Ö, Downey G, Garner MJ, Mogg K, Pine DS. Rejection sensitivity and disruption of attention by social threat cues. Journal of Research in Personality. 2009;43:1064–1072. doi: 10.1016/j.jrp.2009.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bijttebier P, Vertommen H. Coping strategies in relation to personality disorders. Personality and Individual Differences. 1999;26:847–856. [Google Scholar]
- Brodsky BS, Groves SA, Oquendo MA, Mann J, Stanley B. Interpersonal Precipitants and Suicide Attempts in Borderline Personality Disorder. Suicide and Life-Threatening Behavior. 2006;36(3):313–322. doi: 10.1521/suli.2006.36.3.313. [DOI] [PubMed] [Google Scholar]
- Cawood CD, Huprich SK. Late adolescent self-injurious behavior: The roles of coping, self-esteem, and personality pathology. Journal of Personality Disorders. 2011;25:765–781. doi: 10.1521/pedi.2011.25.6.765. [DOI] [PubMed] [Google Scholar]
- Chapman AL, Dixon-Gordon KL, Layden BK, Walters KN. Borderline personality features moderate the effect of a fear induction on impulsivity. Personality Disorders: Theory, Research, and Treatment. 2010;1:139–152. doi: 10.1037/a0019226. [DOI] [PubMed] [Google Scholar]
- Chapman AL, Leung DW, Lynch TR. Impulsivity and emotion dysregulation in borderline personality disorder. Journal of Personality Disorders. 2008;22:148–164. doi: 10.1521/pedi.2008.22.2.148. [DOI] [PubMed] [Google Scholar]
- Coifman KG, Berenson KR, Rafaeli E, Downey G. From negative to positive and back again: Polarized affective and relational experience in borderline personality disorder. Journal of Abnormal Psychology. 2012;121:668–679. doi: 10.1037/a0028502. [DOI] [PubMed] [Google Scholar]
- Coffey SF, Schumacher JA, Baschnagel JS, Hawk LW, Holloman G. Impulsivity and risk-taking in borderline personality disorder with and without substance use disorders. Personality Disorders: Theory, Research, and Treatment. 2011;2:128. doi: 10.1037/a0020574. [DOI] [PubMed] [Google Scholar]
- Crean JP, de Wit H, Richards JB. Reward discounting as a measure of impulsive behavior in a psychiatric outpatient population. Experimental and Clinical Psychopharmacology. 2000;8:155–162. doi: 10.1037//1064-1297.8.2.155. [DOI] [PubMed] [Google Scholar]
- Crowne DP, Marlowe D. A new scale of social desirability independent of psychopathology. Journal of Consulting Psychology. 1960;24:349–354. doi: 10.1037/h0047358. [DOI] [PubMed] [Google Scholar]
- Downey G, Feldman SI. Implications of rejection sensitivity for intimate relationships. Journal of Personality and Social Psychology. 1996;70:1327–1343. doi: 10.1037//0022-3514.70.6.1327. [DOI] [PubMed] [Google Scholar]
- Downey G, Freitas A, Michaelis B, Khouri H. The self-fulfilling prophecy in close relationships: Rejection sensitivity and rejection by romantic partners. Journal of Personality and Social Psychology. 1998;75:545–560. doi: 10.1037//0022-3514.75.2.545. [DOI] [PubMed] [Google Scholar]
- First M, Gibbon M, Spitzer RL, Williams JBW. User’s guide for the Structured Clinical Interview for the DSM-IV Axis I Research Version. Washington, DC: American Psychiatric Press; 1996. [Google Scholar]
- First M, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. User’s guide for the Structured Clinical Interview for the DSM-IV Axis II Personality Disorders (SCID-II) Washington, DC: American Psychiatric Press; 1997. [Google Scholar]
- Gadassi R, Snir A, Berenson KR, Downey G, Rafaeli E. Out of the frying pan, into the fire: Mixed affective reactions to social proximity in borderline and avoidant personality disorders in daily life. Journal of Abnormal Psychology. 2014;123:613–522. doi: 10.1037/a0036929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gagnon J, Daelman S, McDuff P. Correlations of impulsivity with dysfunctional beliefs associated with borderline personality. North American Journal of Psychology. 2013;15:167–178. [Google Scholar]
- Hinvest NS, Anderson IM. The effects of real versus hypothetical reward on delay and probability discounting. The Quarterly Journal of Experimental Psychology. 2010;63:1072–1084. doi: 10.1080/17470210903276350. [DOI] [PubMed] [Google Scholar]
- Johnson MW, Bickel WK. Within-subject comparison of real and hypothetical money rewards in delay discounting. Journal of the Experimental Analysis of Behavior. 2002;77:129–146. doi: 10.1901/jeab.2002.77-129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirby KN, Petry NM, Bickel WK. Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. Journal of Experimental Psychology: General. 1999;128:78–87. doi: 10.1037//0096-3445.128.1.78. [DOI] [PubMed] [Google Scholar]
- Klonsky ED. What is emptiness? Clarifying the 7th Criterion for borderline personality disorder. Journal of Personality Disorders. 2008;22:418–426. doi: 10.1521/pedi.2008.22.4.418. [DOI] [PubMed] [Google Scholar]
- Lagorio CH, Madden GJ. Delay discounting of real and hypothetical rewards III: Steady-state assessments, forced-choice trials, and all real rewards. Behavioural Processes. 2005;69:173–187. doi: 10.1016/j.beproc.2005.02.003. [DOI] [PubMed] [Google Scholar]
- Lawrence KA, Allen JS, Chanen AM. Impulsivity in borderline personality disorder: Reward-based decision-making and its relationship to emotional distress. Journal of Personality Disorders. 2010;24:786–799. doi: 10.1521/pedi.2010.24.6.785. [DOI] [PubMed] [Google Scholar]
- Lawyer SR, Schoepflin F, Green R, Jenks C. Discounting of hypothetical and potentially real outcomes in nicotine-dependent and nondependent samples. Experimental and Clinical Psychopharmacology. 2011;19:263–274. doi: 10.1037/a0024141. [DOI] [PubMed] [Google Scholar]
- Limberg A, Barnow A, Freyberger HJ, Hamm AO. Emotional vulnerability in borderline personality disorder is cue specific and modulated by traumatization. Biological Psychiatry. 2011;69:574–582. doi: 10.1016/j.biopsych.2010.10.024. [DOI] [PubMed] [Google Scholar]
- Links PS, Heslegrave R, van Reekum R. Impulsivity: Core Aspect of Borderline Personality Disorder. Journal of Personality Disorders. 1999;13:1–9. doi: 10.1521/pedi.1999.13.1.1. [DOI] [PubMed] [Google Scholar]
- Madden GJ, Begotka AM, Raiff BR, Kastern LL. Delay discounting of real and hypothetical rewards. Experimental and Clinical Psychopharmacology. 2003;11:139–145. doi: 10.1037/1064-1297.11.2.139. [DOI] [PubMed] [Google Scholar]
- Matusiewicz AK, Carter AE, Landes RD, Yi R. Statistical equivalence and test-retest reliability of delay and probability discounting using real and hypothetical rewards. Behavioural Processes. 2013;100:116–122. doi: 10.1016/j.beproc.2013.07.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGlashan TH, Grilo CM, Skodol AE, Gunderson JG, Shea MT, Morey LC, Stout RL. The collaborative longitudinal personality disorders study: Baseline Axis I/II and II/II diagnostic co-occurrence. Acta Psychiatrica Scandinavica. 2000;102:256–264. doi: 10.1034/j.1600-0447.2000.102004256.x. [DOI] [PubMed] [Google Scholar]
- Meyer B, Ajchenbrenner M, Bowles DP. Sensory sensitivity, attachment experiences, and rejection responses among adults with borderline and avoidant features. Journal of Personality Disorders. 2005;19:641–658. doi: 10.1521/pedi.2005.19.6.641. [DOI] [PubMed] [Google Scholar]
- Morris EP, Stewart SH, Ham LS. The relationship between social anxiety disorder and alcohol use disorders: A critical review. Clinical Psychology Review. 2005;25:734–60. doi: 10.1016/j.cpr.2005.05.004. [DOI] [PubMed] [Google Scholar]
- Olsson I, Dahl AA. Avoidant personality problems - their association with somatic and mental health, lifestyle and social network: A community-based study. Comprehensive Psychiatry. 2012;53:813–821. doi: 10.1016/j.comppsych.2011.10.007. [DOI] [PubMed] [Google Scholar]
- Pfohl B, Blum N, Zimmerman M. Structured interview for DSM-IV personality (SIDP-IV) Washington DC: American Psychiatric Press; 1997. [Google Scholar]
- Rachlin H. Self-control. Behaviorism. 1974;2:94–107. [Google Scholar]
- Powers AD, Gleason MJ, Oltmanns TF. Symptoms of borderline personality disorder predict interpersonal (but not independent) stressful life events in a community sample of older adults. Journal of Abnormal Psychology. 2013;122:469–474. doi: 10.1037/a0032363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rallis BA, Deming CA, Glenn JJ, Nock MK. What is the role of dissociation and emptiness in the occurrence of nonsuicidal self-injury? Journal of Cognitive Psychotherapy: An International Quarterly. 2012;26:287–298. [Google Scholar]
- Reimers S, Maylor EA, Stewart N, Chater N. Associations between a one-shot delay discounting measure and age, income, education and real-world impulsive behavior. Personality and Individual Differences. 2009;47:973–978. [Google Scholar]
- Reynolds B, Schiffbauer R. Delay of Gratification and Delay Discounting: A Unifying Feedback Model of Delay-Related Impulsive Behavior. The Psychological Record. 2005;55:439–460. [Google Scholar]
- Romero-Canyas R, Downey G, Berenson K, Ayduk O, Kang J. Rejection sensitivity and the rejection-hostility link in romantic relationships. Journal of Personality. 2010;78:119–148. doi: 10.1111/j.1467-6494.2009.00611.x. [DOI] [PubMed] [Google Scholar]
- Rubin AM, Perse EM, Powell RA. Loneliness, parasocial interaction, and local television news viewing. Human Communication Research. 1985;12:155–180. [Google Scholar]
- Sauer C, Arens EA, Stopsack M, Spitzer C, Barnow S. Emotional hyper-reactivity in borderline personality disorder is related to trauma and interpersonal themes. Psychiatry Research. 2014;220:468–478. doi: 10.1016/j.psychres.2014.06.041. [DOI] [PubMed] [Google Scholar]
- Svaldi J, Philipsen A, Matthies S. Risky decision-making in borderline personality disorder. Psychiatry Research. 2012;197:112–118. doi: 10.1016/j.psychres.2012.01.014. [DOI] [PubMed] [Google Scholar]
- Torgersen S, Kringlen E, Cramer V. The prevalence of personality disorders in a community sample. Archives of General Psychiatry. 2001;58:590–596. doi: 10.1001/archpsyc.58.6.590. [DOI] [PubMed] [Google Scholar]
- Welch S, Linehan MM. High-risk situations associated with parasuicide and drug use in borderline personality disorder. Journal of Personality Disorders. 2002;16:561–569. doi: 10.1521/pedi.16.6.561.22141. [DOI] [PubMed] [Google Scholar]
- Wilberg T, Karterud S, Pedersen G, Umes Ø. The impact of avoidant personality disorder on psychosocial impairment is substantial. Nordic Journal of Psychiatry. 2009;63:390–396. doi: 10.1080/08039480902831322. [DOI] [PubMed] [Google Scholar]
- Yen S, Pagano M, Shea MT, Grilo C, Gunderson J, Skodol A, McGlashan T, Sanislow C, Bender D, Zanarini M. Recent life events preceding suicide attempts in a personality disorder sample: Findings from the Collaborative Longitudinal Personality Disorders Study. Journal of Consulting and Clinical Psychology. 2005;73:99–105. doi: 10.1037/0022-006X.73.1.99. [DOI] [PMC free article] [PubMed] [Google Scholar]