Abstract
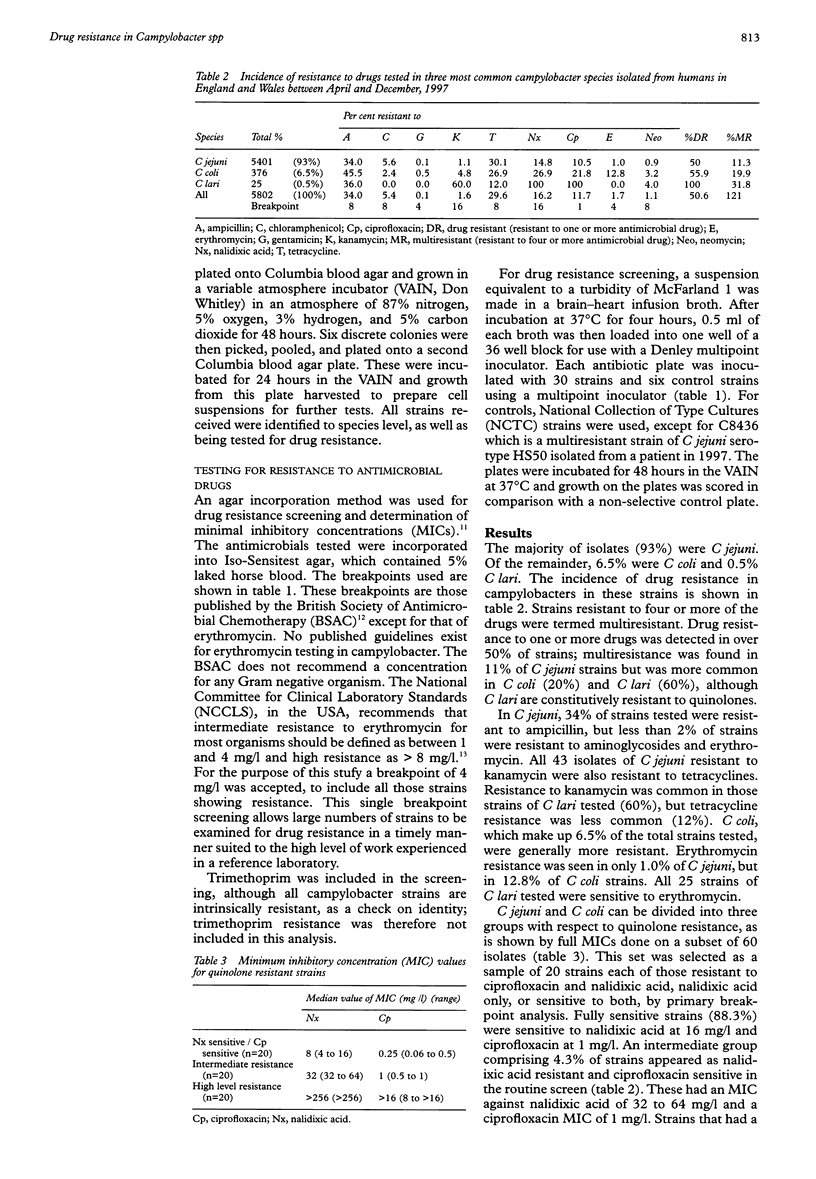
AIMS: To test the sensitivity of strains of Campylobacter species isolated from humans in England and Wales against a range of antimicrobial agents for the purpose of monitoring therapeutic efficacy and as an epidemiological marker. METHODS: An agar dilution breakpoint technique was used to screen isolates against ampicillin, chloramphenicol, gentamicin, kanamycin, neomycin, tetracycline, nalidixic acid, ciprofloxacin, and erythromycin. Minimal inhibitory concentrations (MIC) were also determined for a sample of quinolone resistant strains. RESULTS: Approximately 50% of strains tested were resistant to at least one drug. Strains which were resistant to four or more of the drugs tested were classified as multiresistant; this occurred in 11.3% of C jejuni, 19.9% of C coli, and 63.6% of C lari. Resistance to erythromycin occurred in 1.0% of C jejuni and 12.8% of C coli. Resistance to quinolones occurred in 12% of strains, with a ciprofloxacin MIC of > 8 mg/l and a nalidixic acid MIC of > 256 mg/l; a further 4% of strains had intermediate resistance with a ciprofloxacin MIC of between 0.5 and 2 mg/l (fully sensitive strains, 0.25 mg/l or less) and a nalidixic acid MIC of between 32 and 64 mg/l (fully sensitive strains, 8 mg/l or less). CONCLUSIONS: Resistance to quinolones in campylobacters from human infection may relate to clinical overuse or use of fluoroquinolones in animal husbandry. Both veterinary and clinical use should be reconsidered and fluoroquinolone drugs used only as a treatment for serious infections requiring hospital admission. Erythromycin resistance is still rare in C jejuni but much more common in C coli.
Full text
PDF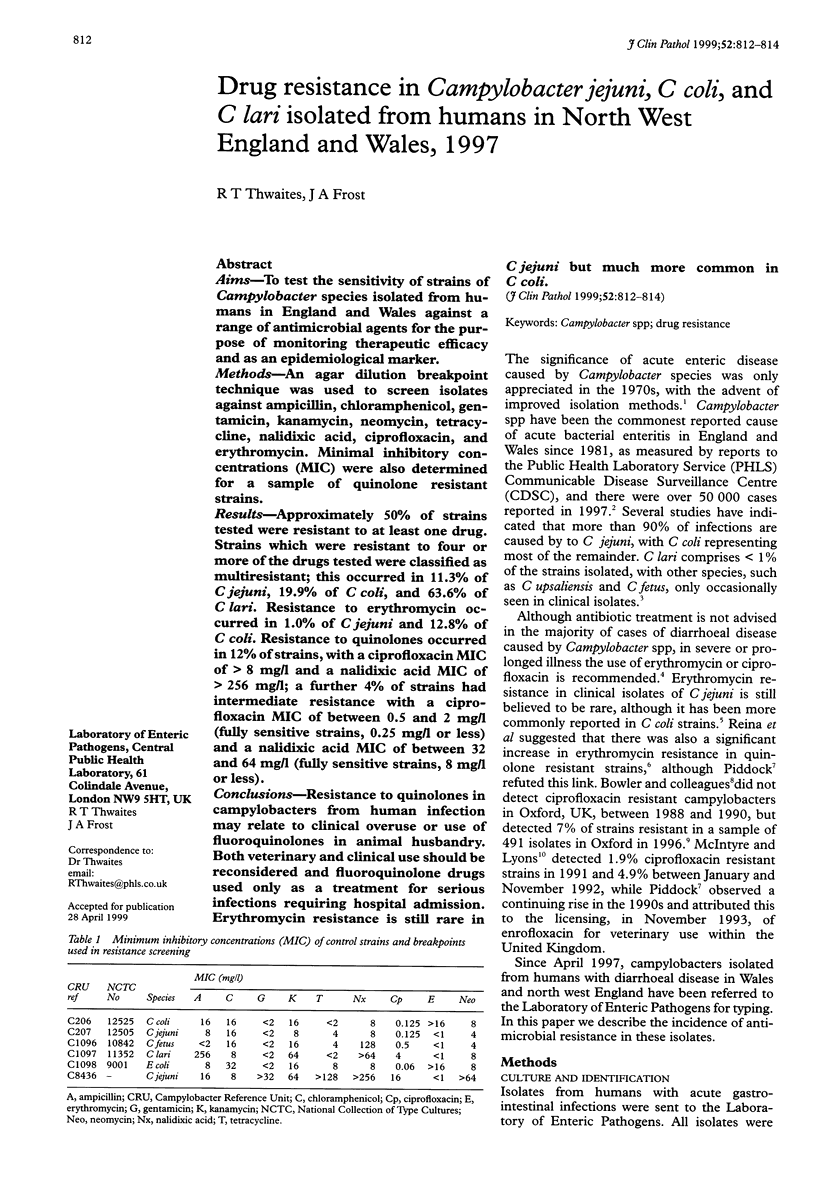

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bowler I. C., Connor M., Lessing M. P., Day D. Quinolone resistance and Campylobacter species. J Antimicrob Chemother. 1996 Aug;38(2):315–315. doi: 10.1093/jac/38.2.315. [DOI] [PubMed] [Google Scholar]
- Bowler I., Day D. Emerging quinolone resistance in campylobacters. Lancet. 1992 Jul 25;340(8813):245–245. doi: 10.1016/0140-6736(92)90517-7. [DOI] [PubMed] [Google Scholar]
- Frost J. A., Oza A. N., Thwaites R. T., Rowe B. Serotyping scheme for Campylobacter jejuni and Campylobacter coli based on direct agglutination of heat-stable antigens. J Clin Microbiol. 1998 Feb;36(2):335–339. doi: 10.1128/jcm.36.2.335-339.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gibreel A., Sjögren E., Kaijser B., Wretlind B., Sköld O. Rapid emergence of high-level resistance to quinolones in Campylobacter jejuni associated with mutational changes in gyrA and parC. Antimicrob Agents Chemother. 1998 Dec;42(12):3276–3278. doi: 10.1128/aac.42.12.3276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntyre M., Lyons M. Resistance to ciprofloxacin in Campylobacter spp. Lancet. 1993 Jan 16;341(8838):188–188. doi: 10.1016/0140-6736(93)90060-t. [DOI] [PubMed] [Google Scholar]
- Piddock L. J. Quinolone resistance and Campylobacter spp. J Antimicrob Chemother. 1995 Dec;36(6):891–898. doi: 10.1093/jac/36.6.891. [DOI] [PubMed] [Google Scholar]
- Reina J., Ros M. J., Fernandez-Baca V. Resistance to erythromycin in fluoroquinolone-resistant Campylobacter jejuni strains isolated from human faeces. J Antimicrob Chemother. 1995 Feb;35(2):351–352. doi: 10.1093/jac/35.2.351. [DOI] [PubMed] [Google Scholar]
- Reina J., Ros M. J., Serra A. Susceptibilities to 10 antimicrobial agents of 1,220 Campylobacter strains isolated from 1987 to 1993 from feces of pediatric patients. Antimicrob Agents Chemother. 1994 Dec;38(12):2917–2920. doi: 10.1128/aac.38.12.2917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skirrow M. B. Campylobacter enteritis: a "new" disease. Br Med J. 1977 Jul 2;2(6078):9–11. doi: 10.1136/bmj.2.6078.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skirrow M. B. Diseases due to Campylobacter, Helicobacter and related bacteria. J Comp Pathol. 1994 Aug;111(2):113–149. doi: 10.1016/s0021-9975(05)80046-5. [DOI] [PubMed] [Google Scholar]
- Tenover F. C., Elvrum P. M. Detection of two different kanamycin resistance genes in naturally occurring isolates of Campylobacter jejuni and Campylobacter coli. Antimicrob Agents Chemother. 1988 Aug;32(8):1170–1173. doi: 10.1128/aac.32.8.1170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Threlfall E.J., Ward L.R., Rowe B. Increasing incidence of resistance to trimethoprim and ciprofloxacin in epidemic Salmonella typhimurium DT104 in England and Wales. Euro Surveill. 1997 Nov;2(11):81–84. doi: 10.2807/esm.02.11.00187-en. [DOI] [PubMed] [Google Scholar]



