Abstract
Purpose
The purpose of this study was to evaluate the feasibility of a new web-based intermittent catheter self-management intervention.
Design
We tested the acceptability and usability of intervention components, which included multiple web-based materials (an online urinary diary adapted for mobile phone use and an educational booklet), three phone calls with a nurse, and a peer led discussion forum.
Subjects and setting
Thirty adults with spinal cord injury using an intermittent catheter for bladder drainage were enrolled; 26 participants received the nurses’ phone based consultations.
Methods
Preliminary effectiveness of new self-efficacy and self-management scales were evaluated using baseline and three month online surveys. Participants’ perceived value of the intervention components, self-management changes, and suggestions were assessed with data from the three month surveys followed by brief tape-recorded interviews.
Results
Several catheter practices improved somewhat over three months including. The frequency of catheterizations every 4–6 hours increased from 71% to 77%. Self-management of neurogenic bladder dysfunction increased significantly (P= .032); participant comments indicated that fluid intake was the biggest change. Catheter related self-efficacy and quality of life scores increased. The frequency of urinary tract infection and pain did not change significantly. For feasibility, intervention components, with the exception of the forum, were rated highly by the majority of participants for usefulness, satisfaction (desired information), and web-based usability.
Conclusion
Further testing of this intervention is recommended in a multi-site randomized clinical trial.
Keywords: web-based intervention, spinal cord injury, neurogenic bladder, urinary catheterization, intermittent catheter, urinary diary
Introduction
Intermittent catheterization (IC) is the bladder management method of choice for people with persistent urinary retention, including individuals with neurogenic bladder dysfunction caused by spinal cord injury (SCI). It is considered the “gold standard” for those who are able to perform catheterization several times a day.1 Often individuals with SCI are started with an intermittent catheter during their early stage of rehabilitation, but some find it difficult to sustain its use and resort to an indwelling catheter.2 Indwelling catheter users have higher rates of complications and hospitalization than people using IC.3 Indwelling catheter users are also prone to catheter encrustation and internal blockage or accidental dislodgement.4, 5
People using IC indefinitely, such as those with SC, must perform catheterization multiple times on a daily basis, self-monitor fluid intake and urinary output, and identify symptoms of urinary tract infection (UTI). They must also learn to preform IC in different locations and conditions, obtain catheters and supplies that suit their needs, and adjust to their changed social situation.6 Better self-management could help people with SCI sustain use of IC. While the internet is available to many people with SCI, research on the development of internet-based IC self-management interventions is lacking. The purpose of this article is to report results of a pilot study testing the feasibility of a new web-based intermittent catheter self-management intervention for adult with SCI.
Methods
The intervention was developed through the research team’s preliminary work involving qualitative interviews with 34 persons using IC, selected literature related to living with an intermittent catheter, modification of a previous intervention with long-term indwelling catheter users,7,8 and consultation with three advanced practice urologic/continence nurses. There were two phases in the study, development and pretesting9 and the pilot study reported in this article.
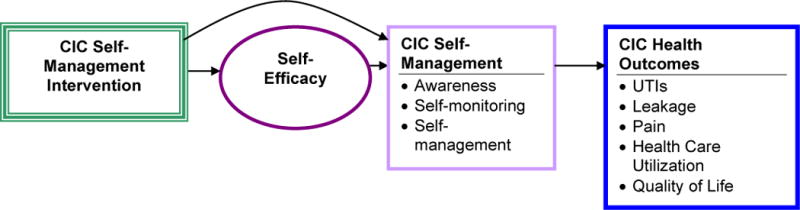
The purpose of the intervention was to teach awareness, self-monitoring (periodic measurements or observations),10 and self-management behaviors to improve adherence to IC frequency and to balance fluid intake with activity. These interventions are critically important in preventing the most common adverse effects of UTIs, urine leakage, and IC related pain and associated health care expenses (Figure 1). The intervention involved web-based information, mostly related to types and features of catheters and supplies, an online educational booklet, an interactive urinary diary for self-monitoring fluid intake and urinary output, three nurse phone call consultations, and peer led discussion forums. The 20 page educational booklet included basic information for self-management and problems and strategies, such as balancing fluids with activities, choosing the best interval for IC, finding suitable catheter supplies, travel, preventing leaking, and identifying symptoms of urinary tract infection. A full description of the intervention has been published previously.11
Fig. 1.
Theoretical model for Self-management of CIC Intervention
During the first pretesting phase of the study, a group of four study participants helped the researchers revise the intervention content. Changes included web site modification and development of mobile phone use mid-way through the pilot phase.9 Two people in the pretesting group continued in the pilot study as discussion leaders for the forums. They were trained together at a face-to-face meeting with the full team. The training involved structured content and a full discussion of possible issues in leading forums, such as sensitive concerns and how to address them. Study nurses also moderated the forums at least weekly to ensure accuracy of content.
The two study nurses were trained together using a manual that had been modified from an indwelling catheter study7 designed to enhance self-efficacy.12 A single study nurse completed all three telephone calls in most cases. During the first call the nurse and participant reviewed the online components, educational booklet, and use of the urinary diary. About a week later the nurse called to review the diary entries, make suggestions based on the data, identify additional web-based content or useful strategies in the educational booklet, and help set goals. The third phone call occurred about two months later; during the interaction, the nurse answered questions, identified barriers, and assisted with goal modification as indicated.
Personal health information in the urinary diary was protected and linked to our administrative site using a web-framework called Django (Django Software Foundation, Lawrence, Kansas). Study participants were able to view only their own urinary diary information. In contrast, discussion forums could be viewed by anyone enrolled in the study. The study nurse viewed participants’ diary information while conducting their phone call consultations and coached the person on how to use the diary. Although participants were asked to complete a 3-day, they were also encouraged to complete as many additional entries as desired. The interactive diary included several drop-down menus with date/time selection. For instance, when completing an intake entry, options for type/amount of fluid and caffeine (Yes/No) were available. For output, urine color and typical characteristics (e.g., mucus or sediment) could be selected. Tables and graphs with cumulative data were calculated automatically and displayed on other pages.
Measures
At the beginning of the study we collected self-reported data on demographics, medical diagnoses, time using IC, functional status, and medication information. At both time points, study participants were asked about catheterization procedures and care, including the frequency and intervals for catheterizing, average urine output estimate, and material sued to contract the catheter (substrate). Several measures related to catheter adverse events were used (e.g., UTI, leakage, catheter pain) based on the researchers’ qualitative study with IC users.6 In addition, an assessment was conducted on the feasibility (acceptance and usability) of the intervention, including analysis of quantitative and qualitative data from our 3 month survey and phone call interviews. Levels of functional ability were measured using the Katz scale13 which asks whether assistance is needed for each of bathing, dressing, toileting, transferring, and feeding self (independent =1; needs assistance =2). Cumulative scores range from 5 to 10; lower scores indicate a higher level of functioning. In addition, a single question was asked about whether a device or a person is needed for getting around.14 The item is scored from 0 to 5 where 0 indicates independently walking without a device or person assisting, 1 indicates using a device or human supervision, 2 indicates requiring assistance from another person at all times, 3 indicates confined to chair but wheeling independently, 4 indicates confined to a chair but unable to wheel self, and 5 indicates bedfast (unable to ambulate or be up in a chair).
Measures on self-efficacy and self-management were developed by the study team based on the researchers’: 1) qualitative study in IC users,6 2) measures used in a pilot15 randomized trial of self-management in people using indwelling catheters7 and 3) relevant literature. Seven new items related to IC content about their confidence to manage their catheter were added by the study team to the five Stanford Chronic Disease Self-Management Program (CDSMP; http://patienteducation.stanford.edu/) self-efficacy items. Additional content related to: adherence to IC frequency and expected volume the patient and provider consider appropriate, notice early symptoms of UTI, perform IC in different settings, choose equipment, and adjust to social needs (Table 3).
Table 3.
Measures – descriptive and change scores
| Measure & individual variables comprising measure | Mean/SD Baseline | Mean/SD 3 months | Change scores |
|---|---|---|---|
| Self-efficacy Scale (12 items) Stem: On a scale of 1–10, how confident are you that you can… (Higher numbers indicate higher self-efficacy.) | 8.07 (1.65) | 8.21 (1.22) | .01 (.90) P=.959 |
| SE1 Keep physical discomfort or pain of your disease from interfering with things you want to do | 7.39 (2.91) | 7.64 (2.17) | |
| SE2Keep the emotional distress caused by your disease from interfering with the things you want to do | 7.57 (2.76) | 7.73 (2.19) | |
| SE3 Keep any other symptoms or health problems you have from interfering with the things you want to do | 7.36 (2.93) | 7.76 (2.28) | |
| SE4 Do the different tasks and activities needed to manage your health condition so as to reduce your need to see a doctor | 8.57 (2.01) | 8.77 (1.38) | |
| SE5 Do things other than just taking medication to reduce how much your illness affects your everyday life | 8.36 (2.15) | 8.57 (1.25) | |
| SE6 Perform IC often enough to prevent urine leakage | 8.25 (1.88) | 8.77 (1.45) | |
| SE7 Monitor amount in catheterizations to keep level to acceptable amount | 7.61 (2.73) | 7.59 (2.20) | |
| SE8 Adjust fluid intake to prevent urine leakage & maintain hydration | 8.04 (2.20) | 7.91 (1.82) | |
| SE9 Notice early signs of UTI for quicker treatment | 8.32 (1.89) | 8.23 (1.82) | |
| SE10 Perform IC in different settings and situations | 8.57 (1.55) | 8.55 (1.57) | |
| SE11 Choose equipment to meet own needs | 8.86 (1.78) | 9.10 (.995) | |
| SE12 Adjust to social needs related to IC | 8.0 (2.36) | 8.05 (2.52) | |
| Self-management Scale (19 items) How often you do these activities, if at all. On a scale of 1–7 with 1 Not at all to 7 Do this very frequently or almost always. (Higher numbers are better.) | 4.80 (.88) | 5.11(.86) | .33(2.44) p=.032 |
| SMG 1 Pay attention to the amount of fluids consumed | 5.32 (1.95) | 5.86 (.990) | |
| SMG2 Make sure to drink enough fluids consistently throughout the day | 5.18 (1.63) | 5.45 (1.22) | |
| SMG3 Make sure to drink enough fluids consistently throughout the day | 5.68 (1.68) | 5.86 (1.61) | |
| SMG4 Keep track of fluid intake amount by writing it down | 1.46 (1.45) | 2.00 (1.75) | |
| SMG5 Pay attention to the urine such as color, odor and amount of urine | 6.21 (1.29) | 6.27 (1.03) | |
| SMG6 Pay attention to early signs of UTI | 5.96 (1.58) | 6.14 (1.36) | |
| SMG7 Contact the healthcare provider if an intermittent catheterization problem seems to be starting (such as UTI or blood in urine) | 5.82 (1.74) | 5.57 (1.63) | |
| SMG8 Ask the healthcare provided to assist with getting more or different types of catheters and supplies as needed | 4.89 (2.33) | 5.23 (2.07) | |
| SMG9 Write down information about IC related problems | 2.43 (2.20) | 3.00 (2.41) | |
| SMG10 Use the written information to make decisions about catheterization management | 2.64 (2.30) | 3.18 (2.52) | |
| SMG11 Plan for going out of the house by knowing where bathrooms are | 4.93 (2.23) | 5.50 (1.74) | |
| SMG12 Talk with other people to get support when the catheterizations are causing problems | 3.39 (2.44) | 3.82 (1.94) | |
| SMG13 Make adjustments for sex | 3.54 (2.44) | 4.48 (2.60) | |
| SMG14 Prevent serious symptoms of Autonomic Dysreflexia by recognizing early symptoms, taking action | 4.86 (2.38 | 5.19 (2.29) | |
| SMG15 Perform IC as often as you are supposed to do it (decided by your physician or a decision that both of you made) | 6.04 (1.23) | 5.68 (2.03) | |
| SMG16 Instead of doing IC, use absorbent products when social or other activities keep you from bathroom access*(reverse scored) | 5.18 (2.44) | 5.45 (2.22) | |
| SMG17(reverse scored) Instead of doing IC, skip it because it is too time consuming*(reverse scored) | 6.61 (1.10) | 6.64 (1.09) | |
| SMG18 Instead of doing IC, don’t go to social event if bathroom access is a concern*(reverse scored) | 4.8 (2.14) | 5.00 (1.83) | |
| SMG19 Instead of doing IC as often as I should, I do it less often because I worry about its effect on my bladder health*(reverse scored) | 6.21 (1.66) | 6.81 (.40) | |
| QOL Pinder et al. Psychological well- being scale (6 items) On a scale of 0–4, please tell us whether you agree or disagree with each of the following 6 questions related to your intermittent catheter, from strongly agree to strongly disagree. (Higher numbers indicate greater satisfaction/QOL) | 13.02 (6.91) | 13.86 (6.45) | 13.86 (6.45) P=.882 |
| P1 I am Self-conscious about need to self-catheterize | 1.79 (1.55) | 1.82 (1.53) | |
| P2 I would feel embarrassed if people saw catheter in its packet | 2.57 (1.55) | 2.82 (1.37) | |
| P3 My need to use a catheter sometimes makes me feel embarrassed | 2.29 (1.49) | 2.59 (1.56) | |
| P4 I worry that catheter doesn’t always empty bladder fully | 2.54 (1.29) | 2.29 (1.38) | |
| P5 My need to use catheters stops from visiting friends & family as often as likes | 2.32 (1.49) | 2.41 (1.56) | |
| P6 I worry about the risk of long term problems from using my catheter | 1.82 (1.49) | 1.91 (1.38) |
Indicates reverse scoring for single items in the Self-management Scale.
Self-management questions included 19 items measuring how often the IC related activities are performed, if at all (Table 3). The items were based on similar content categories as the IC related self-efficacy items; however, they were expanded to reflect the team’s theoretical framework that awareness and self-monitoring (through routine observations or recordings) contribute to self-management behaviors (Figure 1).
Health related quality of life (HRQOL) was measured via the ISC-Q Intermittent Self-Catheter Questionnaire, and the Psychological Well Being Scale (used with permission).34 This scale has six items related to embarrassment, worries, and interference with life. Reliability for this scale was reported as alpha .83; intra-class coefficient .849, P<0.001.16
The Feasibility Questionnaire used in the final survey was modified from the researchers’ pilot study on self-management in indwelling catheter users15 with additional items about acceptance: (useful, satisfied, bladder control) and usability (ease, efficiency, pleasant). A Qualitative Interview Guide was used to ask questions during the final three month tape recorded interview. Questions involved asking about: their overall impression of the study, mobile phone use, length of the intervention, the need for Information Technology (IT) assistance, study nurse contacts, improvements/suggestions, and what they might be doing differently.
Sample and Setting
The sample was recruited through online SCI websites linked to our recruitment website, a urological clinic, and a local SCI support group newsletter. In addition, the study coordinator made personal contacts with various National Spinal Cord Injury Association support group leaders, as well as a medical supply company that specializes in the needs of people with SCI. Other participants were referred by health care providers. Adults aged 18 years and over with neurogenic bladder dysfunction managed by IC for regular bladder drainage were eligible provided they expected to use IC for at least nine months and had use of a phone and computer during the study period. Study procedures were reviewed and approved by the University of Rochester Institutional Review Board for protection of human subjects.
Study Procedures
Potential participants were given an opportunity to view and discuss the recruitment website describing the study during an initial telephone call. The consent process was verbal, with online documents and an electronic consent by clicking a box “yes.” A hard copy of the verbal consent form was sent to the person by mail. Surveys were sent to participants electronically, supported through our university’s REDCap site.17 After receipt of the baseline survey, participants were given authorization, with user ID and password, to access the intervention website. The Project Coordinator (PC) sent the enrolled participant measuring supplies for the urinary diary recordings, i.e., a quart fluid intake measuring cup, a one liter urinary output beaker, non-latex gloves, and a screen shot on paper of the urinary diary.
The three month survey was emailed one month after the completion of the third study nurse phone call. For surveys not received within two weeks, a reminder email was sent. For a few whose non-response persisted, the PC contacted the participant by phone and the link to the survey was sent again if needed. The PC emailed participants to tell them we had received their survey and set up a time for a final phone call interview.
Data Analysis
All instruments for quantitative data were formatted prior to uploading into our University’s REDCap system. Numerical data were verified and processed for analysis using SPSS (ver. 19, IBM Corp. Armonk, NY). Tape recorded qualitative data from the interviews at the end of study participation were transcribed word for word, verified, and entered into Atlas Ti (ver. 7, Quality Software, Berlin, Germany) for content analysis Coding was conducted, with cross-verification, by two members of the team.
We used descriptive statistics for central tendency and dispersion, and calculation of scores and pre-post change scores for self-efficacy, self-management and quality of life measures. Outcomes of UTI, leakage, pain, and the frequency of and hours between catheterizations were examined for changes in the expected direction. To identify issues related to the program and to identify whether self-management learning had taken place, tape recorded transcriptions were content analyzed using Miles and Huberman’s approach in coding, memos, and an iterative process of data reduction and display in tables, conclusions and verification18.
Results
Thirty persons enrolled in the study, but one never returned the initial survey and was lost to follow up (Table 1). One individual withdrew at the beginning of the study citing time limitations, and two subjects were lost to follow up early. Thus, 26 participants completed the first phone call consultation, 25 completed the second phone call (one person’s catheter was discontinued), and 22 completed the third phone call. Twenty three completed surveys and 20 completed interviews.
Table 1.
Demographics of sample (N=29)
| n | % | |
|---|---|---|
| Gender | ||
| Male | 15 | 52 |
| Female | 14 | 48 |
| Age | ||
| Mean | 43.52 | |
| SD | 13.10 | |
| Median | 47 | |
| Race/Ethnicity | ||
| White | 21 | 72 |
| Black | 4 | 14 |
| Asian | 1 | 3 |
| More Than One Race | 3 | 10 |
| Not Hispanic | 28 | 97 |
| Hispanic | 1 | 3 |
| Marital Status | ||
| Married | 8 | 28 |
| Divorced | 6 | 21 |
| Never Married | 15 | 52 |
| Number of People in household | ||
| Four | 3 | 10 |
| Three | 4 | 14 |
| Two | 10 | 35 |
| One | 11 | 38 |
| Missing | 1 | 3 |
| Highest Ed Level | ||
| Vocational/Associates | 7 | 24 |
| HS/GED | 8 | 28 |
| Bachelors | 7 | 24 |
| Masters | 7 | 24 |
| Diagnosis | ||
| SCI Complete | 13 | 45 |
| SCI Incomplete | 13 | 45 |
| Other SC Disease | 3 | 10 |
| How Old is SCI | ||
| Less than 1 year ago | 1 | 3 |
| More than 1 year ago | 27 | 93 |
| Missing | 1 | 3 |
| Level of SCI | ||
| Cervical | 7 | 24 |
| Thoracic | 17 | 59 |
| Cervical/thoracic | 1 | 3 |
| Lumbar/Sacral | 2 | 7 |
| Thoracic/lumbar | 1 | 3 |
| Unknown | 1 | 3 |
| Insurance | ||
| Medicare | 18 | 62 |
| Medicaid | 11 | 38 |
| Private Insurance | 13 | 45 |
| VA | 1 | 3 |
| Currently Employed | ||
| No | 19 | 66 |
| Yes | 10 | 35 |
| Full Time (of those working) | 5 | 50 |
| ADL Bathing | ||
| Independent | 20 | 69 |
| Dependent | 9 | 31 |
| ADL Dressing | ||
| Independent | 24 | 83 |
| Dependent | 5 | 17 |
| ADL Toileting | ||
| Independent | 22 | 76 |
| Dependent | 7 | 24 |
| ADL Transfers | ||
| Independent | 23 | 79 |
| Dependent | 6 | 21 |
| ADL Feeding Self | ||
| Independent | 28 | 97 |
| Dependent | 1 | 3 |
| Medications | ||
| Bladder medicine–baclofen, ditropan or oxybutynine. | 13 | 45 |
| Lasix | 3 | 10 |
| OnabotulinumtoxinA | 3 | 10 |
| Muscle relaxant | 11 | 38 |
| Antibiotic | 8 | 28 |
| Nitrofurantoin | 2 | 7 |
| D-mannose | 2 | 7 |
| Methanomine mandelate/sodium acid phosphate (urine acidifier) | 1 | 3 |
The proportion of men to women participants was approximately equal)52% versus 48%); their mean age was 44 ± 13.1 years (Mean ± SD), median 47 years. It was a diverse sample by race and ethnicity, with 72% white, 14% black, 3% Asian, 10% more than one race, and 3% Hispanic. Five measures of activities of daily living, using the Katz scale,13 had a combined mean of 5.97 ± 1.6, range 5–10 (lower scores indicate more independent function). Most participants were chair-bound but wheeled independently (28 of 29), and one person was able to get around with an assistive device or another person. Multiple medications were used for bladder related conditions.
Catheter and Health Information
The length of time with a spinal cord injury was 16 ± 16 years (range 1–39, Table 2). Three participants reported having used an indwelling catheter (2 were suprapubic), 6 had used a condom catheter, 3 used the Credé maneuver (pressing on bladder) for bladder emptying. Eleven used absorbent products. The frequency of catheterizing at baseline varied from 2–9 times a day; the interval between catheterizations ranged from 2–12 hours. At three months, many persons reported changes in the intervals with more catheterizing every 2–3 hours. However, the majority did the procedure every 4–6 hours and 4–6 times a day at both time points.
Table 2.
Catheter information
| Catheter information | Intake | 3 Month | ||
|---|---|---|---|---|
| N= 29 | % | N= 23 | % | |
| Other Bladder Management Methods | ||||
| Indwelling | 9 | 31 | Asked at baseline only | |
| Suprapubic | 2 | 7 | ||
| Condom | 6 | 21 | ||
| Absorbent products | 11 | 38 | ||
| Crede | 3 | 10 | ||
| No Other Method Used | 8 | 28 | ||
| Frequency of Catheterizing Per Day (Average was used if a range was given) | ||||
| 2 | 2 | 7 | 1 | 5 |
| 4-6 | 20 | 71 | 17 | 77 |
| 7-9 | 6 | 21 | 4 | 18 |
| Hours Between Catheterizing (Average was used if a range was given) | ||||
| 2-3 | 2 | 7 | 6 | 27 |
| 4-6 | 22 | 76 | 13 | 59 |
| 12 | 3 | 10 | 1 | 5 |
| Varies | 1 | 3 | 2 | 9 |
| Typical Catheterizing Output (Average was used if a range was given) | ||||
| <100 | 2 | 7 | 2 | 9 |
| 100-399 | 13 | 45 | 10 | 46 |
| >400 and greater | 9 | 31 | 8 | 36 |
| Don’t Know | 3 | 10 | 2 | 9 |
| Missing | 1 | 1 | ||
| Mean | 323.4 | 355 | ||
| Median | 325 | 350 | ||
| SD | 147.94 | 145.86 | ||
| Range | 30-650 | 80-700 | ||
| Type of Catheter | ||||
| Plastic Not Coated | 10 | 35 | 9 | 41 |
| Hydrophilic | 5 | 17 | 4 | 18 |
| Silicone | 3 | 10 | 7 | 32 |
| Latex | 3 | 10 | 0 | 0 |
| Unknown | 7 | 24 | 2 | 9 |
| Frequency of urine leakage | ||||
| Daily | 3 | 12 | 4 | 24 |
| Several times a week | 7 | 28 | 2 | 12 |
| At least once a week | 5 | 20 | 4 | 24 |
| Several times a month | 4 | 16 | 0 | 0 |
| At least once a month | 3 | 12 | 3 | 18 |
| Once every two months | 3 | 12 | 4 | 24 |
| How Much a Problem is Leakage | ||||
| Not much | 10 | 35 | 11 | 65 |
| Moderate | 14 | 48 | 6 | 35 |
| Large | 1 | 3 | 0 | 0 |
Urinary incontinence between catheterizations was common at baseline (25 of 28, 89%), including 10 who experienced urine loss either daily or several times a week. At 3 months, 17 of 23 (74%) reported leakage, and 6 indicated they leaked daily or several times week. At baseline, catheterization pain was reported by 5 persons. Using a scale from 1–10 with 1 as ‘can hardly feel it’ to 10 meaning ‘very painful requiring a lot of distraction,’ two rated pain as a 2 or 3, one as 6, and 2 as 8 to10. At three months, three persons reported it as 4 or 5.
At baseline, 11of 26 participants (42%) reported having experienced a UTI within the previous three months for a total of 17 events (mean 0.65 ± 0.94). At 3 months, 7 of 23 (30%) reported UTI for a total of 10 events (mean 0.45 ± 0.74). No one reported being hospitalized for a UTI; however multiple missing responses may have influenced these findings.
Self-efficacy, Self-Management and HRQOL
The only statistically significant improvement was the IC self-management; mean scores increased 0.33 ±2.44 points, P= .032 (Table 3). A slight rise in mean IC self-efficacy scores was found but differences were not statistically significant. Scores for five of the six items in the intermittent catheter quality of life psychological well-being scale16 increased slightly (improved) and one decreased, but there was no significant change.
3 month Survey and Interview Results
A 3 month feasibility survey using quantitative items only is summarized in Tables 4 and 5. A majority of participants agreed or strongly agreed indicated that the intake and output diary, journal, educational materials, and calls with the nurse were useful (Table 4). However, responses to the forum were mixed; 41% agreed or strongly agreed the forum was useful. Seven of the 22 respondents (68%) used the mobile phone modifications; four rated it useful or satisfying; three indicated a neutral rating.
Table 4.
Feasibility Assessment at 3 months: Acceptability
| Did Not Use | Strongly Disagree | Disagree | Neutral | Agree | Strongly Agree | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Was the information useful? Do you agree or disagree related to each part of the program below? | ||||||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| I&O | 2 | 9 | 0 | 0 | 1 | 5 | 4 | 18 | 11 | 50 | 4 | 18 |
| Journal | 6 | 27 | 0 | 0 | 1 | 5 | 2 | 9 | 9 | 41 | 4 | 18 |
| Educational Materials | 1 | 4.5 | 0 | 0 | 1 | 4.5 | 2 | 9 | 12 | 55 | 6 | 27 |
| Calls with Nurse | 2 | 9 | 1 | 4.5 | 1 | 4.5 | 2 | 9 | 11 | 50 | 5 | 23 |
| Forum | 4 | 18 | 1 | 4.5 | 2 | 9 | 6 | 27 | 5 | 23 | 4 | 18 |
| Mobile Phone Modification | 15 | 68 | 0 | 0 | 0 | 0 | 3 | 14 | 2 | 9 | 2 | 9 |
| Were you satisfied with the parts of the program, meaning it gave you information that you wanted? | ||||||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | |
| I&O | 2 | 10 | 0 | 0 | 0 | 0 | 3 | 15 | 10 | 50 | 5 | 25 |
| Journal | 5 | 25 | 1 | 5 | 0 | 0 | 1 | 5 | 10 | 3 | 15 | |
| Educational Materials | 0 | 0 | 1 | 5 | 0 | 0 | 4 | 20 | 9 | 45 | 6 | 30 |
| Calls with Nurse | 2 | 10 | 1 | 5 | 0 | 0 | 2 | 10 | 10 | 50 | 5 | 25 |
| Forum | 5 | 24 | 1 | 4 | 2 | 10 | 5 | 24 | 4 | 19 | 4 | 19 |
| Mobile Phone Modification | 15 | 68 | 0 | 0 | 0 | 0 | 3 | 14 | 3 | 14 | 1 | 5 |
Table 5.
Feasibility assessment at 3 months: Usability
| None of the time | A little of the time | Some of the time | A good bit of the time | Most of the time | All of the time | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | n | % | n | % | |
| The program was easy to use… | 0 | 0 | 1 | 5 | 0 | 0 | 1 | 5 | 10 | 46 | 10 | 46 |
| Once I learned the program, I was able to move around the site to do what I wanted to do… | 1 | 5 | 0 | 0 | 1 | 5 | 0 | 0 | 5 | 23 | 15 | 68 |
| After not being on the website for a time, I was able to get back into it… | 1 | 5 | 0 | 0 | 0 | 0 | 0 | 0 | 8 | 36 | 13 | 59 |
| The website was pleasant to use, meaning it was visually attractive… | 2 | 9 | 0 | 0 | 1 | 5 | 2 | 9 | 7 | 32 | 10 | 46 |
| The mobile phone modification was pleasant to use, meaning it was visually attractive | 0 | 0 | 0 | 0 | 3 | 14 | 1 | 5 | 0 | 0 | 3 | 14 |
| I am in control of my bladder… | 0 | 0 | 0 | 0 | 1 | 5 | 7 | 32 | 13 | 59 | 1 | 5 |
Scores for the usability of the web-based information were high, with a majority of participants responding “most of the time” or “all of the time,” and again more variability and fewer who rated the forum highly. The seven who reported using the mobile phone modification rated it as pleasant to use (Table 5).
Comments received during the interviews at the end of the study about the overall program and website were mostly positive. People talked about how they liked the way it was planned and smoothly conducted. It was called a “positive thing; it helped me.” Another individual said it helped “open my eyes to certain things [like] I don’t’ drink enough.” People noticed that they do not always think about the catheter and their everyday lives. One recognized that that “it helped me get to know myself better…..and helped me socially. Now I feel more confident going to places knowing that I’m not going to be incontinent.” A few said that they did not find the information to be personally helpful due to many years’ IC use.
Mobile phone use was described positively by six of the seven who used it, but one person had difficulty in entering cumulative diary data. The length of the study was satisfactory to most, two thought it too lengthy, and five said it could have been longer. One person said that tracking 3 days for fluid intake and urine output was too short. One participant sought assistance from our IT research team member.
Most people enjoyed working with the study nurse. One individual said that “without the one-to-one, I wouldn’t have paid attention to the whole program.” Another person seemed to feel valued and liked “having somebody with a real true interest and really open to have an engaging, positive answer-finding discussion, rather than just taking the information and moving on.” Privacy in talking about personal issues was described as positive. When asked about the study nurse contacts, two people said they already knew the information that was provided because of years with IC.
Participants were asked about suggestions for program improvement. Two people said they would like a visual conversation with the study nurse, e.g. through Skype or FaceTime. One person wanted the mobile device application modified to automatically time and date-stamp each entry and also guide the participant through the intake and output recording process. All participants indicated they would recommend the program to others.
Changes in Self-Care Management
A final question was asked about changes in self-care because of participation in our program. Many people told us that while they had performed IC for a number of years, they had not tracked fluid intake and urine output since their initial rehabilitation days and they had not previously received the type of information to self-manage as in our study. One participant stated, “I think this [urinary diary] is very important and useful for any newly acutely injured individual. It at least gives them a basis on what to look for, how to do it. …Nobody ever tells us that in rehab …they just tell you try not to cath over 400…, [and] don’t go into the details that the self-management study did.” Participants also recognized that a journal could be useful for recognition of UTI symptom patterns.
Other changes included increased fluid intake and heightened awareness of how fluids affects them, trials of new catheter products, increased confidence, and adjusting the frequency of catheterization. One participant noted, “I’m probably more conscious of my intake of fluids than anything because I was one that was really slacking on taking fluids and …I needed to do something about it and I just sort of was lazy… And now I’m probably drinking 36 ounces of water a day.” Another indicated that the online forum provided information on getting new catheters instead of boiling and reusing them, and this gave him more confidence in performing IC. Leakage was of concern to one participant who stated she became more aware of the influence of time intervals between catheterizations.
Usage
Web site usage by participants was monitored and recorded for analysis. All pages of the educational booklet were viewed but every participant did not look at the whole booklet. The booklet pages pertaining to optimal fluid intake, best IC intervals and recognizing symptoms of UTI were viewed most often, which corresponded to the primary topics addressed during study nurse calls. Over half of the total time that participants spent on the website was devoted to use of the urinary diary; 67% marked their entries within 24 hours of the corresponding events.
Urinary Diary
Of the 26 participants who received the first phone consultation with the nurse, 21 recorded I&O for 3 consecutive days and 1 for two consecutive days. Four participants did not record any I&O data. Journal entries were recorded by 15 of the 22 who had tracked I &O: seven had 2 journal entries, and eight had 1 entry (range 1–4). Four persons “tried out” the website for a day prior to their 3-day tracking, and five persons added between one and four additional days (mean 3 days) of I & O tracking.
Forum
Eight of the 22 persons who received all three study nurse consultations and completed the urinary diary also participated in the forums. Ten people exhibited a wide range of activity in forum participation: four people posted once and one person posted 23 times to 8 different threads. Some topics generated as few as 2 posts, while others generated considerably more. The topical threads and posts were merged into similar categories: pre-lubricated catheters (5 posts), catheter supplies for travel (16), insurance issues (9), medications for incontinence (9), concerns about risks of cancer related to IC use (7), UTI (6), fluids (2), and treatments related to SCI (12), acupuncture (11), and onabotulinumtoxinA (5).
Discussion
The smaller sample size led to a low power to detect a small or medium effect rendered any non-significant results uninterpretable. Despite this low power, we did observe a single statistically significant effect on self-management improvement from baseline to post-intervention follow-up.
The percentage catheterizing in the desired frequency of 4–6 times a day1 had increased from 71–77% over three months, but the range of hours between that did not change from 2–12 times a day. It is hard to interpret what this means at a group level because some people might have needed to increase the frequency and/or hours between catheterizing and others might have needed to decrease them (Table 2). Our sample range in frequency of catheterizing was similar to those from a survey of elite international athletes with SCI (N=61) who catheterized an average of 6 ± 2 times daily; they also reported a range of catheterization 1–10 times/day.19
Many people experienced urine loss between catheterizations, and though it decreased a little from 89% to 74% over the three months, roughly 1/3 still experienced urinary incontinence daily or several times a week. Making adjustments in the types and amounts of fluids was the major self-management change reflected in the comments from the three months’ interviews. Urine leakage can interfere greatly with daily life, and in one study of 43 people using IC, 79% experienced it and over 1/3 of them had it daily.6 Therefore, it is not surprising that people might have adjusted their fluid intake to prevent leakage, and realized by self-monitoring I&O that more fluids were needed.
Catheter related pain decreased (including severe pain), but we do not know whether the participants did something differently to decrease it. The only change in health care utilization was that participants asked more questions of their provider.
Intervention Components
Tracking fluid intake and urine output was viewed positively by most participants (Table 4). Many comments were received on the three month interviews about how their initial rehabilitation had not provided enough information about how to balance intake and output with daily activities, and found this exercise was valuable. The educational booklet and study nurse contacts were also viewed favorably. Though the journal was not used often, a few people liked it. We had found similar results in our indwelling catheter study that the journal was the least used component.27
Nine of 22 participants (41%) indicated the forum was of interest to them, but participants who used the forum stated they enjoyed its presence. Forum entries often were read by people who had enrolled later in the study but did not post. Our timing of the forums might have interfered with more active participation because we used a continuing enrollment and did not always have a sufficient cohort at any one time, as in the study by Bloom and colleagues in which a group size of 10 was believed to sustain discussion.20 We also believe that the forum might be more active if tested using a larger sample or if the site went public. We had believed that people who participated fully with the urinary diary recordings and nurse contacts would also participate fully on the forums, but our data showed that only about 1/3 of the participants who had all three nurse contacts also posted to the forum. Therefore, forum participation could reflect individual preferences and capabilities that differ from nurse contacts and diary activities.
Our retention rate of 76% over the three months is similar to that of another online intervention study in which 79% were retained over the same time period, and our initial baseline assessment was completed by 93% as compared with 76% in the other study.20 However, these were very different types of research in that the Bloom and colleagues study targeted abused pregnant women.20
Limitations
Limitations include the small sample size and pre-post design, as compared with a randomized trial. Pretesting of measures and psychometrics were not conducted. Not all participants answered every question on the survey. While many people with SCI and neurogenic bladder dyfunction are younger and have computer access, not everyone has full hand capacity and a web-based intervention could interfere with interest and participation. Therefore, our self-selecting and small sample might not represent the population.
Conclusion
We suggest further testing of this intervention in a multi-site randomized controlled trial in SCI units across the country, particularly focusing on newly injured persons, but also including others with experience in IC who could share their knowledge and tips for healthy living. The web-based urinary diary could be compared with a paper and pencil version of it. Future implementation of the study web site should be modified to include logging/usage beyond that provided by default from web server logs to identify areas of less interest or those which could be improved. Finally, the IC self-efficacy and self-management scales require further development for use in large scale research.
Acknowledgments
We gratefully acknowledge our two research consultants on the study, Eun-Ok Im, PhD, RN and Wonshik Chee, PhD, both from the University of Pennsylvania, and Karen Genett, MS, RN, a faculty member at the School of Nursing, University of Rochester, with urological expertise who assisted us in recruitment and improvements in the educational materials. We sincerely appreciate the efforts of study participants who gave of themselves for this research.
Funding for the study has been provided by the National Institute of Nursing Research, National Institutes of Health (US) #R21 NR012763, the University of Rochester, School of Nursing, PI Wilde, Co-I McMahon. Funding for the mobile phone adaptation was provided by the Leary Fund.
Footnotes
Potential conflicts of interest: Dr. Wilde is a paid consultant for NovaBay Pharmaceutical and for research at the University of Southampton, England. No other authors have conflicts of interest.
References
- 1.Cottenden A, Bliss D, Buckley B, et al. Management using Continence Products. In: Abrams P, Cardozo L, Khoury S, Wein A, editors. Incontinence: 5th International Consultation on Incontinence. 5th. Arnheim, The Netherlands: ICUD-EAU Publishers; 2013. [Google Scholar]
- 2.Cameron AP, Wallner LP, Tate DG, Sarma AV, Rodriguez GM, Clemens JQ. Bladder management after spinal cord injury in the United States 1972 to 2005. J Urol. 2010;184:213–217. doi: 10.1016/j.juro.2010.03.008. [DOI] [PubMed] [Google Scholar]
- 3.Cameron AP, Wallner LP, Forchheimer MB, et al. Medical and psychosocial complications associated with method of bladder management after traumatic spinal cord injury. Arch Phys Med Rehabil. 2011;92:449–456. doi: 10.1016/j.apmr.2010.06.028. [DOI] [PubMed] [Google Scholar]
- 4.Wilde MH, Brasch J, Getliffe K, et al. Study on the use of long-term urinary catheters in community-dwelling individuals. J Wound Ostomy Continence Nurs. 2010;37:301–310. doi: 10.1097/WON.0b013e3181d73ac4. [DOI] [PubMed] [Google Scholar]
- 5.Wilde MH, McDonald MV, Brasch J, et al. Long-term urinary catheter users self-care practices and problems. J Clin Nurs. 2013;22:356–367. doi: 10.1111/jocn.12042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wilde MH, Brasch J, Zhang Y. A qualitative descriptive study of self-management issues in people with long-term intermittent urinary catheters. J Adv Nurs. 2011;67:1254–63. doi: 10.1111/j.1365-2648.2010.05583.x. [DOI] [PubMed] [Google Scholar]
- 7.Wilde MH, McMahon JM, McDonald MV, et al. Self-management intervention for long-term indwelling urinary catheter users: randomized clinical trial. Nurs Res. 2015;64:24–34. doi: 10.1097/NNR.0000000000000071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wilde MH, Zhang F, Fairbanks E, Shah S, McDonald MV, Brasch J. Perceived value of a urinary catheter self-management program in the home. Home Healthcare Nurse. 2013;9:465–473. doi: 10.1097/NHH.0b013e3182a89791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wilde MH, Fairbanks E, Parshall R, et al. Development of a Web-Based Self-management Intervention for Intermittent Urinary Catheter Users With Spinal Cord Injury. Comput Inform Nurs. 2015 doi: 10.1097/CIN.0000000000000182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wilde MH, Garvin S. A concept analysis of self-monitoring. J Adv Nurs. 2007;57:339–50. doi: 10.1111/j.1365-2648.2006.04089.x. [DOI] [PubMed] [Google Scholar]
- 11.Wilde MH, Fairbanks E, Parshall R, et al. A Web-based self-management intervention for intermittent catheter users. Urologic nursing. 2015;35:3. doi: 10.7257/1053-816X.2015.35.3.127:127-133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bandura A. Self-Efficacy: The Exercise of Control. New York: W. H. Freeman; 1997. [Google Scholar]
- 13.Katz S, Ford A, Moskowitz R, Jackson B, Jaffee M. Studies of Illlness in the aged. The index of ADL: A Standardized measure of biological and psychosocial function. JAMA. 1963;185:914–9. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 14.Centers for Medicare and Medicaid Services. US Outcome and Assessment Information Set. Available at: http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/OASIS/index.html?redirect=/oasis/01_overview.asp. Accessed February 4, 2015.
- 15.Wilde MH, Brasch J. Self-monitoring of urine flow in people with long-term urinary catheters. Res Nurs Health. 2008;31:490–500. doi: 10.1002/nur.20281. [DOI] [PubMed] [Google Scholar]
- 16.Pinder B, Lloyd AJ, Elwick H, Denys P, Marley J, Bonniaud V. Development and psychometric validation of the intermittent self-catheterization questionnaire. Clin Ther. 2012;34:2302–2313. doi: 10.1016/j.clinthera.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 17.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miles M, Huberman A. Qualitative Data Analysis. 2nd. Newbury Park, CA: Sage; 1994. [Google Scholar]
- 19.Krassioukov A, Cragg J, West C, Voss C, Krassioukov-Enns D. The good, the bad and the ugly of catheterization practices among elite athletes with spinal cord injury: a global perspective. Spinal Cord. 2014 doi: 10.1038/sc.2014.208. [DOI] [PubMed] [Google Scholar]
- 20.Bloom TL, Glass NE, Case J, Wright C, Nolte K, Parsons L. Feasibility of an online safety planning intervention for rural and urban pregnant abused women. Nurs Res. 2014;63:243–251. doi: 10.1097/NNR.0000000000000036. [DOI] [PubMed] [Google Scholar]


