Abstract
Introduction
Conventionally postpartum hemorrhage (PPH) has been defined as blood loss of more than 500 ml following vaginal delivery and 1000 ml following a cesarean section [Pritchard et al. in Am J Obstet Gynecol 84(10):1271–1282, (1962)]. Another definition labels PPH as any blood loss which causes a 10 % drop in hematocrit [Combs et al. in Obstet Gynecol 77:69–76, (1991)] or which threatens the hemodynamic stability of the patient and necessitates blood transfusion [Prendiville et al. in Cochrane Database Syst Rev 2:CD000007, (2000)]. The purpose of this study was to evaluate the effectiveness of condom tamponade in the management of massive obstetric hemorrhage.
Objective
To evaluate the efficacy of a condom as a tamponade for intrauterine pressure to stop massive PPH.
Methods
This prospective study was done in the Obstetrics and Gynecology Department of NIMS Medical College and Hospital, Jaipur, between December 2013 and February 2015. With aseptic precautions, a sterile rubber catheter fitted with a condom was introduced into the uterus. The condom was inflated with 250–500 ml normal saline according to need. Vaginal bleeding was observed, and further inflation was stopped when bleeding ceased.
Results
In all but 2 (94.44 %) the cases, postpartum bleeding was stopped within 10 min of creation of tamponade. On an average, 350 ml of normal saline was required to create adequate tamponade to stop the bleeding.
Conclusion
Use of condom tamponade can effectively help in reducing both maternal morbidity and mortality associated with PPH. Our study encourages use of condom tamponade which is efficient, cost-effective, easily available and requires lesser skills as compared to the traditional surgical procedures.
Keywords: Condom tamponade, Obstetric hemorrhage, Shivkar’s Pack, Intrauterine pressure to stop massive PPH
Introduction
Conventionally PPH has been defined as blood loss of more than 500 ml following vaginal delivery and 1000 ml following a cesarean section [1]. Another definition labels PPH as any blood loss which causes a 10 % drop in hematocrit [2] or which threatens the hemodynamic stability of the patient and necessitates blood transfusion [3].
Postpartum hemorrhage (PPH) is a leading cause of maternal death all over the world [4]. In developing countries, it is responsible for an annual mortality of approximately 150,000 women per year. It remains a serious complication of childbirth in both developed and developing countries. Two to five percentage of deliveries may lead to PPH with a blood loss of >1000 ml within the first 24 h [5]. Blood loss during first 24 h after delivery is known as primary PPH (placental/extraplacental, depending upon the site of bleed), whereas blood loss from after 24 h up to 6 weeks is termed as late or secondary PPH [6]. The most common cause of PPH is uterine atony. A delay in correction of hypovolemia and delay in the control of bleeding are the main avoidable factors in most maternal deaths caused by hemorrhage [7].
The idea of using a condom as a balloon tamponade was first generated and evaluated in Bangladesh in 2001 by Akhter [8] to fill a need and in response to the high cost of commercially available UBT devices. The precise mechanism of action for UBT is still unclear. The placenta is a low-pressure system, so it seems likely that when the placenta is the source of hemorrhage, the direct pressure of the balloon, even well below systemic pressure, will halt bleeding. When the hemorrhage is instead from an arterial source in the endometrium, it is possible that the balloon’s exerted pressure exceeds the arterial pressure and thus promotes clot formation. A third possibility is that the introduction of the balloon in the atonic uterus causes it to contract [9]. Further study is needed to determine the mechanism of action, which will in turn help ensure proper placement and monitoring.
The purpose of this study is to evaluate the effectiveness of condom tamponade in the management of massive obstetric hemorrhage.
Objective
To evaluate the efficacy of a condom as a tamponade for intrauterine pressure to stop massive postpartum hemorrhage (PPH).
Methods
This prospective study was done in the Obstetrics and Gynecology Department of NIMS Medical College and Hospital, Jaipur, between December 2013 and February 2015. This hospital is located at suburban area. Because of its location at suburban area, it caters to the rural as well as urban women. During the study period of 1 year, total number of delivery was 1756. Thirty-six consecutive patients who developed intractable PPH in the hospital and did not respond to the conventional medical management and in whom traumatic PPH was ruled out were selected.
Initial management of atonic PPH included resuscitative measures, correction of hypovolemia with intravenous fluid/blood transfusion, uterotonics, uterine massage and/or bimanual compression. In the majority of cases, the decision for condom tamponade was made when active continuous hemorrhage persisted despite these initial conservative measures.
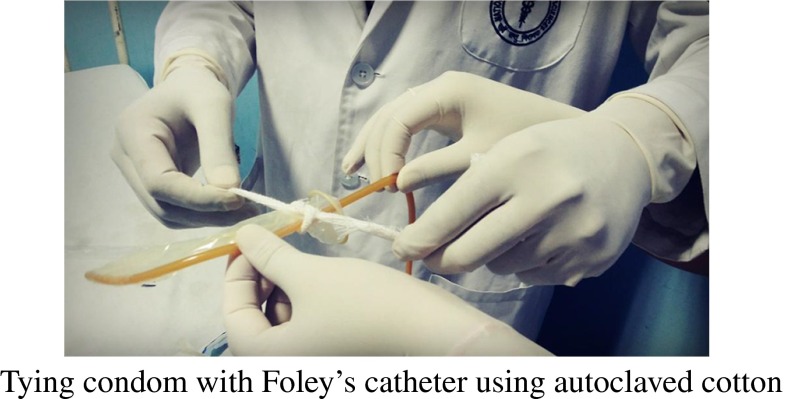
With aseptic precautions, a condom was rolled over a Foley’s catheter (no. 20) and tied with a cotton thread on two sites 1 cm apart. It was inserted as follows.
Condom along with tubing inserted into the uterus. With hands or with sponge holder, it was held lightly else condom may get punctured. (Replaced with a new one when it happened). The catheter was tightened by an umbilical clamp or cotton string and taped to the thigh. Vagina was loosely packed. Indwelling catheter was left in bladder till the condom tamponade was in place. Fundal height was marked on abdomen.
To keep the balloon in situ, the vaginal cavity was filled with roller gauze and finally a sanitary pad. If bleeding continues, this vaginal pack will usually become soaked with blood, and if profuse it will trickle through the introitus to soak the outside pad and undergarments. This did not happen in any of our cases. Take care not to kink the plastic tubing. Make patient’s position comfortable by removing lithotomy position if given.
The fluid source was kept at 60 cm above the abdomen with patient in lying down position, and now the condom balloon was inflated.
- Airway needle was applied to fluid source to open the system to environmental pressure.
- Balancing the hydrostatic pressure with uterine tone (Shivkar’s Pack) [10].
After releasing the flow controller, fluid rushed through the tubing, inflating and pressurizing the uterovaginal canal. As the pressure developed in the condom balloon the fluid flow was reduced and eventually stopped if sufficient uterovaginal tone exists. If the flow continued indefinitely or eventually increased, then we are going in the overstretched uterovaginal condition. This condition will invite more hemorrhage. The fluid source was lowered gradually, till the fluid flow stopped completely or preferably the reversal of fluid flow was observed. This will ensure against overstretched uterovaginal condition. After inflating to 300–400 ml of warm saline using 20-ml syringe, fluid source was lowered to 25 cm from the abdomen to see the reversal of flow. When there was no reversal of flow, further lowering by 5 cm every 5 min was advised to see the reversal of flow. After observing the reversal of flow, height of fluid source was increased if necessary and possible without further appreciable distension (not >50 ml). All the measures to increase uterine tone, i.e., uterotonics, blood transfusion, oxygen and calcium, were continued. Blood loss was measured by keeping a kidney tray at perineum after packing. When blood loss was less than 25 ml/h, it was ignored. If it was up to 50 ml, the availability of blood was checked for transfusion. If it was more than 50 ml, alternative treatment was searched. We did not require any of these.
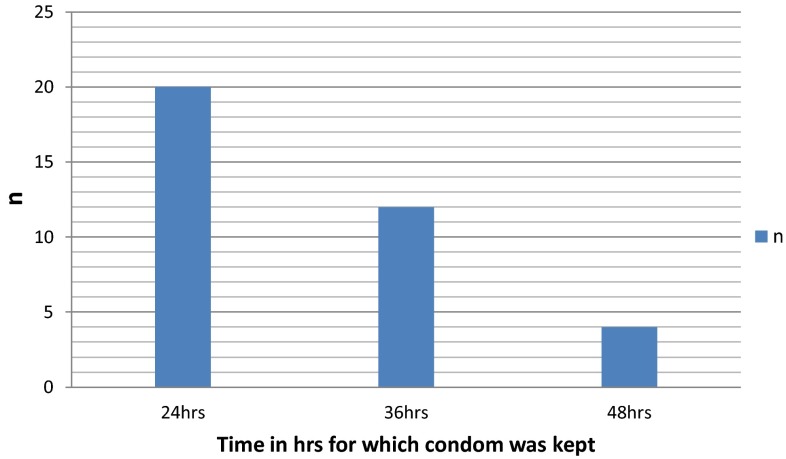
Antibiotics were also administered prophylactically because of the presence of a foreign body inside the uterus. The triple antibiotic regimen used was amoxicillin (500 mg every 6 h) plus metronidazole (500 mg every 8 h) plus gentamicin (80 mg every 8 h) administered intravenously for 7 days. High vaginal culture swab was done to determine whether there was any invading organism even after giving antibiotics, as some organisms may be resistant to this triple antibiotic regimen. None of our patients had any signs of infection, and all the culture reports were sterile. The condom catheter was kept in situ for 24–72 h depending on the severity of initial blood loss.
Results
Patients were in the age group of 19–37 years with a mean age of 28 years with their parity ranging from 1 to 6 with a median of 3. Gestational age was ranging between 10 and 41 weeks.
| Age | Range (19–37) | Mean 28 |
| Parity | Range (1–6) | Median 3 |
| Gestational age | Range (10–41 weeks) |
Of the 36 patients, 23 were booked, which formed around 63.88 %.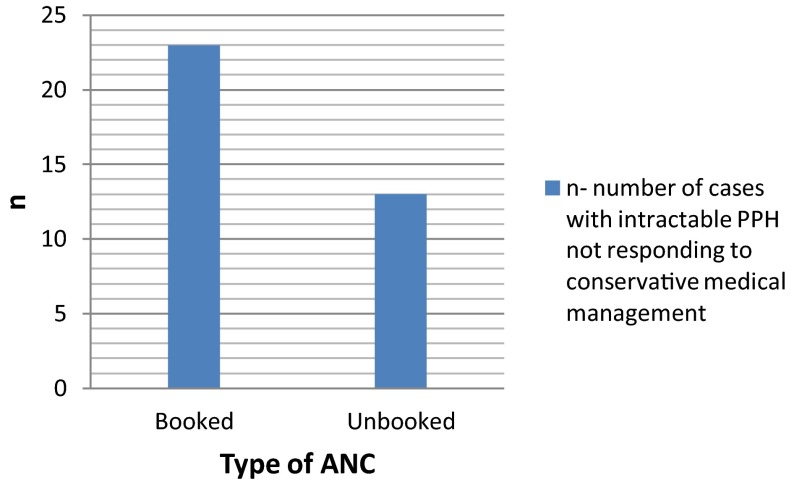
Of the 36 patients, 32 (88.88 %) were of primary PPH and 4 (11.12 %) of secondary PPH. Six patients were in shock at the time of intervention.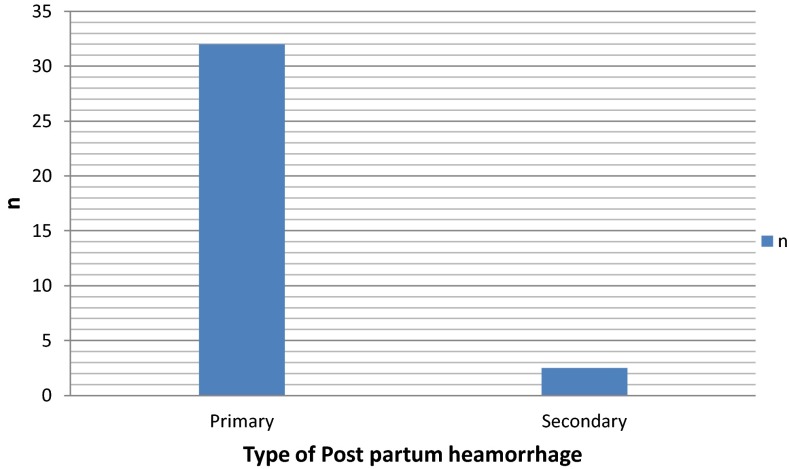
Of the 36 cases, 30 were delivered in hospital, which formed around 83.33 %.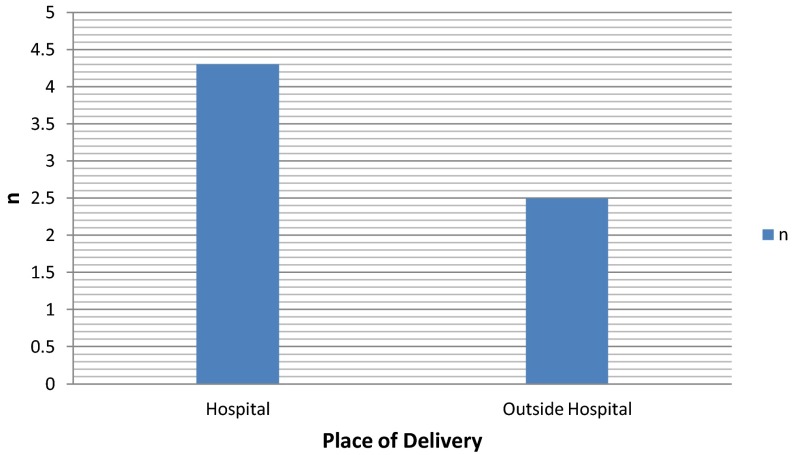
Majority of cases 33 (91.66 %) had spontaneous vaginal delivery and 3 (8.34 %) cases were following a cesarean section.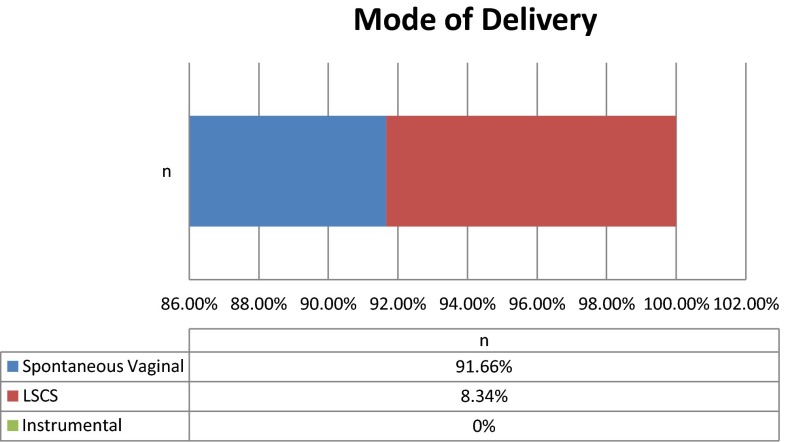
In 34 cases out of 36, PPH occurred within first 24 h and in rest of the two cases PPH occurred on second day.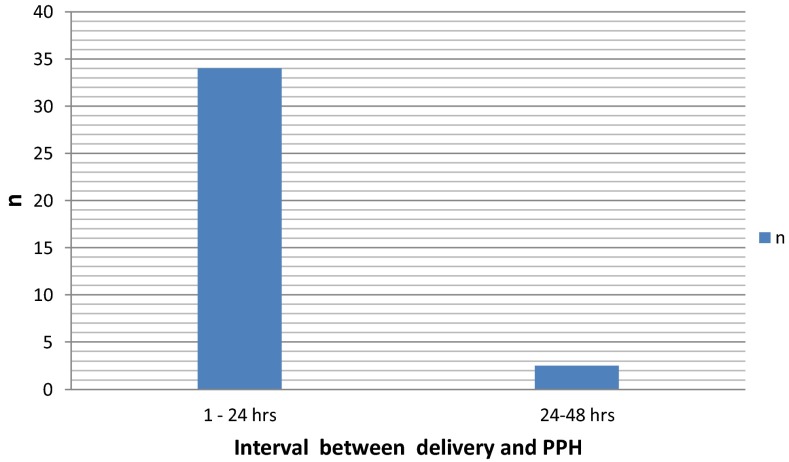
Introduction of Condom
In 34 (94.44 %) cases, condom catheter was introduced within 6 h, while in 2 (5.56 %) cases of secondary PPH on day 2.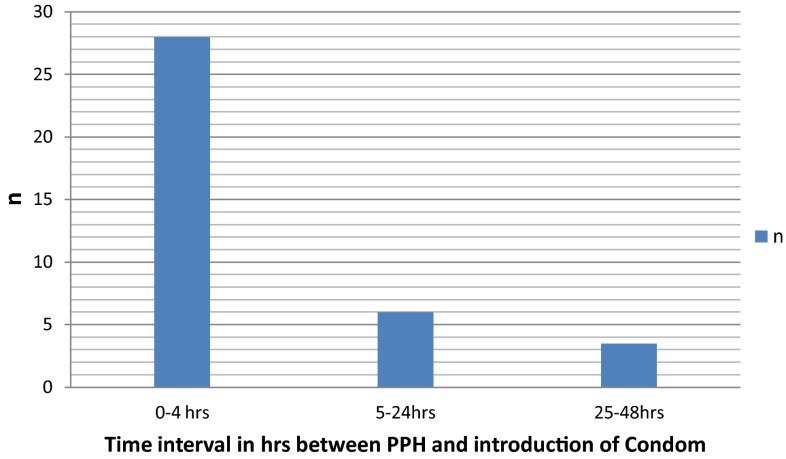
Time in hrs for which condom was kept for Predisposing factors and causes of PPH
In all but 2 (94.44 %) the cases, postpartum bleeding was stopped within 10 min of creation of tamponade.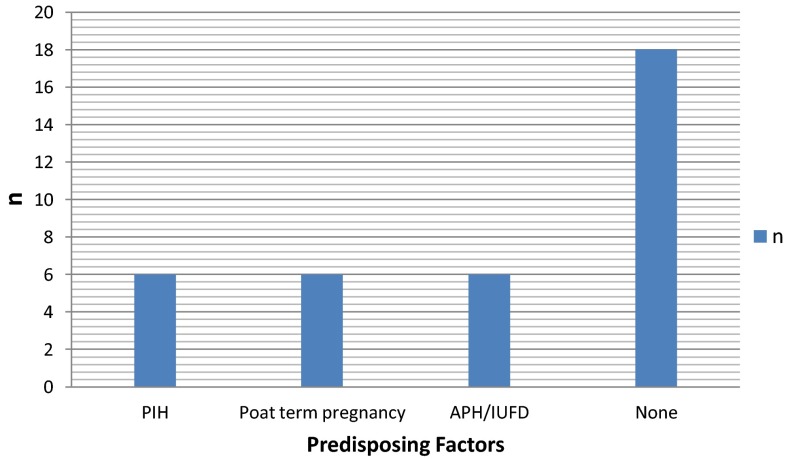
Average Time required for controlling PPH = 0–10 min.
On an average, 350 ml of normal saline was required to create adequate tamponade to stop the bleeding. Blood and crystalloids were transfused as per the assessment of individual patient. There was no difficulty found in applying condom tamponade in patients who delivered by LSCS, and procedure remained the same. No patient went into irreversible shock, and no patient developed any signs of sepsis. Patients were monitored in the hospital for 1 week.
Average Blood transfusion needed = 3 units.
Of the 34 patients (94.44 %) with successful tamponade, none required any further intervention and did not develop any further complications. Out of the remaining two patients who did not respond to tamponade and continued to bleed, one was treated with B-lynch suturing and in the other one emergency hysterectomy was performed.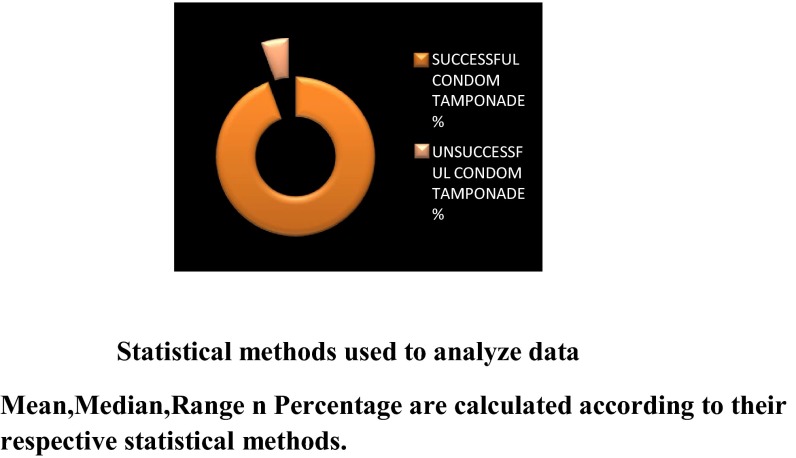
Discussion
PPH—a major composite of obstetric hemorrhage—is ubiquitous as it can kill “even a healthy woman within 2 h, if unattended” [11]. Despite its ubiquity, the root causes of PPH remain obscure; however, the four Ts (tone, trauma, tissue and thrombin) [12] are considered the major factors resulting into the PPH. About 1 in 200 women suffer from massive hemorrhage, which can be severe enough to cause hypotension and shock. Although most can be treated successfully with conservative measures, such as medication, about 10 % of the women with PPH require major surgical procedures and even hysterectomy to save their lives (Rouf S et al., unpublished data). Surgical options for major PPH include uterine compression sutures, vessel ligation and hysterectomy. These procedures are invasive, involve laparotomy, require specialist expertise, may be associated with significant morbidity and may compromise future fertility. In contrast, the balloon tamponade is simpler and handy alternative for arresting the bleeding. It is a well-recognized therapy in patients of intractable PPH, especially due to atony, coagulopathy and placenta accreta, and most of the patients with intractable PPH do respond to tamponade by various balloon devices such as Sengstaken–Blakemore tube, Foley’s catheter and the less expensive “Bakri tube” and condom catheter.
From our results, we can state that condom tamponade saves both time and money with positive results in approximately 95 % cases. It can be used effectively in developing countries as an efficient alternative to the surgical methods of controlling obstetric hemorrhage.
Conclusion
Use of condom tamponade can effectively help in reducing both maternal morbidity and mortality associated with PPH. Our study encourages use of condom tamponade which is efficient, cost-effective, easily available and requires lesser skills as compared to the traditional surgical procedures.
Acknowledgments
Special thanks to Dr. Pallavi Rathod, Dr. Raksha Sharma, Dr. Shilpa Gupta, Dr. Sumedha Aggarwal and Nessy John.
Dr. Rakesh Hasabe
I have done my MBBS from RCSM GMC, Kolhapur, and now I am studying in second year of DNB at NIMS University, Jaipur. I want to go for higher studies after DNB probably in infertility.
Compliance with Ethical Standards
Conflict of interest
Dr. Rakesh Hasabe, Dr. Kumud Gupta and Dr. Pallavi Rathode declare that they have no conflict of interest.
Human and Animal Rights
This article does not contain any studies with human or animal subjects.
Footnotes
Dr. Rakesh Hasabe is a MBBS from RCSM GMC, Kolhapur, second year of DNB at NIMS University, Jaipur; Dr. Kumud Gupta is a Associate Professor of NIMS University Jaipur; Dr. Pallavi Rathode is a MBBS from RCSM GMC, Kolhapur.
References
- 1.Pritchard J, Baldwin R, Dickey J, et al. Blood volume changes in pregnancy and the puerperium. Am J Obstet Gynecol. 1962;84(10):1271–1282. [Google Scholar]
- 2.Combs C, Murphy E, Laros R. Factors associated with postpartum hemorrhage and vaginal births. Obstet Gynecol. 1991;77:69–76. [PubMed] [Google Scholar]
- 3.Prendiville W, Elbourne D, Mc Donald S. Active versus expectant management in the third stage of labor. Cochrane Database Syst Rev. 2000;2:CD000007. doi: 10.1002/14651858.CD000007. [DOI] [PubMed] [Google Scholar]
- 4.Hayman RG, Arulkumaran S, Steer PJ. Uterine compression sutures: surgical management of postpartum haemorrhage. Obstet Gynaecol. 2002;99:502–506. doi: 10.1016/s0029-7844(01)01643-x. [DOI] [PubMed] [Google Scholar]
- 5.Vangsgaard K. “B-Lynch-suture” in uterine atony. Ugeshr-Laeger. 2000;162:3468. [PubMed] [Google Scholar]
- 6.El-Rafaey H, Charles R. Postpartum hemorrhage: definitions, medical and surgical management. A time for change. Br Med Bull. 2003;67:20517. doi: 10.1093/bmb/ldg016. [DOI] [PubMed] [Google Scholar]
- 7.Maine D, Rosenfield A, Wallis M. Prevention of maternal death in developing countries. New York: The Center for Population of Family Health; 1999. [Google Scholar]
- 8.Akhter S, Begum MR, Kabir Z, et al. Use of a condom to control massive postpartum hemorrhage. Posted: September 11, 2003. Medscape General Medicine. 2003;5(3) © 2003 Medscape. [PubMed]
- 9.Yorifuji T, Tanaka T, Makino S, et al. Balloon tamponade in atonic bleeding induces uterine contraction: attempt to quantify uterine stiffness using acoustic radiation force impulse elastography before and after balloon tamponade. Acta Obstet Gynecol Scand. 2011;90(10):1171–1172. doi: 10.1111/j.1600-0412.2011.01169.x. [DOI] [PubMed] [Google Scholar]
- 10.Drshivkar’s Blog. ‘SHIVKAR’s PACK’. N.p., 2011. Web. 27 Aug. 2015.
- 11.World Health Organisation (WHO). The World Health Report 2005: make every mother and child count. Geneva: WHO Press; 2005. (Cited on March 25). http://www.who.int/whr/2005/en/index.html.
- 12.Evensen A, Anderson J, Chapter J. Postpartum hemorrhage: third stage pregnancy. 2013: e1–e20. (Cited on April 4, 2014). http://www.aafp.org/dam/AAFP/documents/about_us/initiatives/also-blso/also_syllabus/chapterj-postpartum-hemorrhage.pdf.