Abstract
Purpose
In this study, we aimed to correlate thromboelastography (TEG) variables versus conventional coagulation profile in all patients presenting with pre-eclampsia/eclampsia and to see whether TEG would be helpful for evaluating coagulation in parturients before regional anaesthesia.
Materials and Methods
This was a prospective study on 100 pre-eclampsia/eclampsia patients undergoing lower-segment caesarean section under regional anaesthesia. Two blood samples were collected. First sample was used for TEG measurement and second sample for laboratory tests. The following TEG data were obtained—reaction time, kinetic time, alpha angle, and maximum amplitude (MA). The following laboratory tests were obtained—haematology (haemoglobin, TLC, DLC, platelet count) and coagulation test [prothrombin time (PT), activated partial thromboplastin time (aPTT), thrombin time (TT)].
Result
Out of 100 patients enrolled in the study, 80 (80 %) had a normal coagulation profile, while remaining 20 (20 %) had hypocoagulation profile. The results show that TEG parameters have a good correlation with conventional coagulation profile and also showed excellent independent predictive efficacy for prediction of hypocoagulation. PT, aPTT, and TT were directly proportional to R-time and K-time and inversely proportional to alpha angle (p < 0.001). Platelet count showed a strong positive correlation with MA (p < 0.001).
Conclusion
By giving a global picture of haemostasis, TEG can lead to improved decision-making about safety of using regional anaesthesia. Its fast feedback time makes it ideal for monitoring in a fast moving situation such as in obstetric emergency.
Keywords: Thromboelastography, Coagulation, Regional anaesthesia
Introduction
Thromboelastography (TEG) has enormous potential in the operating room and labour ward for assisting obstetric anaesthesiologist in decision-making. It has been used to assess hypercoagulable states and coagulation defects in pregnancy [1]. Pre-eclampsia/eclampsia is one of the most common comorbid conditions we as anaesthesiologists face in emergency in obstetric anaesthesia. This is associated with risk of abnormal haemostasis that occurs because of thrombocytopenia [2] and rarely because of a mild disseminated intravascular coagulation. The risk of abnormal haemostasis increases with severity of pre-eclampsia. Regional anaesthesia is the mainstay therapy for both in normal and in pre-eclampsia/eclampsia patients. Thrombocytopenia is a relative contraindication of neuraxial anaesthesia due to risk of intraspinal bleed and epidural haematoma despite clear foetal and maternal benefits of regional anaesthesia.
Thromboelastography was developed first by Hartert in 1948 [3]. It is small and compact equipment that is attached to the computer. It did not gain widespread usage in clinical practice. However, in the past few years there has been a resurgence of interest in techniques that evaluate the viscoelastic properties of whole blood during preoperative and perioperative period.
Advantage of TEG
While conventional tests evaluate the coagulation pathway until the formation of first fibrin strands, the TEG documents the interaction of platelets with the protein coagulation cascade from the time of the initial platelet–fibrin interaction, through platelet aggregation, clot strengthening, and fibrin cross-linkage to eventual clot lysis. Hence, it is dynamic and gives information on the entire coagulation process and not just on isolated part. TEG tracings are specific (“signature tracings”) to the individual. TEG is a bedside procedure, and rapid results facilitate timely intervention. Also, being computerized process, it is easy to use and results can be recorded and stored.
Disadvantage of TEG
The disadvantages of TEG include relatively high coefficient of variation, poorly standardized methodologies, and limitations on specimen stability of native whole blood samples. TEG cannot identify the individual coagulation factors, e.g. VIII, IX, and X.
Routine laboratory tests are generally performed on centrifuged plasma fractions and examine only isolated portions of the coagulation cascade. Conventional coagulation screens (prothrombin time PT, activated partial thromboplastin time aPTT, and platelet count) take time and are frequently inadequate for the purpose of monitoring coagulation [4], and they give no information about the vital interaction between platelets and the coagulation cascade. In fact, it is theoretically possible to have normal PT and aPTT values but still have active bleeding as a result of abnormal haemostasis. TEG may be useful, therefore, for in vitro assessment of platelet function in whole blood and coagulopathy. TEG can be used to assess hypercoagulable states and coagulation defects in pregnancy [5].
By giving a global picture of haemostasis, TEG can lead to improved decision-making about safety of using regional anaesthesia. So for this purpose the present study was carried out with an aim to correlate TEG variables versus conventional coagulation profile in all patients presenting with pre-eclampsia/eclampsia for LSCS and see whether in future TEG can be used safely as an alternative to coagulation profile in emergencies.
Materials and Methods
After taking ethical consent from the university ethical committee, this prospective study was planned on pre-eclampsia/eclampsia patients undergoing lower-segment caesarean section under regional anaesthesia. After getting informed consent, patients presenting to delivery suite with a diagnosis of pre-eclampsia/eclampsia were entered in the study.
The thromboelastographic study was performed on the thromboelastometer—Hemologix™ (TEM-A [Framar biomedica (s.r.l. Zona Industriale Roma Nord—Via degli Olmetti 36 00,060 Formello (RM)—Italy)].
Pre-eclampsia was defined as a systolic pressure >140 mm Hg, diastolic pressure >90 mm Hg, and proteinuria >0.3 gm/24 h. Eclampsia is diagnosed on documented history of recent convulsion in any patient presenting with other features of pre-eclampsia without any history of epilepsy and in whom no other cause for convulsion could be determined.
Normal pregnancy is associated with an increased incidence of thrombocytopenia, with 6.6 % of pregnant women presenting with platelet count less than 1.5 lakh/mm3. In addition, pre-eclampsia may complicate up to 12 % of pregnancies and is often associated with abnormalities of haemostasis, although thrombocytopenia may occur in up to 50 % of patients with severe disease. Platelet dysfunction may also be presented despite adequate platelet numbers. Parturients frequently require regional anaesthesia, and despite the ready availability of platelet counts and coagulation tests, the lower limit of platelet count at which safe regional anaesthesia can be performed is unclear. TEG is an on-site monitor that measures all phases of coagulation to clot retraction. Its usefulness, compared with conventional coagulation tests, has been described during liver transplantation and after cardiopulmonary bypass [1].
The patients who had any confounding conditions that could have altered the coagulation tests such as placental abruption or previa, stillborn, sepsis or heavy vaginal bleeding or recent ingestion of antiplatelet medications with in previous week were excluded. Thrombocytopenia was defined as platelet count <100,000/mm3. PT and aPTT were considered abnormal if PT was >13 s and aPTT > 40 s.
After admission, patients with diagnosis of pre-eclampsia/eclampsia who were planned for lower-segment caesarean section were taken into operation theatre. Patient’s blood pressure was recorded in operation theatre and intravenous infusion of crystalloid started. Two blood samples were collected. First sample was used for TEG measurement and second sample for laboratory tests.
The following TEG data were obtained
Reaction time (R-time)
Kinetic time (K-time)
Alpha angle (α-angle)
Maximum amplitude (MA)
The following laboratory tests were obtained
Haematology (haemoglobin and platelet count)
-
Coagulation test [(prothrombin time (PT), activated partial thromboplastin time (aPTT), and thrombin time (TT)]
All data were analysed statistically.
Results
The present study was carried out with an aim to correlate TEG variables versus conventional coagulation profile in all patients presenting with pre-eclampsia/eclampsia. For this purpose, a total of 100 parturient women presenting with pre-eclampsia/eclampsia (78 % pre-eclampsia and 22 % eclampsia) were enrolled in the study. Out of 100 patients enrolled in the study, 80 (80 %) had a normal coagulation profile, while remaining 20 (20 %) had hypocoagulation profile.
Mean age of patients was 22.74 ± 2.15 years. The demographic profile is summarized in Table 1.
Table 1.
Demographic profile
| Diagnosis | Total (n = 100) | |
|---|---|---|
| Mean | Standard deviation (SD) | |
| Age (years) | 22.74 | 2.15 |
| Weight (kg) | 55.88 | 4.52 |
| Height (cm) | 154.9 | 4.52 |
| Body mass index (kg/m2) | 23.32 | 2.10 |
n is total no. of parturients included in the study
Table 2 shows comparison of Hb, TEG parameters and conventional coagulation profile in normal and hypocoagulable profile patients. To test the significance of two means, the Student’s t test was used. Mean R-time, K-time, prothrombin time, activated prothrombin time, and thrombin time values were significantly lower in group I as compared to group II, whereas mean alpha angle, MA, and platelet count values were significantly higher in group I as compared to group II. For all the TEG parameters and conventional coagulation profile, the difference was statistically significant (p < 0.001).
Table 2.
Comparison of Hb, TEG parameters, and coagulation profile
| Parameter | Patients with normal coagulation (n = 80) | Patients with hypocoagulation (n = 20) | Significance of difference | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | t | p | |
| Hb (gm/dl) | 10.08 | 1.60 | 9.73 | 1.84 | 0.592 | 0.557 |
| R-time (min) | 5.92 | 2.32 | 16.66 | 11.07 | −5.806 | <0.001 |
| K-time (min) | 2.50 | 1.49 | 9.35 | 6.74 | −6.039 | <0.001 |
| Alpha angle | 58.26 | 12.83 | 28.05 | 11.23 | 6.813 | <0.001 |
| MA (mm) | 74.46 | 17.08 | 38.91 | 14.55 | 6.045 | <0.001 |
| PT (s) | 12.80 | 0.72 | 21.00 | 6.46 | −8.071 | <0.001 |
| aPTT (s) | 23.13 | 1.76 | 41.50 | 10.02 | −11.248 | <0.001 |
| TT (s) | 12.78 | 0.77 | 20.80 | 5.27 | −9.525 | <0.001 |
| Platelet count (lakh/cumm) | 2.37 | 0.62 | 0.93 | 0.31 | 7.148 | <0.001 |
Data were analysed using Pearson correlation coefficient (r) and level of significance (p). There is a strong positive correlation of TEG parameters R-time and K-time with conventional parameters PT, aPTT, and TT{correlation coefficient (r) >0.9 and level of significance (p) <0.001}. TEG parameter alpha angle showed moderate inverse correlation with PT (r = −0.67) and a strong inverse correlation with aPTT and TT (r < −0.70). Alpha angle also showed a moderate positive correlation with platelet count (r = 0.50). TEG parameter MA showed moderate inverse correlation with PT, aPTT and TT (r < −0.50) and a moderate positive correlation with platelet count (r = 0.61).
In patients of hypocoagulation by conventional method, PT, aPTT, and TT showed a strong and significant positive correlation with R-time and K-time (r > 0.7), a strong inverse correlation with alpha angle (r < −0.80), and a poor correlation with MA. Platelet count showed a weak correlation with R-time, K-time and alpha angle (r < 0.3) and a strong positive correlation with MA (r = 0.83).
Table 3 shows that with increasing R-time and K-time values, a significant increase in proportion of patients with hypocoagulative profile was observed (p < 0.001). With decreasing alpha angle and MA values, a significant increase in proportion of patients with hypocoagulative profile was observed (p < 0.001). By analysing R-time and K-time, it is also clear that 85.7 % parturients were hypocoagulable in group II. By analysing MA, 12 out of 20 parturients in group II were having abnormal platelet function.
Table 3.
Validation of cut-off values of different TEG parameters for evaluation of coagulation
| Parameter | Total | Group I | Group II | Significance of difference | ||
|---|---|---|---|---|---|---|
| No. | % | No. | % | p | ||
| R-time (min) | ||||||
| <9.5 min | 60 | 58 | 96.7 | 2 | 3.3 | <0.001 |
| 9.5–14.0 min | 36 | 20 | 76.9 | 6 | 23.1 | |
| >14.0 min | 14 | 2 | 14.3 | 12 | 85.7 | |
| K-time (min) | ||||||
| <4.0 min | 34 | 34 | 100.0 | 0 | 0.0 | <0.001 |
| 4.0–6.5 min | 52 | 44 | 84.6 | 8 | 15.4 | |
| >6.5 min | 14 | 2 | 14.3 | 12 | 85.7 | |
| Alpha angle | ||||||
| <29° | 22 | 6 | 27.3 | 16 | 72.7 | <0.001 |
| 29°–43° | 12 | 10 | 83.3 | 2 | 16.7 | |
| >43° | 66 | 64 | 97.0 | 2 | 3.0 | |
| MA | ||||||
| <48 mm | 12 | 0 | 0.0 | 12 | 100.0 | <0.001 |
| 48–60 mm | 8 | 6 | 75.0 | 2 | 25.0 | |
| >60 mm | 80 | 74 | 92.5 | 6 | 7.5 | |
All the correlations tested were significant statistically.
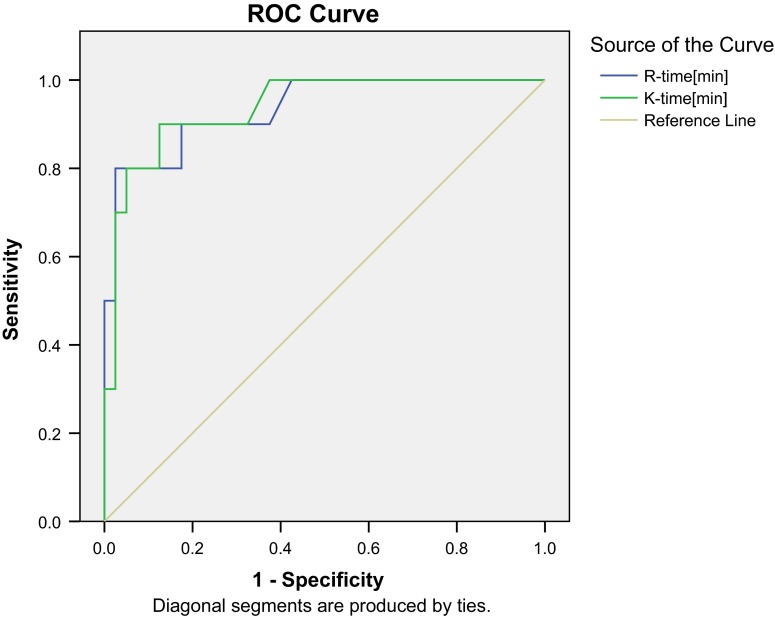
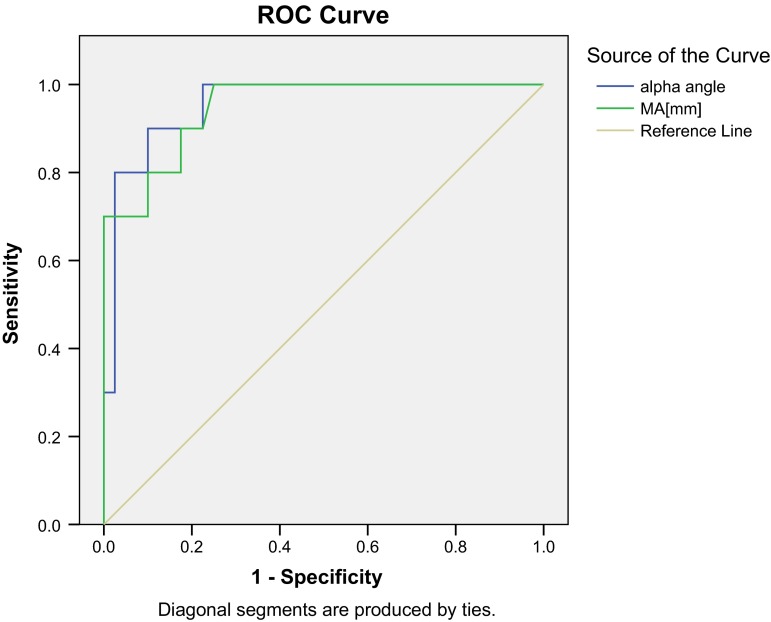
Receiver operating characteristic (ROC) curve analysis for calculation of new cut-off values of TEG parameters for prediction of hypocoagulation shows that for R-time and K-time (Fig. 1) area under curve (AUC) values were 0.935 and 0.938, respectively. Both indicated a significant association with outcome (hypocoagulation) (p < 0.001). On evaluating the coordinates of the curve, the cut-off value of ≥8.25 for R-time and >3.25 for K-time had a sensitivity of 90 % each and specificity of 82.5 and 87.5 %, respectively. Thus, K-time had a better projected sensitivity and specificity as compared to R-time. For alpha angle and MA (Fig. 2), area under curve (AUC) values were 0.955 and 0.949, respectively. Both indicated a significant association with outcome (hypocoagulation) (p < 0.001). On evaluating the coordinates of the curve, the cut-off value of ≤39.21 for alpha angle and ≤61.425 for MA had a projected sensitivity of 90 % each and specificity of 90 % and 82.5 %, respectively. Thus, alpha angle had a better projected sensitivity and specificity as compared to MA.
Fig. 1.
Receiver operating characteristic (ROC) curve analysis for calculation of new cut-off values of TEG parameters (R-time and K-time) for prediction of hypocoagulation
Fig. 2.
Receiver operating characteristic (ROC) curve analysis for calculation of new cut-off values of TEG parameters (alpha angle and MA) for prediction of hypocoagulation
The results show that TEG parameters have a good correlation with conventional coagulation parameters and also showed excellent independent predictive efficacy for prediction of hypocoagulation. PT, aPTT, and TT were directly proportional to R-time and K-time and inversely proportional to alpha angle. Platelet count showed a strong positive correlation with MA.
Discussion
In the general population, the incidence of neuraxial haematoma after epidural and spinal anaesthesia has been estimated at 1:150,000 and 1:220,000, respectively [6]. As the incidence of neuraxial haematoma after regional anaesthesia is very rare, it is difficult to design a prospective and randomized study to determine the lowest platelet count at which anaesthesiologists can safely administer regional anaesthesia in obstetric patients. TEG could provide a reasonable alternative to answer this question. It measures whole blood coagulation and provides information about the adequacy of platelet function and other clotting factors, all in a short time. So that in times of emergency a quick TEG profile could be used as a guide for the relative safety of patients with pre-eclampsia/eclampsia.
Pregnancy is a unique situation where significant physiological changes in all maternal organ systems take place. Most of these changes return to normal after delivery. During normal pregnancy, the haemostatic changes are in the direction of hypercoagulability, that decreases bleeding complications at the time of delivery. The pregnancy-associated hypercoagulability sets a foundation for haemostatic abnormalities during pregnancy and may be associated with pregnancy complications. Pre-eclampsia/eclampsia is an idiopathic multisystem disorder. Haematological abnormalities such as thrombocytopenia and decrease in some plasma clotting factors may develop in pre-eclamptic/eclamptic women. The risk of abnormal haemostasis increases with the severity of pre-eclampsia. The platelet count is routinely used as a primary test to evaluate the coagulation status in these parturients [7]. It has been shown that when the platelet count is less than 100,000/mm3, other haemostatic abnormalities, such as prolonged prothrombin time (PT) and partial thromboplastin time (PTT), and reduced fibrinogen concentration, may also be presented [8].
Assessment of the haemostatic status in pregnancy and its complications can be critical to diagnosis and management. Conventional global tests such as prothrombin time and activated partial thromboplastin time cannot define this status appropriately, and full assessment requires measurements of several parameters. Thromboelastography (TEG) is a global haemostatic test that can analyse both coagulation and fibrinolysis. The technique has been available since 1940s, but only recently it has shown great impact within the clinical practice. TEG measures the interactive dynamic coagulation process from the initial fibrin formation to platelet interaction and clot strengthening to fibrinolysis, which makes it superior to other conventional tests. In addition, TEG can guide therapy by documenting changes in coagulation in vitro before a therapy is instituted and also by helping the clinician make critical decisions. Despite the clear value as a test for monitoring haemostatic status of pregnancy-related complications, TEG is still underused for reasons such as poor awareness regarding the technique and interpretations, lack of full standardization, and the unavailability of large clinical studies. However, the fact remains that TEG is undoubtedly attractive to both researchers and clinicians [9].
Literature [8] shows that pre-eclamptic/eclamptic women are usually hypercoagulable. However, as the severity of disease increases, blood coagulability decreases, and severe pre-eclamptic/eclamptic women may be significantly hypocoagulable. In the 20 hypocoagulable parturients, results were analysed, taking into view of following facts.
PT, aPTT, and TT showed a strong and significant positive correlation with R-time and K-time and a strong inverse correlation with α-angle. PT is functional determination of the extrinsic pathway of coagulation, and it measures clotting factors I, II, V, VII, and X. aPTT is functional determination of the intrinsic pathway of coagulation, and it measures clotting factors XII, XI, IX, VIII, V, II, and I. TT is a screening coagulation test designed to assess fibrin formation from fibrinogen in plasma. R-time represents the functional behaviour of clotting factors/clotting cascade and is an indicative of clotting time. K-time represents the dynamics of clot formation, indicative of fibrinogenesis/levels of fibrin.
α-angle represents the rate of fibrin build-up (rate of polymerization) and cross-linking. MA is the result of two components: a modest contribution of the fibrin and, largely, that of the platelets functionality.
Thus, the values of R-time and K-time are directly and α-angle inversely proportional to the coagulation status. So we can get a definite idea from the TEG values as to the coagulation status of the patient. MA is directly proportional to the function of the platelets and thus reflects the platelet count. Coagulation index (CI), a description of a patient’s global coagulable state derived from the patient’s overall coagulation, is calculated from the R, K, MA, and α-angle. Normal values are from −3.0 to +3.0; values less than −3.0 represent hypocoagulable state and more than +3.0 represent hypercoagulable state [10].
Thromboelastographic parameters are interrelated and reflect activities of clotting factors, platelets, and fibrinogen, and their interaction, whereas coagulation profile monitors an isolated portion of the coagulation cascade. Therefore, TEG provides a better assessment of whole blood coagulability than does routine coagulation profile. The principle and interpretation of TEG are well described in the literature [11]. As shown by our results and other studies, pre-eclamptic/eclamptic women with a platelet count <100,000/mm3 were significantly hypocoagulable (an increase in R- and K-time and a reduction in α-angle and MA) when compared to other women. Leduc et al. [8] also demonstrated that in severe pre-eclamptic women when the platelet count is less than 100,000/mm3, other coagulation indices also become abnormal.
Shiv Sharma et al. [12] suggest that the platelet count alone is not enough to predict haemorrhagic complications in pre-eclamptic women. Some pre-eclamptic/eclamptic women with normal platelet count may also develop coagulation factors deficiency and have a potential for severe bleeding. Therefore, in pre-eclamptic/eclamptic women with thrombocytopenia, other standard tests of coagulation such as TEG should also be performed to determine the adequacy of coagulation.
In our study, three parturients with platelet counts >100,000/mm3 (1.1 lakh, 1.2 lakh, and 1.6 lakh) and their platelets function assessed by TEG were also normal (MA-60.45, 62.8, and 54.3 mm, respectively), but regional anaesthesia was not given to them because of an increased R-time and K-time. The conventional coagulation profile further also revealed an increased PT, aPTT, and TT. So we felt that TEG correlated well with the coagulation profile in parturients before regional anaesthesia.
The incidence of hypocoagulative profiles was 20 % in our study, out of which 17 % parturients (17 of 100) with platelet count <100,000/mm3 had hypocoagulation profile and 3 % parturients (3 of 100) with platelet count >100,000/mm3 had hypocoagulation profile. As our results show, if we only considered the platelet counts of <100,000/mm3 as a cause of abnormal haemostasis, we would have missed some of the cases with real coagulation abnormalities. So our results are against the concept that all pre-eclamptic/eclamptic women with a coagulation abnormality [9] would have platelet counts <100,000/mm3. We also realized that a normal platelet count can alone not assure the anaesthesiologist that no other significant clotting abnormalities are present in pre-eclampsia/eclampsia.
The major limitation is the small sample size as it was done as a pilot study. TEG cannot identify the individual coagulation factors, e.g. VIII, IX, and X. Also, this technique has never been formally validated or standardized by the haematologists in comparison with conventional coagulation tests. Sample needs to be processed within 3–4 min of collection [13], which may necessitate multiple machines in strategic areas of the hospital rather than a centralized laboratory. Transport of sample to a central area necessitates using citrated blood to prevent clotting, which can be used within 2 h. But that defeats the purpose of on-the-spot help that is required.
So the conclusion is that TEG has enormous potential in the labour ward for assisting anaesthesiologists and obstetrician. It has been used to assess hypercoagulable states and coagulation defects in pregnancy. By giving a global picture of haemostasis, TEG can lead to improved decision-making about safety of using regional anaesthesia. Its fast feedback time makes it ideal for monitoring in a fast moving situation such as in obstetric emergency.
Asrar Ahmad
graduated from Ganesh Shankar Vidyarthi Memorial Medical College, Kanpur, and postgraduated (in Anaesthesiology) from King George Medical University, Lucknow. Presently, he works as Assistant Professor in Department of Anaesthesiology in T. S. Mishra Medical College and Hospital, Lucknow. He works in all fields of anaesthesiology, but has special interest in obstetric anaesthesia.
Compliance with Ethical Standards
Conflict of interest
Dr. Monica Kohli, Dr. Anita Malik, Dr. Megha Kohli, Dr. Jaishri Bogra, Dr. Haider Abbas, Dr. Rajni Gupta, Dr. B. B. Kushwaha declare that they have no conflict of interest.
Ethical Approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national).
Footnotes
Dr. Asrar Ahmad M.D. (Anesthesiology), Assistant Professor, T. S. Mishra Medical College and Hospital; Prof. Monica Kohli M.D. (Anesthesiology), PDCC, Professor, King George’s Medical University; Prof. Anita Malik M.D. (Anesthesiology), Professor, King George’s Medical University; Dr. Megha Kohli, Junior Resident 3 (Anesthesiology and Intensive Care), Maulana Azad Medical College; Prof. Jaishri Bogra D.A., M.D. (Anesthesiology), Professor, King George’s Medical University; Prof. Haider Abbas M.D. (Anesthesiology), Professor, King George’s Medical University; Prof. Rajni Gupta M.D. (Anesthesiology), Professor, King George’s Medical University; Dr. B. B. Kushwaha M.D. (Anesthesiology), Associate Professor, King George’s Medical University.
References
- 1.Orlikowski CEP, Rocke DA, Murray WB, et al. Thromboelastography changes in pre-eclampsia and eclampsia. Br J Anaesth. 1996;77:157–161. doi: 10.1093/bja/77.2.157. [DOI] [PubMed] [Google Scholar]
- 2.Cunningham FG, Prichard JA. Hematologic considerations of pregnancy induced hypertension. Semin Perinatol. 1978;2:29–38. [PubMed] [Google Scholar]
- 3.Hartert H. Blutgerinnung studien mit der thromboelastographie, einen Neuen Untersuchingsverfahen. Klin Wochenschr. 1948;1948(26):577–583. doi: 10.1007/BF01697545. [DOI] [PubMed] [Google Scholar]
- 4.Mallett SV, Cox DJA. Thrombelastography. Br J Anaesth. 1992;69:307–313. doi: 10.1093/bja/69.3.307. [DOI] [PubMed] [Google Scholar]
- 5.Wong CA, Liu S, Glassenberg R. Comparison of thromboelastography with common coagulation tests in preeclampsia and healthy parturients. Reg Anesth. 1995;20:521–527. [PubMed] [Google Scholar]
- 6.Vandermeulen EP, Van Aken H, Vermylen J. Anticoagulants and spinal-epidural anesthesia. Anesth Analg. 1994;79:1165–1177. doi: 10.1213/00000539-199412000-00024. [DOI] [PubMed] [Google Scholar]
- 7.Voulgatopoulos DS, Palmer CM. Coagulation studies in the preeclamptic parturient: a survey. J Clin Anesth Analg. 1994;79:1165–1177. doi: 10.1016/0952-8180(93)90134-z. [DOI] [PubMed] [Google Scholar]
- 8.Leduc L, Wheeler JM, Kirshon B, et al. Coagulation profile in severe preeclampsia. Obstet Gynecol. 1992;79:14–18. [PubMed] [Google Scholar]
- 9.Othman M, Falcon BJ, Kadir R. Global hemostasis in pregnancy: are we using thromboelastography to its full potential ? Epub. 2010;36(7):738–748. doi: 10.1055/s-0030-1265290. [DOI] [PubMed] [Google Scholar]
- 10.Narani KK. Thromboelastography in the perioperative period. Indian J Anaesth. 2005;49(2):89–95. [Google Scholar]
- 11.Zuckerman L, Cohen E, Vagher JP, et al. Comparison of thromboelastography with common coagulation tests. Thromb Haemost. 1981;46:752–756. [PubMed] [Google Scholar]
- 12.Sharma S, Dadarkar P, Philip J, et al. Assessment of whole blood coagulation using modified thromboelastography in women with severe preeclampsia, Dept of Anesthesiology and pain mgmt, Southwestern Medical Center, Dallas, Texas; 2002, A-1056.
- 13.White H, Zollinger C, Jones M, et al. Can Thromboelastography performed on kaolin-activated citrated samples from critically ill patients provide stable and consistent parameters. Int J Lab Hematol. 2010;32(2):167–173. doi: 10.1111/j.1751-553X.2009.01152.x. [DOI] [PubMed] [Google Scholar]