Abstract
Purpose of the Study
To study the role of endometrial and subendometrial blood flow measured by 3D power Doppler as predictors of pregnancy in frozen embryo transfer (FET) cycles.
Methods
A hospital-based prospective study of two hundred and twenty-one (221) women undergoing FET cycles with a triple-line endometrium ≥7 mm on day 14 endometrial and subendometrial blood flow was assessed using 3D power Doppler, and various indices endometrial volume, subendometrial volume and their vascularisation index (VI), flow index (FI) and vascularisation flow index (VFI) were obtained and compared between the pregnant and the non-pregnant group. Primary outcome was clinical pregnancy.
Results
Out of 221 women, 97(43.89 %) became pregnant, while 124 (56.10 %) failed to become pregnant. The endometrial volume was comparable between the two groups. Endometrial VI, FI and VFI were significantly higher in the pregnant as compared to the non-pregnant group. There was a significant difference in subendometrial VI and VFI between the two groups, but FI was similar.
Conclusions
Endometrial and subendometrial vascularity by 3D power Doppler can be a useful parameter in predicting pregnancy in FET cycles.
Keywords: Endometrial subendometrial vascularity, 3D power Doppler, Clinical pregnancy, FET cycles
Introduction
A receptive endometrium is essential for successful implantation. Endometrial thickness and pattern are useful prognostic factors for successful pregnancy. Uterine artery Doppler has been used as a marker to predict chances of pregnancy. An elevated uterine artery PI has been correlated with low implantation and pregnancy rates [1]. However, uterine artery Doppler is not so specific for predicting pregnancy [2]. Endometrial blood flow reflects receptivity of the endometrium since implantation takes place in the endometrium [3]. The advent of transvaginal ultrasound with 2D and 3D power Doppler has provided a perfect non invasive tool to assess endometrial receptivity. Measurement of endometrial and subendometrial blood flow using 3 D power Doppler in IVF cycles and their role in predicting IVF cycle outcome has attracted a lot of attention across the world in recent years. The results of various studies assessing the role of endometrial and subendometrial blood flow in IVF outcome are conflicting.
The aim of this study was to evaluate the role of endometrial and subendometrial blood flows measured by 3D power Doppler ultrasound as the predictive factors for pregnancy during FET cycles. Endometrial and subendometrial blood flows between pregnant and non-pregnant patients were compared.
Materials and Methods
It was a prospective non-randomized observational study conducted in the Dept of Obstetrics and Gynecology at IKDRC-ITS from June 2014 to December 2014. A total of 221 women undergoing frozen embryo transfer (FET) cycles, irrespective of their previous embryo transfer outcomes, were included in the study. Informed consent was obtained from all the women participating in the study.
Inclusion criteria were infertile patients between 20 to 40 years of age, FET cycles, normal uterine cavity as assessed by prior hysteroscopy. Embryo freezing was done by vitrification technique, and at least two or three good-quality grade A embryos were available for transfer, transfer of day 3, 8-celled cleavage-stage embryos. Patients with uterine pathology like fibroid, polyp, etc., hydrosalpinx and patients with blastocyst transfer were excluded from the study.
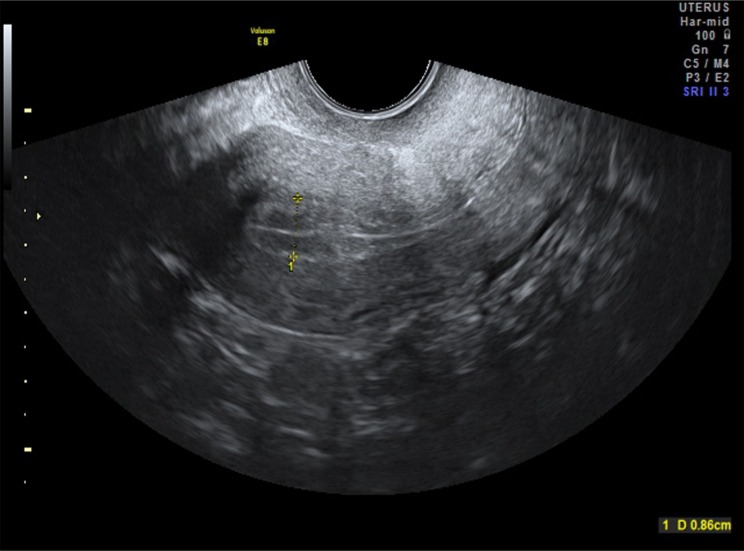
In frozen cycles, a baseline transvaginal ultrasound was done on cycle day 2 to confirm endometrial thickness <5 mm and to rule out any ovarian cyst. Endometrial preparation was started with estradiol valerate, and endometrial assessment was done on day 14. Endometrial thickness was measured on a longitudinal section of uterus at the point of maximum thickness, and endometrial pattern was noted (as shown in Fig. 1). If triple-line endometrium ≥7 mm was noted, endometrial and subendometrial blood flow was assessed using 3D power Doppler. All the assessments were done using Voluson E 8, GE Wipro medical system USG machine and done by a single person to avoid inter observer variations. The power Doppler characteristics were a Color gain-10, pulse repetition frequency of 600 Hz and wall motion filter of 50 Hz. The ultrasound machine was switched to the 3D mode with power Doppler. The setting for this study was: frequency mid; dynamic set 2; power Doppler map 5. The sector of interest covering the endometrial cavity in a longitudinal plane of the uterus was adjusted, and the sweep angle was set to 90° to ensure that a complete uterine volume including the entire subendometrium was obtained. 3D volume was acquired keeping the patient and the 3D transvaginal probe still during the volume acquisition.
Fig. 1.
2D ultrasound (B mode) showing triple-line pattern of endometrium
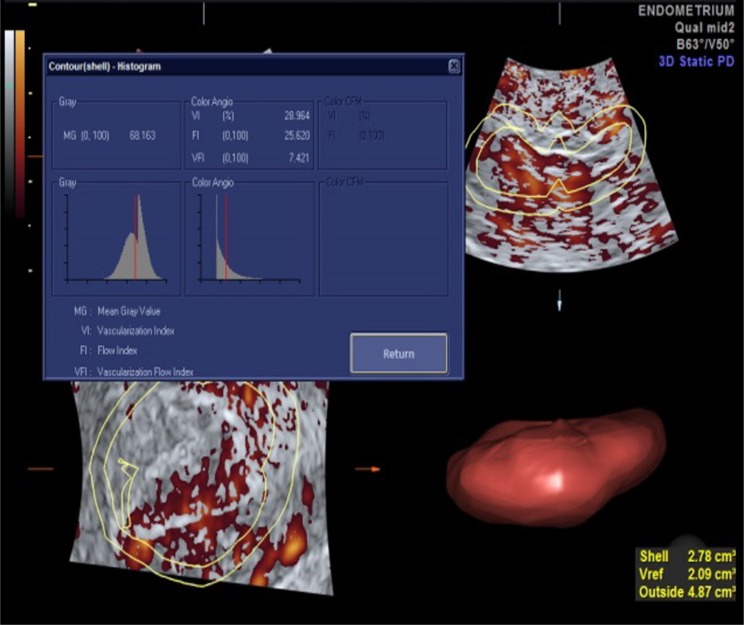
Endometrial volume and various indices VI, FI and VFI were measured using the virtual organ computer-aided analysis (VOCAL) imaging program for the 3D power Doppler histogram analysis. Six contour planes were analyzed with a 30° rotation step for the endometrium to cover 180°. Volume histogram was obtained to measure endometrial volume, VI, FI and VFI (as shown in Fig. 2). Vascularization index (VI) represents the presence of blood vessels (vascularity) in the endometrium. It is measured as the ratio of the number of color voxels to the total number of voxels and is expressed as a percentage (%) of the endometrial volume. Flow index (FI) is the mean power Doppler signal intensity inside the endometrium and represents the average intensity of flow. Vascularization flow index (VFI) is a combination of vascularity and flow intensity. Following the assessment of the endometrial vascularity, shell-imaging was used to measure subendometrial blood flow within 2-mm shell of endometrial myometrial contour. Volume, VI, FI and VFI of the subendometrial region were obtained accordingly (as shown in Fig. 3).
Fig. 2.
3D power Doppler with volume histogram of endometrium
Fig. 3.
3D power Doppler with volume histogram of subendometrium
Progesterone supplementation was started on day 14, and cleavage stage embryo transfer was done after 3 days of progesterone supplementation (i.e., day 17 of patient’s menstrual cycle). A serum β hCG > 25 mIU/ml at 14 days after embryo transfer was considered as positive for pregnancy.
The primary outcome of the study was clinical pregnancy defined as the presence of one or more intrauterine gestational sac at 6 weeks.
Statistical Analysis
Statistical analysis was done using data analysis software system SPSS V20. Continuous data were expressed as mean ± SD. P value <0.05 was considered statistically significant. Continuous data follow normal distribution and non-normal distribution both. Independent t test and Mann–Whitney test have been used to calculate statistically significant value, i.e., P value. NS represents non-significant difference between two groups.
Results
Mean age, BMI and baseline hormonal characteristics of the pregnant and the non-pregnant group are shown in Table 1. Ninety-seven out of 221 (43.89 %) patients became pregnant, while 124 (56.10 %) did not conceive. Endometrial thickness and various indices were compared between the two groups. The mean endometrial thickness on day 14 in the pregnant group was more (7.94 ± 1.29 mm) as compared to the non-pregnant group (7.84 ± 1.16 mm) although the difference was not statistically significant. There was no significant difference in the mean endometrial volume between the two groups (2.35 ± 0.87 in pregnant v/s 3.59 ± 11.22 in non-pregnant). VI, FI and VFI were significantly higher in the pregnant (3.18 ± 4.10, 23.21 ± 15.72, 1.22 ± 2.94) as compared to the non-pregnant group (3.04 ± 6.07, 21.24 ± 4.76, 0.78 ± 1.65) as shown in Table 2. When subendometrial blood flow was compared between the two groups, it was seen that the volume of the shell was slightly higher in the non-pregnant group, but the difference was not statistically significant (3.28 ± 4.07 v/s 3.34 ± 4.79). Among the indices, VI (5.51 ± 7.49 v/s 4.66 ± 9.79) and VFI (1.53 ± 2.19 v/s 1.44 ± 3.13) were found to be significantly higher in the pregnant group, while there was no difference in FI (24.80 ± 3.64 v/s 24.04 ± 5.06) between the two groups (Table 3). Pregnancy outcome does not depend upon the cause of IVF or the protocol used as shown in Tables 4 and 5.
Table 1.
Baseline characteristics and hormonal profile
| Variables | Pregnant (N = 97) | Non-pregnant (N = 124) | P value |
|---|---|---|---|
| Age (years) | 30.04 ± 4.85 | 30.70 ± 5.14 | 0.36 (NS) |
| BMI (Kg/m2) | 22.05 ± 2.62 | 21.91 ± 1.97 | 0.90 (NS) |
| FSH (IU/ml) | 7.78 ± 7.21 | 8.15 ± 4.74 | 0.44 (NS) |
| LH (IU/ml) | 5.05 ± 3.33 | 5.44 ± 2.86 | 0.14 (NS) |
| TSH (µIU/ml) | 1.89 ± 0.95 | 2.06 ± 1.23 | 0.41 (NS) |
| Prolactin (ng/ml) | 13.30 ± 5.78 | 15.83 ± 16.25 | 0.15 (NS) |
| Estradiol (pg/ml) | 44.66 ± 21.33 | 49.03 ± 23.86 | 0.26 (NS) |
P value <0.05 considered to be statistically significant difference
Here, NS represents non-significant difference between these groups
* represents significant difference between these groups
Table 2.
Relationship of endometrial vascularity and pregnancy outcome
| Pregnant (N = 97) | Non-pregnant (N = 124) | P value | |
|---|---|---|---|
| Endometrial thickness (mm) | 7.94 ± 1.29 | 7.84 ± 1.16 | 0.49 (NS) |
| Volume (cm3) | 2.35 ± 0.87 | 3.59 ± 11.22 | 0.68 (NS) |
| VFI (0-100) | 1.22 ± 2.94 | 0.78 ± 1.65 | <0.01* |
| FI (0-100) | 23.21 ± 15.72 | 21.24 ± 4.76 | <0.01* |
| VI (%) | 3.18 ± 4.10 | 3.04 ± 6.07 | <0.01* |
P value <0.05 considered to be statistically significant difference
Here, NS represents non-significant difference between these groups
* represents significant difference between these groups
Table 3.
Relationship of subendometrial vascularity and pregnancy outcome
| Subendometrial shell (2 mm) | Pregnant (N = 97) | Non-pregnant (N = 124) | P value |
|---|---|---|---|
| Volume (cm3) | 3.28 ± 4.07 | 3.34 ± 4.79 | 0.62 (NS) |
| VFI (0–100) | 1.53 ± 2.19 | 1.44 ± 3.13 | <0.01* |
| FI (0–100) | 24.80 ± 3.64 | 24.04 ± 5.06 | 0.22 (NS) |
| VI (%) | 5.51 ± 7.49 | 4.66 ± 9.79 | <0.01* |
P value <0.05 considered to be statistically significant difference
Here, NS represents non-significant difference between these groups
* represents significant difference between these groups
Table 4.
Relationship of protocol used and pregnancy outcome
| Protocol | Positive (N = 97) | Negative (N = 124) | P value |
|---|---|---|---|
| Long | 64 (65.98 %) | 81 (65.32 %) | 0.92 (NS) |
| Short | 13 (13.40 %) | 20 (16.13 %) | 0.57 (NS) |
| Antagonist | 18 (18.56 %) | 22 (17.74 %) | 0.89 (NS) |
P value <0.05 considered to be statistically significant difference
Here, NS represents non-significant difference between these groups
* represents significant difference between these groups
Table 5.
Relationship of indication for IVF and pregnancy outcome
| Indications for IVF | Positive (N = 97) | Negative (N = 124) | P value |
|---|---|---|---|
| Unexplained | 27 (27.84 %) | 29 (23.39 %) | 0.45 (NS) |
| Tubal | 28 (28.87 %) | 29 (23.39 %) | 0.36 (NS) |
| Male | 25 (25.78 %) | 41 (93.06 %) | 0.24 (NS) |
| Ovarian | 10 (10.31 %) | 20 (16.13 %) | 0.21 (NS) |
| Male + Ovarian | 3 (3.09 %) | 1 (0.81 %) | 0.32 (NS) |
| Hypogonadotropic hypogonadism | 1 (1.03 %) | 0 (0 %) | 0.44 (NS) |
| Serodiscordant couple | 0 (0 %) | 1 (0.81 %) | 1.00 (NS) |
P value <0.05 considered to be statistically significant difference
Here, NS represents Non-significant difference between these groups
* represents significant difference between these groups
Discussion
The role of receptive endometrium in implantation has been well established. Successful implantation requires a close cross talk between a good-quality embryo and a receptive endometrium. A good blood supply is essential for endometrial receptivity. Various studies have focused on measurement of endometrial and subendometrial blood flow using 3D power Doppler and their role in predicting cycle outcome, but the results are conflicting. 3D power Doppler assessment of endometrial–subendometrial blood flow is an effective way of improving IVF outcomes.
The endometrial volume must be at least 2.0–2.5 ml for achieving a pregnancy [4]. In our study, endometrial volume of all the patients was >2 cm3.
In a study by Merce et al. [1], it was seen that endometrial volume measured on the day of hCG was significantly higher in the pregnant group as compared to the non-pregnant group. However, in our study endometrial thickness and endometrial volume were comparable between the two groups and were not predictive of pregnancy. These results are similar to a study by Schilder et al. [5] who showed that the endometrial volume measured by 3D ultrasound is not predictive of pregnancy.
Ng et al. [6] in his study showed that in IVF treatment, endometrial volume measured by three-dimensional (3D) ultrasound was comparable for pregnant and non-pregnant women.
Some studies have shown a positive correlation of subendometrial and endometrial blood flows with pregnancy rates [7, 8]. Similarly in our study, endometrial and subendometrial vascularity was significantly higher in the pregnant group as compared to the non-pregnant group.
Different studies have used different thickness of subendometrial shell to assess subendometrial vascularity. We studied subendometrial blood flow in 2-mm shell surrounding the original myometrial endometrial contour. Schild et al. and Wu et al. used 5-mm subendometrial region, while Ng et al. considered 1-mm subendometrial shell in their studies [5, 6, 9].
Wu HM et al. found that subendometrial VFI may be useful in predicting implantation and pregnancy rates in IVF [9]. In our study also, subendometrial VI and VFI were found to be significantly higher in the pregnant group although there was no significant difference in subendometrial FI between the two groups. These results are in contrast to a study of 89 patients by Kupesic et al. [10] where he found that subendometrial FI on the day of embryo transfer was significantly higher in pregnant as compared to non-pregnant patients, whereas subendometrial VI and VFI were similar between the two groups.
Ernest in his study of 293 patients undergoing the first IVF cycle showed that endometrial and subendometrial blood flow on the days of HCG and embryo transfer were not predictive of pregnancy [11].
Zackova et al. concluded that assessment of endometrial characteristics using 3D power Doppler is not helpful in predicting the response in FET cycles [12]. Similarly, Check et al. [13] did not find any relationship between endometrial and subendometrial blood flow and pregnancy rates in FET cycles.
In a study of FET and IVF–ET groups by Tekay et al. [14], it was seen that the Doppler velocimetry measurements between conception and non-conception cycles were not significantly different. They concluded that impaired uterine blood flow negatively affects implantation, while an adequate uterine blood may not necessarily result in pregnancy.
However, Ng et al. [15] found that endometrial and subendometrial blood flow was significantly higher in pregnant females with live birth than those with a miscarriage.
The results of these studies are conflicting, and different studies have measured blood flows on different days, i.e., day of hCG, day of oocyte retrieval, day of embryo transfer, when endometrium >7 mm in FET cycles. There is still no consensus as to when these measurements should be done. The limitation of our study was a small sample size and a large age group. Further large studies are required to reach to definite conclusion.
Conclusion
Endometrial and subendometrial vascularity as measured by 3D power Doppler is a useful predictor for pregnancy in FET cycles. However, further large randomized trials are required to establish the definitive role of endometrial–subendometrial vascularity in determining cycle outcome.
Acknowledgments
No grants or any specific assistance has been taken from any outside source for preparing the manuscript.
Dr. Vineet Mishra
is the head of the Department of Obst. and Gynaec IKDRC, Ahmedabad. He has been a very active member of FOGSI and has been elected as VP FOGSI West Zone 2016. Over the years, Dr. Vineet Mishra’s contribution in academics has taken him all across the globe. He has been actively involved in fellowship programmes in Obst. and Gynaec since 2005. He is a great teacher and mentor for the young aspiring gynecologist throughout the country. He is a strong believer of revolution through innovation and is an eminent gynecologist. He has specialized in urogynecology, minimally invasive surgeries, assisted reproductive techniques, high-risk pregnancy care and runs a state-of-the-art Genetic Lab and fetal medicine unit. Dr. Vineet Mishra has been the organizing chairperson of urogynecology committee from year 2011 to 2013. He has a strong vision and has organized many prestigious CME programmes and has shared his knowledge as a guest lecturer across the country.
Compliance with Ethical Standards
Conflicts of interest
None Declared.
Ethical statement
Informed written consent taken from every patient to enroll them in this study.
Footnotes
Dr. Vineet V Mishra MD, Phd Professor and Head of Department, Obstetrics and Gynecology, IKDRC-ITS, Ahmedabad; Dr. Ritu Agarwal M.S. Senior Resident, Dept. Of Obstetrics and Gynecology, IKDRC-ITS, Ahmedabad; Dr. Urmila Sharma M.S. Clinical Fellow, Dept. Of Obstetrics and Gynecology, IKDRC-ITS, Ahmedabad; Dr. Rohina Aggarwal MS Associate Professor, Dept. Of Obstetrics and Gynecology IKDRC Ahmedabad; Dr Sumesh Choudhary MD Assistant professor, Dept. Of Obstetrics and Gynecology IKDRC Ahmedabad; Dr Pradeep Bandwal Senior Resident, Dept. of Obstetrics and Gynecology IKDRC Ahmedabad.
References
- 1.Mercé LT, Barco MJ, Bau S, et al. Are endometrial parameters by three-dimensional ultrasound and power Doppler angiography related to in vitro fertilization/embryo transfer outcome? Fertil Steril. 2008;89:111–117. doi: 10.1016/j.fertnstert.2007.02.029. [DOI] [PubMed] [Google Scholar]
- 2.Friedler S, Schenker JG, Herman A, et al. The role of ultrasonography in the evaluation of endometrial receptivity following assisted reproductive treatments: a critical review. Hum Reprod Update. 1996;2:323–335. doi: 10.1093/humupd/2.4.323. [DOI] [PubMed] [Google Scholar]
- 3.Merce LT. Ultrasound markers of implantation. Ultrasound Rev Obstet Gynecol. 2002;2:110–123. doi: 10.1080/14722240208500468. [DOI] [Google Scholar]
- 4.Zollner U, Zollner KP, Specketer MT, et al. Endometrial volume as assessed by three-dimensional ultrasound is a predictor of pregnancy outcome after in vitro fertilization and embryo transfer. Fertil Steril. 2003;80:1515–1517. doi: 10.1016/j.fertnstert.2003.08.004. [DOI] [PubMed] [Google Scholar]
- 5.Schild RL, Knoblock C, Dorn C, Fimmers R, et al. Endometrial receptivity in an in vitro fertilization program as assessed by spiral artery blood flow, endometrial thickness, endometrial volume, and uterine artery blood flow. Fertil Steril. 2001;75:361–366. doi: 10.1016/S0015-0282(00)01695-2. [DOI] [PubMed] [Google Scholar]
- 6.Ng EHY, Chan CCW, Tang OS, et al. The role of endometrial and subendometrial vascularity measured by three-dimensional power Doppler ultrasound in the prediction of pregnancy during frozen thawed embryo transfer cycles. Hum Reprod. 2006;21:1612–1617. doi: 10.1093/humrep/dei502. [DOI] [PubMed] [Google Scholar]
- 7.Wang L, Qiao J, Li R, et al. Role of endometrial blood flow assessment with color Doppler energy in predicting pregnancy outcome of IVF-ET cycles. Reprod Biol Endocrinol. 2010;8:122. doi: 10.1186/1477-7827-8-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Singh N, Bahadur A, Mittal S, et al. Predictive value of endometrial thickness, pattern and sub-endometrial blood flows on the day of hCG by 2D Doppler in vitro fertilization cycles: a prospective clinical study from a tertiary care unit. J Hum ReprodSci. 2011;4:29–33. doi: 10.4103/0974-1208.82357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu HM, Chiang CH, Huang HY, et al. Detection of the subendometrial vascularization flow index by three-dimensional ultrasound may be useful for predicting the pregnancy rate for patients undergoing in vitro fertilization-embryo transfer. FertilSteril. 2003;79:507–511. doi: 10.1016/s0015-0282(02)04698-8. [DOI] [PubMed] [Google Scholar]
- 10.KupesicS Bekavac I, Bjelos D, et al. Assessment of endometrial receptivity by transvaginal color Doppler and three-dimensional power Doppler ultrasonography in patients undergoing in vitro fertilization procedures. J Ultrasound Med. 2001;20:125–134. doi: 10.7863/jum.2001.20.2.125. [DOI] [PubMed] [Google Scholar]
- 11.Ng EHY, Chan CCW, Tang OS, et al. Changes in endometrial and subendometrial blood flow in IVF. Reprod BioMed Online. 2009;18(2):269–275. doi: 10.1016/S1472-6483(10)60265-9. [DOI] [PubMed] [Google Scholar]
- 12.Zácková T, Järvelä IY, Tapanainen JS, et al. Assessment of endometrial and ovarian characteristics using three dimensional power Doppler ultrasound to predict response in frozen embryo transfer cycles. Reprod Biol Endocrinol. 2009;7:151. doi: 10.1186/1477-7827-7-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Check JH, Dietterich C, Lurie D, et al. The relationship of color and power Doppler ultrasound parameters of pulsatility and resistance indices and sub-endometrial blood flow with endometrial thickness on day prior to progesterone administration and their relationship to clinical pregnancy rate following frozen embryo transfer. Fertil Steril. 2003;80:S123. doi: 10.1016/S0015-0282(03)01197-X. [DOI] [Google Scholar]
- 14.Tekay A, Martikainen H, Jouppila P. Blood flow changes in uterine and ovarian vasculature, and predictive value of transvaginal pulsed colour Doppler ultrasonography in an in vitro fertilization programme. Hum Reprod. 1995;10:688–693. doi: 10.1093/oxfordjournals.humrep.a136013. [DOI] [PubMed] [Google Scholar]
- 15.Ng EH, Chan CC, Tang OS, et al. Endometrial and subendometrial vascularity is higher in pregnant patients with livebirth following ART than in those who suffer a miscarriage. Hum Reprod. 2007;22:1134–1141. doi: 10.1093/humrep/del458. [DOI] [PubMed] [Google Scholar]