Abstract
Objective
This study examined associations among health behaviors, psychosocial work factors, and health status.
Methods
Correctional supervisors (n=157) completed a survey that assessed interpersonal and organizational views on health. Chi-square and logistic regressions were used to examine relationships among variables.
Results
Respondents had a higher prevalence of obesity and comorbidities compared to the general U.S. adult population. Burnout was significantly associated with nutrition, physical activity, sleep duration, sleep quality, diabetes, and anxiety/depression. Job meaning, job satisfaction and workplace social support may predict health behaviors and outcomes.
Conclusions
Correctional supervisors are understudied and have poor overall health status. Improving health behaviors of middle-management employees may have a beneficial effect on the health of the entire workforce. This paper demonstrates the importance of psychosocial work factors that may contribute to health behaviors and outcomes.
INTRODUCTION
The reported health status of correctional employees is alarming. In 1984, the life expectancy of corrections officers (COs) was 59 years,1 and recent data suggests no significant improvement.2,3 The current life expectancy in the United States is 79 years.4 In Connecticut, male COs life expectancy trails that of other State workers by more than 12 years. Correctional employees face unique sources of job stress5,6 and have poor reported psychological health7,8 compared to other professional groups. Studies reporting on the health status of COs3,6,9,10 describe elevated rates of overweight, obesity, hypertension, and less healthy eating and exercise habits compared to the general population of U.S. adults.3,11
To date, the only existing research on correctional supervisor health has examined job stress;12,13 little else is known regarding their health status. Supervisory staff (including lieutenants, captains, and counselor supervisors) represent middle management and experience additional stress from job content that includes administrative responsibilities, lack of higher level support, and conflict resolution between officers.12,14
Challenging work environments have been linked to psychological,15,16 musculoskeletal,17 and behavioral processes18 that contribute to chronic disease risk.15-18 Numerous studies have reported associations between the workplace environment and health behaviors associated with chronic disease,19-23 such as nutrition,24-26 physical activity,27,28 and sleep.29-31
Understanding the psychosocial components of work such as burnout, job meaning, job satisfaction, and social support that may contribute to health behaviors and outcomes can guide the development of effective and sustainable health interventions. For correctional supervisors, a high-stress occupational group that experiences unique barriers to achieving optimal health, there is particular pertinence. Different health behaviors may coincide with one another, and therefore inclusion of multiple health behavior measures in research is warranted. The following section will provide a brief review of the literature relating to these variables.
Burnout
Working under high job demands, low control, low workplace support (i.e., coworker, supervisor), and a high effort-reward imbalance is particularly associated with the psychosocial construct of burnout.32 Burnout is a psychological term used to describe emotional exhaustion, detachment from occupational responsibilities and feelings of lack of accomplishment.33 Unhealthy behaviors such as uncontrolled and emotional eating,34 lack of physical activity,35,36 and sleep deprivation37,38 have been associated with burnout. Burnout is also linked to health outcomes, such as obesity and cardiovascular disease risk.34,36,39 Burnout in correctional officers has been studied5,40-43 and linked to increased sick leave, higher medical expenses, mental illnesses such as anxiety/depression,42 and lower life satisfaction.43 There is a deficiency of research on the physical and psychological impacts of work in correctional supervisors, a group that likely experiences elevated rates of burnout.
Job Meaning and Job Satisfaction
Job meaning or “meaningful work”, is the perceived value of the work experience that contributes to psychological well-being.44 This construct includes factors such as purpose and opportunities for growth.44 Job satisfaction includes current contentment with job responsiblities.45 Job meaning and job satisfaction have been linked to measures of mental health, well-being, and depression.46,47 Job satisfaction is linked to sleep disorders,48 depression,49 physical ailments, such as headaches and gastrointestinal problems,48 and mental health traits, such as anxiety, depression, and low self-esteem. However, findings are mixed in regards to job satisfaction and physical health outcomes.50 Correctional employees report decreases in job satisfaction coincident with job tenure.51
Workplace Social Support
Health behavior decisions are made in context of an individual's social environment. Coworker support describes feelings of psychosocial support by individuals in the work environment that may reduce job stress, improve safety climate and have positive associations with other work-factors such as job performance.52-54 Supervisor support describes engagement with supervisor staff through provision of resources, emotional support, and guidance. Sorensen et al. (1998) emphasize the importance of workplace social support in promoting health behavior change.55 Worksite environment and social influences may improve dietary habits56 and physical activity levels.18,57-60 Likewise, higher perceived supervisor support might be associated with improved sleep.61 Sleep habits may partly account for the relationship between work factors (job strain, supervisor support) and dietary habits.61
A high prevalence of obesity, hypertension and cardiovascular disease risk factors have been reported among corrections staff,3,6,11 but little is known about the health status or behaviors of correctional supervisors. Understanding work aspects that influence supervisors’ health will provide an opportunity to develop more effective and tailored interventions for this workgroup, which may eventually improve quality of life and life expectancy. Further, the findings from this study may have application to other public safety sector occupations that mandate physical fitness and good health as an occupational safety requirement going into the job (i.e., police, fire, EMS, etc.). The objectives of this study were to test the following hypotheses:
Hypothesis 1
Correctional supervisors exhibit: a) a high rate of unhealthy behaviors (nutrition, physical activity, sleep) and, b) worse health status, evidenced by a higher prevalence of chronic disease risk factors than the general adult population in the United States.
Hypothesis 2
Work characteristics (burnout, job meaning, job satisfaction, coworker support, supervisor support) will be associated with a) health behaviors (nutrition, physical activity, sleep duration, sleep quality) and b) health status measures (diabetes, hypertension, elevated cholesterol, anxiety/depression, obesity [BMI]) among correctional supervisors.
METHODS
Measures
This was a cross-sectional observational study examining health behaviors, health outcomes, and psychosocial work characteristics in supervisory staff (lieutenants, captains, counselor supervisors) within the Department of Corrections (DOC) in a northeastern state. As part of a participatory action research (PAR) project, a design team consisting of six correctional supervisors and two university researchers, developed a survey to enable the teams’ development of tailored health interventions for the correctional supervisors. The survey was administered in January 2015. Survey questions were developed using a PAR design in which university researchers and supervisors/union representatives contributed equally to ensure acceptability and feasibility of item content. The primary variables included: demographics, health behaviors, health status variables and work characteristics.
Demographic Variables
Age, sex, race, family income, educational level, marital status, job classification, shift, and weekly overtime were self-reported and explored in statistical analyses.
Health Behaviors
Nutrition, physical activity, sleep duration, and sleep quality were all self-reported using a Likert scale. Nutrition habits were assessed using the following question: “Nutrition experts recommend filling half your plate with fruits and vegetables at every meal and snacking occasion. How often do you meet this goal?” The question was adapted from the U.S. Dietary Guidelines for Americans (2010).62 A higher score is indicative of healthier dietary intake. Physical activity was assessed with the following question: “Health experts say that you should do strength training exercise twice a week plus do other activities that increase your heart rate and breathing on several days each week. How often do you meet this goal?” This question was adapted from the U.S. Department of Health and Human Services Physical Activity Guidelines for Americans (2010).63 A higher score is indicative of more frequent physical activity. Sleep duration was assessed by asking respondents, “During the work week, about how many hours of sleep do you typically get per 24-hour period?” Response choices included: 6 hours or less, about 7 hours, about 8 hours, about 9 hours, about 10 or more hours. This item was developed by investigators of the Center for the Promotion of Health in the New England Workplace (CPH-NEW).64 Lastly, sleep quality was assessed by asking participants to rate the quality of their sleep on a typical night on a scale ranging from 1 (very poor) to 4 (very good). This item was also developed by CPH-NEW investigators.64
Health Status
Four major health conditions and the respondents’ body mass index (BMI) were assessed by self-report. The four health conditions - elevated blood sugar or diabetes, hypertension, elevated cholesterol level, anxiety/depression - were characterized as ever diagnosed or currently requiring medication. Diagnosis and dose were combined as a single variable. That is, each of the four health conditions was coded dichotomously as 0 (no diagnosis received nor medication taken) and 1 (yes, diagnosis received and/or medication taken). The two factors were combined because of uncertainty, recognized in focus groups, over the distinction between curative treatment, which tended to censor an associated diagnosis, and compliance. Another uncertainty involved perception of having control over their condition resulting in poor medication adherence and compliance.65 Refinement of accuracy was deemed non-contributory. BMI was calculated from the reported height (in inches) and weight (in pounds) using the Centers for Disease Control and Prevention (CDC) formula below.66
Work Characteristics
All measures used to assess burnout, job meaning, job satisfaction, coworker support, and supervisor support used a Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree). A mean score was created by averaging the survey items for each construct. Burnout was assessed using the following 2 items: “More and more often, I talk about my work in a negative way” and “At work, I often feel emotionally drained.” This factored construct was developed by CPH-NEW investigators and has previously been used in surveys for correctional personnel.64 Spreitzer's (1995) measure of meaningful work, or job meaning was adopted.67 It includes the following 3 items: “The work I do is very important to me”, “My job activities are personally meaningful to me”, and “The work I do is meaningful to me.” Job satisfaction was assessed using the following 2 items: “All in all, I am satisfied with my job,” and “Overall I would recommend working with this organization to my family and friends.” These items were adapted from the Organizational Assessment Survey.68 Coworker support was assessed using the following 2 items: “The people I work with take a personal interest in me,” and “The people I work with can be relied on when I need help.” These items were adapted from the Job Content Questionnaire (Karasek et al., 1985).69 Lastly, supervisor support was assessed using the following 2 items: “My supervisor is concerned about the welfare of those under him/her,” and “My supervisor is helpful in getting the job done.” These items were adapted from the Job Content Questionnaire (Karasek et al., 1985).69
Sample
Participants were recruited using convenience sampling methods among membership of the supervisors’ bargaining unit. Of 452 invitations, a total of 157 individuals from 20 facilities completed the survey, providing a response rate of 35%. The survey was administered online and open over a four week period. Supervisors received access to the survey electronically via email. The voluntary, anonymous survey consisted of 64 items and took approximately 20 minutes to complete. Participants were assured that their responses were confidential and could not be linked to their name or employee identification number. This study was approved by the Institutional Review Board at the University of Connecticut. Participants provided consent electronically prior to beginning the survey.
Statistical Analyses
Data was analyzed using IBM SPSS™ version 21 to recode variables and create new variables (i.e., mean scores) and SAS version 9.3 for statistical test assumptions, descriptive statistics, frequency distributions, chi-square tests, and logistic regression. The primary variables analyzed included: demographic variables, health behaviors, health status including BMI, and work characteristics. Nonparametric tests were used when applicable due to the ordinal nature of the variables.70 However, new variables were also created from mean scores of Likert items and were treated as continuous variables, as this is considered an acceptable statistical approach.71,72
Key variables were assessed for normality and appropriate test assumptions prior to running statistical inference tests. Missing variables were excluded from syntax. The maximum number of participants excluded from any analysis due to missing data was two. Frequency analyses were run for categorical variables. Chi-square tests were performed to examine differences between categorical variables. Ordinal logistic regressions were used to evaluate continuous work-related variables as predictors of categorical health behavior and health outcome survey items. An odds ratio of greater than 1 was used as a cut-off to explain that the predictor variable was associated with higher odds of the outcome dependent variable.73 A p value of < 0.05 was set as the cut-off for statistical significance.
RESULTS
Descriptive Statistics
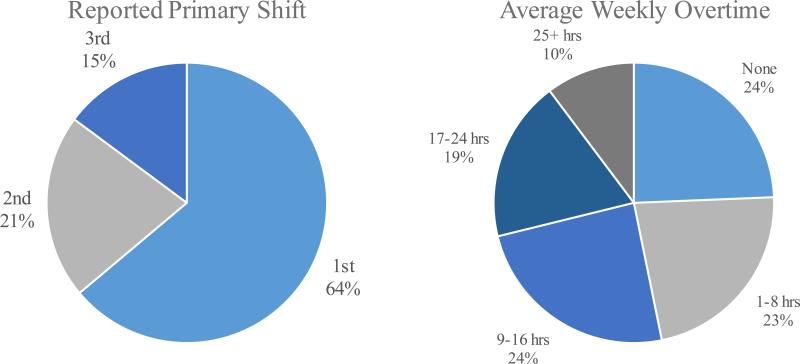
Demographic and anthropometric data are presented in Table 1. Over three-quarters of the sample were male (78.2%), and the mean [standard deviation (SD)] age was 42.3 [±6.1] years. The majority of participants had attained some college education (84.6%) and were married or living with their partner (73.0%). Almost two-thirds of respondents worked first shift (63.8%). Most were supervising lieutenants (59.6%), followed by captains and counselors. Almost one-third of participants reported doing at least 2 or more overtime shifts per week (Figure 1). Of respondents that worked two or more additional shifts per week, lieutenants worked most frequently (85.5%), followed by captains (12%), and then counselors (2.4%). These were statistically significant differences (p<0.001).
Table 1.
Demographic & Anthropometric Variables (n=157)
| Male | 78.2 % (n=122) |
| Female | 21.8% (n=34) |
| Age in years (mean ± SD) | 42.3 (±6.1) |
| Body Mass Index (BMI) (mean ± SD) | 30.1 (±4.6) |
| Underweight (<18.5) or Normal Weight (18.5-24.9) | 11.5% |
| Overweight (25.0-29.9) | 37.8% |
| Obese (≥30) | 50.6% |
| Race/Ethnicity | |
| White, European, or European American | 69.2% |
| Black, African American, or African | 16.0% |
| Hispanic, Latino or Hispanic American | 9.6% |
| Other | 3.2% |
| Asian, Asian American, or Pacific Islander | 1.3% |
| Middle Eastern, Arab, or Arab American | 0.6% |
| Education | |
| High school graduate or GED | 15.3% |
| Some college | 38.8% |
| College degree (2 or 4-year college) | 35.0% |
| Graduate degree | 10.8% |
| Marital Status | |
| Married or live with partner | 73.0% |
| Widowed | 1.9% |
| Divorced or separated | 16.0% |
| Single, never married | 8.9% |
| Family Income | |
| $50,000-74,999 | 1.3% |
| $75,000-99,999 | 24.5% |
| $100,000-124,999 | 29.7% |
| $125,000-149,999 | 15.5% |
| More than $150,000 | 29.0% |
| Job Classification | |
| Counselor Supervisor | 11.5% |
| Lieutenant | 59.6% |
| Captain | 28.8% |
Figure 1.
Distribution of shift and average weekly overtime among survey respondents (n=157).
Hypothesis 1
Health Behaviors
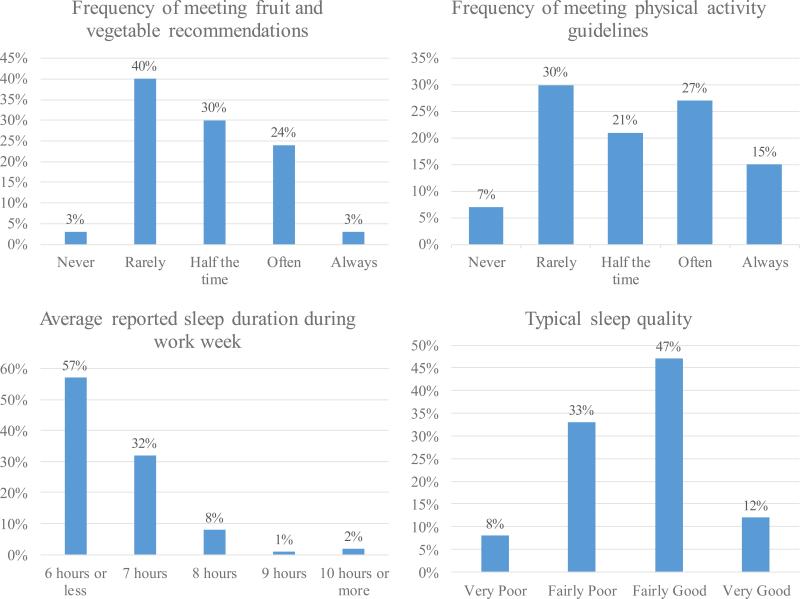
Frequency distributions were performed on categorical health behavior variables to assess the prevalence of unhealthy behaviors (see Figure 2). Analyses of survey item responses revealed that 43% of respondents reported never or rarely meeting the guideline for fruit and vegetable intake. Only 3% of respondents reported always meeting these guidelines. For comparison, findings from the Behavioral Risk Factor Surveillance System (BRFSS) conducted in the United States revealed 13.1% of adults consumed the recommended servings of fruit and 8.9% consumed the recommended servings of vegetables in 2013.74 Similarly, approximately 37% of respondents reported never or rarely meeting the guidelines for cardiorespiratory and resistance exercise and approximately 42% often or always meet these guidelines. In comparison, findings from the National Health Interview Survey in 2014 suggests that of U.S. adults over the age of 18, 49.2% meet recommendations for aerobic physical activity, and 20.8% meet recommendations for both cardiorespiratory and resistance activities.75 Over half the sample (57%) reported that they typically slept an average of 6 hours or less during the work week, which is less than the 7 to 9 hours that the National Sleep Foundation recommends adults over the age of 18 sleep per night.76 In comparison, findings from the 2014 BRFSS reveal that approximately 65% of US adults meet the recommended sleep guidelines of ≥ 7 hours per night.77 Further, 41% of respondents reported poor sleep quality. Consistent with Hypothesis 1a, survey respondents exhibited a high rate of unhealthy behaviors compared to US national data averages pertaining to nutrition, physical activity, sleep duration, and sleep quality.
Figure 2.
Distribution of health behaviors (nutrition, physical activity, sleep duration, sleep quality) among survey respondents (n=157).
Health Status
Corresponding to Hypothesis 1b, participants in this sample of supervisors were primarily overweight or obese - mean [SD] BMI 30.2 [±4.3] - with 37.8% of the participants being overweight and 50.6% being obese, formally surpassing the threshold for obesity. Table 2 provides a comparison to the US adult population, where the percentage of overweight and obesity is 33.6% and 34.9%, respectively.78 There was no significant difference in BMI by job class or shift. In addition, 10.2% of the sample reported being diagnosed with and/or taking medication for elevated blood sugar/diabetes. In comparison, 9.3% of the American population had diabetes in 2012.79 Of the total sample, 22.9% reported being diagnosed with and/or taking medication for high blood pressure (hypertension). This was lower than the national average of 29% in the National Health and Nutrition Examination Survey of 2011-2012.80 In addition, 24.2% of the sample reported being diagnosed with and/or taking medication for elevated cholesterol. This was nearly double the average adult percentage in the U.S. (13.4%).81 Of the total participants, 14.6% reported being diagnosed with and/or taking medication for anxiety/depression. In comparison, 3.1% of U.S. adults reportedly suffer from anxiety and 6.7% of adults suffer from depression.82 In summary, with the exception of hypertension, which was not adjusted for age, survey respondents exhibited a higher prevalence of chronic diseases than the general adult population in the United States, which is consistent with Hypothesis 1b.
Table 2.
Comparison of health status between study sample and general U.S. adult population
Hypothesis 2
Health Behaviors
Chi-square tests were performed to examine the relationships between measured health behaviors. In general, nutrition and physical activity behaviors were significantly associated with each other (p<0.001). Participants reporting “never” meeting nutrition recommendations were more likely to also report never meeting physical activity recommendations. Nutrition behavior was significantly associated with sleep quality (p<0.05), but not sleep duration (p=0.32). Participants reporting “often” or “always” meeting nutrition recommendations were more likely to report good sleep. Physical activity behavior was not associated with sleep duration (p=0.66) or sleep quality (p=0.47). Reported sleep duration and sleep quality shared a significant association (p<0.01). Participants reporting “very poor” quality sleep were most likely to report sleeping 6 hours or less per night.
Health Behaviors and Work Characteristics
Logistic ordinal regression tests were used to test Hypothesis 2a and examine associations between mean scores of psychosocial work characteristics, the independent variables (IVs) and health behaviors, the dependent variables (DVs). Burnout was significantly associated with nutrition, physical activity, sleep duration and sleep quality. A one-unit increase in burnout was associated with a 0.35 increase in the odds of a lower nutrition score (indicating less frequently meeting nutrition guidelines), with an odds ratio of 0.71 (95%CI: 0.54, 0.92), p<0.05. Similarly, a one-unit increase in burnout was associated with a 0.39 increase in the odds of lower physical activity, with an odds ratio of 0.68 (95%CI: 0.52, 0.88), p<0.01. No other work characteristics (job meaning, job satisfaction, coworker support, supervisor support) were significantly associated with nutrition or physical activity.
Job satisfaction and coworker support were significantly associated with sleep duration. A one-unit increase in job satisfaction was associated with a 0.41 increase in the odds of higher reported hours of sleep, with an odds ratio of 1.5 (95%CI: 1.01, 2.24), p<0.05. Higher coworker support more than doubled the odds (OR=2.25, 95%CI: 1.40, 3.61) of greater reported sleep duration (p<0.01). All work characteristics (burnout, job meaning, job satisfaction, coworker support, supervisor support) were significantly associated with sleep quality. Positive work characteristics were associated with better sleep quality, evidenced by a positive parameter estimate, whereas burnout was associated with poor sleep quality, evidenced by a negative parameter estimate. Higher job satisfaction (OR=2.12, 95%CI: 1.46, 3.08, p<0.001) and coworker support (OR=2.39, 95%CI: 1.58, 3.63, p<0.001) were associated with more than double the odds of better sleep quality. Table 3 summarizes the associations between work characteristics and health behaviors. In summary, burnout was associated with most health behaviors (nutrition, physical activity, sleep duration, sleep quality); job satisfaction and coworker support were associated with sleep duration; and all work characteristics (burnout, job meaning, job satisfaction, coworker support, supervisor support) were associated with sleep quality. The results are consistent with Hypothesis 2a.
Table 3.
Associations between work characteristics and health behaviors
| Dependent Variable | Independent Variable | Model χ2 | Parameter Estimate (±SE) | p value | Odds Ratio | 95% Confidence Interval |
|---|---|---|---|---|---|---|
| Nutrition | Burnout | 6.66 | −0.35 ±0.14 | 0.010** | 0.71 | 0.54, 0.92 |
| Job Meaning | 2.35 | 0.27 ±0.18 | 0.125 | 1.32 | 0.93, 1.87 | |
| Job Satisfaction | 0.00 | 0.01 ±0.18 | 0.946 | 1.01 | 0.72, 1.42 | |
| Coworker Support | 3.12 | 0.35 ±0.20 | 0.078 | 1.42 | 0.96, 2.10 | |
| Supervisor Support | 0.01 | −0.01 ±0.15 | 0.930 | 0.99 | 0.73, 1.33 | |
| Physical Activity | Burnout | 8.79 | −0.39 ±0.13 | 0.003** | 0.68 | 0.52, 0.88 |
| Job Meaning | 0.05 | 0.04 ±0.17 | 0.824 | 0.96 | 0.69, 1.34 | |
| Job Satisfaction | 3.52 | 0.32 ±0.17 | 0.061 | 1.38 | 0.99, 1.94 | |
| Coworker Support | 2.63 | 0.31 ±0.19 | 0.105 | 1.37 | 0.94, 1.99 | |
| Supervisor Support | 0.35 | 0.09 ±0.15 | 0.554 | 1.09 | 0.81, 1.47 | |
| Sleep Duration | Burnout | 6.73 | −0.38 ±0.15 | 0.009** | 0.68 | 0.51, 0.91 |
| Job Meaning | 0.39 | −0.12 ±0.19 | 0.534 | 0.89 | 0.62, 1.28 | |
| Job Satisfaction | 4.10 | 0.41 ±0.20 | 0.043* | 1.51 | 1.01, 2.24 | |
| Coworker Support | 11.11 | 0.81 ±0.24 | 0.001** | 2.25 | 1.40, 3.61 | |
| Supervisor Support | 2.80 | 0.29 ±0.17 | 0.094 | 1.34 | 0.95, 1.88 | |
| Sleep Quality | Burnout | 34.44 | −0.92 ±0.16 | <0.0001** | 0.40 | 0.29, 0.54 |
| Job Meaning | 5.45 | 0.42 ±0.18 | 0.020** | 1.53 | 1.07, 2.18 | |
| Job Satisfaction | 15.73 | 0.75 ±0.19 | <0.0001** | 2.12 | 1.46, 3.08 | |
| Coworker Support | 16.79 | 0.87 ±0.21 | <0.0001** | 2.39 | 1.58, 3.63 | |
| Supervisor Support | 12.73 | 0.59 ±0.17 | 0.0004** | 1.80 | 1.30, 2.49 |
p < 0.05
p < 0.01
Health Status and Work Characteristics
Binomial logistic regression tests were used to test Hypothesis 2b and evaluate associations between mean scores of work characteristics, the independent variables (IVs) and health status measures, as dependent variables (DVs). Obesity (BMI>30) was an additional variable used to examine relationships between comorbidities. Table 4 provides logistic regression results. Burnout and job satisfaction were significantly associated with elevated blood sugars/diabetes. A one-unit increase in mean burnout score was associated with a 0.60 greater odds of diabetes risk, with an odds ratio of 1.80 (95%CI: 1.10, 3.03), p<0.05. In contrast, job satisfaction was protective against diabetes, as evidenced by a negative parameter estimate (β=−0.56, p<0.05). Burnout was also significantly associated with anxiety/depression, and a one-unit increase in burnout was associated with a 0.67 increase in nearly double the odds of having anxiety/depression, with an odds ratio of 1.90 (95%CI: 1.25, 3.03), p<0.01. Supervisor support was protective against anxiety/depression (β=−0.53, p<0.05). No work characteristics were significantly associated with hypertension or elevated cholesterol in this sample. Elevated BMI was significantly associated with diabetes (p<0.05) and hypertension (p<0.01) but not with elevated cholesterol (p=0.14) or anxiety/depression (p=0.35). In summary, with the exception of work characteristics sharing associations with hypertension or elevated cholesterol, some work characteristics (burnout, job satisfaction, supervisor support) were associated with diabetes and anxiety/depression. The results are consistent with Hypothesis 2b.
Table 4.
Associations between work characteristics and BMI and health status measures
| Dependent Variable | Independent Variable | Model χ2 | Parameter Estimate | p value | Odds Ratio | 95% Confidence Interval |
|---|---|---|---|---|---|---|
| Elevated blood sugar/diabetes | Burnout | 5.456 | 0.60 ±0.26 | 0.020* | 1.83 | 1.10, 3.03 |
| Job Meaning | 0.00 | −0.01 ±0.31 | 0.971 | 0.99 | 0.54, 0.97 | |
| Job Satisfaction | 3.91 | −0.56 ±0.28 | 0.048* | 0.57 | 0.33, 0.99 | |
| Coworker Support | 2.20 | −0.49 ±0.33 | 0.138 | 0.62 | 0.32, 1.17 | |
| Supervisor Support | 0.16 | 0.12 ±0.29 | 0.687 | 1.12 | 0.64, 1.97 | |
| BMI | 5.97 | 0.15 ±0.06 | 0.015* | 1.16 | 1.03, 1.31 | |
| Hypertension | Burnout | 1.85 | 0.24 ±0.17 | 0.174 | 1.27 | 0.90, 1.78 |
| Job Meaning | 0.30 | −0.12 ±0.22 | 0.584 | 0.89 | 0.58, 1.37 | |
| Job Satisfaction | 1.28 | 0.28 ±0.24 | 0.257 | 1.32 | 0.82, 2.12 | |
| Coworker Support | 0.04 | 0.05 ±0.25 | 0.844 | 1.05 | 0.64, 1.73 | |
| Supervisor Support | 0.00 | 0.01 ±0.20 | 0.957 | 1.01 | 0.68, 1.50 | |
| BMI | 11.32 | 0.17 ±0.05 | 0.001** | 1.18 | 1.07, 1.30 | |
| Elevated cholesterol | Burnout | 0.42 | 0.11 ±0.17 | 0.519 | 1.11 | 0.80, 1.55 |
| Job Meaning | 0.01 | 0.02 ±0.22 | 0.916 | 1.02 | 0.66, 1.56 | |
| Job Satisfaction | 0.05 | 0.05 ±0.22 | 0.829 | 1.05 | 0.68, 1.63 | |
| Coworker Support | 0.11 | −0.08 ±0.25 | 0.744 | 0.92 | 0.57, 1.50 | |
| Supervisor Support | 0.08 | 0.06 ±0.20 | 0.776 | 1.06 | 0.72, 1.56 | |
| BMI | 2.15 | 0.06 ±0.04 | 0.143 | 1.07 | 0.98, 1.16 | |
| Anxiety/depression | Burnout | 8.66 | 0.67 ±0.23 | 0.003** | 1.95 | 1.25, 3.03 |
| Job Meaning | 0.44 | −0.17 ±0.26 | 0.509 | 0.85 | 0.51, 1.39 | |
| Job Satisfaction | 0.01 | −0.03 ±0.27 | 0.920 | 0.97 | 0.58, 1.65 | |
| Coworker Support | 0.23 | −0.14 ±0.29 | 0.631 | 0.87 | 0.49, 1.55 | |
| Supervisor Support | 5.52 | −0.53 ±0.22 | 0.019* | 0.59 | 0.38, 0.92 | |
| BMI | 0.88 | 0.05 ±0.05 | 0.348 | 1.05 | 0.95, 1.16 |
p < 0.05
p < 0.01
DISCUSSION
Correctional institutions are often located in desolate areas, food choices are limited to take-out food or vending machines, and employees often have long work days due to mandated overtime or rotating shifts. In addition, correctional employees experience unique job stress, psychological demands, and little job control. These factors and many others put correctional employees at high-risk of comorbid conditions influencing their longevity and health-related quality of life. These individual costs also unfavorably affect the employer and society. This present study is a considerable addition to what is admittedly a sparse existing literature on workplace and health associations in correctional supervisors. Previous studies are particularly limited in their exploration of the psychosocial environment and its’ impact on health.
Public safety sector occupations, such as corrections, that require new recruits to perform at high levels of fitness and health, have a positive baseline for maintaining and improving health of all employees. The hierarchical organizational structure also provides supervisors with opportunity to model behavior for lower-ranked employees. There are studies that emphasize the role of middle-management in improving lower ranked employees’ physical83,84 and mental health85 in other sectors. In the correctional employee literature, several studies have highlighted the role of supervisor support, suggesting that these middle managers can be instrumental in reducing occupational stress86,87 and burnout,88 improving job satisfaction,89 increasing organizational commitment among COs, and potentially reducing job turnover.90 Despite the prominent role of supervisors in supporting the health of other employees, limited literature exists examining their health status and potential relationships among health behaviors, health outcomes, and work characteristics.
Health Behaviors and Health Status of Supervisors
A large percentage of the sample in this study reported not meeting nutrition recommendations, physical activity recommendations or sleep guidelines compared to data averages on US adults. Nutrition behavior shared associations with physical activity and sleep quality. This is consistent with previous studies reporting relationships between nutrition, exercise,91 and sleep quality.92 Correctional supervisors in this study exhibited poorer health status than the general U.S. population. Over 85% of the sample was overweight or obese, a contributing risk factor to cardiovascular disease. Potential explanations for the elevated rates of obesity in supervisor staff may be related to job tasks promoting sedentary behavior and the level of job responsibilities may interfere with leisure time physical activity.
Participants in this study reported higher rates of diabetes, elevated cholesterol, and anxiety/depression compared to the general U.S. population. The study sample had averages for hypertension that were lower than the national population. This finding conflicts with previous research reporting higher hypertension in male and female COs compared to national norms.3 In our own evaluation of the CO population (Cherniack et al., 2016), where blood pressure was directly measured, age-adjusted hypertension was considerably higher than national norms.93 In addition, a recent report on cardiovascular health reported that 17% of U.S. adults have undiagnosed hypertension;94 it is possible that hypertension was underreported in this study. Consistent with previous work,95 BMI was significantly associated with diabetes and hypertension, but was not associated with elevated cholesterol in this sample. Understanding contributing workplace factors that increase obesity and chronic disease risk in correctional employees remains an important area of research.
Work Characteristics and Health Behaviors
Regarding psychosocial work factors, health behaviors and health outcomes in correctional supervisor staff, Faghri et al. (2015) examined COs and found that positive emotions were associated with better nutrition, physical activity, and sleep quality. Those findings in line-officers from this same workforce duplicate the associations seen here in their supervisors. The psychological and physiological health impact from poor coping mechanisms, changes in health behaviors, morbidity and mortality among correctional employees reiterates a need for understanding the relationships among work characteristics and health behaviors.
Burnout was significantly associated with all four health diagnoses. There was an inverse relationship, indicating that higher burnout was associated with poorer nutrition, physical activity, less sleep and poor sleep quality. Similarly, Hu et al. (2015) reported associations between emotional exhaustion and cynicism (domains within burnout) with sleep disorders, exercise, chronic disease, work hours, and shift.41 Mignano et al. (2016) used a theory-driven approach and created the psychological health, behavior, and body weight (PBBW) model based on the CO population described in this study. The authors found that poor psychological health, such as higher depression levels, were associated with less healthy diet and exercise behaviors, and increased body weight. Stress may play a moderating role in the relationship between mood, health behaviors, and obesity.96 This finding was absent when depression was used as a predictor variable, which may be attributed to underreporting of stress levels in this occupational group.10,97 There may be an indirect relationship between psychological health and chronic disease risk factors, such as obesity, which may be explained by health behaviors.96 In summary, reducing feelings of burnout in correctional employees may have a spillover effect on health behaviors.
Job satisfaction and coworker support were associated with sleep duration, suggesting that individuals who feel positively about their job and social network at the workplace may be more likely to meet sleep guidelines. The relationship between supervisor support and sleep duration approached significance. All five psychosocial work characteristics (burnout, job meaning, job satisfaction, coworker support, and supervisor support) were associated with sleep quality. Burnout was inversely related, whereas the other variables were positively related. This finding suggests that emotional experiences at work may significantly influence sleep hygiene. Previous research has linked sleep to physical98,99 and mental health,100 and therefore improving psychosocial work factors and health climate in the workplace may have a spillover effect on health.
We did not find relationships between job meaning, job satisfaction, or social support with nutrition or physical activity. This conflicts prior research demonstrating relationships among coworker18,101-103 and supervisor support,104 to higher fruit and vegetable intake and inversely associated with obesity. In general, more supportive social work environments are associated with healthier behaviors.57,60,105,106
Work Characteristics and Health Outcomes
Burnout was associated with diabetes and anxiety/depression. Participants were nearly twice as likely to report anxiety/depression if reporting symptoms of burnout. This finding is consistent with previous research suggesting relationships between burnout, mental health outcomes,107 and type 2 diabetes.108 Job satisfaction was significantly associated with diabetes and supervisor support was significantly associated with anxiety/depression. These items were inversely related, suggesting that higher levels of job satisfaction or supervisor support would be associated with lower odds of developing the respective health outcome. Therefore, psychosocial work factors may increase the odds of developing some comorbid conditions, or alternatively, may protect against chronic disease risk factors. No psychosocial work factors were associated with hypertension or elevated cholesterol in this study. It is likely there are complex interrelationships among demographic, environmental, biological, and psychosocial factors.
Limitations
Despite the significant findings of this study, there are several limitations that need to be acknowledged. This study was limited by the measures used to capture health behaviors and outcomes. However, this study utilized a participatory action research approach, involving supervisors in survey development, possibly improving the acceptability of the questions used. In addition, this study relies on self-reported data and convenience sampling, and thus, the ability to generalize to other correctional supervisors or public safety occupations may be limited. However, survey respondents represented 20 correctional facilities, thus increasing the likelihood that the supervisors were a representative sample to strengthen these preliminary findings. Despite these limitations, this study adds to existing literature examining work characteristics and health behaviors in a worker group at elevated chronic disease risk. A large proportion of the sample was classified as overweight or obese, and therefore it may be difficult to determine predictors of obesity. Despite these limitations, this study provides much-needed insight into the health status of correctional supervisors.
CONCLUSIONS
This study adds to the existing literature on correctional supervisors. To our knowledge, this is the first study that examines correctional supervisor health status in the United States. Correctional supervisors are an understudied population within the DOC organization, and this group of middle-management has the opportunity to encourage health-promoting practices in the workplace by connecting policies from administrators to fellow coworkers and line-level officers. Workplace health promotion programs primarily direct interventions towards individual-level behavior change. Use of psychosocial work constructs will allow investigators to direct their attention to organizational factors that may derail health behaviors and outcomes in the workplace, posing additional costs from increased use of sick days, workers compensation claims, and lost productivity.
This study examined work factors that may predict health behaviors and outcomes in a group of high-stress employees. Higher levels of burnout and lower levels of meaningful work, job satisfaction and workplace social support were associated with poor health behaviors and outcomes. This may be due to negative emotions associated with work responsibilities and the environment. Burnout was significantly associated with nutrition, physical activity, sleep duration, sleep quality, diabetes, and anxiety/depression. Job meaning, job satisfaction, and workplace social support may also be associated with sleep. Sleep may impact numerous physiological processes and chronic disease risk,29 and thus, improving the psychosocial work environment may support a public health impact. Future research should utilize psychosocial work measures and objective health outcome measures to clarify these relationships. The health status and behaviors of correctional supervisors versus officers should be a research comparison, as this may provide direction for policy change and interventions.
Acknowledgements
This work was supported by the Center for the Promotion of Health in the New-England Workplace (CPH-NEW).
The authors would also like to acknowledge the Correctional Supervisors Council for their initiation and support of the project, as well as their involvement on the Design Team. In addition, the Connecticut Department of Corrections supervisors who participated in the study.
Funding Source:
Grant sponsor: This publication was supported by The National Institute for Occupational Safety and Health (NIOSH). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of NIOSH. Grant Number: R01OH008929.
Footnotes
Conflict of Interest:
The authors have no relationships that would present conflict of interest.
REFERENCES
- 1.Cheek F. Stress management for correctional officers and their families. 1984 [Google Scholar]
- 2.Parker JR. Florida mortality study: Florida law enforcement and corrections officers compared to Florida general population. 2011 [Google Scholar]
- 3.Morse T, Dussetschleger J, Warren N, Cherniack M. Talking about health: Correction employees' assessments of obstacles to healthy living. J Occup Environ Med. 2011;53(9):1037–1045. doi: 10.1097/JOM.0b013e3182260e2c. [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention [October, 2015];Life expectancy. FastStats Web site. http://www.cdc.gov/nchs/fastats/life-expectancy.htm. Updated 2015.
- 5.Finney C, Stergiopoulos E, Hensel J, Bonato S, Dewa CS. Organizational stressors associated with job stress and burnout in correctional officers: A systematic review. BMC Public Health. 2013;13:82–2458-13-82. doi: 10.1186/1471-2458-13-82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brower J. OJP Diagnostic Center. Correctional officer wellness and safety literature review. Correctional Officer Health and Safety Literature Review. 2013 [Google Scholar]
- 7.Johnson S, Cooper C, Cartwright S, Donald I. The experience of work-related stress across occupations. J Manage Psychol. 2005;20(1):178–187. [Google Scholar]
- 8.Spinaris CG, Denhof MD, Kellaway JA. Posttraumatic stress disorder in United States corrections professionals: Prevalence and impact on health and functioning. Desert Waters Correctional Outreach. 2012 [Google Scholar]
- 9.Lester N, Wright M, Northrup K. Examining the health risks for corrections professionals. 2001;63(6):106–108. [Google Scholar]
- 10.Faghri PD, Mignano C, Cherniack M, Huedo-Medina TB. Psychological health and overweight and obesity among high stressed work environments. 2015;1(1) doi: 10.16966/2380-5528.101. doi: http://dx.doi.org/10.16966/ooa.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ferraro L, Faghri PD, Henning R, Cherniack M, Center for the Promotion of Health in the New England Workplace Team Workplace-based participatory approach to weight loss for correctional employees. J Occup Environ Med. 2013;55(2):147–155. doi: 10.1097/JOM.0b013e3182717cd4. [DOI] [PubMed] [Google Scholar]
- 12.Owen SS. Occupational stress among correctional supervisors. Prison J. 2006;86(2):164. [Google Scholar]
- 13.Lambert E, Hogan N, Allen R. Correlates of correctional officer job stress: The impact of organizational structure. Am J Crim Just. 2006;30(2):227–246. [Google Scholar]
- 14.Finn P. Addressing correctional officer stress: Programs and strategies. NCJ 183474. National Institute of Justice; 2000. p. 13. [Google Scholar]
- 15.Theorell T, Hammarstrom A, Aronsson G, et al. A systematic review including meta-analysis of work environment and depressive symptoms. BMC Public Health. 2015;15:738–015-1954-4. doi: 10.1186/s12889-015-1954-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bronkhorst B, Tummers L, Steijn B, Vijverberg D. Organizational climate and employee mental health outcomes: A systematic review of studies in health care organizations. Health Care Manage Rev. 2015;40(3):254–271. doi: 10.1097/HMR.0000000000000026. [DOI] [PubMed] [Google Scholar]
- 17.Bernal D, Campos-Serna J, Tobias A, Vargas-Prada S, Benavides FG, Serra C. Work-related psychosocial risk factors and musculoskeletal disorders in hospital nurses and nursing aides: A systematic review and meta-analysis. Int J Nurs Stud. 2015;52(2):635–648. doi: 10.1016/j.ijnurstu.2014.11.003. [DOI] [PubMed] [Google Scholar]
- 18.Miranda H, Gore RJ, Boyer J, Nobrega S, Punnett L. Health behaviors and overweight in nursing home employees: Contribution of workplace stressors and implications for worksite health promotion. ScientificWorldJournal. 2015;2015:915359. doi: 10.1155/2015/915359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.French SA, Story M, Jeffery RW. Environmental influences on eating and physical activity. Annu Rev Public Health. 2001;22:309–335. doi: 10.1146/annurev.publhealth.22.1.309. [DOI] [PubMed] [Google Scholar]
- 20.Sallis JF, Glanz K. Physical activity and food environments: Solutions to the obesity epidemic. Milbank Q. 2009;87(1):123–154. doi: 10.1111/j.1468-0009.2009.00550.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Larson N, Story M. A review of environmental influences on food choices. Ann Behav Med. 2009;38(Suppl 1):S56–73. doi: 10.1007/s12160-009-9120-9. [DOI] [PubMed] [Google Scholar]
- 22.Booth SL, Sallis JF, Ritenbaugh C, et al. Environmental and societal factors affect food choice and physical activity: Rationale, influences, and leverage points. Nutr Rev. 2001;59(3 Pt 2):S21–39. doi: 10.1111/j.1753-4887.2001.tb06983.x. discussion S57-65. [DOI] [PubMed] [Google Scholar]
- 23.Sorensen G, Linnan L, Hunt MK. Worksite-based research and initiatives to increase fruit and vegetable consumption. Prev Med. 2004;39(Suppl 2):S94–100. doi: 10.1016/j.ypmed.2003.12.020. [DOI] [PubMed] [Google Scholar]
- 24.Fung TT, Rimm EB, Spiegelman D, et al. Association between dietary patterns and plasma biomarkers of obesity and cardiovascular disease risk. Am J Clin Nutr. 2001;73(1):61–67. doi: 10.1093/ajcn/73.1.61. [DOI] [PubMed] [Google Scholar]
- 25.Kant AK. Dietary patterns and health outcomes. J Am Diet Assoc. 2004;104(4):615–635. doi: 10.1016/j.jada.2004.01.010. [DOI] [PubMed] [Google Scholar]
- 26.Kerver JM, Yang EJ, Bianchi L, Song WO. Dietary patterns associated with risk factors for cardiovascular disease in healthy US adults. Am J Clin Nutr. 2003;78(6):1103–1110. doi: 10.1093/ajcn/78.6.1103. [DOI] [PubMed] [Google Scholar]
- 27.Warburton DE, Nicol CW, Bredin SS. Health benefits of physical activity: The evidence. CMAJ. 2006;174(6):801–809. doi: 10.1503/cmaj.051351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sofi F, Capalbo A, Cesari F, Abbate R, Gensini GF. Physical activity during leisure time and primary prevention of coronary heart disease: An updated meta-analysis of cohort studies. Eur J Cardiovasc Prev Rehabil. 2008;15(3):247–257. doi: 10.1097/HJR.0b013e3282f232ac. [DOI] [PubMed] [Google Scholar]
- 29.Perry GS, Patil SP, Presley-Cantrell LR. Raising awareness of sleep as a healthy behavior. Prev Chronic Dis. 2013;10:E133. doi: 10.5888/pcd10.130081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cappuccio FP, Taggart FM, Kandala NB, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31(5):619–626. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cappuccio FP, Cooper D, D'Elia L, Strazzullo P, Miller MA. Sleep duration predicts cardiovascular outcomes: A systematic review and meta-analysis of prospective studies. Eur Heart J. 2011;32(12):1484–1492. doi: 10.1093/eurheartj/ehr007. [DOI] [PubMed] [Google Scholar]
- 32.Nieuwenhuijsen K, Bruinvels D, Frings-Dresen M. Psychosocial work environment and stress-related disorders, a systematic review. Occup Med (Lond) 2010;60(4):277–286. doi: 10.1093/occmed/kqq081. [DOI] [PubMed] [Google Scholar]
- 33.Jackson SE, Schwab RL, Schuler RS. Toward an understanding of the burnout phenomenon. J Appl Psychol. 1986;71(4):630–640. [PubMed] [Google Scholar]
- 34.Nevanpera NJ, Hopsu L, Kuosma E, Ukkola O, Uitti J, Laitinen JH. Occupational burnout, eating behavior, and weight among working women. Am J Clin Nutr. 2012;95(4):934–943. doi: 10.3945/ajcn.111.014191. [DOI] [PubMed] [Google Scholar]
- 35.Cecil J, McHale C, Hart J, Laidlaw A. Behaviour and burnout in medical students. Med Educ Online. 2014;19:25209. doi: 10.3402/meo.v19.25209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ahola K, Pulkki-Raback L, Kouvonen A, Rossi H, Aromaa A, Lonnqvist J. Burnout and behavior-related health risk factors: Results from the population-based finnish health 2000 study. J Occup Environ Med. 2012;54(1):17–22. doi: 10.1097/JOM.0b013e31823ea9d9. [DOI] [PubMed] [Google Scholar]
- 37.Chin W, Guo YL, Hung YJ, Yang CY, Shiao JS. Short sleep duration is dose-dependently related to job strain and burnout in nurses: A cross sectional survey. Int J Nurs Stud. 2015;52(1):297–306. doi: 10.1016/j.ijnurstu.2014.09.003. [DOI] [PubMed] [Google Scholar]
- 38.Yoo H, Franke WD. Sleep habits, mental health, and the metabolic syndrome in law enforcement officers. J Occup Environ Med. 2013;55(1):99–103. doi: 10.1097/JOM.0b013e31826e294c. [DOI] [PubMed] [Google Scholar]
- 39.Kakiashvili T, Leszek J, Rutkowski K. The medical perspective on burnout. Int J Occup Med Environ Health. 2013;26(3):401–412. doi: 10.2478/s13382-013-0093-3. [DOI] [PubMed] [Google Scholar]
- 40.Schaufeli WB, Peeters MC. Job stress and burnout among correctional officers: A literature review. International Journal of Stress Management. 2000;7(1):19–48. [Google Scholar]
- 41.Hu S, Wang JN, Liu L, et al. The association between work-related characteristic and job burnout among Chinese correctional officers: A cross-sectional survey. Public Health. 2015;129(9):1172–1178. doi: 10.1016/j.puhe.2015.05.006. [DOI] [PubMed] [Google Scholar]
- 42.Stoyanova RG, Harizanova SN. Assessment of the personal losses suffered by correctional officers due to burnout syndrome. Int J Occup Environ Med. 2016;7(1):33–41. doi: 10.15171/ijoem.2016.680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lambert EG, Barton-Bellessa S, Hogan NL. The consequences of emotional burnout among correctional staff. 2015;5(2) [Google Scholar]
- 44.Steger MF, Dik BJ, Duffy RD. Measuring meaningful work. Journal of Career Assessment. 2012;20(3):322–337. [Google Scholar]
- 45.Judge TA, Kammeyer-Mueller J. Job attitudes. Annu Rev Psychol. 2012;63:341–367. doi: 10.1146/annurev-psych-120710-100511. [DOI] [PubMed] [Google Scholar]
- 46.Sancassiani F, Campagna M, Tuligi F, Machado S, Cantone E, Carta MG. Organizational wellbeing among workers in mental health services: A pilot study. Clin Pract Epidemiol Ment Health. 2015;11:4–11. doi: 10.2174/1745017901511010004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Arnold KA, Turner N, Barling J, Kelloway EK, McKee MC. Transformational leadership and psychological well-being: The mediating role of meaningful work. J Occup Health Psychol. 2007;12(3):193–203. doi: 10.1037/1076-8998.12.3.193. [DOI] [PubMed] [Google Scholar]
- 48.Aazami S, Shamsuddin K, Akmal S, Azami G. The relationship between job satisfaction and psychological/physical health among Malaysian working women. Malays J Med Sci. 2015;22(4):40–46. [PMC free article] [PubMed] [Google Scholar]
- 49.Ruggiero JS. Health, work variables, and job satisfaction among nurses. J Nurs Adm. 2005;35(5):254–263. doi: 10.1097/00005110-200505000-00009. [DOI] [PubMed] [Google Scholar]
- 50.Faragher EB, Cass M, Cooper CL. The relationship between job satisfaction and health: A meta-analysis. Occup Environ Med. 2005;62(2):105–112. doi: 10.1136/oem.2002.006734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Clemente M, Reig-Botella A, Coloma R. The occupational health of correctional officers in Peru. The Prison Journal. 2015;95(2):244–263. [Google Scholar]
- 52.Yang T, Shen YM, Zhu M, et al. Effects of co-worker and supervisor support on job stress and presenteeism in an aging workforce: A structural equation modelling approach. Int J Environ Res Public Health. 2015;13(1) doi: 10.3390/ijerph13010072. 10.3390/ijerph13010072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Turner N, Chmiel N, Hershcovis MS, Walls M. Life on the line: Job demands, perceived coworker support for safety, and hazardous work events. J Occup Health Psychol. 2010;15(4):482–493. doi: 10.1037/a0021004. [DOI] [PubMed] [Google Scholar]
- 54.Nagami M, Tsutsumi A, Tsuchiya M, Morimoto K. Job control and coworker support improve employee job performance. Ind Health. 2010;48(6):845–851. doi: 10.2486/indhealth.ms1162. [DOI] [PubMed] [Google Scholar]
- 55.Sorensen G, Stoddard A, Macario E. Social support and readiness to make dietary changes. Health Educ Behav. 1998;25(5):586–598. doi: 10.1177/109019819802500506. [DOI] [PubMed] [Google Scholar]
- 56.Lemon SC, Zapka J, Li W, Estabrook B, Magner R, Rosal MC. Perceptions of worksite support and employee obesity, activity and diet. Am J Health Behav. 2009;33(3):299–308. doi: 10.5993/ajhb.33.3.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Apostolopoulos Y, Shattell MM, Sonmez S, Strack R, Haldeman L, Jones V. Active living in the trucking sector: Environmental barriers and health promotion strategies. J Phys Act Health. 2012;9(2):259–269. doi: 10.1123/jpah.9.2.259. [DOI] [PubMed] [Google Scholar]
- 58.Kegler MC, Swan DW, Alcantara I, Wrensford L, Glanz K. Environmental influences on physical activity in rural adults: The relative contributions of home, church and work settings. J Phys Act Health. 2012;9(7):996–1003. doi: 10.1123/jpah.9.7.996. [DOI] [PubMed] [Google Scholar]
- 59.French SA, Harnack LJ, Hannan PJ, Mitchell NR, Gerlach AF, Toomey TL. Worksite environment intervention to prevent obesity among metropolitan transit workers. Prev Med. 2010;50(4):180–185. doi: 10.1016/j.ypmed.2010.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Bopp M, Child S, Campbell M. Factors associated with active commuting to work among women. Women Health. 2014;54(3):212–231. doi: 10.1080/03630242.2014.883663. [DOI] [PubMed] [Google Scholar]
- 61.Buxton OM, Quintiliani LM, Yang MH, et al. Association of sleep adequacy with more healthful food choices and positive workplace experiences among motor freight workers. Am J Public Health. 2009;99(Suppl 3):S636–43. doi: 10.2105/AJPH.2008.158501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.U.S. Department of Agriculture and U.S. Department of Health and Human Services [March 12, 2014];Dietary guidelines for americans. 2010 http://www.cnpp.usda.gov/DGAs2010-PolicyDocument.htm. Published December 2010.
- 63.U.S. Department of Health and Human Services 2008 physical activity guidelines for americans. 2010 [Google Scholar]
- 64.Center for the Promotion of Health in the New England Workplace (CPH-NEW) Correctional supervisors' council healthy workplace survey items. 2015 [Google Scholar]
- 65.Patel RP, Taylor SD. Factors affecting medication adherence in hypertensive patients. Ann Pharmacother. 2002;36(1):40–45. doi: 10.1345/aph.1A046. [DOI] [PubMed] [Google Scholar]
- 66.Division of Nutrition, Physical Activity and Obesity, National Center for Chronic Disease Prevention and Health Promotion . Healthy weight. Centers for Disease Control and Prevention (CDC); Web site. http://www.cdc.gov/healthyweight/assessing/bmi/adult_bmi/index.html#Interpreted. Updated 2015-2016. [Google Scholar]
- 67.Spreitzer GM. Psychological empowerment at the workplace: Dimensions, measurements, and validation. Academy of Management Journal. 1995;38:142–146. [Google Scholar]
- 68.Office of Performance Monitoring (OPM) Organizational assessment survey (OAS) http://www.opm.gov/employ/html/org_asse.asp.
- 69.Karasek RA, Pieper CF, Schwartz JE. Job content questionnaire and user's guide revision 11. developed at Columbia University. 1985 [Google Scholar]
- 70.Jamieson S. Likert scales: How to (ab)use them. Med Educ. 2004;38(12):1217–1218. doi: 10.1111/j.1365-2929.2004.02012.x. [DOI] [PubMed] [Google Scholar]
- 71.Carifio J, Perla RJ. Two common misunderstandings, misconceptions, persistent myths and urban legends about Likert scales and Likert response formats and their antidotes. Journal of Social Sciences. 2007;3(3):106–116. [Google Scholar]
- 72.Sullivan GM, Artino AR. Analyzing and interpreting data from Likert-type scales. Journal of Graduate Medical Education. 2013;5(4):541–542. doi: 10.4300/JGME-5-4-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Szumilas M. Explaining odds ratios. J Can Acad Child Adolesc Psychiatry. 2010;19(3):227–229. [PMC free article] [PubMed] [Google Scholar]
- 74.Moore L, Thompson F. Adults meeting fruit and vegetable intake recommendations - United States, 2013. 2015;26:709–713. [PMC free article] [PubMed] [Google Scholar]
- 75.U.S. Department of Health and Human Services, Centers for Disease Control and Prevention Early release of selected estimates based on data from the National Health Interview Survey. 2014 http://www.cdc.gov/nchs/data/nhis/earlyrelease/earlyrelease201506_07.pdf. Updated 2015-2016.
- 76.Hirshkowitz M, Whiton K, Albert SM, et al. National sleep foundation's updated sleep duration recommendations: Final report. Sleep Health: Journal of the National Sleep Foundation. 1(4):233–243. doi: 10.1016/j.sleh.2015.10.004. [DOI] [PubMed] [Google Scholar]
- 77.Liu Y, Wheaton AG, Chapman DP, Cunningham TJ, Lu H, Croft JB. Prevalence of healthy sleep duration among adults - United States, 2014. 2016;65(6):137–141. doi: 10.15585/mmwr.mm6506a1. [DOI] [PubMed] [Google Scholar]
- 78.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311(8):806–814. doi: 10.1001/jama.2014.732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Centers for Disease Control and Prevention . National diabetes statistics report: Estimates of diabetes and its burden in the United States, 2014. U S Department of Health and Human Services; 2014. [Google Scholar]
- 80.Nwankwo T, Yoon SS, Burt V, Gu Q. Hypertension among adults in the US: National Health and Nutrition Examination Survey, 2011-2012. National Center for Health Statistics, Centers for Disease Control and Prevention, US Dept of Health and Human Services. 2013 (NCHS Data Brief, No. 133) [Google Scholar]
- 81.National Center for Health Statistics . Health, United States, 2014: With special feature on adults aged 55-64. U S Department of Health and Human Services; 2015. [PubMed] [Google Scholar]
- 82.Anxiety and Depression Association of America (ADAA) [March 8, 2016];Facts & statistics. http://www.adaa.org/about-adaa/press-room/facts-statistics. Updated 2014.
- 83.Karlin WA, Brondolo E, Schwartz J. Workplace social support and ambulatory cardiovascular activity in New York City traffic agents. Psychosom Med. 2003;65(2):167–176. doi: 10.1097/01.psy.0000033122.09203.a3. [DOI] [PubMed] [Google Scholar]
- 84.Tsutsumi A. Development of an evidence-based guideline for supervisor training in promoting mental health: Literature review. J Occup Health. 2011;53(1):1–9. doi: 10.1539/joh.r10002. [DOI] [PubMed] [Google Scholar]
- 85.Anagnostopoulos F, Demerouti E, Sykioti P, Niakas D, Zis P. Factors associated with mental health status of medical residents: A model-guided study. J Clin Psychol Med Settings. 2015;22(1):90–109. doi: 10.1007/s10880-014-9415-2. [DOI] [PubMed] [Google Scholar]
- 86.Brough P, Williams J. Managing occupational stress in a high- risk industry: Measuring the job demands of correctional officers. Crim Justice Behav. 2007;34(4):555. [Google Scholar]
- 87.Lambert E, Jiang S, Hogan N. The issue of trust in shaping the job stress, job satisfaction, and organizational commitment of correctional staff. Professional Issues in Criminal Justice. 2008;3(4):37–64. [Google Scholar]
- 88.Lambert EG, Hogan NL, Barton-Bellessa S, Jiang S. Examining the relationship between supervisor and management trust and job burnout among correctional staff. Crim Justice Behav. 2012;39(7):938–957. [Google Scholar]
- 89.Yang S, Brown GC, Moon B. Factors leading to corrections officers' job satisfaction. Public Personnel Management. 2011;40(4):359–369. [Google Scholar]
- 90.Lambert E, Hogan N, Jiang S, Jenkins M. I am fried: The issues of stressors and burnout among correctional staff. Corrections Compendium. 2009;34(2):16–23. [Google Scholar]
- 91.Pearson N, Biddle SJ. Sedentary behavior and dietary intake in children, adolescents, and adults. A systematic review. Am J Prev Med. 2011;41(2):178–188. doi: 10.1016/j.amepre.2011.05.002. [DOI] [PubMed] [Google Scholar]
- 92.Knowlden AP, Burns M, Harcrow A, Shewmake ME. Cross-sectional analysis of food choice frequency, sleep confounding beverages, and psychological distress predictors of sleep quality. Int J Adolesc Med Health. 2016 doi: 10.1515/ijamh-2015-0120. [DOI] [PubMed] [Google Scholar]
- 93.Cherniack M, Dussetschleger J, Dugan A, et al. Participatory action research in corrections: The HITEC 2 program. Appl Ergon. 2016;53(Pt A):169–180. doi: 10.1016/j.apergo.2015.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Mozaffarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics--2015 update: A report from the american heart association. Circulation. 2015;131(4):e29–322. doi: 10.1161/CIR.0000000000000152. [DOI] [PubMed] [Google Scholar]
- 95.Bays HE, Chapman RH, Grandy S. The relationship of body mass index to diabetes mellitus, hypertension and dyslipidaemia: Comparison of data from two national surveys. Int J Clin Pract. 2007;61(5):737–747. doi: 10.1111/j.1742-1241.2007.01336.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Mignano C, Faghri PD, Huedo-Medina T, Cherniack MC. Psychological health, behavior, and bodyweight ( PBBW) model: An evaluation of predictors of health behaviors and body mass index ( BMI). Journal of Workplace Behavioral Health. 2016;31(1):37–56. [Google Scholar]
- 97.Cheek FE, Miller M. The experience of stress for correction officers: A double-bind theory of correctional stress. Journal of Criminal Justice. 1983;11(2):105–120. [Google Scholar]
- 98.Wu Y, Zhai L, Zhang D. Sleep duration and obesity among adults: A meta-analysis of prospective studies. Sleep Med. 2014;15(12):1456–1462. doi: 10.1016/j.sleep.2014.07.018. [DOI] [PubMed] [Google Scholar]
- 99.Xi B, He D, Zhang M, Xue J, Zhou D. Short sleep duration predicts risk of metabolic syndrome: A systematic review and meta-analysis. Sleep Med Rev. 2014;18(4):293–297. doi: 10.1016/j.smrv.2013.06.001. [DOI] [PubMed] [Google Scholar]
- 100.Zhai L, Zhang H, Zhang D. Sleep duration and depression among adults: A meta-analysis of prospective studies. Depress Anxiety. 2015;32(9):664–670. doi: 10.1002/da.22386. [DOI] [PubMed] [Google Scholar]
- 101.Wang ML, Pbert L, Lemon SC. Influence of family, friend and coworker social support and social undermining on weight gain prevention among adults. Obesity (Silver Spring) 2014;22(9):1973–1980. doi: 10.1002/oby.20814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Winston GJ, Phillips EG, Wethington E, et al. Social network characteristics associated with weight loss among black and hispanic adults. Obesity (Silver Spring) 2015;23(8):1570–1576. doi: 10.1002/oby.21155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Greaves CJ, Sheppard KE, Abraham C, et al. Systematic review of reviews of intervention components associated with increased effectiveness in dietary and physical activity interventions. BMC Public Health. 2011;11:119–2458-11-119. doi: 10.1186/1471-2458-11-119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Garcia-Rojas IJ, Choi B, Krause N. Psychosocial job factors and biological cardiovascular risk factors in mexican workers. Am J Ind Med. 2015;58(3):331–351. doi: 10.1002/ajim.22410. [DOI] [PubMed] [Google Scholar]
- 105.Lucove JC, Huston SL, Evenson KR. Workers' perceptions about worksite policies and environments and their association with leisure-time physical activity. Am J Health Promot. 2007;21(3):196–200. doi: 10.4278/0890-1171-21.3.196. [DOI] [PubMed] [Google Scholar]
- 106.Umstattd MR, Baller SL, Blunt GH, Darst ML. Correlates of perceived worksite environmental support for physical activity. J Phys Act Health. 2011;8(Suppl 2):S222–7. [PubMed] [Google Scholar]
- 107.Leiter MP, Maslach C. Burnout and health. Handbook of health psychology. 2001:415. [Google Scholar]
- 108.Melamed S, Shirom A, Toker S, Shapira I. Burnout and risk of type 2 diabetes: A prospective study of apparently healthy employed persons. Psychosom Med. 2006;68(6):863–869. doi: 10.1097/01.psy.0000242860.24009.f0. [DOI] [PubMed] [Google Scholar]