Abstract
Purpose
The present study is a prospective, randomized comparative study of abdominal, vaginal and laparoscopic hysterectomies comparing various parameters such as indications, blood loss, post operative pain, time taken for surgery, intraoperative and postoperative complications and total hospital stay.
Materials and Methods
50 patients were selected in each group over a period of 18 months. The patients were selected in such a way that they could be operated by all 3 routes. Thus patients undergoing hysterectomy for non malignant conditions, having no adnexal masses, having no severe endometriosis, uterine size not more than 12 weeks and uterine descent of not more than 1st degree were selected.
Results
The most common indication for hysterectomy was found to be DUB, the maximum time taken was in TLH, the minimum blood loss was found in TLH. There was significant difference in the pain scores using VAS among the three groups on day 0 and day 1, where the scores were significantly lower in VH group, the hospital stay was maximum in TAH group while there was no difference between VH and TLH groups.
Conclusion
TLH is a better alternative for TAH and with good equipment, expertise and excellent teamwork TLH will be the future candidate for mode of surgery.
Keywords: Abdominal hysterectomy, Vaginal hysterectomy, Laparoscopic hysterectomy
Introduction
Hysterectomy is one of the most common operations performed by the gynecologist. Until recently, a hysterectomy could either be performed abdominally or vaginally. In the recent years, there have been enormous advances in our ability to use minimal invasive surgeries to access the abdominal and pelvic cavities.
At present, hysterectomy [1] can be performed in several ways, and many techniques have been devised and modified to suit individual requirements. Laparoscopy has revived the thought process of choosing the best route and/or technique for hysterectomy but has confused many young and inexperienced gynecologists regarding definitive criteria for selection. Fortunately, one can pick and choose the right technique except in a small gray zone of cases between total laparoscopic hysterectomy (TLH) and total abdominal hysterectomy (TAH), and vaginal hysterectomy (VH). Most of the times, it is difficult to decide the type of surgery, which depends on the experience of the operating surgeon. The decision should be the optimal one for a given patient under the given circumstances.
No other factor should interfere in this holistic decision, keeping in mind the advice of Hippocrates, “If choicest is not chosen it is harm” and “If you can do no good, do no harm”.
In this era of evidence-based medicine, clear scientific evidence exists to determine the superiority for selection between all three methods available that is VH, TAH, and TLH.
Aims and Objectives
Aims and objectives of the present study were to compare the following:
Indications
Intraoperative and postoperative complications
Times taken for surgery
Blood loss
Postoperative pain and mobilization
Duration of hospital stay
The above mentioned parameters were studied in Vaginal, Abdominal and Laparoscopic Hysterectomies carried out by surgeons of similar caliber at our teaching institute.
Materials and Methods
150 patients were taken into this study over a period of 18 months at a tertiary care charitable hospital.
Patients satisfying the following conditions were included in the study as they could be operated by any of the three routes.
Patients undergoing hysterectomy for
Non-malignant conditions.
Having no adnexal masses.
Having no severe endometriosis.
Having descent of no more than 1st degree of uterus.
Uterine size <12 weeks.
They were randomly selected for any of the three routes of surgery and the results were compared
Results and Observations
The outcomes and observations of this study are given in Table 1 and Charts 1, 2, and 3.
Table 1.
Indications
| Diagnosis | Group | Total | |||
|---|---|---|---|---|---|
| Abdominal | Laparoscopy | Vaginal | |||
| DUB | No. | 27 | 22 | 28 | 77 |
| % | 54.0 % | 44.0 % | 56.0 % | 51.3 % | |
| Fibroid | No. | 19 | 19 | 19 | 57 |
| % | 38.0 % | 38.0 % | 38.0 % | 38.0 % | |
| Adenomyosis | No. | 4 | 8 | 3 | 15 |
| % | 8.0 % | 16.0 % | 6.0 % | 10.0 % | |
| Others | No. | 0 | 1 | 0 | 1 |
| % | 0.0 % | 2.0 % | 0.0 % | 0.7 % | |
| Total | No. | 50 | 50 | 50 | 150 |
| % | 100.0 % | 100.0 % | 100.0 % | 100.0 % | |
The most common indication for hysterectomy was dysfunctional uterine bleeding (51.3 %)
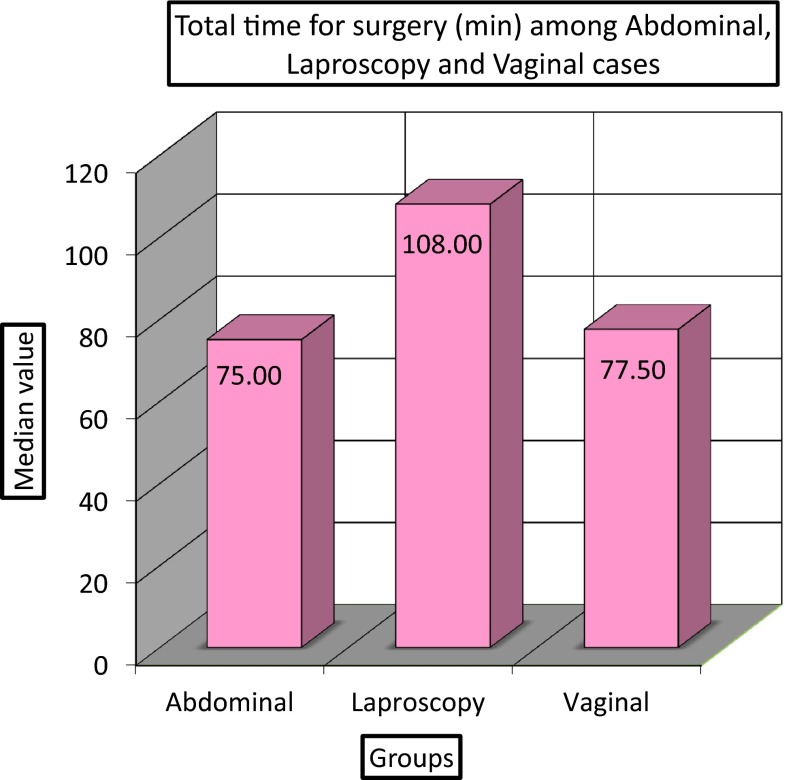
Chart 1.
Total time for surgery. The average time taken for total laparoscopic hysterectomy was 108 min, time taken for abdominal hysterectomy was 75 min, and time taken for vaginal hysterectomy was 77.50 min
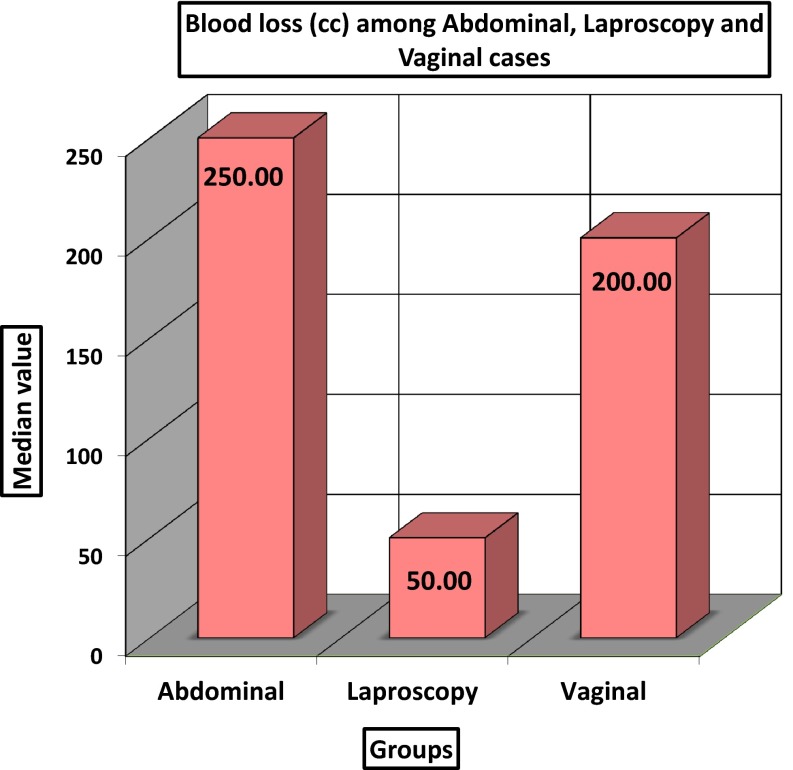
Chart 2.
Blood loss. The average blood loss for total laparoscopic hysterectomy was the least
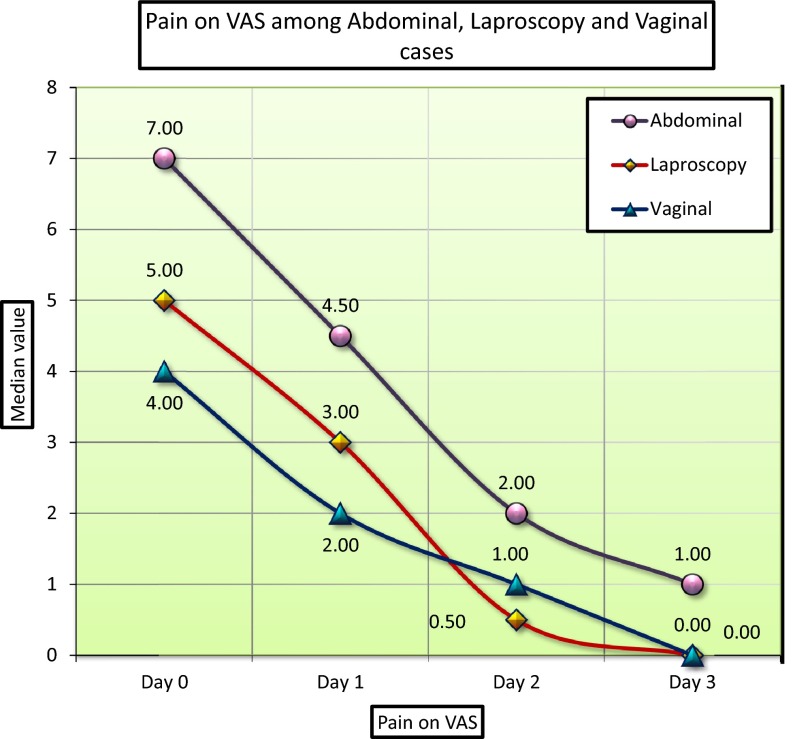
Chart 3.
Pain score on vas scale. Postop pain on VAS scale was the maximum in total abdominal hysterectomy on all the days postsurgery. There is no significant difference between the VAS score in patients undergoing vaginal and total laparoscopic hysterectomies on day 2 and day 3 postsurgery
Intraoperative Complications
One patient with a prior history of two cesarean sections undergoing TAH had an injury to the urinary bladder.
One patient undergoing TAH had a slippage of ligature to the uterine artery stump.
There were no cases of injury to the GI tract among all three routes.
Five patients undergoing TAH had to be given blood transfusion, while only one patient each in the other two groups underwent transfusion with blood.
Delayed Complications
Five patients who underwent abdominal hysterectomy had full-length wound gape. None of the TLH patients had wound gapes.
One patient undergoing abdominal hysterectomy had burst abdomen diagnosed on day 7 on wound inspection.
Two patients undergoing VH had vault prolapsed and two patients undergoing VH had vault granulomas.
1 patient undergoing TLH had been diagnosed with deep vein thrombosis found on day 3 of the surgery.
92.7 % of the patients had no delayed complications (Chart 4).
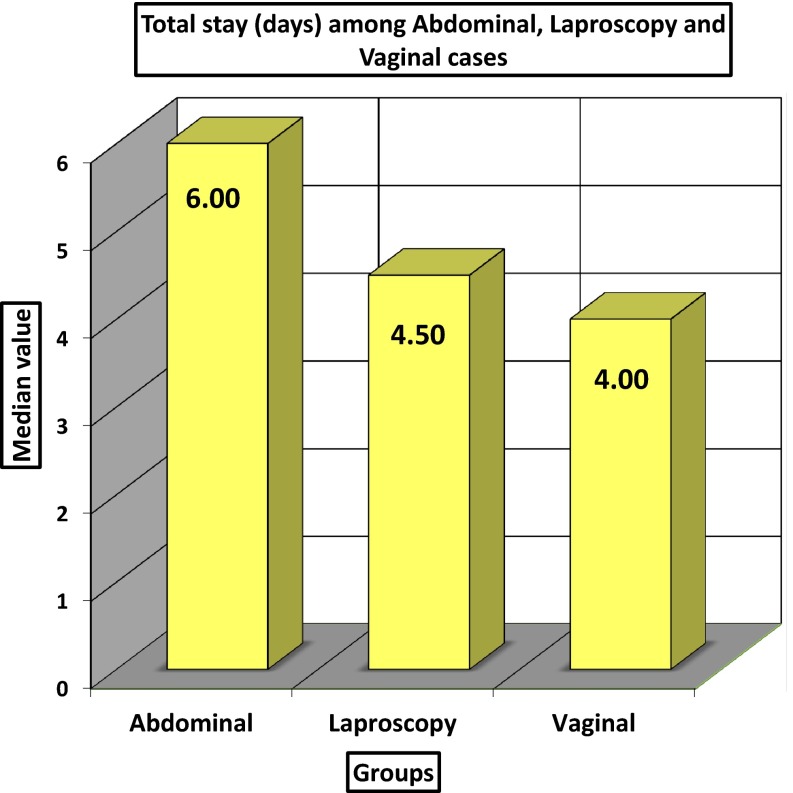
Chart 4.
Total hospital stay. The total hospital stay was maximum in TAH group with average stay of 6 days. There was no significant difference in hospital stay between VH and TLH groups
Discussion
Indications
The most common indication for hysterectomy in the present study was found to be DUB (51.3 %), 38 % of the cases had fibroid, 10 % were suffering from adenomyosis, and 1 case was that of severe mental retardation.
Comparison
Operating Time (min)
The average operating time was maximum in TLH in the present study and was comparable to other studies which showed the same result. However, today many experienced and trained laparoscopic surgeons perform laparoscopic hysterectomy in shorter time. Time is cut short nowadays due to the larger number of cases performed, and due to experience and more sophisticated equipments.
Blood Loss (ml)
In the present study, the blood loss was minimum in cases of TLH with the average blood loss being 50 ml.
The maximum blood loss was seen in Total abdominal hysterectomy (TAH) in the present study with the average blood loss being 250 ml. There was no significant difference between the blood losses in TAH and VH (p value >0.05).
The average blood loss in the present study was significantly lower in TLH compared to the other two groups (p value <0.05). The blood loss in TLH in the present study was also found to be much less compared to other studies.
The blood loss was found to be the least in TLH due to better magnification, better hemostasis due to vessel-sealing devices/coagulation devices, smaller incision, and pressure due to pneumoperitoneum.
Intraoperative Complications
In the present study, one patient undergoing abdominal hysterectomy had urinary bladder injury (2 %). One patient in the same group had excessive bleeding on table due to slippage of ligature. A total of five patients undergoing TAH had blood transfusion (10 %).
However, in the present study, no major intraoperative complications were found in TLH and VH group except in one patient in each group requiring blood transfusion due to blood loss (2 % in each group). There was significant difference in requirements of blood transfusion between abdominal hysterectomy and the other two groups (p value—0.041 by Fisher’s exact test).
A study conducted by O’Hanlan [6] on complications in TLH reported urinary tract injury in 2.8 %, GI tract injury in 0.8, whereas 3 % required blood transfusion.
Total complication compared to other studies:
Postoperative Complications/Morbidity
| Type of surgery | Postop fever (%) | Wound discharge (%) | Wound gape (%) | Burst abdomen (%) | Vault prolapse (%) | Vault granuloma (%) | DVT (%) |
|---|---|---|---|---|---|---|---|
| VH | 4 | 4 | 4 | 0 | |||
| TAH | 26 | 12 | 10 | 2 | 0 | 0 | 0 |
| TLH | 8 | 0 | 0 | 0 | 0 | 0 | 2 |
Postoperative morbidity was seen maximum in TAH group in the present study.
Zao [10] et al. 2009 in their study found that organ injury appeared to be relatively more common in abdominal hysterectomy than in laparoscopic and vaginal hysterectomies: 0.76 % in TAH, 0.21 % in TLH, and 0 % in VH.
In their study, Zao et al. found pelvic hematoma and vaginal stump bleeding to be more common in TLH (1.65 %) and VH (3.08 %) than in TAH (0.76 %). Wound dehiscence was only found in TAH.
Hospital Stay (days)
The maximum hospital stay was compared for cases of TAH in the present study as well as in other studies.
In the present study, the average hospital stay was significantly higher in TAH compared to the other groups (p value <0.05). There was no significant difference in the hospital stay between VH and TLH (p value >0.05). The hospital stay was prolonged due to detailed observation of patients postop, as most patients belonged to lower strata of society, and there was fear of loss to follow-up.
Pain
Postoperative pain on VAS scale was maximum in TAH on all the days postsurgery compared to the other two routes (p value <0.05). There was no significant difference in pain on postop days 2 and 3 between TLH and VH groups (p value >0.05).
In a study done by Perino et al. it was observed that there was significantly more pain in patients undergoing TAH on all postoperation days compared to those undergoing TLH.
Conclusion
From the present study, it is concluded that with good expertise, equipment, and teamwork, the total laparoscopic hysterectomy (TLH) is better than total abdominal hysterectomy (TAH) and is the future candidate mode of surgery.
TAH was found to have maximum intraoperative and postoperative morbidities.
Patients undergoing TAH were mobilized earlier, started oral feeding earlier, and were discharged around the same time as in the case of vaginal hysterectomy (VH) despite it being an abdominally invasive route.
Patients undergoing TLH had cosmetically better scar than abdominal hysterectomy.
Unlike VH TLH has an advantage of identifying incidental pathology in the abdomen which could be missed on USG and due to better magnification and good vessel sealing device TLH had less blood loss or injury to adjacent organs compared to TAH and VH.
Patients undergoing TLH were highly satisfied due to all of the above reasons.
With better training in teaching institutions and training centers this surgery will be performed on a larger scale and with the cost of the equipment within the reach of most hospitals this surgery will come to stay. It will have its applicability as a routine surgery as is performed like conventional surgeries. As more surgeries will be performed laparoscopically and with greater innovation of the equipments and shorter learning curves it will be a great boon for the patients.
However, vaginal hysterectomies have their own advantages and whenever VH is easily possible it will remain the surgery of choice.
Dr. Anand Murari Nanavati
has obtained his M.B.B.S degree from Lokmanya Tilak Municipal Medical College, Mumbai, and after completing his post-graduation training at the National Board of Examination at K.J. Somaiya hospital, Mumbai, he obtained his DNB degree in June 2015. He has presented papers at the AICOG and MOGS conferences. 
Compliance with Ethical Standards
Conflict of interest
Anand Murari Nanavati and Sudhir Gokral declare that they have no conflict of interest.
Informed consent in studies with human studies
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all patients being included in this study.
Footnotes
Dr. Anand Murari Nanavati is a Resident at KJ Somaiya hospital and Research Centre, Mumbai; Sudhir B. Gokral is a Professor at KJ Somaiya hospital and Research Centre, Mumbai.
References
- 1.Gomel V. Operative laparoscopy: time for acceptance. Fertil Steril. 1989;52:1–11. doi: 10.1016/S0015-0282(16)60779-3. [DOI] [PubMed] [Google Scholar]
- 2.Bharatnur S. Comparative study of abdominal versus vaginal hysterectomy in non-descent cases. Internet J Obstet Gynaecol. 2010;15(2):1528. [Google Scholar]
- 3.Chakraborty S, Goswami S, Mukherjee P, et al. Hysterectomy….Which route? J Obstet Gynaecol India. 2011;61(5):554–557. doi: 10.1007/s13224-011-0076-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schindlebeck C, Klauser K, Dian D. Comparison total laparoscopic, vaginal and abdominal hysterectomy. Arch Gynaecol Obstet. 2008;277(4):331–332. doi: 10.1007/s00404-007-0481-7. [DOI] [PubMed] [Google Scholar]
- 5.Aninliene R, Varzgaliche L, Varzgalis M. A comparative analysis of hysterectomies. Medicina (Kaunas) 2007;43(2):118–124. [PubMed] [Google Scholar]
- 6.O’Hanlan KA, Dibble SL, Garnier AC. Total laparoscopic hysterectomy: technique and complications of 830 cases. JSLS. 2007;11(1):45–53. [PMC free article] [PubMed] [Google Scholar]
- 7.Landen LB, Bell MC, Hubert HB, et al. Clinical and cost comparisons for hysterectomy via abdominal, standard laparoscopic, vaginal and robot-assisted approaches. SD Med. 2011;64(6):197–199. [PubMed] [Google Scholar]
- 8.Meltomaa SS, Makinen J, Taalikka MC, et al. One-year cohort of abdominal, vaginal, and laparoscopic hysterectomies: complications and subjective outcomes. J Am Coll Surg. 1999;189(4):389–396. doi: 10.1016/S1072-7515(99)00170-2. [DOI] [PubMed] [Google Scholar]
- 9.Cosson M, Lambadic E, Bonkerran M. Vaginal, laparoscopic, or abdominal hysterectomies for benign disorders: immediate and early postoperative complications. Eur J obstet Gynaecol Reprod Biol. 2001;98(2):231–236. doi: 10.1016/S0301-2115(01)00341-4. [DOI] [PubMed] [Google Scholar]
- 10.Zao J, Tan XJ, Lang JH, et al. PMID:20137653. Zhongua Yi Xue Za Zhi. 2009;89(41):2931–2933. [PubMed] [Google Scholar]