Abstract
Background
Oligohydramnios is a known obstetric complication which is associated with operative interferences and perinatal morbidity and mortality. l-arginine is a precursor of nitric oxide and may play a role in local vasodilatation. Administration of l-arginine has been suggested to improve amniotic fluid index (AFI) in oligohydramnios.
Aims and Objectives
To study the effect of l-arginine in optimizing fetal outcome in cases of oligohydramnios.
Materials and Methods
A retrospective study was conducted at Dr L H Hiranandani hospital consisting of 100 antenatal patients diagnosed with oligohydramnios [AFI < 8 cm] remote from term. Patients were evaluated for all antenatal risk factors and were started on l-arginine sachets (3 g, 3 sachets a day). The treatment was continued till an adequate improvement in liquor was noted. However, patients were considered for delivery if the liquor remained <5. Further, mean increase in AFI, intervention delivery interval, and neonatal outcome were studied.
Results
The mean gestational age at the time of recruitment was 32.3 weeks. The mean AFI noted was 5.421 cm. These patients were delivered at 35 ± 1.1 weeks, and thus, pregnancy could be prolonged by 2.4 ± 1.1 weeks. The mean AFI at the end of therapeutic intervention was 8.753, and thus, an AFI increase of 3.332 cm could be obtained. There was no significant neonatal morbidity in these patients. Significant improvement in liquor volume was obtained in these patients after intervention with l-arginine sachets.
Conclusion
l-arginine supplementation is promising in improving volume of amniotic fluid in cases of oligohydramnios and prolonging pregnancy by a mean of 2.4 weeks, allowing fetal lung maturation thus benefiting the neonatal outcome.
Keywords: l-arginine, Oligohydramnios, Amniotic fluid index
Introduction
Amniotic fluid (AF) surrounds the fetus after first few weeks of gestation which serves to protect the fetus and umbilical cord from compression. It is an important aspect for adequate fetal growth and good fetal outcome. Oligohydramnios is a decreased amount of amniotic fluid affecting 3–5 % of pregnancies. Decreased amniotic fluid is associated with placental insufficiency, impaired lung development in fetus, and fetal growth restriction (FGR). Long-term complications of oligohydramnios are cord compression and variation in fetal heart rate during labor and increased chance of operative deliveries. Surviving infants may have anatomic and functional abnormalities, such as skeletal deformities, contractures, and pulmonary hypoplasia.
Normally amniotic fluid increases about a liter between 32 and 34 weeks of gestation, but afterwards it decreases till term to around 400 ml. The amount of AF is most commonly evaluated by ultrasound using amniotic fluid index (AFI) or single largest pocket (SLP). An AFI of 8 cm and above is considered normal, between 5 cm and 8 cm is low normal, and <5 cm is oligohydramnios.
In chronic placental insufficiency, the fetus tries to acclimatize by redirecting blood flow to vital organs such as brain and heart at the cost of renal circulation. There is significant reduction in urine output, which results in reduction in available intrauterine space for adequate fetal growth. Subjected to pressure from all sides, the fetus assumes a peculiar appearance and musculoskeletal deformities such as club foot, talipes, and wry neck. Lack of movement of amniotic fluid within the tracheobronchial tree results in pulmonary hypoplasia.
Different medical interventional methods have been tried to treat oligohydramnios. This study was done to find out the effect of l-arginine on AFI, the mode of delivery, and the fetal outcome. l-arginine, a semi-essential amino acid and the sole endogenous precursor of nitric oxide (NO), is involved in the regulation of blood flow in vascular beds [1]. It is an important regulator of placental perfusion [2]. It causes vasodilatation and shows aggregative effect on platelets. This mechanism increases the volume and viscosity of blood in the fetomaternal circulation [3].
l-arginine promotes the intrauterine growth of the fetus by increasing bioavailability of endothelial NO production and improving the umbilical artery flow in pregnancy induced hypertension and fetal growth restriction.
Materials and Methods
It is a retrospective study of 100 patients diagnosed with oligohydramnios by ultrasound (AFI less than 5th percentile for gestational age, AFI <8 cm) carried out at Dr. L H Hiranandani hospital, Powai, Mumbai.
Inclusion Criteria
The inclusion criteria were: 24–36 weeks gestational age in singleton pregnancies with or without complications and initial AFI between 4 and 8 in presence of intact membranes.
Exclusion Criteria
Exclusion criteria were smoking and chronic illnesses like hypertension, congenital heart disease, renal disease, diabetes mellitus, fetal malformations, severe preeclampsia, severe FGR, preterm premature rupture of membranes (PPROM).
The amniotic fluid volume was calculated with the four-quadrant technique. The AFI was calculated by summing up the maximum vertical fluid pockets (measured in cm) in each of the four quadrants.
Patients were administered l-arginine 3 gm per sachet in oral form. Serial ultrasound monitoring at regular intervals was performed, and patients were followed up till delivery. Effect of l-arginine on oligohydramnios and intrauterine growth was analyzed.
Close monitoring was carried out for any hemodynamic alterations. Patient compliance was good, and no detrimental side effects were noted due to l-arginine intervention. The treatment was continued till the liquor improved significantly. Additional risk factors were managed as per usual standard protocols. Serial non-stress test (NST) and biophysical profile (BPP) were mandatory as a monitoring protocol for all patients. However, patients were considered for delivery if the liquor remained <5 irrespective of the gestational age. These patients were given two doses of injection betamethasone 12 mg intramuscularly 24 h apart to accelerate fetal lung maturity.
Student’s t test was used to find the statistical significance of the observations. The differences were considered significant if the P value was <0.05 and highly significant if it was <0.01.
Results
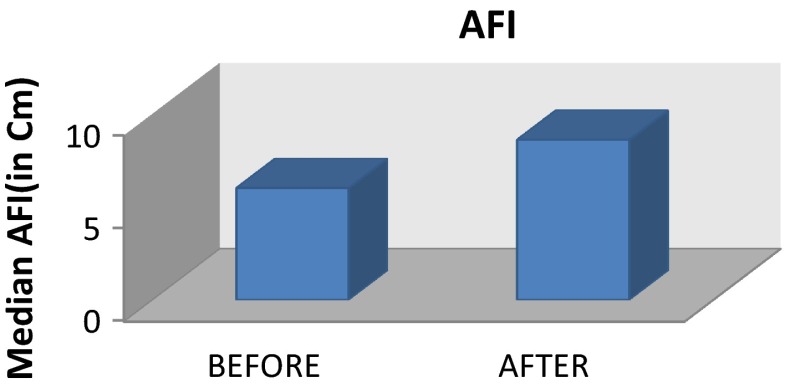
The average neonatal birth weight after giving l-arginine was 2.76 kg. Average gestational age at delivery was 36 weeks. It was observed that l-arginine supplements increases the amniotic fluid volume, accelerates the fetal weight, and helps to prolong the duration of pregnancy. Among the 100 patients, 19 patients had preterm delivery. Most of the patients were primigravida. They were detected to have low liquor during their third trimester between 29 and 35 weeks of gestation. Total number of patients, parity, mean gestational age, and mean AFI at intervention are shown in Table 1. Antenatal risk factors are described in Table 2. The overall improvement in AFI is shown in Graph 1.
Table 1.
Parity, mean gestational age and AFI
| Total no. of patients | 100 |
|---|---|
| Parity | Primigravida—74 (74 %) Multigravida—26 (26 %) |
| Mean gestational age | 32.3 weeks (range 29–35 weeks) |
| Mean AFI before intervention | 5.421 |
Table 2.
Antenatal risk factors
| Complications | Number (100) = percentage |
|---|---|
| Mild FGR | 34 |
| Threatened preterm | 18 |
| Hypertension in pregnancy | 22 |
| Anemia | 4 |
| Previous LSCS | 8 |
| Hypothyroidism | 4 |
| Asthma | 2 |
| No complications | 8 |
Graph 1.
Improvement in AFI with l-arginine
The overall increase in liquor was found to be 2.6 cm [pretreatment AFI 6 (SD 1.205), post-treatment AFI 8.6 (SD 1.042); P < 0.05]. The increase was statistically significant in all the classes.
The end point of the intervention was to achieve reasonable gestational age of 36–37 weeks in our study. The average gestational age at the time of delivery was 35 ± 1.1 weeks, and thus, 2.4 weeks of prolongation period was noted with the therapy. Overall growth of the fetus and improvement was noted due to increased gestational period. There was no significant neonatal morbidity in the babies born.
Rate of cesarean delivery noted is 72 %. Main indication is fetal distress (46 %) as fetuses with less amount of liquor are likely to experience cord compression and variable deceleration. Table 3 shows the overall obstetric outcome of these patients. Neonatal outcome in these 100 singleton pregnancies is noted in Table 4.
Table 3.
Mode of delivery
| Mode of delivery | Frequency |
|---|---|
| Normal delivery | 28 |
| Cesarean section | 72 |
Table 4.
Weight of baby at birth
| Weight of baby at birth | Frequency |
|---|---|
| Below 2500 gms | 20 |
| 2501–2900 gms | 32 |
| 2901 gms and above | 48 |
There were no perinatal deaths. There were nine neonates who had 5-min APGAR score between 4 and 6. Four of them recovered in neonatal intensive care unit (NICU) with continuous positive airway pressure (CPAP) ventilation. Two babies developed respiratory distress and required invasive mechanical ventilation; however, the babies recovered completely. There was no incidence of necrotizing enterocolitis, hypoxic ischemic encephalopathy, or sepsis in any of the babies. Neonatal outcomes are given in Table 5.
Table 5.
Neonatal outcomes
| Birth weight | 2.3–2.9 kg |
|---|---|
| Small for gestational age | 34 (34 %) |
| APGAR score | |
| < 4 | Nil |
| 4–6 | 6 |
| > 7 | 94 |
| Still birth/neonatal death | Nil |
| NICU admissions | 19 (19 %) |
Discussion
Amniotic fluid has major role in development of fetal lungs, and early severe oligohydramnios leads to pulmonary hypoplasia. Low amniotic fluid is defined as <200, <500 ml [4], below 3rd percentile, which is equal to AFI 4 for gestational age or a single largest pocket of 2 cm [5]. Nabhan and Abdelmoula, in their Cochrane review which included five randomized controlled trials comprising 3226 women, found that for AFI <5 cm, there were more induction rates, higher induction failures, more cesarean deliveries for fetal distress without much difference in NICU admission rate, and improved perinatal outcome [6]. They have opined that lower cutoffs such as below 3rd percentile which is equal to AFI 4 for gestational age or a single largest pocket of 2 cm used for oligohydramnios may be of more end benefits. So we have used the range of 4–8 cm for our study.
l-arginine is a semi-essential amino acid acting as a substrate for synthesis of NO [7]. NO has a diverse role in obstetrics as it plays a vital role in labor, cervical ripening, preeclampsia, and intrauterine growth restriction. Nitric oxide (NO) is an important regulator of placental perfusion and plays an important role in placental vascular endothelial function. NO is synthesized from the physiologic precursor l-arginine by stereospecific enzyme NO synthase in what is called the l-arginine/NO pathway, and l-arginine is the only substrate for the NO [8]. NO diffuses into the underlying vascular smooth muscle cells and mediates vasodilatation and platelet stabilization by a cyclic GMP-dependant process [9].
l-arginine promotes intrauterine growth of the fetus by increasing bioavailability of endothelial nitric oxide (NO) production and improving the umbilical artery flow in pregnant women with pregnancy-induced hypertension and fetal growth restriction.
l-Arginine is also reported to improve growth hormone releasing hormone secretion and as a consequence increase in plasmatic growth hormone influencing somatic growth. It is also suggested that it may play a significant role in fetal growth, by stimulating insulin secretion, and as a precursor for both polyamine synthesis and NO production [10]. l-arginine treatment accelerates fetal weight gain and improves biophysical profile [11].
Gene expression and protein tissue content of arginase II (enzyme that degrades arginine to ornithine) were found to be higher in preeclamptic villi than in normotensive pregnancy [12]. Arginase II over-expression is seen in lower l-arginine concentration which causes increase in peroxynitrite (isoform of nitric oxide synthase). Peroxynitrite is a cytotoxic anion that inhibits mitochondrial electron transport, oxidizes proteins, initiates lipid peroxidation, and nitrates aromatic amino acid. Peroxynitrite by causing vascular damage contributes to the increased placental vascular resistance [13].
The combination of a deficiency of NO and increase in peroxynitrite is associated with placental dysfunction, increased thromboxanes and endothelin 1, and decrease in prostacyclins. Therefore, studies recommend the supplementation of l-arginine and antioxidants in pregnancy to maintain the levels of NO so as to facilitate the required vasodilatation and have a beneficial role in the fetal growth.
Delivery of patients with gestational age <34 weeks with oligohydramnios is a challenging situation. To avoid serious complications related to mother and fetus, therapeutic intervention is desirable to prolong the pregnancy, so that the risk of prematurity is minimized. Oral l-arginine can be used as cheap and feasible method.
Anita Soni
has presented many papers and publications to her credit. She has won many awards in various state and national conferences with a recent first prize for best paper at the National Conference (AICOG 2013). Her special interests are high-risk pregnancy, and she is in charge of first of its kind high-risk pregnancy unit at Dr L H Hiranandani Hospital. She has been an invited speaker at national- and state-level conferences and has represented the hospital at the FIGO World Congress at Vancouver.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they do not have any conflict of interest.
Ethical Approval
This study is approved by the institutional scientific and ethical committee. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Anita Soni is consultant Obstetrician and Gynecologist in the Department of Obstetrics and Gynaecology at Dr L H Hiranandani Hospital, at Seth G. S. Medical College and K. E. M. Hospital; Seeru Garg is junior consultant Obstetrician and Gynecologist in the Department of Obstetrics and Gynaecology at Dr L H Hiranandani Hospital; Khushboo Patel is DGO resident in the Department of Obstetrics and Gynaecology at Dr L H Hiranandani Hospital; Zarna Patel is DNB resident in the Department of Obstetrics and Gynaecology at Dr L H Hiranandani Hospital.
References
- 1.Zhang N, Xiong AH, Xiao X, et al. Effect and mechanism of l-arginine therapy for fetal growth retardation due to pregnancy-induced hypertension. Nan Fang Yi Ke Da Xue Xue Bao. 2007;27(2):198–200. [PubMed] [Google Scholar]
- 2.RCOG Nitric oxide, the endothelium, pregnancy and preeclampsia. Br J Obstet Gynaecol. 1996;103:4–15. doi: 10.1111/j.1471-0528.1996.tb09508.x. [DOI] [PubMed] [Google Scholar]
- 3.Appleton J. Arginine: clinical potential of a semi essential amino acid. Altern Med Rev. 2002;7:512–522. [PubMed] [Google Scholar]
- 4.Magann EF, Nolan TE, Hess LW, et al. Measurement of amniotic fluid volume: accuracy of ultrasonography techniques. Am J Obstet Gynecol. 1992;167:1533–1537. doi: 10.1016/0002-9378(92)91734-R. [DOI] [PubMed] [Google Scholar]
- 5.Magann EF, Sanderson M, Martin JN, et al. The amniotic fluid index, single deepest pocket, and two-diameter pocket in normal human pregnancy. Am J Obstet Gynecol. 2000;182:1581–1588. doi: 10.1067/mob.2000.107325. [DOI] [PubMed] [Google Scholar]
- 6.Nabhan AF, Abdelmoula YA. Amniotic fluid index versus single deepest vertical pocket as a screening test for preventing adverse pregnancy outcome. Cochrane Database Syst Rev. 2008;3:CD006593. doi: 10.1002/14651858.CD006593.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mittal R, Satwant K, Mittal N, et al. l-arginine supplementation in intrauterine growth retardation. Int J Pharm Chem Sci. 2013;2(3):1569–72. (ISSN: 2277–5005).
- 8.Viviana DP, Giuseppe C, Fabio F. Clinical use of nitric oxide donors and l-arginine in obstetric. J Mater Fetal Neonatal Med. 2007;20(8):569–579. doi: 10.1080/14767050701419458. [DOI] [PubMed] [Google Scholar]
- 9.Lampariello C, De Blasio A, Merenda A, et al. Use of l-arginine in intrauterine growth retardation (IUGR): authors’ experience. Minerva Ginecol. 1997;49:577–581. [PubMed] [Google Scholar]
- 10.Staff AC, Berge L, Haugen G, et al. Dietary supplementation with l-arginine or placebo in women with pre-eclampsia. Acta Obstet Gynecol Scand. 2004;83:103–107. [PubMed] [Google Scholar]
- 11.Thureen PJ, Baron KA, Fennessey PV, et al. Ovine placental and fetal arginine metabolism at normal and increased maternal plasma arginine concentrations. Pediatr Res. 2002;51:464–471. doi: 10.1203/00006450-200204000-00011. [DOI] [PubMed] [Google Scholar]
- 12.Xiao XM, Li LP. L-Arginine treatment for asymmetric fetal growth restriction. Int J Gynecol Obstet. 2005;88:15–18. doi: 10.1016/j.ijgo.2004.09.017. [DOI] [PubMed] [Google Scholar]
- 13.Myatt L, Rosenfield RB, Eis ALW, et al. Nitrotyrosine residues in placenta evidence of peroxynitrite formation and action. Hypertension. 1996;28:488–493. doi: 10.1161/01.HYP.28.3.488. [DOI] [PubMed] [Google Scholar]