Abstract
Objectives
To audit the data of caesarean sections carried out in single-handed-run small private hospitals on the basis of the modified Robson criteria (Canada), to know the changing trends of caesarean sections over a considerable duration of time (15 years) in private sector, and to focus on a particular group out of the classification of caesarean section in the efforts to reduce the caesarean section rate.
Methods
It is a retrospective observational study of 7342 caesarean section cases carried out in different small private maternity hospitals over a period of 15 years. The data analysed by applying the modified Robson criteria (Canada) and the changing trends were studied in the view of reducing caesarean section rate.
Results
Statistically significant increasing trend was observed in groups of both primary and repeat caesarean section cases done before the onset of labour in the last 5 years.
Conclusion
Auditing the data of caesarean sections on the basis of the modified Robson criteria (Canada) is a better way of classification as compared to Ten Group Classification System (TGCS). The change in trends is seen only in the last 5 years, which suggests that there is shift in attitude of the obstetricians of small private hospitals in performing caesarean sections before onset of labour than performing it after the onset of labour. Our analysis suggests the obstetricians from small private hospitals to target groups 2B, 4B and 5C.
Keywords: TGCS (Canada), Small private maternity hospitals, Caesarean section
Introduction
The problem of rising incidence of caesarean sections and efforts to reduce the same has reached an enigmatic level. The results of many studies in the world show increasing trend in the caesarean section rate. The concern is being expressed as ‘Global Epidemic’ of caesarean section in some countries. It is a matter of concern not only for the obstetricians and people in the society, but also for the social scientists.
Facilities for caesarean sections are provided by teaching and nonteaching hospitals, public and private multispecialty institutions, and small single-handed-run obstetric units. Obstetric healthcare units are expected to provide the services throughout the day. As the facility and care system differ, the rate of caesarean sections can differ. The literature shows results of studies from bigger institutes located in major cities. However, nowadays the facilities for caesarean sections are made available at smaller towns also. The audit of caesarean sections at such centres needs to be done as the trend of caesarean section at such centres can influence the overall caesarean section rates. Audit also plays an important role in knowing the changing trends in caesarean section rate, the needs and benefits of such changes, and to modify the obstetricians’ view towards performing caesarean delivery [1]. To address this issue, in 2001, Dr. Michael Robson of National Maternity Hospital, Dublin, proposed the new Ten Group Classification System (TGCS). These ten groups are mutually exclusive, simple to use and read, yet include the total sample. The Robson ten-group way of classification facilitates comparative analysis of caesarean sections between hospitals/centres nationally, internationally and globally.
Authors from teaching hospitals in many countries have reported their positive experience with this classification which can be used more extensively [2]. The feasibility to use this classification in India is also mentioned. [3].
The studies from the other parts of the world, for example, in Europe [4] and Canada [5], also emphasise the importance of TGCS in monitoring caesarean section rates. The modification in the original classification suggested by M. Robson was approved by the Executive and Council of Society of Obstetricians and Gynaecologists of Canada in 2012. The modified Robson criteria (Canada) [6] maintain the same basic concept of classification of caesarean sections as suggested in the original Robson criteria. The original TGCS divides the caesarean sections into ten groups, and in fact, the modified criteria make it into 24 groups considering all the subgroups (Table 1). The modification is at the level of adding subgroups so as to provide more clarity. It helps to focus on a particular group in the efforts to reduce the caesarean section rate.
Table 1.
Description of original Robson criteria and the modified Robson criteria
| Group | M. Robson ten group | The modified Robson |
|---|---|---|
| 1. | Nulliparous women with single cephalic pregnancy, at ≥37 weeks gestation in spontaneous labour | Nullipara, singleton cephalic, ≥37 weeks, spontaneous labour |
| 2. | Nulliparous women with single cephalic pregnancy, ≥37 weeks gestation, who either had labour induced or were delivered by caesarean section before labour | Nullipara, singleton cephalic, ≥37 weeks, A: Induced B: Caesarean section before labour |
| 3. | Multiparous women, without a previous uterine scar with single cephalic pregnancy, ≥37 weeks gestation in spontaneous labour | Multipara, singleton cephalic, ≥37 weeks, spontaneous labour |
| 4. | Multiparous women, without a previous uterine scar with single cephalic pregnancy, ≥37 weeks gestation who either had labour induced or were delivered by caesarean section before labour | Multipara, singleton cephalic, ≥37 weeks, A: Induced B: Caesarean section before labour |
| 5. | All multiparous women, with at least one previous uterine scar and a single cephalic pregnancy ≥37 weeks gestation | Previous caesarean section, Singleton cephalic, ≥37 weeks A: Spontaneous labour B: Induced labour C: Caesarean section before labour |
| 6. | All nulliparous women with a single breech pregnancy | All nulliparous breeches A: Spontaneous labour B: Induced labour C: Caesarean section before labour |
| 7. | All multiparous women with a single breech pregnancy including, women with previous uterine scars | All multiparous breeches (including previous caesarean section) A: Spontaneous labour B: Induced labour C: Caesarean section before labour |
| 8. | All women with multiple pregnancies, including women with previous uterine scars | All multiple pregnancies (including previous caesarean section) A: Spontaneous labour B: Induced labour C: Caesarean section before labour |
| 9. | All women with a single pregnancy with a transverse or oblique lie, including women with previous uterine scars | All abnormal lies (including previous caesarean section but excluding breech) A: Spontaneous labour B: Induced labour C: Caesarean section before labour |
| 10. | All women with single cephalic pregnancy at less than or equal to 36 weeks gestation, including women with previous scars | All singleton cephalic, ≤36 weeks (including previous caesarean section) A: Spontaneous labour B: Induced labour C: Caesarean section before labour |
The circumstances both medical and nonmedical in which the decision of caesarean section is taken in small private hospitals are different from public and private institutions. The increasing trend in caesarean section rate is not only observed in private hospitals, but is increasing in institutions also. The results of the study conducted in a teaching hospital in Singapore show that caesarean section rate has increased from 19.9 to 29.6 per 100 births from 2000 to 2010. The increase in caesarean section rate is attributed largely to rising caesarean section rate in group 5 followed by group 1 [7]. There is an increase in trend in both primary and repeat caesarean rates [8].
Although issues such as medicolegal pressure are often invoked as responsible for the increasing caesarean delivery rate, it is not clear whether this is responsible for large degree of the problem. Rather, issues such as staffing and workload seem to be important. A caesarean delivery requires approximately two hours of a physician’s time and can be scheduled and planned. A vaginal delivery, on the other hand, is unpredictable and requires a physician’s presence for far longer. In our hurried culture, patience is often limited on the part of patients and providers. Finally, for the labour and delivery provider, pressures include not only the extra workload of a vaginal delivery, but also the desire not to leave unfinished work to colleagues at change of shift. Attention to staffing, systems approaches and consideration of the human factor in mode of delivery are important additional perspectives that should be considered in trying to solve this complex problem [9].
Most of the articles in the literature review are from teaching institutions. The literature lacks a report of collected data from small private hospitals run by only one obstetrician (usually owner). Caesarean sections from such hospitals form a major bulk in towns and small cities. The present study has this as a unique feature.
The aim of present study is (1) to audit the data of caesarean sections carried out in single-handed-run small private hospitals on the basis of the modified Robson criteria (Canada), (2) to know the changing trends of caesarean sections over a considerable duration of time (15 years) in private sector and (3) to focus on a particular group out of the classification of caesarean section in the efforts to reduce the caesarean section rate.
Methods
The present study has been carried out at a district place located in west zone of India. This place provides maternity services to the society through three public institutions and many small maternity hospitals in private sector. The annual average of deliveries in public institutions and private hospitals in the last 4 years was similar, 11,799 and 11,785 respectively. The incidence of caesarean section in public institute was 22.46 %, and that in private sector was 36.47 % (14 % more in private sector).
It is a retrospective observational study of 7342 caesarean section cases carried out in different small private maternity hospitals over a period of 15 years. The period of the study is from 24 July 1999 to 23 July 2014. Indication of each caesarean section was noted down immediately after the procedure by the author himself in a pro forma in which many other clinical parameters were also included. The author is a visiting (on-call) obstetrician. Majority of his participation in caesarean section cases was in 12 different small maternity hospitals. He participated in all the 7342 cases included in the study. These 7342 cases were grouped according to the modified Robson criteria (Canada) and the data analysed. Table 1 describes both, the Robson TGCS and the modified Robson criteria. To study the changes in the trends, the data were grouped in three different slots of 5 years each. For quick understanding, the first 5-year data (from 24 July 1999 to 23 July 2004) was labelled as F5, middle 5 years (from 24 July 2004 to 23 July 2009) as M5, and last 5 years (from 24 July 2009 to 23 July 2014) as L5. The changing trends observed were analysed in each group on the basis of the modified Robson criteria (Canada) and the figures of F5, M5 and L5 compared. Statistical analysis of the data was done. ‘Z’ test for a difference between proportions was used to test the statistical significance.
This work does not involve any modification of existing therapy or surgical procedure. It is just an observational study analysing the recorded data. Hence, ethical committee approval was not obtained.
Results
The total number of cases studied in 15 years was 7342. The number of cases in the first 5 years (F5) were 1681, in the middle 5 years (M5) 2380, and in the last 5 years (L5) 3281. These cases were classified according to the modified Robson criteria (Canada). Table 2 shows the distribution of cases in each group. A reducing trend was observed in group 1. The percentage of group 1 cases in F5 was 35.33, in M5 was 31.38, and in L5 was 26.12. An increasing trend is seen in group 2B. The percentage of group 2B cases in F5 was 9.57, in M5 was 11.05, and in L5 was 21.27. No much change was observed in group 3 in F5 and M5; however, the percentage decreased in L5. Decreasing trend was observed in group 4A. The percentage of cases in group 4B was one and half times more in L5 (4.32) as compared to cases in F5 (2.79).
Table 2.
Distribution of cases in each group during each 5 year
| Group | First 5 years (F5) N = 1681 (%) |
Middle 5 years (M5) N = 2380 (%) |
Last 5 years (L5) N = 3281 (%) |
(F5) versus (M5) ‘p’ value |
(M5) versus (L5) ‘p’ value |
(F5) versus (L5) ‘p’ value |
|---|---|---|---|---|---|---|
| I | II | III | ||||
| 1 | 594 (35.33) | 747 (31.38) | 857 (26.12) | Z = 2.62, p < 0.01 more significant | Z = 4.30, p < 0.001 highly significant | Z = 6.60, p < 0.001, highly significant, |
| 2A | 81 (4.81) | 127 (5.33) | 108 (3.290 | |||
| 2B | 161 (9.57) | 263 (11.05) | 698 (21.27) | Z = 1.54, p > 0.05 insignificant | Z = 10.6, p < 0.001 highly significant | Z = 11.5, p < 0.001 highly significant |
| 3 | 103 (6.12) | 148 (6.21) | 147 (4.48) | |||
| 4A | 23 (1.36) | 30 (1.26) | 33 (1.00) | |||
| 4B | 47 (2.79) | 71 (2.98) | 142 (4.32) | Z = 0.36, p > 0.05 insignificant | Z = 2.69, p < 0.01 more significant | Z = 2.85, p < 0.01 more significant |
| 5A | 263 (15.64) | 351 (14.74) | 333 (10.41) | Z = 0.78, p > 0.05 insignificant | Z = 4.8, p < 0.001 highly significant | Z = 5.06, p < 0.001 highly significant |
| 5B | 06 (0.35) | 05 (0.21) | 00 | |||
| 5C | 197 (11.71) | 337 (14.15) | 610 (18.59) | Z = 2.3, p < 0.05 significant | Z = 4.5, p < 0.001 highly significant | Z = 6.63, p < 0.001 highly significant |
| 6A | 55 (3.27) | 72 (3.02) | 43 (1.31) | |||
| 6B | 00 | 00 | 00 | |||
| 6C | 17 (1.01) | 35(1.47) | 84 (2.56) | |||
| 7A | 25 (1.48) | 46 (1.93) | 37 (1.12) | |||
| 7B | 00 | 00 | 00 | |||
| 7C | 19 (1.13) | 43 (1.80) | 61 (1.85) | |||
| 8A | 18 (1.07) | 31 (1.30) | 27 (0.82) | |||
| 8B | 00 | 01 (0.04) | 00 | |||
| 8C | 05 (0.29) | 13 (0.54) | 16 (0.48) | |||
| 9A | 23 (1.36) | 15 (0.63) | 10 (0.30) | |||
| 9B | 00 | 00 | 00 | |||
| 9C | 03 (0.17) | 03 (0.12) | 10 (0.30) | |||
| 10A | 14 (0.83) | 16 (0.67) | 36 (1.09) | |||
| 10 B | 03 (0.17) | 04 (0.16) | 02 (0.06) | |||
| 10C | 24 (1.42) | 22 (0.92) | 27 (0.82) |
* Z test for a difference between proportions is used to test the statistical significance (table value of Z = 1.96, p = 0.05; Z = 2.58, p = 0.01; Z = 3.29, p = 0.001)
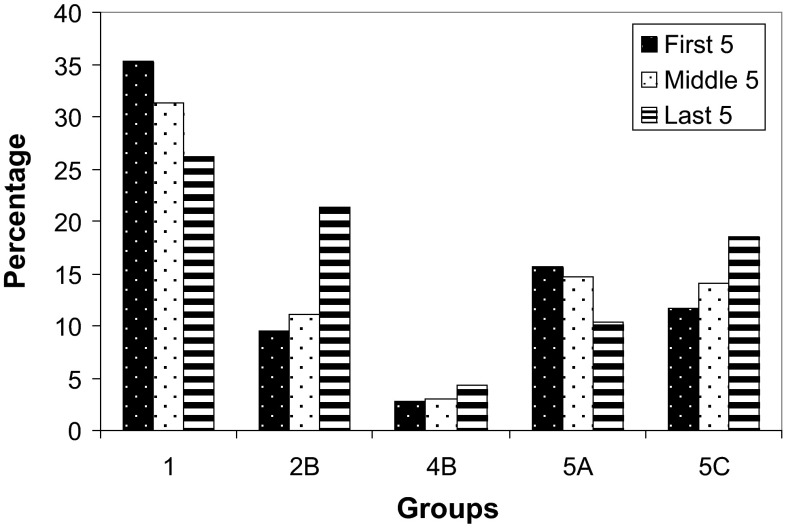
Changing trends were also noted in previous caesarean section cases. A reducing pattern was observed in group 5A. In L5, the proportion of cases in this group was 10.41 as compared to 15.64 in F5. We observed an increasing trend in group 5C. The percentage of cases in this group increased from 11.71 in F5 to 18.59 in L5. Interestingly, the number of previous caesarean cases in group 5B was very less in both F5 and M5, and reduced to nil in L5. Decreasing trend was observed in group 6A, and an increasing trend in group 6C. However, the trend remains unchanged in multiparous breech cases (groups 7A, 7B and 7C). Group 8 belongs to twin pregnancy, and group 9 to abnormal presentations. There appears to be no much change in both these groups. There is hardly any change observed in all preterm cases with cephalic presentation (group 10). The statistically significant changing trends observed in our study are shown in bar diagram (Fig. 1).
Fig. 1.
Comparison of trends in nullipara and previous caesarean section
Discussion
There is enough evidence in the literature stating the importance of M. Robson TGCS and its modifications in the efforts to reduce the caesarean section rate. In fact, it is established that classification of the data of caesarean sections undertaken in any kind of obstetric unit in the world becomes a fundamental step towards these efforts.
Analysis of our data by applying the modified Robson criteria (Canada) enables us to target our efforts more specifically. The results of our study help us to know which subgroup of the caesarean sections shows the increasing trend. The statistically significant increasing trend in group 2B, especially in the last 5 years, shows that in nulliparous patients at term having cephalic presentation, more cases are undertaken for caesarean section before the onset of labour than in spontaneous labour. Same is true, when we look at our observations of previous caesarean section cases. This changed trend in groups 2B and 5C cases indicates the shift in the attitude of the obstetricians in favour of caesarean section before the onset of labour rather than after the onset of labour. This attitude denies the patients from the opportunity of possibility of vaginal delivery after caesarean section (VBAC).
It is expected that one who delivered vaginally earlier would deliver vaginally again than the ones needing a caesarean section. In such multiparous cases (group 4B), we expect the incidence of caesarean section to be the same. In the present study, the trend shows significant rise in the last 5 years in this group. It suggests that multiparas having unscarred uteri were also taken for caesarean section before the onset of labour, more frequently in the last 5 years. Targeting this group would help the efforts in reducing the caesarean section rate.
The cases in groups 1, 2A and 2B are nullipara. Group 1 shows decreasing trend in the last 5 years. This trend appears at the cost of group 2B which shows a rise. As such, the rate of caesarean section in nullipara (groups 1, 2A and 2B together) appears almost unchanged (Table 3). But there is just a shift of trend from group 1 to group 2B. In other words, in the last 5 years, more nulliparas are subjected to caesarean section before the onset of labour instead after the onset of labour. It is possible to make out such shifts of trends only by the use the modified Robson criteria (Canada).
Table 3.
Comparison of trends in nullipara and previous caesarean section
| Group | First 5 years N = 1681 (%) F5 |
Middle 5 years N = 2380 (%) M5 |
Last 5 years N = 3281 (%) L5 |
|---|---|---|---|
| 1 | 594 (35.33) | 747 (31.38) | 857 (26.12) |
| 2A | 81 (4.81) | 127 (5.33) | 108 (3.290 |
| 2B | 161 (9.57) | 263 (11.05) | 698 (21.27) |
| 1 + 2A + 2B | 836 (49.73) | 1137 (47.77) | 1663 (50.68) |
| 5A | 263 (15.64) | 351 (14.74) | 333 (10.41) |
| 5B | 06 (0.35) | 05 (0.21) | 00 |
| 5C | 197 (11.71) | 337 (14.15) | 610 (18.59) |
| 5A + 5B + 5C | 466 (27.72) | 693 (29.11) | 943 (28.74) |
The trend is of performing less caesarean sections in group 5A, but more in 5C in the last 5 years, keeping the overall rate unchanged for previous caesarean section cases as observed in nullipara (Table 3). Thus, the obstetricians in our locality over these 15 years have treated the cases of previous caesarean section in the same manner as they treated the nullipara.
This audit shows that small private hospital obstetricians are more in favour of caesarean section before the onset of labour than after the onset of labour in both nullipara and previous caesarean cases, in the last 5 years. Similar approach in managing multipara is obvious, as there is rising trend in multipara with unscarred uterus before the onset of labour.
Obstetricians having individual small maternity homes in private sector work 24 × 7 face problem of monitoring of labour meticulously. In the world of people having accepted the concept of small family norm, every baby to be born is precious. The inclination of the obstetricians from private sector to take a decision of caesarean section before labour is to have almost zero risk of neonatal morbidity and mortality in the process of monitoring of labour. This contributes to the increasing trend of primary and repeat caesarean section before labour. More number of caesarean sections are performed in multiparous cases having unscarred uterus for the same reasons.
It might be suggested that single obstetrician of small private hospitals needs additional qualified help in labour monitoring. This help would alleviate their fear of labour monitoring and reduce their workload. The stress of working 24 × 7 will be shared allowing enthusiastic and more meticulous labour monitoring. With this arrangement, obstetricians of small private hospitals would welcome women in labour thereby attempting reduction in caesarean section rate by improved labour monitoring in unscarred and scarred uteri.
Conclusion
Auditing the data of caesarean sections by modified Robson criteria (Canada) is a better way of classification as compared to TGCS. The results of our study show statistically significant rising trends in groups 2B, 4B and 5C and reducing trends in groups 1 and 5A. The change in trends is not uniform over 15 years, but is seen only in the last 5 years. This suggests that there is a shift in attitude of the obstetricians of small private hospitals in doing caesarean sections before onset of labour than doing it after the onset of labour in the last 5 years. The trend is shifting from ‘spontaneous labour’ status to ‘before labour’ status both in primary and repeat caesarean section cases. Our analysis suggests the obstetricians from small private hospitals to target groups 2B, 4B and 5C. To target these groups in order to reduce the caesarean section rate, these obstetricians need to involve qualified personnel who would help them in monitoring labour.
Acknowledgments
We thank all the owner obstetricians of small private maternity hospitals for permitting us to use the caesarean section data for this study. We also thank Mr. B. K. Kadam, from V. M. Medical college, Solapur, for helping us in statistical analysis of the collected data.
Kishore B. Atnurkar
is a senior obstetric gynec specialty practitioner from Nanded, Maharashtra, and has special interests in Medical Sociology, Health Education, and Counselling related to Women’s Health. He is awarded Ph.D. in Social Sciences for his work in Population Control Program. He runs a counselling centre which deals with reproductive health of women. He holds an MS in Counselling and Psychotherapy as well. As a visiting obstetric surgeon, he has documented different aspects of caesarean section in about 8000 cases in the last 16 years.
Compliance with Ethical Requirements
Conflict of interest
There are no copyright and conflict of interest issues. No financial support from any agency.
Ethical Standards
This work does not involve any modification of existing therapy or surgical procedure. It is just an observational study analysing the recorded data. Hence, ethical committee approval was not obtained.
Footnotes
Kishore B. Atnurkar is a senior obstetric gynec specialty practitioner from Nanded, Maharashtra. Arun R. Mahale is a Consultant Obstetrician & Gynecologist, Mahale Hospital, Borban, Nanded, Maharashtra.
References
- 1.Das S, Char D, Sarkar S, et al. Changing trends in caesarean section: rate and indications. J Dental Med Sci (IOSR-JDMS) 2014;13(1):7–9. [Google Scholar]
- 2.Torloni MR, Betran AP, Souza JP, et al. Classifications for cesarean section: a systematic review. PLoS ONE. 2011;6(1):e14566. doi: 10.1371/journal.pone.0014566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prasad M. Good time to adopt ten-group Robson classification to report LSCS rates in india? Letter to the Editor. J Obstet Gynecol India. 2015;65(4):286–287. doi: 10.1007/s13224-014-0656-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scarella A, Chamy V, Sepulveda M, et al. Medical audit using the Ten Group Classification System and its impact on the caesarean section rate. Eur J Obstet Gynecol Reprod Biol. 2011;154(2):136–140. doi: 10.1016/j.ejogrb.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 5.Kelly S, Sprague A, Fell DB, et al. Examining caesarean section rates in Canada using the Robson classification system. J Obstet Gynaecol Can. 2013;35(3):206–214. doi: 10.1016/S1701-2163(15)30992-0. [DOI] [PubMed] [Google Scholar]
- 6.Farine D, Shephard D. Classification of caesarean sections in Canada: the modified Robson criteria. J Obstet Gynaecol Can. 2012;34(10):976–983. doi: 10.1016/S1701-2163(16)35412-3. [DOI] [PubMed] [Google Scholar]
- 7.Cheryl C, Lin LS, Arijit B. Changing trends of caesarean section births by Robson Ten group classification in a tertiary teaching hospital. Acta Obstet Gynecol Scand. 2012 doi: 10.1111/j.1600-0412.2012.01529.x. [DOI] [PubMed] [Google Scholar]
- 8.Barber EL, Lundsberg LS, Belanger K, et al. Indications contributing to the increasing caesarean delivery rate. Obstet Gynecol. 2011;118(1):29–38. doi: 10.1097/AOG.0b013e31821e5f65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Norton ME. Editorial comment on Safe prevention of the Primary Ceasarean Delivery. Obstet Gynecol Survey. 2014;69(7):381–383. doi: 10.1097/OGX.0000000000000083. [DOI] [Google Scholar]