Abstract
Background
Mammograms, unlike magnetic resonance imaging (MRI), are relatively geographically accessible. Additional travel time is often required to access breast MRI. However, the amount of additional travel time and whether it varies based on sociodemographic or breast cancer risk factors is unknown.
Methods
We examine screening mammograms and MRIs between 2005 and 2012 in the Breast Cancer Surveillance Consortium (BCSC) by a) travel time to the closest and actual mammography facility used, and the difference between the two; b) woman's breast cancer risk factors and c) socio-demographic characteristics. We used logistic regression to examine the odds of traveling farther than the closest facility in relation to women's characteristics.
Results
Among 821,683 screening mammograms, 76.6% occurred at the closest facility compared to 51.9% of screening MRIs (N=3,687). The median differential travel time among women not using the closest facility for mammography was 14 minutes (IQR: 8-25) versus 20 minutes (IQR 11-40) for breast MRI. Differential travel time for both imaging modalities did not vary notably by breast cancer risk factors, but was significantly longer for non-urban residents. For non-Hispanic black, compared to non-Hispanic white women, the adjusted odds of traveling farther than the closest facility were 9% lower for mammography (OR 0.91; 95% CI:0.87-0.95), but more than two times higher for MRI (OR 2.64; 95% CI:1.36-5.13).
Conclusions
Breast cancer risk factors were not related to excess travel time for screening MRI, but sociodemographic factors were, suggesting the possibility that geographic distribution of advanced imaging may exacerbated disparities for some vulnerable populations.
Introduction
Mammography has been shown to be readily available in most geographic areas of the U.S. given its decades of diffusion and population-based need.1,2Studies reporting the influence of travel time to the nearest mammography facility on mammography utilization have found no significant association3. However, advanced breast imaging modalities, such as breast magnetic resonance imaging (MRI), have more limited geographic accessibility, 2 and may be imposing travel burdens on women who seek breast MRI examinations.
Breast MRI use has increased in the U.S. over the past decade for all clinical indications, including screening, preoperative assessment, treatment monitoring, and surveillance.4 Since 2007 when the American Cancer Society (ACS) released guidelines for use of breast MRI as an adjunct to screening mammography in women with a lifetime breast cancer risk of ≥20%5, use has accelerated4. In the U.S., this risk is met by an estimated 880,000 women6. Breast MRI's clinical benefits, combined with more limited geographic accessibility compared to mammography, raises the concern that travel burden may be a barrier to use of MRI by women who may benefit. Proximity to, and utilization of MRI may be related to breast cancer risk and sociodemographic factors.
Geographic access is often estimated as travel time based on the closest facility to a patient's residence. For breast cancer screening, most studies have measured the nearest mammography facility to women's locations2,7-12, with few studies measuring locations of facilities actually used by women.13 Understanding the travel time difference between the closest facility and that actually used will help to quantify the additional travel burden experienced by women seeking supplemental breast MRI screening, which will inform patterns of breast MRI use. For example, in a national sample, use of breast MRI was more common among women with breast cancer risk factors and less common among women from vulnerable populations.4 Travel time to breast MRI is greater than to mammography2 but whether this affects patterns of use for subpopulations is unknown.
Our objective was to examine whether clinical and sociodemographic characteristics of women in a breast screening population are associated with traveling farther than the nearest breast imaging facility when using mammography and breast MRI. We hypothesized that breast cancer risk factors may be associated with greater differential travel time to MRI since women with higher risk may be more willing to travel further for advanced imaging and that vulnerable populations would have greater differential travel time due to fewer advanced imaging services being located in proximity.
Methods
Study Population and Data
The study population included data from consenting women ages 30 and above in the National Cancer Institute (NCI)-funded BCSC with at least one screening breast exam from 2005-2012. The BCSC is comprised of population-based breast cancer screening registries in New Hampshire, New Mexico, North Carolina, San Francisco, Vermont, and Western Washington State.14 All participating sites within the BCSC have received institutional review board (IRB) approval for either active or passive consenting processes or a waiver of consent to enroll participants, link data, and perform analytic studies. All procedures are Health Insurance Portability and Accountability Act (HIPAA) compliant and all registries and the Statistical Coordinating Center (SCC) have received a Federal Certificate of Confidentiality and other protection for the identities of women, physicians, and facilities involved in this research.
Patient and Imaging Exam Characteristics
Information on women's breast cancer risk factors, breast screening history, and socio-demographics was captured at each breast imaging exam. Women self-reported demographic and clinical information such as date of birth/age, race/ethnicity, educational attainment, residential address, breast screening history, family and personal history of breast cancer, and history of breast procedures. Breast density and breast screening history was also recorded by radiologists and/or radiology technologists. The BCSC data also includes a calculated BCSC 5-year breast cancer risk score15 based on the combination of the risk factor information collected. Rurality of residence for each women was based on the 4-category Rural-Urban Commuting Area (RUCA) code corresponding to her ZIP code.16,17 We randomly selected one exam per type (mammography and MRI) per woman when multiple mammography or MRI exams were found within the study period and only included exams classified as screening examinations. Exams were classified as screening using standard definitions developed by the BCSC18 .The BCSC data record the facility at which each exam was performed.
Geocoded Data and Travel Time Measures
Addresses for women, for BCSC facilities visited by members of the study population, and for all Food and Drug Administration (FDA)-certified mammography facilities within the BCSC regions, were geocoded to street-level latitude and longitude point locations using ArcGIS version 10 (ESRI - Environmental System Research Institute, Redlands, CA). We created an Origin-Destination Matrix (O-D Matrix)19 by calculating the travel time for each woman to each breast imaging facility within her BCSC registry's catchment area, which allowed us to determine travel time to her closest facility, as well as travel time to the facility at which she had a breast imaging exam on record. The O-D Matrix was derived using ESRI's Origin-Destination Matrix tool in ArcGIS and its Streetmap North America road network dataset20. Travel times were calculated within a 180-minute travel time buffer from the woman's residential address. Women residing >180 minutes from either the closest or the facility actually used were excluded. Closest travel time was defined as the travel time in minutes from a woman's residence to the breast imaging facility with the least travel time from her residence. Actual travel time was defined as the travel time from a woman's residence to the facility at which she received a given breast exam. Differential travel time was defined as the difference between the closest and actual travel times. A differential travel time of zero indicates that the facility used for a given exam was the closest facility to a woman's residence. To account for small variations in street address for imaging facilities within a medical center campus, we considered a five minute or less differential travel time to represent use of the same/closest facility.
Statistical Analysis
We summarized the percent of exams occurring at the closest facility for all exams combined and by patient characteristics for both mammography and MRI. We calculated the median and interquartile range of differential travel time among women who did not use their closest facility for both mammography and MRI, overall and by patient characteristics. Additionally, we estimated cumulative distribution functions for actual travel time stratified by patient characteristics. Using multivariable logistic regression, we estimated likelihood of not using the closest facility in relation to clinical and sociodemographic characteristics: age, prior screening mammography, rurality, race/ethnicity, and educational attainment. In addition to adjusting for woman-level characteristics, we also adjusted for BCSC regional registry and facility characteristics: imaging and biopsy services offered, academic medical center, facility type (multispecialty, full diagnostic radiology, breast imaging only, non-radiology), profit/not-for-profit. All statistical analyses were conducted in R 3.1.221.
Results
Overall, 825,370 breast screening exams were included in the study (821,683 mammography; 3,687 breast MRI). (Table 1) The majority of women were: aged 50-69, non-Hispanic white, college graduates, urban residents, of average risk for breast cancer, screened within the past 30 months, not dense-breasted, and not having history of a breast procedure. (Table 1) Differences in the proportion of women receiving MRI compared to mammography were notable for race/ethnicity, education, rurality, and breast cancer risk. Specifically women of the following characteristics were represented much more in the MRI group relative to mammography: non-Hispanic white, college graduate or post-graduate education, urban residence, high risk of breast cancer, breast cancer screening in the past 30 months, dense breasts, positive family history of breast cancer, and prior breast biopsy. (Table 1) The median actual travel times for MRI exams and mammograms were 10 min. (IQR:5-20 min.) and 14 min. (IQR:6-32 min.), respectively. (Table 2) The greatest differences in actual travel times between MRI and mammography were seen by rural/urban category of residence.
Table 1.
Number and proportion of breast imaging exams by women's characteristics included in the study population from 2005-2012 in the Breast Cancer Surveillance Consortium.
| Mammogram (n=821,683) | MRI (n=3,687) | |
|---|---|---|
| Age (years) | N (%)* | |
|
|
||
| <40 | 28,137 (3.4) | 482 (13.1) |
| 40-49 | 222,061 (27.0) | 1,125 (30.5) |
| 50-59 | 241,697 (29.4) | 1,190 (32.3) |
| 60-69 | 178,486 (21.7) | 675 (18.3) |
| 70-79 | 102,551 (12.5) | 173 (4.7) |
| 80+ | 48,751 (5.9) | 42 (1.1) |
| Race/ethnicity | ||
| Non-hispanic white | 512,556 (71.3) | 2,843 (82.1) |
| Non-hispanic black | 45,639 (6.4) | 86 (2.5) |
| Non-hispanic Asian | 86,691 (12.1) | 307 (8.9) |
| Hispanic | 56,708 (7.9) | 121 (3.5) |
| Other | 16,945 (2.4) | 107 (3.1) |
| Education | ||
| < HS grad | 51,684 (9.1) | 49 (1.5) |
| HS grad or GED | 124,676 (22.0) | 310 (9.3) |
| Some College | 139,179 (24.5) | 596 (17.9) |
| College grad/post grad | 252,122 (44.4) | 2,377 (71.3) |
| Rural/Urban by Zip Code | ||
| Large Rural town | 117,783 (14.4) | 420 (11.4) |
| Small town/Isolated rural | 135,990 (16.6) | 556 (15.1) |
| Suburban | 60,579 (7.4) | 144 (3.9) |
| Urban Core | 506,426 (61.7) | 2,562 (70.0) |
| BCSC 5 year risk score | ||
| High Risk (>1.67) | 231,074 (37.1) | 827 (56.2) |
| Average Risk (<1.67) | 391,714 (62.9) | 644 (43.8) |
| Breast screening history | ||
| Screened in past 30 months | 585,063 (78.0) | 3,430 (95.5) |
| Not screened in past 30 months | 165,488 (22.0) | 161 (4.5) |
| Family history | ||
| Positive | 124,700 (15.2) | 1,869 (50.7) |
| Negative | 665,636 (81.0) | 1,707 (46.3) |
| Breast density | ||
| Almost entirely fatty | 41,326 (9.5) | 105 (3.7) |
| Scattered fibroglandular | 202,334 (46.4) | 881 (30.7) |
| Heterogeneously dense | 159,493 (36.5) | 1,334 (46.5) |
| Extremely dense | 33,247 (7.6) | 551 (19.2) |
| History of breast procedure | ||
| None | 590923 (79.0) | 782 (23.7) |
| Biopsy only | 112069 (15.0) | 1743 (52.7) |
| Aspiration only | 15590 (2.1) | 38 (1.1) |
| Both biopsy and aspiration | 29027 (3.9) | 743 (22.5) |
Missing values were as follows: Race/ethnicity: mammogram: 103,144 (12%), MRI: 223 (6%); Education: mammogram: 254,022 (31%), MRI: 355 (9%); Rural/urban: mammogram: 905 (0.1%), MRI: 5 (0.1%); BCSC 5 year risk score: mammogram: 198,895 (24%), MRI: 2,216 (60%); Breast screening history: mammogram: 71,132 (9%), MRI: 96 (3%); Family history: mammogram: 31,347 (4%), MRI: 111 (3%); Breast density: mammogram: 385,283 (47%), MRI: 816 (22%); History of breast procedure: mammogram: 74,074 (9%), MRI: 381 (10%).
Table 2.
Travel time to screening breast imaging exams recorded in the Breast Cancer Surveillance Consortium from 2005-2012 (N=825,370).
| Mammography (N=821,683) | MRI (N=3,687) | |||
|---|---|---|---|---|
|
| ||||
| Closest Travel Time | Actual Travel Time | Closest Travel Time | Actual Travel Time | |
|
|
||||
| Median time; IQR (min.) | Median time; IQR (min.) | |||
| All exams | 6 (3,13) | 10 (5,20) | 5 (2,13) | 14 (6,32) |
| Age (years) | ||||
| <40 | 6 (3,13) | 11 (6,23) | 5 (2,21.5) | 17 (5,55) |
| 40-49 | 7 (3,15) | 11 (6,24) | 6 (3,23) | 18 (7,66) |
| 50-59 | 7 (3,16) | 12 (6,24) | 6 (3,21) | 17 (8,52) |
| 60-69 | 7 (3,16) | 11 (6,23) | 7 (3,21) | 17 (7.5,49) |
| 70-79 | 6 (3,14) | 10 (5,20) | 7 (4,14) | 13 (7,45) |
| 80+ | 5 (2,11) | 8 (4,15) | 5.5 (3,15.25) | 7 (5,18.25) |
| Race | ||||
| Non-hispanic white | 8 (4,17) | 12 (6,24) | 7 (3,22) | 18 (7,55) |
| Non-hispanic black | 6 (3,14) | 11 (6,26) | 7.5 (3,17) | 23.5 (11.25,57) |
| Hispanic | 4 (2,6) | 9 (5,15) | 4 (3,8) | 12 (6,28.5) |
| Non-hispanic Asian | 5 (2,12) | 9 (5,21) | 5 (2,19) | 13 (7,41) |
| Non-hispanic Other | 6 (3,17) | 11 (5,25) | 7 (2,24.5) | 17 (8,68) |
| Education | ||||
| < HS grad | 5 (2,16) | 9 (4,22) | 5 (3,24) | 12 (5,41) |
| HS grad or GED | 8 (4,19) | 12 (5,25) | 13 (5,26) | 28 (12,65) |
| Some College | 7 (3,17) | 11 (5,25) | 7 (4,24) | 20 (9,57) |
| College grad/post grad | 6 (3,16) | 11 (5,23) | 6 (2,20) | 16 (6,50) |
| Rural/Urban by Zip Code | ||||
| Large Rural town | 9 (4,16) | 13 (5,25) | 12 (5,17) | 27 (7,57.25) |
| Small town/Isolated rural | 17 (7,28) | 22 (9,36) | 25 (13,33) | 53 (37,89) |
| Suburban | 19 (12,26) | 24 (16,33) | 19 (13,26.25) | 28 (22,41) |
| Urban Core | 5 (2,9) | 9 (5,15) | 5 (2,10) | 11 (6,25) |
| BCSC 5 year risk score | ||||
| High Risk (>1.67) | 8 (4,16) | 11 (6,23) | 7 (3,22) | 18 (7.5,52) |
| Average Risk (<1.67) | 7 (3,15) | 11 (6,23) | 6 (2,22) | 16 (6,49) |
| Breast screening history | ||||
| Screened in past 30 months | 7 (3,16) | 11 (6,24) | 6 (3,21) | 17 (7,51) |
| Not screened in past 30 months | 6 (3,14) | 10 (5,21) | 7 (2,24) | 18 (8,67) |
| Family history | ||||
| Positve | 7 (3,16) | 11 (6,23) | 6 (3,21) | 16 (6,49) |
| Negative | 7 (3,15) | 11 (6,23) | 6 (3,22) | 17 (8,57) |
| Breast density | ||||
| Almost entirely fatty | 7 (3,16) | 11 (5,23) | 10 (4,22) | 22 (9,42) |
| Scattered fibroglandular | 8 (4,16) | 11 (6,24) | 8 (3,23) | 20 (8,57) |
| Heterogeneously dense | 8 (4,16) | 12 (6,23) | 7 (3,21) | 17 (7,53.75) |
| Extremely dense | 7 (3,15) | 11 (6,23) | 6 (2,26) | 18 (6,70.5) |
| History of breast procedure | ||||
| None | 6 (3,15) | 11 (5,22) | 6 (2,21.75) | 16.5 (6,47) |
| Biopsy only | 7 (4,16) | 11 (6,23) | 6 (3,22.5) | 17 (7,63.5) |
| Aspiration only | 6 (3,14) | 11 (6,23) | 5 (4,11) | 18.5 (8.25,31) |
| Both biopsy and aspiration | 9 (4,20) | 12 (6,26) | 8 (3.5,22) | 18 (8,48) |
Cumulative probability distributions of actual travel time showed the proportion of women (vertical axis) with actual travel time less than or equal to the times given on the horizontal axis. When stratified by women's clinical breast characteristics, notably longer travel times were seen between mammography and MRI, but almost no differences within exam type by the clinical breast factors. (Figure 1) When plotting the cumulative probability functions by sociodemographic characteristics, we again saw a consistently greater travel time for MRI compared to mammography. We also observed marked differences in actual travel time to mammography and MRI by sociodemographic characteristics. For example, within MRI exams, the distribution of women's actual travel times varied markedly by rural-urban category of residence. (Figure 2) Actual travel time to mammography was the same by educational attainment level, but differed for MRI, with higher educational attainment showing a greater proportion of women with shorter travel times compared to lower educational attainment. (Figure 2) For age and race/ethnicity, small differences in actual travel time distributions can be seen, but these are not marked, and are similar for both mammography and MRI. (Figure 2)
Figure 1.
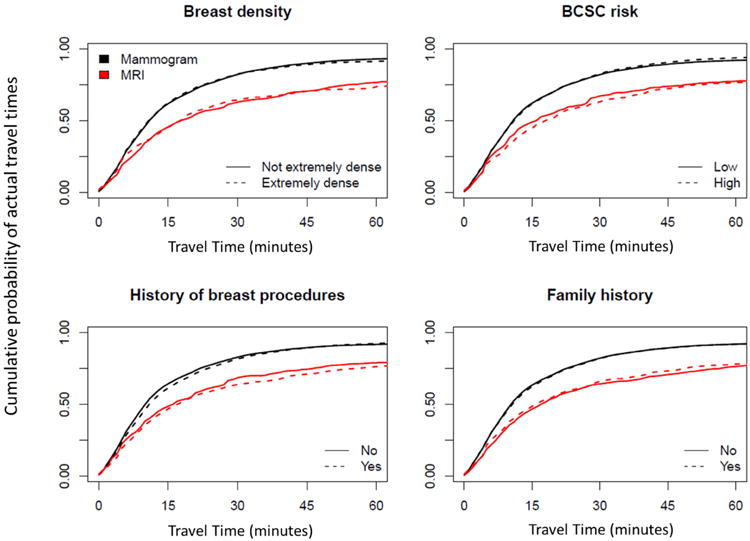
Cumulative probability of actual travel times for women (N=825,370) to breast imaging modalities in relation to breast cancer risk factors.
Figure 2.
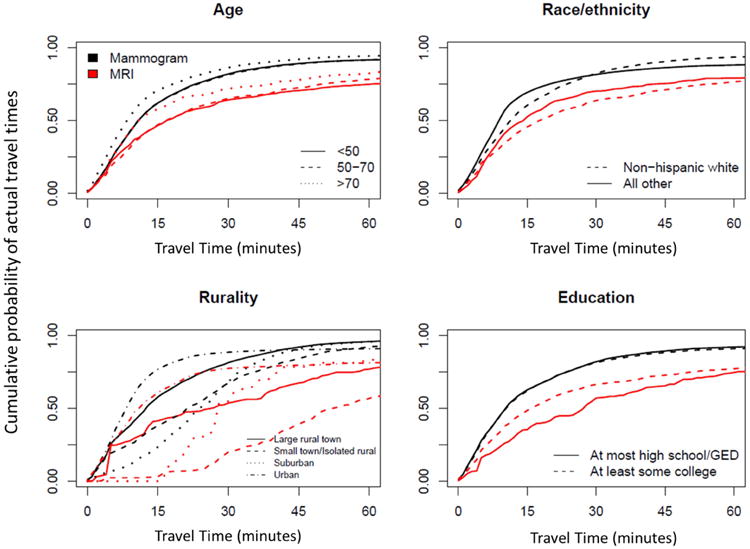
Cumulative probability of actual travel times for women (N=825,370) to breast imaging modalities in relation to sociodemographic factors.
For women receiving mammography screening, almost one quarter (23.4%) did not use their closest facility; whereas for MRI, almost half did not t use their closest facility (48.1%). (Table 3) For both mammography and MRI, older women, ages 70 and above, had lower proportions not using their closest facility. Non-Hispanic black women and women residing in small towns or isolated rural areas had the highest proportion not using the closest facility for MRI (64.9% and 75.9%, respectively), but this was not the case for mammography. (Table 3) For both mammograms and MRIs, the proportion of women using the closest facility did not vary notably by breast cancer risk factors.
Table 3.
Proportion of women not using their closest facility and for the subset not using the closes facility, differential travel time to screening breast imaging exams recorded in the Breast Cancer Surveillance Consortium from 2005-2012 (N=825,370).
| Mammography (N=821,683) | MRI (N=3,687) | |||
|---|---|---|---|---|
|
| ||||
| Not using closest* facility (%) | Differential travel time (min.); median (IQR) ** | Not using closest* facility (%) | Differential travel time (min.); median (IQR) ** | |
| All exams | 23.4 | 14 (8,25) | 48.1 | 20 (11,40) |
| Age (years) | ||||
| <40 | 29.6 | 15 (9,25) | 42.6 | 22 (13,38) |
| 40-49 | 25.8 | 14 (8,24) | 50.1 | 20 (11,40) |
| 50-59 | 24.7 | 14 (8,25) | 49.8 | 19 (11,39) |
| 60-69 | 22.7 | 14 (8,25) | 49.1 | 20 (11,41) |
| 70-79 | 18.9 | 13 (7,25) | 43.8 | 16 (10,45) |
| 80+ | 14.9 | 12 (7,23) | 15.4 | 8 (8,9) |
| Race | ||||
| Non-Hispanic white | 22.0 | 15 (9,26) | 47.5 | 22 (12,45) |
| Non-Hispanic black | 27.0 | 18 (10,31) | 64.9 | 25 (14,43) |
| Hispanic | 32.5 | 9 (6,14) | 46.9 | 13 (8,22) |
| Non-Hispanic Asian | 23.7 | 12 (7,22) | 50.0 | 12 (6,23) |
| Non-Hispanic Other | 24.7 | 13 (8,22) | 53.3 | 17 (7,27) |
| Education | ||||
| < HS grad | 19.2 | 10 (7,20) | 41.3 | 12 (8,46) |
| HS grad or GED | 19.8 | 15 (9,26) | 51.2 | 35 (19,56) |
| Some College | 23.8 | 15 (9,25) | 51.3 | 22 (11,45) |
| College grad/post grad | 24.8 | 14 (8,23) | 46.4 | 17 (10,35) |
| Rural/Urban by ZIP Code | ||||
| Large Rural town | 23.2 | 25 (13,35) | 51.9 | 34 (23,58) |
| Small town/Isolated rural | 23.1 | 23 (13,38) | 75.9 | 41 (23,67) |
| Suburban | 28.3 | 15 (9,24) | 57.9 | 20 (18,30) |
| Urban Core | 22.9 | 11 (7,17) | 39.5 | 14 (8,20) |
| BCSC 5 year risk score | ||||
| High Risk (>1.67) | 21.1 | 16 (9,27) | 49.1 | 20 (11,46) |
| Average Risk (<1.67) | 24.3 | 14 (8,25) | 41.6 | 20 (11,43) |
| Breast screening history | ||||
| Screened in past 30 months | 22.9 | 14 (8,25) | 47.3 | 19 (11,39) |
| Not screened in past 30 months | 23.5 | 13 (8,23) | 50.4 | 24 (13,48) |
| Family history | ||||
| Positive | 22.5 | 15 (8,25) | 45.6 | 20 (11,43) |
| Negative | 23.4 | 14 (8,25) | 50.0 | 19 (10,40) |
| Breast density | ||||
| Almost entirely fatty | 21.8 | 15 (8,25) | 45.7 | 22 (15,46) |
| Scattered fibroglandular | 22.6 | 16 (9,28) | 46.7 | 24 (14,46) |
| Heterogeneously dense | 24.4 | 15 (8,26) | 47.3 | 22 (12,43) |
| Extremely dense | 26.1 | 13 (7,22) | 48.5 | 18 (10,38) |
| History of breast procedure | ||||
| None | 23.1 | 13 (8,23) | 46.5 | 17 (9,33) |
| Biopsy only | 23.6 | 15 (8,26) | 49.6 | 19 (11,39) |
| Aspiration only | 27.3 | 15 (8,26) | 58.8 | 15 (7,21) |
| Both biopsy and aspiration | 21.1 | 17 (10,27) | 46.2 | 23 (13,46) |
Closest defined a s any facility within 5 minutes of geographical closest facility
Median and interquartile range (IQR) of differential travel time for subjects not using the c losest facility.
Among women who did not use their closest facility, median differential travel time was 14 min. (IQR:8-25 min.) for mammography and was 20 min. (IQR:11-40 min.) for MRI (Table 3). While overall, for almost all sociodemographic and breast characteristics, differential travel time to MRI was notably longer than to mammography, there was little variation in differential travel time across patient characteristics for most factors. (Table 3) The largest discrepancies in differential travel time between mammography and MRI were seen for women living in rural areas and those who had not been screened in the prior 30 months. The median differential travel time to mammography for women living in small towns or isolated rural areas was 23 min. (IQR:13-38 min.), but was much longer for MRI (median 41 min., IQR:23-67 min.). For women not screened in the past 30 months, median differential travel time to mammography was 13 min. (IQR:8-23 min.) and was 24 min. (IQR:13-48 min.) to MRI.
The likelihood of not using the closest facility significantly higher for all other rural/urban categories compared to urban core. This was evident for both mammography and MRI, with a much more pronounced effect in MRI. (Table 4) For example, women living in small towns or isolated rural areas were over three times more likely to use a facility other than their closest compared to women living in urban areas (OR:3.31;95% CI 3.21-3.42, urban reference). For MRI, women living in small towns or isolated rural areas were more than 14 times more likely than urban women to not use their closest facility (OR:14.06; 95% CI 9.49-20.81, urban reference). (Table 4) The association between race and differential travel time varied by imaging exam type. Specifically, for mammography, non-Hispanic black women were less likely to use a facility other than the closest compared to non-Hispanic white women (OR: 0.91; 95% CI 0.87-0.95; white reference). However, for MRI, non-Hispanic black women had over two times greater odds than non-Hispanic white women of not using the closest facility (OR:2.64;95% CI 1.36-5.13; white reference). (Table 4)
Table 4.
Likelihood (odds ratios and 95% confidence intervals) of not using the closest facility in relation to women's sociodemographic and clinical characteristics for screening breast imaging exams in the Breast Cancer Surveillance Consortium (2005-2012).
| Mammograms | MRI | |
|---|---|---|
|
| ||
| Patient characteristic | OR* (95% CI) | OR** (95% CI) |
| n = 419,446 | n= 2,973 | |
| Age (years) | ||
| <40 | 1.00 (ref) | 1.00 (ref) |
| 40-49 | 0.82 (0.77, 0.87) | 1.39 (1.06, 1.84) |
| 50-59 | 0.79 (0.74, 0.84) | 1.39 (1.05, 1.82) |
| 60-69 | 0.75 (0.70, 0.80) | 1.24 (0.92, 1.68) |
| 70-79 | 0.61 (0.57, 0.66) | 1.00 (0.65, 1.54) |
| 80+ | 0.48 (0.45, 0.52) | 0.24 (0.09, 0.69) |
| Screened in past 30 months | ||
| No | 1.00 (ref) | 1.00 (ref) |
| Yes | 1.01 (0.98, 1.04) | 0.80 (0.53, 1.21) |
| Rurality | ||
| Urban Core | 1.00 (ref) | 1.00 (ref) |
| Large Rural Town | 1.78 (1.73, 1.84) | 2.68 (1.79, 4.04) |
| Small Town/Isolated Rural | 3.31 (3.21, 3.42) | 14.06 (9.49, 20.81) |
| Sub-Urban | 1.34 (1.29, 1.39) | 5.27 (3.25, 8.54) |
| Race | ||
| Non-Hispanic White | 1.00 (ref) | 1.00 (ref) |
| Non-Hispanic Black | 0.91 (0.87, 0.95) | 2.64 (1.36, 5.13) |
| Asian | 1.09 (0.98, 1.22) | 1.18 (0.89, 1.57) |
| Hispanic | 0.82 (0.77, 0.88) | 1.26 (0.81, 1.96) |
| Other | 1.14 (1.07, 1.23) | 1.20 (0.75, 1.92) |
| Education | ||
| At most high school/GED | 1.00 (ref) | 1.00 (ref) |
| At least some college | 1.09 (1.07, 1.11) | 1.22 (0.92, 1.61) |
Adjusted for all patient, facility characteristics, and BCSC site
Adjusted for all patient characteristics and site
Discussion
This study is the first to examine differential travel time to mammography and breast MRI exams.As expected, we found longer actual travel times and greater differential travel times to breast MRI compared to mammography. Differential travel time for mammography and breast MRI did not vary notably according to breast cancer risk factors. However, sociodemographic factors – particularly rural residence, non-Hispanic black race/ethnicity, and lower educational attainment were associated with greater differential travel time for MRI.
This study augments prior work by: a) measuring travel time from women's residential locations to facilities actually used versus the closest; b) examining MRI in addition to mammography; c) including breast cancer risk factors, which may modify breast imaging needs and behaviors, and d) including individually-measured socio-demographic characteristics. This study provides novel evidence on potential travel burdens for breast MRI among subgroups of women participating in breast cancer screening, which is estimated to include approximately 67% of women age 40 and older in the U.S. 22
Travel time has been shown to be important to utilization of some breast cancer services, so our a priori hypothesis was that breast cancer risk factors might influence breast cancer screening with MRI. However, we did not find any risk factors or the quantitative breast cancer risk score to be significantly related to differential travel time to mammography or MRI. Thus, our findings do not support a role for risk in modifying travel behaviors for women undergoing breast cancer screening for either modality. Women may not know their individual breast cancer risk, so may not factor it into decision making.
There are several limitations in our study. First, we were limited to the BCSC screening population rather than the entire U.S. Given that we included over 800,000 women, who are largely representative of the breast cancer screening population23, we still have a population-based sample that is reasonably generalizable, although we recognize that some subgroups did not have large numbers using MRI, and were geographically clustered. Second, we included only screening exams, as clinical recommendations, patient motivations, and referral patterns can differ between screening and diagnostic indications, which are beyond the scope of this study. Third, we did not adjust for insurance in our multivariable models due to limited data availability. Fourth, we assumed that each woman had access to a vehicle and was not taking public transportation. This is a common limitation in travel time studies2,3,8-11,24-27. Finally, we do not have a validated measure of what constitutes an acceptable travel time for subgroups of women.
Our findings suggest that differential travel time may pose a burden for more rural women and black women, but not any more of a burden for women with breast cancer risk factors than without. The clinical implications of these findings point to a need to more closely examine equity in access to breast MRI for vulnerable populations. Further, attention should be given to ensuring that women at high risk for breast cancer are accessing breast MRI as needed.
Acknowledgments
We thank the participating women, mammography facilities, and radiologists for the data they have provided for this study. A list of the BCSC investigators and procedures for requesting BCSC data for research purposes are provided at: http://breastscreening.cancer.gov/. The collection of cancer and vital status data used in this study was supported in part by several state public health departments and cancer registries throughout the US. For a full description of these sources, please see: http://breastscreening.cancer.gov/work/acknowledgement.html”
This research was funded by the Breast Cancer Surveillance Consortium program project (P01CA154292) and NIH Grant T32 CA 9168-37. Data collection for this work was supported in part by additional funding from the National Cancer Institute (HHSN261201100031C, U54CA163303). “We thank the Norris Cotton Cancer Center's GeoSpatial Resource: http://cancer.dartmouth.edu/res/geospatial.html
Conflict of interest: Dr. Hubbard reports grants from NIH, during the conduct of the study; Dr. Lee reports grants from GE Healthcare, outside the submitted work.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Christoph I. Lee, Email: stophlee@gmail.com.
David Benkeser, Email: benkeser@uw.edu.
Jennifer Alford-Teaster, Email: paolajo@gmail.com.
Jennifer S. Haas, Email: JHAAS@PARTNERS.ORG.
Anna N. A. Tosteson, Email: Anna.N.A.Tosteson@dartmouth.edu.
Deirdre Hill, Email: dahill@salud.unm.edu.
Xun Shi, Email: Xun.Shi@dartmouth.edu.
Louise M. Henderson, Email: louise_henderson@med.unc.edu.
Rebecca A. Hubbard, Email: rhubb@mail.med.upenn.edu.
References
- 1.Celaya MO, Berke EM, Onega TL, et al. Breast cancer stage at diagnosis and geographic access to mammography screening (New Hampshire, 1998-2004) Rural and remote health. 2010 Apr-Jun;10(2):1361. [PMC free article] [PubMed] [Google Scholar]
- 2.Onega T, Hubbard R, Hill D, et al. Geographic access to breast imaging for US women. Journal of the American College of Radiology : JACR. 2014 Sep;11(9):874–882. doi: 10.1016/j.jacr.2014.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Onega T, Cook A, Kirlin B, et al. The influence of travel time on breast cancer characteristics, receipt of primary therapy, and surveillance mammography. Breast cancer research and treatment. 2011 Aug;129(1):269–275. doi: 10.1007/s10549-011-1549-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wernli KJ, et al. Patterns of breast magnetic resonance imaging use in community practice. JAMA internal medicine. 2014;174(1):125–132. doi: 10.1001/jamainternmed.2013.11963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saslow D, Boetes C, Burke W, Harms S, Leach MO, Lehman CD, Morris E, Pisano E, Schnall M, Sener S, Smith RA, Warner E, Yaffe M, Andrews KS, Russell CA. American Cancer Society Guidelines for Breast Screening with MRI as an Adjunct to Mammography†. CA: A Cancer Journal for Clinicians. 2007;57(2):75–89. doi: 10.3322/canjclin.57.2.75. [DOI] [PubMed] [Google Scholar]
- 6.Graubard BI, F A, Gail MH. Five-year and lifetime risk of breast cancer among U.S. subpopulations: implications for magnetic resonance imaging screening. CEBP. 2010;19(10):2430–2436. doi: 10.1158/1055-9965.EPI-10-0324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boscoe FP, Johnson CJ, Henry KA, et al. Geographic proximity to treatment for early stage breast cancer and likelihood of mastectomy. Breast (Edinburgh, Scotland) 2011 Aug;20(4):324–328. doi: 10.1016/j.breast.2011.02.020. [DOI] [PubMed] [Google Scholar]
- 8.Berke EM, Shi X. Computing travel time when the exact address is unknown: a comparison of point and polygon ZIP code approximation methods. International journal of health geographics. 2009;8:23. doi: 10.1186/1476-072X-8-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Elkin EB, Ishill NM, Snow JG, et al. Geographic access and the use of screening mammography. Medical care. 2010 Apr;48(4):349–356. doi: 10.1097/MLR.0b013e3181ca3ecb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Onega T, Duell EJ, Shi X, Wang D, Demidenko E, Goodman D. Geographic access to cancer care in the U.S. Cancer. 2008 Feb 15;112(4):909–918. doi: 10.1002/cncr.23229. [DOI] [PubMed] [Google Scholar]
- 11.Peipins LA, Graham S, Young R, et al. Time and distance barriers to mammography facilities in the Atlanta metropolitan area. Journal of community health. 2011 Aug;36(4):675–683. doi: 10.1007/s10900-011-9359-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Peipins LA, Miller J, Richards TB, et al. Characteristics of US counties with no mammography capacity. Journal of community health. 2012 Dec;37(6):1239–1248. doi: 10.1007/s10900-012-9562-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mobley LR, Kuo TM, Clayton LJ, Evans WD. Mammography facilities are accessible, so why is utilization so low? Cancer causes & control : CCC. 2009 Aug;20(6):1017–1028. doi: 10.1007/s10552-009-9295-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.(NCI) NCI. Breast Cancer Surveillance Consortium (BCSC) [Accessed 11/3/14];2014 http://breastscreening.cancer.gov/ 2014.
- 15.Consortium BCS. Breast Cancer Surveillance Consortium Risk Calculator. [Accessed July 24, 2015];2015 https://tools.bcsc-scc.org/BC5yearRisk/intro.htm.
- 16.Health WSDo. Guidelines for Using Rural-Urban Classification Systems for Public Health Assessment. [Accessed July 24, 2015];2009 http://www.doh.wa.gov/Portals/1/Documents/5500/RuralUrbGuide.pdf.
- 17.Washington TUo. WWAMI Rural Health Research Center. [Accessed July 24, 2015];2015 http://depts.washington.edu/uwruca/ruca-data.php.
- 18.(NCI) NCI. BCSC Glossary of Terms 2009; BCSC Glossary of Terms. [Accessed September 9, 2015]; [Google Scholar]
- 19.(ESRI) ESRI. Definition: origin-destination cost matrix. [Accessed July 24, 2015];2015 http://support.esri.com/en/knowledgebase/GISDictionary/term/origin-destination%20cost%20matrix.
- 20.TomTom North America I. US and Canada Detailed Streets (Version 2012-03-01) Redlands, California, USA: ESRI; 2007. [Google Scholar]
- 21.R: A language and environment for statistical computing. 2014 [Google Scholar]
- 22.(ACS) ACS. Breast Cancer: Mammography Statistics. [Accessed July 24, 2015];2015 http://www.cancer.org/research/infographicgallery/mammography-statistics.
- 23.Ballard-Barbash R, et al. Breast Cancer Surveillance Consortium: a national mammography screening and outcomes database. AJR Am J Roentgenol. 1997;169(4):1001–1008. doi: 10.2214/ajr.169.4.9308451. [DOI] [PubMed] [Google Scholar]
- 24.Onitilo AA, Liang H, Stankowski RV, et al. Geographical and seasonal barriers to mammography services and breast cancer stage at diagnosis. Rural and remote health. 2014 Jul-Sep;14(3):2738. [PubMed] [Google Scholar]
- 25.Huang B, Dignan M, Han D, Johnson O. Does distance matter? Distance to mammography facilities and stage at diagnosis of breast cancer in Kentucky. The Journal of rural health : official journal of the American Rural Health Association and the National Rural Health Care Association. 2009 Fall;25(4):366–371. doi: 10.1111/j.1748-0361.2009.00245.x. [DOI] [PubMed] [Google Scholar]
- 26.Kempe KL, Larson RS, Shetterley S, Wilkinson A. Breast cancer screening in an insured population: whom are we missing? The Permanente journal. 2013 Winter;17(1):38–44. doi: 10.7812/TPP/12-068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Henry KA, Boscoe FP, Johnson CJ, Goldberg DW, Sherman R, Cockburn M. Breast cancer stage at diagnosis: is travel time important? Journal of community health. 2011 Dec;36(6):933–942. doi: 10.1007/s10900-011-9392-4. [DOI] [PubMed] [Google Scholar]


