Abstract
Aim and Objectives
To analyze which is superior, Doppler velocimetry or non-stress test or both by means of categorization into four groups and comparing the prediction of perinatal outcome in high-risk pregnancies like anemia, hypertensive disorders of pregnancies.
Materials and Methods
This was a prospective study conducted at the Department of Obstetrics and Gynaecology, ISO KGH, Madras Medical College, Chennai, in the year 2014. Two hundred high-risk pregnancies like anemia, hypertensive disorders of pregnancy were included in the study. They were examined systematically, and Doppler velocimetry and non-stress test were done. The main vessels studied by Doppler were umbilical artery and middle cerebral artery, and the indices were calculated. The results of the non-stress test were interpreted as reactive and non-reactive. Based on the results of Doppler and non-stress test, the 200 cases were categorized into four groups and the results were analyzed.
Results
Among the 200 cases of high-risk pregnancies, those with a normal Doppler study and a reactive non-stress test had good perinatal outcome. When both were abnormal, there was a higher percentage of adverse outcome as compared to that of either Doppler alone being abnormal or non-stress test alone being non-reactive. It was also found that abnormal Doppler but with a reactive non-stress test had the advantage of prolonging the pregnancy and bringing a better outcome indicating that non-stress test is surely a good test of well-being. When Doppler was normal, but non-stress test was non-reactive, there was an increase in the rate of cesarean section.
Conclusion
Each method of fetal surveillance reflects different aspect of maternal and fetal pathophysiology. Hence, combining these will help to bring out better perinatal outcome.
Keywords: Doppler velocimetry, Non-stress test, High-risk pregnancy, Perinatal
Introduction
Fetal surveillance is performed to identify the “at-risk” fetuses correctly, and a timed intervention is more useful in cases of high-risk pregnancies.
Complete knowledge about the disease and some intervention possible at the correct time can prevent mortality and morbidity. The recent trend is to combine the modalities of fetal surveillance like biophysical profile, Doppler to monitor the fetuses.
Doppler Velocimetry [1, 2]
Doppler Effect
When the reflector or the target is moving, there is a shift in the frequency of the reflected echoes.
Doppler Detects
The presence or absence of flow,
Flow direction,
Flow characteristics.
Doppler Indices
S—peak systolic velocity,
D—end diastolic velocity,
S/D—systolic/diastolic ratio,
RI—resistance index—(S–D)/S,
PI—pulsatility index—(S–D)/M,
CPR—PI of MCA/PI of umbilical artery.
Doppler in Obstetrics
Uteroplacental circulation—uterine artery,
Feto-placental circulation—umbilical artery,
Fetal circulation—middle cerebral artery, ductus venosus.
Uterine Artery
Uterine artery is a branch of anterior division of internal iliac artery.
Uterine Artery Doppler
Up to 16 weeks of gestation, an early diastolic notch is usually present in the uterine artery.
Abnormalities in uterine artery Doppler are the presence of early diastolic notch in the second trimester, RI more than 0.6 and PI more than 1.45.
Abnormal uterine artery Doppler is a predictor of preeclampsia and IUGR.
Umbilical Artery [3]
Abnormal waveforms of the umbilical arteries occur in case of occlusion arteries of tertiary villi due to thrombosis, fibrinoid necrosis, etc.
Fetal Middle Cerebral Artery [4, 5]
Middle cerebral artery has the advantage of being highly reproducible, and hence, it is chosen for study. Fetal cerebral blood flow is controlled by an autoregulatory mechanism which responds to oxygen saturation. Reduction in oxygen saturation causes dilatation of the intracerebral vessels which leads to an increased diastolic blood flow to the brain. Doppler study is carried out just beyond the origin of MCA at the circle of Willis.
Doppler study of the MCA is also useful in fetal anemia which is reflected in the fetal MCA by increase in the PSV which is greater than 1.5 times MOM.
Cerebro-Placental Ratio
It is the ratio of PI in the umbilical artery to the PI in the MCA. In normal fetuses, it is greater than 1, while in fetal hypoxia it is less than or equal to 1.
The Non-stress Test
The following are the main components [6–9].
Baseline fetal heart rate,
Baseline variability of fetal heart rate,
Accelerations,
Decelerations.
Baseline Fetal Heart Rate
It is the average fetal heart rate in increments of 5 beats per minute for a minimum of 2 min during a 10-min segment.
Normal range: 110–160 beats per minute,
Tachycardia: More than 160 beats per minute,
Bradycardia: Less than 110 beats per minute.
Baseline Abnormalities
Tachycardia
Causes
Stress, hypoxia, infections, etc.
Bradycardia
Fetal hypoxemia.
Local anesthetics,
Partial cord compression.
Baseline Variability
It refers to fluctuations in the baseline FHR which are irregular in amplitude and frequency.
Absent: undetectable amplitude,
Minimal: amplitude 5 beats per minute,
Moderate: amplitude between 6 and 25 beats per minute,
Marked: amplitude more than 25 bpm.
Changes in Baseline Variability
-
(A)
Fetal hypoxia,
-
(B)
Fetal acidosis,
-
(C)
Prematurity,
-
(D)
Fetal sleep.
Accelerations
A visually apparent abrupt increase (onset to peak in less than 30 s) in the fetal heart rate. Causes: fetal movement, uterine contractions, fetal stimulation [10, 11].
Deceleration
These are decreases in the fetal heart rate which go at least 15 beats below the baseline and last at least 15 s.
Early Deceleration
Visually apparent usually symmetrical gradual decrease and return of the FHR associated with the uterine contraction.
Causes
Head compression.
Late Deceleration
Usually symmetrical gradual decrease and return of the FHR associated with the uterine contraction.
Intrauterine Causes
Placental insufficiency.
Variable Deceleration
Visually apparent abrupt decrease in FHR which may or may not be related to contractions and vary in onset in depth and duration.
Causes
Short or Long cord,
Oligohydramnios,
Sinusoidal Pattern
Visually apparent, smooth, sine wave-like undulating pattern seen in fetal anemia.
Categorization [12]
| Feature | Baseline (beats per minute | Variability | Decelerations | Accelerations |
|---|---|---|---|---|
| Reassuring | 110–160 | ≥5 | None | Present |
| Non-reassuring | 100–109 | <5 for 40–90 min | Typical variable decelerations with over 50 % of contractions occurring for over 90 min | The absence of accelerations with otherwise normal trace is of uncertain significance |
| 161–180 | Single prolonged deceleration for up to 3 min | |||
| Abnormal | <100 | <5 for >90 min | Either atypical variable decelerations with over 50 % of contractions or late decelerations, both for over 30 min | |
| >180 | ||||
| Sinusoidal pattern ≥10 min | Single prolonged deceleration for more than 3 min |
Materials and Methods
Study Design
Prospective study.
Duration of Study
One year.
Cases
The study included two hundred high-risk pregnancies attending antenatal clinic at ISO KGH who satisfied the inclusion criteria.
Inclusion Criteria
Women with gestational age greater than 34 weeks with risk factors like anemia, GDM.
Exclusion Criteria
Pregnancies with gestational age <34 weeks, postdated pregnancies, etc.
Complete history taking and general physical and systemic examination and investigations were done for all the patients. They were followed up till delivery, and the outcome was studied in detail. NST was repeated biweekly, and Doppler was performed once in 15 days or more frequently based on the findings.
Follow-Up
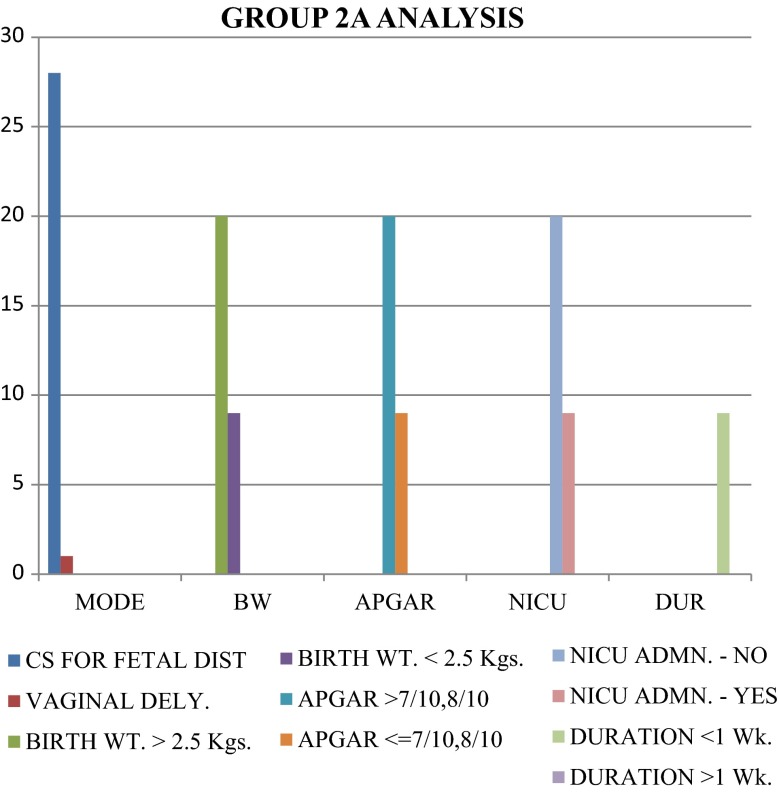
Gestational age at delivery, mode of delivery, APGAR, birth weight, NICU admission, etc., were the outcomes analyzed.
Results were tabulated, analyzed statistically and evaluated.
Patients were categorized into four groups as follows:
- Group I
Doppler normal and NST reactive,
- Group IIA
Doppler normal but NST non-reactive,
- Group IIB
Doppler abnormal but NST reactive.
- Group III
Doppler abnormal and NST non-reactive.
Results
Totally, 35 % cases had hypertensive disorders in pregnancy.
| Within the group | Group I | % | Group IIA | % | Group IIB | % | Group III | % |
|---|---|---|---|---|---|---|---|---|
| No | 86 | 68.80 | 12 | 41.38 | 6 | 60 | 25 | 69.44 |
| Yes | 39 | 31.20 | 17 | 58.62 | 4 | 40 | 11 | 30.56 |
| Total | 125 | 100 | 29 | 100 | 10 | 100 | 36 | 100 |
| Among the groups | No | % in “no” | Yes | % in “yes” |
|---|---|---|---|---|
| Group I | 86 | 66.67 | 39 | 54.93 |
| Group IIA | 12 | 9.30 | 17 | 23.94 |
| Group IIB | 6 | 4.65 | 4 | 5.63 |
| Group III | 25 | 19.38 | 11 | 15.49 |
| Total | 129 | 100 | 71 | 100 |
The incidence of GDM was 17 %
| Among the groups | No | % in “no” | Yes | % in “yes” |
|---|---|---|---|---|
| Group I | 105 | 63.25 | 20 | 58.82 |
| Group IIA | 23 | 13.86 | 6 | 17.65 |
| Group IIB | 9 | 5.42 | 1 | 2.94 |
| Group III | 29 | 17.47 | 7 | 20.59 |
| Total | 166 | 100 | 34 | 100 |
IUGR
| Within the group | Group I | % | Group IIA | % | Group IIB | % | Group III | % |
|---|---|---|---|---|---|---|---|---|
| No | 123 | 98.40 | 28 | 96.55 | 9 | 90 | 25 | 69.44 |
| Yes | 2 | 1.60 | 1 | 3.45 | 1 | 10 | 11 | 30.56 |
| Total | 125 | 100 | 29 | 100 | 10 | 100 | 36 | 100 |
| Among the groups | No | % in “no” | Yes | % in “yes” |
|---|---|---|---|---|
| Group I | 123 | 66.49 | 2 | 13.33 |
| Group IIA | 28 | 15.14 | 1 | 6.67 |
| Group IIB | 9 | 4.86 | 1 | 6.67 |
| Group III | 25 | 13.51 | 11 | 73.33 |
| Total | 185 | 100 | 15 | 100 |
P value <0.001
Totally, there were 15 cases of IUGR, and 74 % of them belonged to Group III. P value is <0.001 and hence highly significant.
LIQUOR
| Within the group | Group I | % | Group IIA | % | Group IIB | % | Group III | % |
|---|---|---|---|---|---|---|---|---|
| Normal | 117 | 93.60 | 23 | 79.31 | 8 | 80 | 25 | 69.44 |
| Oligohydramnios | 6 | 4.80 | 6 | 20.69 | 2 | 20 | 11 | 30.56 |
| Polyhydramnios | 2 | 1.60 | 0 | 0.00 | 0 | 0 | 0 | 0.00 |
| Total | 125 | 100 | 29 | 100 | 10 | 100 | 36 | 100 |
| Among the groups | Normal | % in normal | Oligohydramnios | % in oligohyd. | Polyhydramnios | % in poly hyd. |
|---|---|---|---|---|---|---|
| Group I | 117 | 67.63 | 6 | 24.00 | 2 | 100.00 |
| Group IIA | 29 | 13.29 | 6 | 24.00 | 0 | 0.00 |
| Group IIB | 8 | 4.62 | 2 | 8.00 | 0 | 0.00 |
| Group III | 25 | 14.45 | 11 | 44.00 | 0 | 0.00 |
| Total | 173 | 100 | 25 | 100 | 2 | 100 |
P value 0.002
Of the 25 cases with oligohydramnios, 44 and 8 %, respectively, fell into Groups III and IIB which was significant. P value is .002 and hence highly significant.
MCA
| Description | Frequency | Percent |
|---|---|---|
| Normal | 154 | 77 |
| Abnormal | 46 | 23 |
Mode of delivery
| Among the groups | Vaginal dely. | % in vaginal dely. | CS for fetal distress | % in CS for fetal distress | CS for others | % in CS for others |
|---|---|---|---|---|---|---|
| Group I | 89 | 90.82 | 1 | 1.49 | 35 | 100.00 |
| Group IIA | 1 | 1.02 | 28 | 41.79 | 0 | 0.00 |
| Group IIB | 3 | 3.06 | 7 | 10.45 | 0 | 0.00 |
| Group III | 5 | 5.10 | 31 | 46.27 | 0 | 0.00 |
| Total | 98 | 100 | 67 | 100 | 35 | 100 |
P value <0.001
In Group IIA, in about 97 % cases cesarean section was done for fetal distress. In Group IIB where Doppler was abnormal but still NST was reactive, successful induction was done in 30 % of cases. In Group III when Doppler and NST were abnormal, 90 % of the cases ended up in cesarean section.
Birth weight
| Among the groups | >2.5 | % in >2.5 | 2–2.5 | % in 2–2.5 | <2.5 | % in <2.5 |
|---|---|---|---|---|---|---|
| Group I | 122 | 80.26 | 3 | 7.69 | 0 | 0.00 |
| Group IIA | 20 | 13.16 | 9 | 23.08 | 0 | 0.00 |
| Group IIB | 4 | 2.63 | 4 | 10.26 | 2 | 22.22 |
| Group III | 6 | 3.95 | 23 | 58.97 | 7 | 77.78 |
| Total | 152 | 100 | 39 | 100 | 9 | 100 |
P value <0.001
In Group III, 82 % cases had low birth weight. P value is <0.001 and hence highly significant.
NICU admission
| Among the groups | No | % in “no” | Yes | % in “yes” |
|---|---|---|---|---|
| Group I | 123 | 84.83 | 2 | 3.64 |
| Group IIA | 20 | 13.79 | 9 | 16.36 |
| Group IIB | 1 | 0.69 | 9 | 16.36 |
| Group III | 1 | 0.69 | 35 | 63.64 |
| Total | 145 | 100 | 55 | 100 |
P value <0.001
Among the 55 cases admitted, only 11 of them were from the Doppler normal group. In Group IIA where NST alone was non-reactive, only 9 cases were admitted among the 29. In Groups IIB and III, 90 and 98 % cases, respectively, were admitted. P value is <0.001 and hence highly significant.
There was a high incidence of cesarean section in this group. But perinatal outcome was not adverse.
Comparison of adverse outcome among different Doppler abnormalities showed a higher incidence of adverse perinatal outcome with the worsening of Doppler changes.
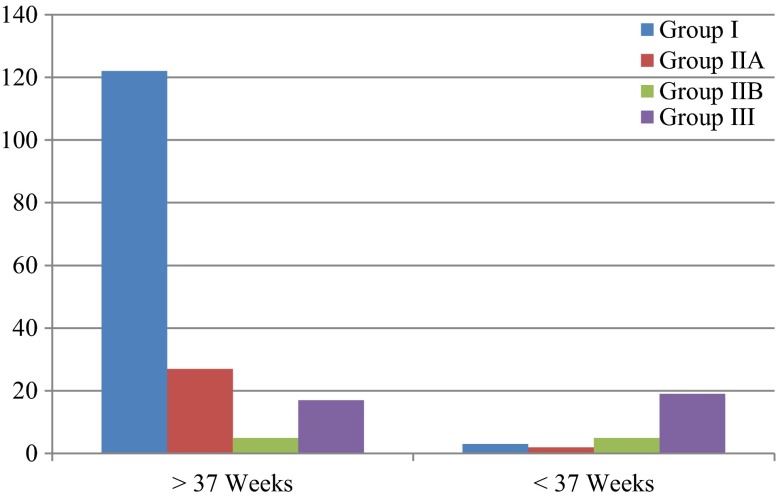
In Groups I and IIA, where Doppler was normal, 98 and 94 % cases, respectively, were terminated after 37 weeks. In Group IIB where Doppler was abnormal, but NST was still reactive, 50 % of the cases were delivered after 37 weeks. But in Group III where both were abnormal, nearly 53 % were terminated preterm. Overall, more than 80 % of preterm deliveries belonged to Doppler abnormal group among which 65 % belonged to Group III where NST was also non-reactive. P value is <0.001 and hence highly significant.
| Description | Frequency | Percent |
|---|---|---|
| >1 | 154 | 77 |
| 1 | 30 | 15 |
| <1 | 16 | 8 |
Discussion
This is a prospective study to analyze the efficacy of Doppler and the non-stress test in predicting perinatal outcome in high-risk pregnancies and find out the superior option.
When both Doppler and non-stress test were normal, most of the pregnancies were carried successfully till term. Likewise, when Doppler was normal but NST was non-reactive, there were only 7 % of deliveries before term. But on the other hand when Doppler and NST both were abnormal, nearly 53 % cases were terminated before term which indicates that adverse outcome is more common in this group. In the Group IIB where Doppler was abnormal, but still NST remained reactive, it was possible to carry 50 % pregnancies till term.
In these cases after trying measures to resolve the pattern, NST was repeated for a period of 90 min, but still there was no improvement and the patterns remained the same. Hence, these pregnancies were terminated.
CPR Versus APGAR, Birth Weight and NICU Admission
When CPR was greater than 1 (154 cases), most of these babies (93 %) had good APGAR scores. When CPR was less than or equal to 1, those babies had low APGAR scores.
When CPR was greater than 1 (152 cases), 93 % of the babies had normal birth weight. When it was less than or equal to 1, most of the babies had low birth weight (76 and 80 %, respectively).
Similarly, when CPR was less than or equal to 1, most of the babies required NICU admission.
Risk Factors
Among the total 15 cases of IUGR, 11 cases belonged to Group III, indicating a higher association with abnormal Doppler and abnormal NST.
Birth Weight
Doppler abnormality was associated with a higher incidence of low-birth-weight babies. In Group I, there were only 2 % cases with low birth weight. In Group IIA, where Doppler was normal about 70 % babies had normal weight. This indicates good correlation between normal Doppler findings and the growth of the fetus. Coming to Group IIB, out of the 10 cases, 6 cases had low-birth-weight babies. In these cases, NST was still reactive and these babies had better outcome though they were admitted in NICU when compared to the Group III cases where NST was also non-reactive. In this group (both abnormal), about 80 % babies had low birth weight and most of them were admitted in NICU with 36 % cases having a longer duration of stay. Considering NST as a test of well-being when it is reactive, surely it indicates a better prognosis.
APGAR
Among the 29 cases in Group IIA, where decision was taken based on non-reactive NST, only 9 cases had low APGAR which proves the false positivity of NST. In Group IIB, there were 7 cases with low APGAR. The reason behind this though the NST was reactive, could have been the fact that these fetuses were already compromised (had abnormal Doppler findings) and could have faced an acute insult during the process of labor. Anyway these babies had better outcome when compared to Group III babies of which 98 % had low APGAR.
Ventilator Support
When both Doppler and NST were abnormal, six of the babies needed ventilator’s support and three of them died. All three of the babies were born to mothers with severe preeclampsia. These patients had already developed irreversible changes in Doppler when they had their first visit to our hospital.
Conclusion
The main aim of this study was to use the time-tested methods of fetal surveillance, the Doppler velocimetry and non-stress test to precisely predict the perinatal outcome in high-risk pregnancies and find out which is superior.
Not all high-risk pregnancies with abnormal Doppler alone are indications for immediate termination. Those with abnormal Doppler with reactive NST could be successfully monitored and can be prolonged so that the little time period available can be utilized for steroid prophylaxis and planning the mode of delivery rather than an immediate cesarean section.
On the contrary, a non-reactive NST with a normal Doppler study need not necessarily mean an adverse outcome. Considering the high false-positive rate of NST, it is better to look beyond and take a wise decision to avoid unnecessary cesarean sections.
Also it is found that an abnormal Doppler with a non-reactive NST is definitely associated with an adverse perinatal outcome than when only one of the above was abnormal. The incidence of premature induction, cesarean section for fetal distress, low APGAR, NICU admissions and need for ventilation were more in cases where both these tests were abnormal. Hence by combining the two, and acting appropriately, the incidence of adverse perinatal outcome may be reduced.
In pregnancies with multiple high-risk conditions, it is recommended to initiate testing as early as 26–28 weeks of gestation.
Initiation of testing at 32–34 weeks of gestation is considered appropriate for pregnancies with increased risk of adverse outcome. A reassuring test should be repeated weekly or, depending on the test used and the presence of certain high-risk conditions, twice weekly until delivery.
Hence, no single test result should be considered for decision making in case of high-risk pregnancy because each test reflects different aspects of maternal and fetal pathophysiology. It is advisable to repeat the test and combine with other modes of fetal surveillance before decision making to improve the perinatal outcome and for better prediction of adverse events.
Funding
This study was funded by self.
Abbreviation
- NST
Non-stress test
- PSV
Peak systolic velocity
- MCA
Middle cerebral artery
- UA
Umbilical artery
- EDV
End diastolic velocity
- IUGR
Intrauterine growth retardation
- S/D ratio
Systolic-to-diastolic ratio
- APLA
Antiphospholipid antibody syndrome
- NICU
Neonatal intensive care unit
- GAD
Gestational age at delivery
- GDM
Gestational diabetes mellitus
- Mode of del
Mode of delivery
- Birth wt
Birth weight
- CPR
Cerebro-placental ratio
Dr. S. Vijaya MD DGO
working as Professor of Obstetric and Gynaecology at the Institute of Social Obstetrics and Government Kasturba Gandhi Hospital attached to Madras Medical College, Chennai. She has been a undergraduate and postgraduate examiner in Tamil Nadu, Kerala and Karnataka. She has more than 20 years of teaching experience and executive committee member of OGSSI. She has presented paper in national conference. Her field of interest is operative laparoscopy and social obstetrics.
Compliance with Ethical Standards
Conflict of interest
Authors have no conflicts of interest.
Ethical Approval
Humans were involved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Vijaya Subramanian is Professor in the Institute of Social Obstetrics, Kasturba Gandhi Hospital; Janani Venkat is Doctor in the Institute of Social Obstetrics, Kasturba Gandhi Hospital; Mohana Dhanapal is Doctor in the Institute of Social Obstetrics, Kasturba Gandhi Hospital.
References
- 1.Maulik D, Yarlagadda P, Downing G. Doppler velocimetry in obstetrics. Obstet Gynecol Clin N Am. 1990;17:163–186. [PubMed] [Google Scholar]
- 2.Maulik D. Basic principles of Doppler ultrasound as applied in obstetrics. Clin Obstet Gynecol. 1989;32:628–644. doi: 10.1097/00003081-198912000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Giles WB, Trudinger BJ, Baird PJ. Fetal umbilical artery flow velocity waveforms and placental resistance: pathological correlation. Br J Obstet Gynaecol. 1985;92:31–38. doi: 10.1111/j.1471-0528.1985.tb01045.x. [DOI] [PubMed] [Google Scholar]
- 4.Vyas S, Nicolaides KH, Bower S, et al. Middle cerebral artery flow velocity waveforms in fetal hypoxaemia. Br J Obstet Gynaecol. 1990;97:797–803. doi: 10.1111/j.1471-0528.1990.tb02573.x. [DOI] [PubMed] [Google Scholar]
- 5.Burns PN. Doppler flow estimations in the fetal and maternal circulations: principles, techniques and some limitations. In: Maulik D, McNellis D, editors. Doppler ultrasound measurement of maternal-fetal hemodynamics. Ithaca: Perinatology Press; 1987. pp. 43–78. [Google Scholar]
- 6.Krebs HB, Petres RE. Clinical application of a scoring system for evaluation of antepartum fetal heart rate monitoring. Am J Obstet Gynecol. 1978;130:765. doi: 10.1016/0002-9378(78)90006-6. [DOI] [PubMed] [Google Scholar]
- 7.Lyons ER, Bylsma-Howell M, Siamsi S, et al. A scoring system for nonstressed antepartum fetal heart rate monitoring. Am J Obstet Gynecol. 1979;133:242. doi: 10.1016/0002-9378(79)90673-2. [DOI] [PubMed] [Google Scholar]
- 8.Devoe LD, Yanowitch G, Azor H. The application of multiple-parameter scoring to antepartum fetal heart rate testing. J Reprod Med. 1981;26:250. [PubMed] [Google Scholar]
- 9.Pearson JF, Weayer JB. A six-point scoring system for antenatal cardiotocographs. Br J Obstet Gynaecol. 1978;85:321–327. doi: 10.1111/j.1471-0528.1978.tb14886.x. [DOI] [PubMed] [Google Scholar]
- 10.Nathanielsz PW, Bailey A, Poore ER, et al. The relationship between myometrial activity and sleep state and breathing in fetal sheep throughout the last third of gestation. Am J Obstet Gynecol. 1980;138:653. doi: 10.1016/0002-9378(80)90083-6. [DOI] [PubMed] [Google Scholar]
- 11.Powell OH, Melville A, MacKenna JL. Fetal heart rate acceleration in labor: excellent prognostic indicator. Am J Obstet Gynecol. 1979;134:36. doi: 10.1016/0002-9378(79)90792-0. [DOI] [PubMed] [Google Scholar]
- 12.Sharbaf FR, Amjadi N, Alavi A, et al. Normal and indeterminate pattern of fetal cardiotocography in admission test and pregnancy outcome. J Obstet Gynaecol Res. 2014;40(3):694–699. doi: 10.1111/jog.12226. [DOI] [PubMed] [Google Scholar]