Case Report
A 48 years lady presented with lump in left breast. On examination there was 2 × 2 cm lump in lower inner quadrant of left breast without involvement of skin, pectoralis major muscle or chest wall. There was no axillary lymphadenopathy. General examination revealed a 3 × 2 cm thyroid swelling. There was no cervical lymphadenopathy.
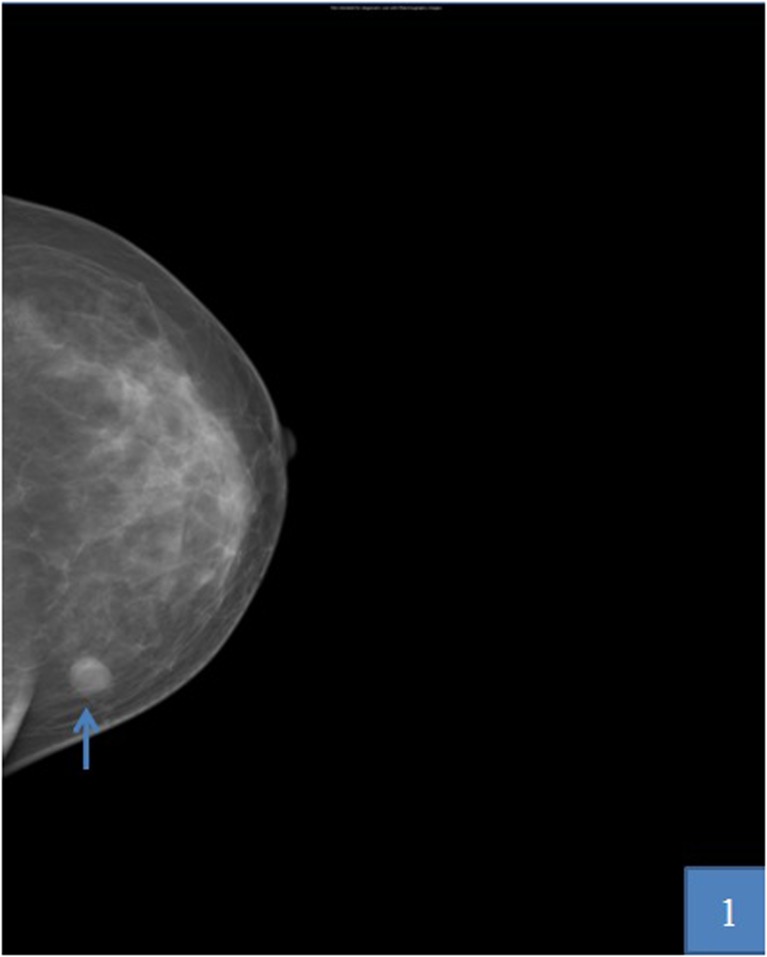
Mammography revealed a well defined, soft tissue density in the left inner & lower quadrant (Fig. 1), corresponding to 20 × 18 mm well defined hypoechoic lesion on sonography. Fine needle aspiration cytology (FNAC) from the breast lump was non diagnostic. FNAC from thyroid nodule was suggestive of papillary carcinoma thyroid. Excision biopsy of breast lump was done.
Fig. 1.
Mammographic images showing mass in lower inner quadrant (arrow head)
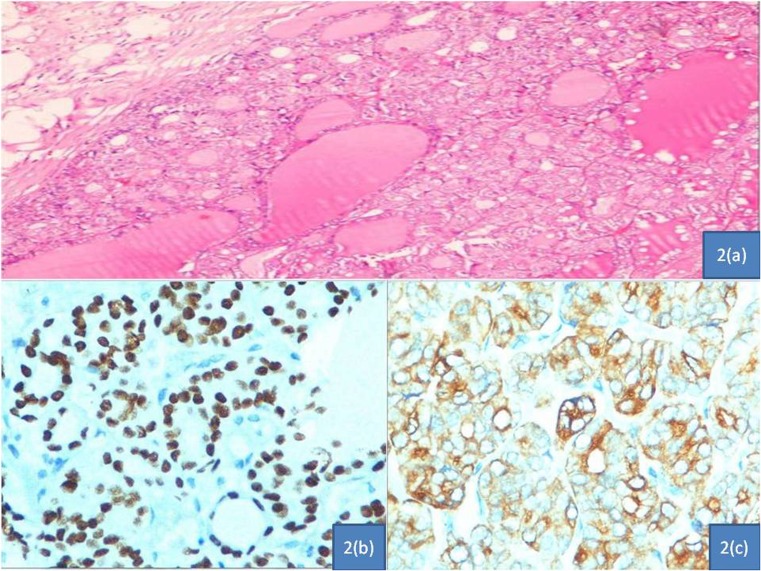
Histopathological examination of breast lump revealed well circumscribed nodule consisting of compactly arranged follicles separated by delicate vascularised septae. The follicles were small to medium sized and lined by cells with ground glass appearance. Nuclear grooves were seen. There was neither ductal carcinoma in situ (DCIS) nor elastosis of the adjacent breast parenchyma (Fig. 2a). Psammomatous calcifications were not seen. Immunohistochemical positivity for Thyroid transcription factor 1 (TTF-1) (Fig. 2b), Thyroglobulin (Fig. 2c) and Cytokeratin 19 was noted. The findings were consistent with metastatic papillary carcinoma of thyroid to breast.
Fig. 2.
a- Photomicrograph of breast lump demonstrating papillary thyroid cancer deposits. Fibrofatty tissue containing a well circumscribed nodule consisting of compactly arranged follicles with ground glass appearance and grooving of the nuclei suggestive of papillary thyroid cancer deposits. Hemotoxylon & Eosin staining 100×. b- Immunohistochemistry for TTF 1 shows strong nuclear positivity in photomicrograph of breast lump. c- Immunohistochemistry for Thyroglobulin shows strong positivity in photomicrograph of breast lump
Patient subsequently underwent total thyroidectomy. Intraoperatively a nodule of 3 × 2 cms was present in right lobe of thyroid. Left lobe, isthmus and rest of the neck were normal. Histopathology was suggestive of follicular variant of papillary carcinoma of thyoid (PTC).
Four week after surgery whole body radioactive iodine-131 (131I-WBS) scan revealed uptake in right ala of sacrum, transverse process of D1 vertebra and upper end of right femur suggestive of metastasis. A final diagnosis of Follicular variant of papillary carcinoma thyroid with skeletal & left breast metastases was made. Radioabalation was done with 100 mci of 131I. Further radioabalation was done with 300 mci, 200 mci, 200 mci of 131I at intervals of 1 year each. Latest whole body radioactive iodine-131 scan is showing good response to therapy. She is under follow up for last 3 years and is doing well.
Discussion
A total of 90 % of thyroid cancers are well-differentiated cancers. Papillary carcinomas are the most common type of well-differentiated cancers. They contribute 80 to 85 % of malignant epithelial thyroid tumors [1]. A thyroid nodule or a neck mass is usually the first manifestation and less frequently regional lymph nodes metastases. Distant metastases are rare and usually occur in advanced disease, usually in lungs, bones [2].
Reports of differentiated thyroid carcinoma with metastasis to breast are sparse. To our knowledge only 7 cases has been reported in literature [3–9]. Four cases of PTC, 2 cases of follicular thyroid cancer, 1 case of hurthle cell cancer were reported. Among PTC with breast metastasis, one was follicular variant, one tall cell variant and one was anaplastic carcinoma developing in PTC deposit in breast.
The first detailed documentation of metastatic follicular carcinoma of the thyroid to the breast was by Crisholm et al. in a 75-year-old woman with two previous neck operations for follicular carcinoma of the thyroid who presented with a breast mass 9 years after diagnosis [3]. The mass recurred one month after excisional biopsy . Pathological examination revealed metastatic follicular carcinoma. Tan et al. reported a case of immunohistologically proven breast metastasis from a thyroid papillary carcinoma [4]. Cristallani et al. described a case of breast metastasis from follicular cancer of thyroid [5]. Loureiro et al. reported a case of papillary carcinoma (follicular variant) of the thyroid with recurring cutaneous and breast metastases that appeared in the absence of other sites of tumor dissemination [6]. Fiche et al. described a case of breast metastasis from a tall cell variant of papillary thyroid carcinoma in a 59-year-old woman [7].
Al-abed et al. reported a case of metastatic hurthle cell carcinoma to breast [8]. A 77 year old lady had total thyroidectomy and bilateral neck dissection followed by radiotherapy for a high grade metastatic hurthle cell carcinoma of the thyroid. Ten months later she presented with left breast lump (upper inner) and a lump at the left axilla. Fine needle aspiration cytology of the lumps and histology after wide local excision of the breast lump confirmed metastatic Hurthle cell carcinoma [8]. Angeles-angeles et al. reported a case of metastatic anaplastic spindle and giant cell carcinoma originating in a papillary thyroid carcinoma deposit in breast in a 58 year lady who underwent hemithyroidectomy for PTC, then a completion thyroidectomy and neck dissection for cervical nodes recurrence 2 years later [9]. Seventeen years later she had axillary metastasis (from PTC) for which axillary dissection was done. Three month later underwent radical mastectomy for huge breast recurrence invading skin, skeletal muscle and replacing almost entire breast parenchyma. Histologic examination revealed a pleomorphic spindle and giant cell carcinoma with focal rhabdoid features and extensive necrosis. Focal (less than 10 %) papillary structures lined by cuboidal cells with nuclear features of PTC were identified. Thyroglobulin and TTF-1 staining were negative [9].
In our case it was follicular variant of papillary carcinoma thyroid with skeletal & breast metastases. The soft clues that helped in alerting towards a metastatic spread to the breast other than classic nuclear features of papillary carcinoma of thyroid were relative circumscription of the tumour, lack of elastosis and absence of DCIS albeit this can happen even in a primary invasive carcinoma of the breast. Immunohistochemistry for TTF-1, Thyroglobulin and cytokeratin 19 established the diagnosis. Lack of Estrogen Receptors (ER) and Gross Cystic Disease Fluid Protein GCDFP 15 expression further negated the possibility of this being a primary in the breast.
Metastases to the breast are associated with poor prognosis [2]. Because of its high sensitivity and specificity, post-therapeutic 131I-WBS and 131I Single photon emission computed tomography/computed tomography (131I-SPECT/CT) currently remain indispensable for the management of patients with DTC [2]. 131I-SPECT/CT is of incremental value over 131I-WBS at increasing diagnostic accuracy, reducing pitfalls and modifying therapeutic strategies [10].
Conclusions
Follicular variant of papillary carcinoma thyroid presenting with breast metastases is an unusual and rare occurence. Hence, it is presented here for its rarity and to enhance literature.
Compliance with Ethical Standards
Conflict of Interest
The authors declare that they have no conflict of interest.
References
- 1.Carling T, Udelsman R. Thyroid tumors. In: Devita VT, Lawrence TS, Rosenberg SA, editors. DeVita, Hellman and Rosenbergʾs Cancer: Principles & Practice of Oncology. 9e. Philadelphia: Lippincott Williams and Wilkins; 2011. pp. 1457–1472. [Google Scholar]
- 2.Song HJ, Xue YL, Xu YH Qiu ZL, Luo QY. Rare metastases of differentiated thyroid carcinoma: pictoral review. Endocr Related Cancer. 2011 Aug 30;18(5):R165-74. [DOI] [PubMed]
- 3.Chisholm RC, Chung EB, Tuckson W, Khan T, White JE. Follicular carcinoma of the thyroid with metastasis, to the breast. J Natl Med Assoc 1980 Nov;72(11):1101–4. [PMC free article] [PubMed]
- 4.Tan PK, Chua CL & Pob WT. Thyroid papillary carcinoma with unusual breast metastasis. Ann Acad Med Singapore 1991 Nov;20(6):801–2. [PubMed]
- 5.Cristallini EG, Ascani S, Nati S, Liberati F, Farabi R. Breast metastasis of thyroid follicular carcinoma. Acta Oncol. 1994;33(1):71–3. doi: 10.3109/02841869409098381. [DOI] [PubMed] [Google Scholar]
- 6.Loureiro MM, Leite VH, Boavida JM, Raposo JF, Henriques MM, Limbert ES, Sobrinho LG. An unusual case of papillary carcinoma of the thyroid with cutaneous and breast metastases only. Eur J Endocrinol 1997 Sep;137(3):267–9. [DOI] [PubMed]
- 7.Fiche M, Cassagnau E, Aillet G, Bailly J, Chupin M Classe JM, Bodic MF. Breast metastasis from a “tall cell variant” of papillary thyroid carcinoma. Ann Pathol 1998 Apr;18(2):130–2. [PubMed]
- 8.Al-Abed Y, Gray E, Wolfe K, Watters GW, Philpott JM. Metastatic hurthle cell carcinoma of the thyroid presenting as a breast lump : a case reporting. Int Semin Surg Oncol 2008 May 27;5:14. [DOI] [PMC free article] [PubMed]
- 9.Angeles-Angeles A, Chable-Montero F, Martinez-Benitez B, Albores Saavedra J. Unusual metastases of papillary thyroid carcinoma: report of 2 cases. Ann Diag Pathol 2009 Jun;13(3):189–96. [DOI] [PubMed]
- 10.Spanu A, Solinas ME, Chessa F, Sanna D, Nuvoli S, Madeddu G. 131 I-SPECT/CT in the follow-up of differentiated thyroid carcinoma: Incremental value versus planar imaging. J Nucl Med 2009 Feb;50(2):184–90. [DOI] [PubMed]