Abstract
Background
To examine Cesarean delivery rates based on the Robson’s Ten-group classification system (TGCS), over a 10-year period.
Methods
All Vaginal Deliveries and cesarean sections (CSs) performed over a 10-year period from 2004 to 2013 were included in the analysis. The data were compiled according to Robson’s TGCS of cesarean section for every year. Risk Ratios (crude RRs) with 95 % confidence intervals for delivery by cesarean section were calculated for each Robson’s group.
Results
The TGCS was easily applied in this large dataset of 40,086 deliveries. The 10-year overall cesarean section rate (CSR) was 25.17 %. Groups 1 and 3 represented 60 % of the total obstetric population. The largest contributions to the total CSR are group 1 (37.62 %) and group 5 (17.06 %). Group 3 which was the second largest group contributed 15 % to the overall CSR. Group 2 and group 4 had high group CSRs of 47.28 and 34.74 % respectively, although the total group size was small (n = 1375;3.43 %). Maternal age and presentation were found to have an independent association with mode of delivery on logistic regression.
Conclusion
The Ten-group classification helped to identify the main groups of subjects who contribute most to the overall CSR. It also helped to identify subgroups requiring closer monitoring for more in-depth analyses of the indications for caesarean section. It is important to focus on the first four TGCS groups which constitute about 75 % of all deliveries. It is in the low-risk groups that one is likely to find the highest and most inappropriate indications for cesarean sections.
Keywords: Caesarean section, Robson, Ten group classification
Introduction
Cesarean section rate (CSR) is one of the most frequently used indicators of healthcare quality at the national and international levels for clinical governance. The CSR has been increasing in the last 50 years [1]. In the last decade, there has been a dramatic increase in the CSR worldwide, which now exceeds 30 % in some regions [1].
Although several guidelines, including those issued by the World Health Organization [2] and the United States Healthy People 2000 initiative [3] suggest that the optimal CSR is 15 %, there seems to be little effect on the current CSR. In 2001, a new classification system for CS known as the “Ten-group” CS (TGCS) or Robson’s classification was proposed. This classification system categorizes women into ten mutually exclusive groups, considering the following a priori criteria: parity, the previous obstetric record of the woman, the course of labor, including pre-labor CS, and gestational age [4]. A recent systematic review critically appraised various classification systems and found that with the best overall scores in this group (Robson and Denk) are easy to understand, clear, mutually exclusive, totally inclusive, reproducible and allow prospective identification of categories [5].
The aim of this study was to examine Cesarean delivery rates at the department of Obstetrics and Gynecology, Medical Collage Baroda based on the Robson’s TGCS, over a 10-year period.
Materials and Methods
This study was carried, over a period of 10 years from January 1, 2004 to December 31, 2013. All Vaginal deliveries and cesarean sections performed over a 10-year period from 2004 to 2013 were included in the analysis. Data were compiled from the departmental records.
The data were compiled according to Robson’s TGCS of cesarean sections for every year and total births in that year were calculated from the departmental records. The percentage of total cesarean delivery was calculated against vaginal delivery.
The indications of cesarean section were classified according to Robson’s TGCS) as follows:
Nulliparous, single cephalic, >37 weeks in spontaneous labor.
Nulliparous, single cephalic, >37 weeks induced or CS before labor.
Multiparous (excluding previous cs), single cephalic, >37 weeks in spontaneous labor.
Multiparous (excluding previous cs), single cephalic, >37 weeks induced or CS before labor.
Previous CS, single cephalic, >37 weeks.
All nulliparous breeches.
All multiparous breeches (including previous CS).
All multiple pregnancies (including previous CS).
All abnormal lies (including previous CS).
All single, cephalic, <36 weeks (including previous CS).
All relevant obstetric information (parity, mode of previous deliveries, previous cesarean section and indications, and spontaneous or induced labor) and the gestational age were entered on a questionnaire and then transferred into Microsoft excel sheet, and analysis was carried out on the entire dataset.
For data analysis, the distribution of cases among all 10 groups of Robson’s classification for total births, for cesarean section deliveries and the contribution of each group to the overall CS rates with differences were assessed using Chi-square test for trends. CS rates were calculated as the ratio of cesarean deliveries to total deliveries. Risk Ratios (crude RRs) with 95 % confidence intervals for delivery by cesarean section were calculated for each Robson’s group. Statistical significance was set at 0.05. For variables like maternal age, gestational age, parity, birth weight, singleton or multiple pregnancies were studied for mode of delivery and association with LSCS by using Chi-square test. Multiple linear regression was used to establish the independent association of significant variables with the outcome using Epi info-7 (C.D.C) and the MedCalc software.
Results
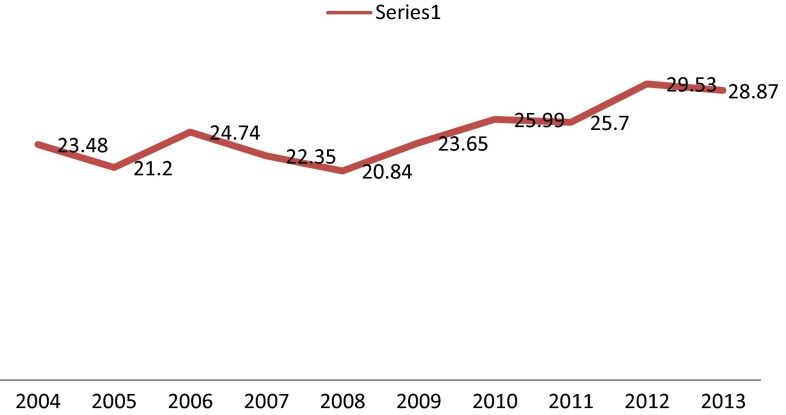
There were 29,993 vaginal deliveries and 10,093 cesarean deliveries during this study period. The 10-year overall CSR was 25.17 %. The CSR was 23.48 % in 2004 and has steadily risen to 29 % in 2012–2013 (Fig. 1). The number of total deliveries has also risen from 2717 in 2004 to 6071 in 2013.
Fig. 1.
Yearwise CSR (%)
Robson’s group 1 (1 = Nulliparous, single cephalic, >37 weeks in spontaneous labor) had the maximum number of subjects (n = 14,925), of which 25 % (n = 3797) had cesarean section. The second largest group of subjects were in group 3 (Multiparous (excluding previous cs), single cephalic, >37 weeks in spontaneous labor) of which, 11.6 % (n = 1524) underwent cesarean section. The group CSR % for induced labors in nulliparae and multiparae were high at 47.28 % (CRR 1.916, 95 % CI 1.78–2.057) and 34.74 % (CRR 1.38, 95 % CI 1.22–1.5), respectively.
The rates of Cesarean section was 100 % for group 9 (≥37 weeks, abnormal lie), 68 % for group 6 (>37 weeks, primi breech), and 64.8 %.for group 5 (Previous CS, single cephalic, >37 weeks).
The largest contributions to the total CS rate are group 1 (37.62 %) and group 5 (All multiparous with at least one previous uterine scar, with single cephalic pregnancy, ≥37 weeks gestation) (17.06 %). Group 3 which was the second largest group contributed 15 % to the overall CSR (Tables 1, 2).
Table 1.
Robson’s group specific, group CSR (%)
| Robson’s group | Total delivery no (%) | Vaginal delivery with no (%) | Cesarean with no (%) | Group CSR (%) | CD risk ratio with 95 % CI | P value |
|---|---|---|---|---|---|---|
| 1 | 14,925 (37.23) | 11,128 (74.55) | 3797 (25.44) | 25.44 | 1.06 (0.981–0.052) | 0.175 |
| 2 | 903 (2.25) | 476 (52.71) | 427 (47.28) | 47.28 | 1.916 (1.785–2.057) | <0.001 |
| 3 | 13,107 (32.7) | 11,583 (88.37) | 1524 (11.62) | 11.62 | 0.366 (0.348–0.385) | <0.001 |
| 4 | 472 (1.17) | 308 (65.25) | 164 (34.74) | 34.74 | 1.386 (1.223–1.570) | <0.001 |
| 5 | 2656 (6.62) | 934 (35.16) | 1722 (64.83) | 64.83 | 2.899 (2.802–2.998) | <0.001 |
| 6 | 866 (2.16) | 277 (31.98) | 589 (68.01) | 68.01 | 2.806 (2.672–2.947) | <0.001 |
| 7 | 701 (1.74) | 353 (50.35) | 348 (49.64) | 49.64 | 2.006 (1.858–2.615) | <0.001 |
| 8 | 323 (0.8) | 204 (63.15) | 119 (36.84) | 36.84 | 1.468 (1.272–1.695) | <0.001 |
| 9 | 101 (0.25) | 00 (00) | 101 (100) | 100 | 4.001 (3.934–4.070) | <0.001 |
| 10 | 6032 (15.04) | 4730 (78.41) | 1302 (21.58) | 21.58 | 0.836 (0.794–0.880) | <0.001 |
| TOTAL | 40,086 | 29,993 | 10,093 |
Table 2.
Relative contribution of each group to total CSR
| Robson’s group | Total delivery | Vaginal delivery no (%) | Cesarean no (%) | Contribution to total CSR (%) |
|---|---|---|---|---|
| 1 | 14,925 | 11,128 (74.55) | 3797 (25.44) | 37.62 |
| 2 | 903 | 476 (52.71) | 427 (47.28) | 4.23 |
| 3 | 13,107 | 11,583 (88.37) | 1524 (11.62) | 15.0 |
| 4 | 472 | 308 (65.25) | 164 (34.74) | 1.62 |
| 5 | 2656 | 934 (35.16) | 1722 (64.83) | 17.06 |
| 6 | 866 | 277 (31.98) | 589 (68.01) | 5.83 |
| 7 | 701 | 353 (50.35) | 348 (49.64) | 3.44 |
| 8 | 323 | 204 (63.15) | 119 (36.84) | 1.17 |
| 9 | 101 | 00 (00) | 101 (100) | 1.00 |
| 10 | 6032 | 4730 (78.41) | 1302 (21.58) | 12.90 |
Table 3 show that the increases in CS rates are seen primarily within groups with a high likelihood of having spontaneous vaginal deliveries (Robson’s classes 1 and 3) and in groups where planned intervention had been instituted (Robson’s classes 2 and 4). Significant rising trends are also seen in group 5 and group 7. This rising trends in these groups are highly significant.
Table 3.
Relative changes in the cesarean section rates in Robson’s ten groups from 2004 to 2013
| Year | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | Total | Chi square test for trends | P value |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total delivery | 2717 | 2894 | 3410 | 3068 | 4461 | 3585 | 4931 | 3778 | 5171 | 6071 | 40,086 | ||
| Vaginal delivery | 2079 | 2283 | 2543 | 2391 | 3531 | 2737 | 3660 | 2807 | 3644 | 4318 | 29,993 | ||
| Robson’s class | |||||||||||||
| 1 | 187 | 205 | 350 | 280 | 232 | 328 | 682 | 301 | 625 | 607 | 3797 | 60.951 | <0.0001 |
| 2 | 20 | 20 | 40 | 49 | 29 | 44 | 35 | 47 | 54 | 89 | 427 | 10.117 | 0.0015 |
| 3 | 145 | 101 | 120 | 95 | 107 | 150 | 141 | 162 | 270 | 233 | 1524 | 25.98 | <0.0001 |
| 4 | 10 | 14 | 21 | 19 | 9 | 20 | 10 | 16 | 10 | 30 | 164 | 9.6 | 0.0018 |
| 5 | 100 | 102 | 129 | 107 | 107 | 137 | 160 | 213 | 304 | 365 | 1722 | 124.312 | <0.0001 |
| 6 | 50 | 53 | 59 | 38 | 48 | 72 | 48 | 54 | 68 | 99 | 589 | 3.06 | 0.0802 |
| 7 | 34 | 47 | 50 | 29 | 31 | 30 | 20 | 33 | 30 | 44 | 348 | 24.433 | <0.0001 |
| 8 | 4 | 3 | 12 | 10 | 9 | 10 | 17 | 8 | 15 | 31 | 119 | 1.453 | 0.228 |
| 9 | 5 | 3 | 14 | 16 | 7 | 5 | 4 | 5 | 5 | 37 | 101 | na | na |
| 10 | 83 | 63 | 72 | 34 | 353 | 52 | 145 | 132 | 150 | 218 | 1302 | 0.0552 | 0.8143 |
| Total | 638 | 611 | 867 | 677 | 930 | 848 | 1262 | 971 | 1527 | 1753 | 10,093 | ||
Table 4 shows the maternal characteristics and mode of delivery. The maternal variables studied were birth weight, presentation (cephalic and abnormal), single or multiple gestation, gestational age in weeks, maternal age in years, and parity. All characteristics except the number of fetuses were found to have a significant association with mode of delivery on bivariate analysis. However, when logistic regression was applied, birth weight, gestational age, and parity were not found to be independent risk factors for mode of delivery, whereas, maternal age and presentation were found to have an independent association.
Table 4.
Maternal characteristics and modes of delivery
| Maternal characteristic | Total delivery | Vaginal delivery (%) | Cesarean (%) | Chi square test value | P value | Multiple linear regression coefficient | P value |
|---|---|---|---|---|---|---|---|
| Birth weight | |||||||
| <1000 GMS | 922 | 881 (95.55) | 41 (4.44) | 30.54 | <0.0001 | −0.09257 | <0.0001 |
| 1000–1499 | 2059 | 1770 (85.96) | 289 (14.03) | ||||
| 1500–2499 | 16,935 | 11,937 (70.48) | 4998 (29.51) | ||||
| 2500–3999 | 20,439 | 15,584 (76.24) | 4855 (23.75) | ||||
| >4000 | 54 | 25 (46.29) | 29 (53.70) | ||||
| Presentation | |||||||
| Cephalic | 37,365 | 28,762 (76.97) | 8603 (23.02) | 1354.2 | <0.0001 | 0.7302 | <0.0001 |
| Abnormal | 2721 | 1231 (45.24) | 1490 (54.75) | ||||
| N of fetuses | |||||||
| Single | 39,317 | 29,436 (74.86) | 9881 (25.13) | 2.25 | 0.13 | 0.08828 | 0.061 |
| Multiple | 769 | 557 (72.43) | 212 (27.17) | ||||
| Gestational age | |||||||
| >37 weeks | 33,787 | 24,954 (73.85) | 8833 (26.14) | 141.16 | <0.0001 | −0.4523 | <0.001 |
| 30–36 weeks | 4975 | 3890 (78.19) | 1085 (21.80) | ||||
| <30 weeks | 1324 | 1149 (86.78) | 175 (13.21) | ||||
| Maternal age | |||||||
| 18–20 years | 6315 | 4859 (76.94) | 1456 (23.05) | 67.30 | <0.0001 | 0.01187 | <0.0001 |
| 21–25 years | 21,211 | 16,047 (75.65) | 5164 (24.34) | ||||
| 26–30 years | 9649 | 7071 (73.28) | 2632 (27.27) | ||||
| 31–35 years | 2359 | 1703 (72.19) | 656 (27.80) | ||||
| >35 years | 552 | 357 (64.67) | 185 (33.51) | ||||
| Parity | |||||||
| Nullyparous | 18,648 | 13,480 (72.28) | 4918 (26.09) | 43.80 | <0.0001 | −0.1158 | <0.0001 |
| Multiparous | 21,438 | 16,513 (77.02) | 5175 (23.50) | ||||
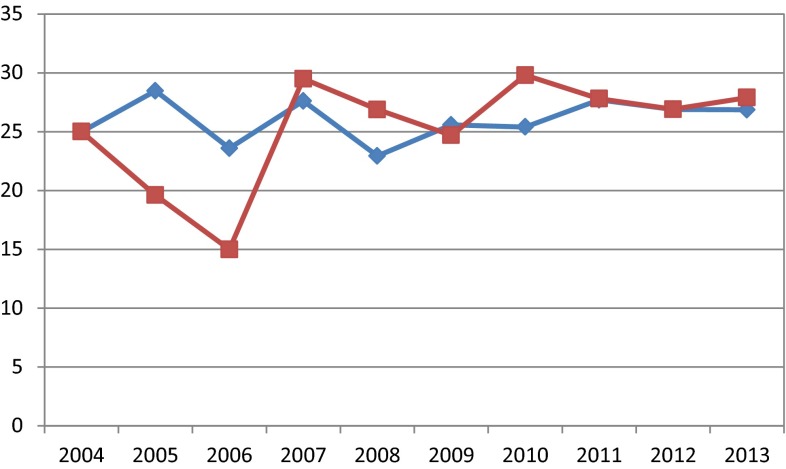
Figure 2 shows the neonatal mortality rate (NMR) for vaginal delivery, which varied from 25/1000 live births in 2004 to 26.8/1000 live births in 2013. The NMR for cesarean births was 25/1000 live births in 2004, which declined to 14.9/1000 in 2006, increased to 29.5 in 2007, and thereafter plateaued out at 27/1000 in 2013. Thus, the rise in CSR has not improved the neonatal mortality rate for babies delivered by cesarean section.
Fig. 2.
NMR for vaginal and cesarean deliveries
Discussion
Robson’s TGCS was successfully implemented to this dataset of 40,086, and it demonstrates the need to focus on the care of women in groups 1, 2, and 5 in particular, if CS rates are to be reduced. Women with single cephalic pregnancy at term without previous cesarean section and who entered into labor spontaneously (groups 1 and 3) represented 60 % of the total obstetric population. Group 2 (nulliparous with single cephalic pregnancy, ≥37 weeks gestation who either had labor induced or were delivered by CS before labor) and group 4 (multiparous without a previous uterine scar, with single cephalic pregnancy, ≥37 weeks gestation who either had labor induced or were delivered by CS before labor) had high group CSRs of 47.28 and 34.74 %, respectively, although the total group size was small (n = 1375;3.43 %). Their contribution to the overall CSR was 5.85 %. Groups 6 through 9 presented high rates of CS due to the particular obstetric conditions within which these are defined. However, their contribution to the overall CS rate was (11.44 %). Group 10 (All women with a single cephalic pregnancy ≥36 weeks gestation, including women with previous scars) was the third largest group (n = 6032;15 %) contributing 12.9 % to the overall CSR.
Robson stated that the Cesarean delivery rate in Group 1 should be below 15 %, and in group 4, it should be below 20 %. In our study, the rates of CS were 25.44 % in group 1 and 34.74 % in group 4. The higher-than-acceptable CSR is probably because of the high CSR for non-reassuring fetal heart rate pattern [6].
The 25.44 % of CSR in group 1 contrasts markedly with other published rates such as the 6.7 % in the National Maternity Hospital in Dublin in 2006 [7], or 14.8 % in New Jersey in 2004, but is closer to the WHO global survey in Latin America (27.7 %) [8].
Group 3, multiparous women with a singleton foetus in a normal cephalic presentation, who enter labor spontaneously at term, usually constitutes the largest group among all delivering women representing 31 % of the total population in the present study. Compared with other groups, these women are less likely to have obstetric indications for CS since they present very low risk in general. Hence, the CS rate in this group can be expected to be low. However, in our study, the CS rate in this group was 11.62 %. This is similar to the WHO Global survey in Latin America where they found a CS rate of 10 % in this group [9].
A study by Lithorp et al. on a dataset of 137,094 from 2000 to 2011 found that the three largest groups (groups 1, 3, and 5) contributed most to the total CS rate over the study period [10].
Howell et al. applied the TGCS retrospectively to the Queensland Perinatal data and found that CS rates have risen in all groups under Robson’s TGCS between 1997 and 2006. The trend was pronounced among multiparous women with a previous cesarean delivery (Group 5), among women with multiple pregnancies (Group 8), and among nulliparous women who had labor induced or were delivered by CS prior to the onset of labor (Group 2) [11].
Brennan et al. analyzed data from nine institutional cohorts (total 47,402; range 1962–7985) from nine different countries using this classification system. They found that the overall CS rates correlated with the CS rates in singleton cephalic nullipara (r = 0.992; P < 0.001). While CS rates in induced labor were similar, the greatest institutional variations were seen in spontaneously laboring multiparas (6.7-fold difference) and nulliparas (3.7-fold difference).The authors concluded that the Ten-group analysis of international obstetric cesarean practice identifies wide variations in women in spontaneous cephalic term labor, a low-risk cohort amenable to effective intrapartum corrective intervention [12].
A WHO global survey using the Ten-group classification found that the overall rate of cesarean section was 35.4 %. Women with single cephalic pregnancy at term without previous cesarean section who entered into labor spontaneously (groups 1 and 3) represented 60 % of the total obstetric population. Although women with a term singleton cephalic pregnancy with a previous cesarean section (group 5) represented only 11.4 % of the obstetric population, this group was the largest contributor to the overall CSR (26.7 % of all the cesarean sections). The second and third largest contributors to the overall CSR were nulliparous women with single cephalic pregnancy at term in spontaneous labor (group 1) and induced or delivered by cesarean section before labor (group 2), which were responsible for 18.3 and 15.3 % of all cesarean deliveries, respectively [9].
In our study, Cesarean section for fetal distress was the leading indication varying from 42.7 % in group 1 to 56 % in group 4. The second leading indication was abnormal pelvis. Failure of induction was seen in 108 (25.29 %) in group 2 and 28 (17.0) % in group 4. In group 10, the leading indications for CS were fetal distress (409, 31.41 %) and previous scar (213, 16.35 %).
In a study by Barber et al., the cesarean delivery rate increased from 26 to 36.5 % between 2003 and 2009; 50.0 % of the increase was attributable to an increase in primary cesarean delivery. Among the documented indications, non-reassuring fetal status, arrest of dilation, multiple gestation, preeclampsia, suspected macrosomia, and maternal request increased over time, while arrest of descent, malpresentation, maternal-fetal indications, and other obstetric indications (e.g., cord prolapse, placenta previa) did not increase [13]. Other studies from China and Bangladesh have reported similar results [14–16].
Cesarean section rates did not significantly improve the neonatal mortality rates. A WHO in a publication has stated that perinatal mortality declines are steep until CSRs reach approximately 8 per cent of deliveries, after which point the relationship becomes less clear [9]. Goldenberg et al. and Stanton et al. [16, 17] observed that Cesarean section availability in low-/middle-income countries was associated with reductions in intrapartum stillbirths. They reported that intrapartum stillbirths dropped by 1.61 per 1000 births for every one percentage point increase in Cesarean section from 0 to 8 per cent. Thereafter, they observed a small, nonsignificant increase in intrapartum stillbirths for each per cent increase in Cesarean section.
The Ten-group classification is based on well-defined parameters, and it could be easily applied to this dataset of 40,086 deliveries. It helped to identify the main groups of subjects who contribute most to the overall CS rate. It also helped to identify subgroups requiring closer monitoring for more in-depth analyses of the indications for cesarean section. It is important to focus on the first four groups of TGCS which constitute about 75 % of all deliveries. It is in the low-risk groups that one is likely to find the highest and most inappropriate indications for cesarean sections.
Dr. Rayshang G Yadav
had completed his MBBS from S. P. University, Vallabh Vidyanagar, Gujarat. He worked as Class 2 Medical Officer for 10 years in a Community Health Center in Bhavnagar district. He then completed residency training in Obstetrics and Gynecology from the Medical College Baroda in April 2015. He is presently working as a Superintendent and fulltime Gynecologist at the Community Health Center in Sihor, Bhavnagar District, Gujarat. 
Compliance with Ethical Standards
Conflict of interest
Dr. R. G. Yadav has no conflict of interest; Dr. Nandita Maitra has no conflict of Interest.
Ethical standards
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed consent
None.
Footnotes
Rayshang G. Yadav is a Class 2 Medical Officer and Nandita Maitra is the Professor and Head at Department of Obstetrics and Gynecology, The Medical College, Baroda, Vadodara, India.
References
- 1.National Institutes of Health state-of-the-science conference statement Cesarean delivery on maternal request. Obstet Gynecol. 2006;107:1386–1397. doi: 10.1097/00006250-200606000-00027. [DOI] [PubMed] [Google Scholar]
- 2.Appropriate technology for birth. Lancet 1985;2:436–7. [PubMed]
- 3.Department of Health and Human Services; Centers for Disease Control and Prevention; National Center for Health Statistics. Healthy People 2000: national health promotion and disease prevention objectives: Full report, with commentary (DHHS publication no. (PHS) 91–50212). Washington: Government Printing Office; 1990:378.
- 4.Robson MS. Can we reduce the cesarean section rate? Best Pract Res Clin Obstet Gynaecol. 2001;15:179–194. doi: 10.1053/beog.2000.0156. [DOI] [PubMed] [Google Scholar]
- 5.Torloni MR, Betran AP, Souza JP, et al. Classifications for cesarean section: a systematic review. PLoS ONE. 2011;6(1):e14566. doi: 10.1371/journal.pone.0014566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Perinatal Services BC (2011). Examining caesarean delivery rates in British Columbia using the Robson Ten Classification. Part 1: Understanding the Ten Groups. Vancouver.
- 7.Sachs BP, Kobelin C, Castro MA, et al. The risk of lowering the caesarean delivery rate. N Engl J Med. 1999;340(1):54–57. doi: 10.1056/NEJM199901073400112. [DOI] [PubMed] [Google Scholar]
- 8.Denk CE, Kruse LK, Jain NJ. Surveillance of caesarean section deliveries, New Jersey 1999–2004 New Jersey Department of health and SeniorServices; 2005.
- 9.Betran AP, Gulmezoglu AM, Robson M, et al. WHO global survey on maternal and perinatal health in Latin America: classifying caesarean sections. Reproductive Health. 2009;6:18. doi: 10.1186/1742-4755-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Litorp H, Kidanto HL, Nystrom L, et al. Increasing caesarean section rates among low-risk groups: a panel study classifying deliveries according to Robson at a university hospital in Tanzania. BMC Pregnancy and Childbirth. 2013;13:107. doi: 10.1186/1471-2393-13-107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Howell S, Johnston T, Macleod S-L. Trends and determinants of caesarean sections births in Queensland, 1997–2006. ANZJOG. 2009;49(6):606–611. doi: 10.1111/j.1479-828X.2009.01100.x. [DOI] [PubMed] [Google Scholar]
- 12.Brennan DJ, Robson MS, Murphy M, et al. Comparative analysis of international caesarean delivery rates using 10-group classification identifies significant variation in spontaneous labor. Am J Obstet Gynecol. 2009;201:308.e1–308.e8. doi: 10.1016/j.ajog.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 13.Barber EL, Lundsberg LS, Belanger K, et al. Contributing indications to the rising delivery rates. Obstet Gynecol. 2011;118(1):29–38. doi: 10.1097/AOG.0b013e31821e5f65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gao Y, Xue Q, Chen G, et al. An analysis of the trends in caesarean section in a teaching hospital in China. Eur J Obstet Gynecol Reprod Biol. 2013;170(2):414–418. doi: 10.1016/j.ejogrb.2013.08.009. [DOI] [PubMed] [Google Scholar]
- 15.Aminu M, Utz B, Halim A, et al. Reasons for performing a caesarean section in public hospitals in rural Bangladesh. BMC Pregnancy Childbirth. 2014;14(1):130. [DOI] [PMC free article] [PubMed]
- 16.Goldenberg RL, McClure EM, Bann CM. The relationship of intrapartum and antepartum stillbirth rates to measures of obstetric care in developed and developing countries. ActaObstet Gynecol Scand. 2007;86:1303–1309. doi: 10.1080/00016340701644876. [DOI] [PubMed] [Google Scholar]
- 17.Stanton C, Lawn JE, Rahman H, et al. Stillbirth rates: delivering estimates in 190 countries. The Lancet. 2006;367:1487–1494. doi: 10.1016/S0140-6736(06)68586-3. [DOI] [PubMed] [Google Scholar]