VOLUME 284 (2009) PAGES 11309–11317
In this article, we provided immunological, histological, and physiological evidence that hyaluronan mediates the development of inflammation and airway hyperresponsiveness (AHR) after ozone inhalation (1). After publication of our article, we became aware that the airway physiology measurements reported in Figs. 5, 6, and 9 of the original manuscript, which were provided by the animal pulmonary physiology laboratory at Duke University, may have been unreliable.
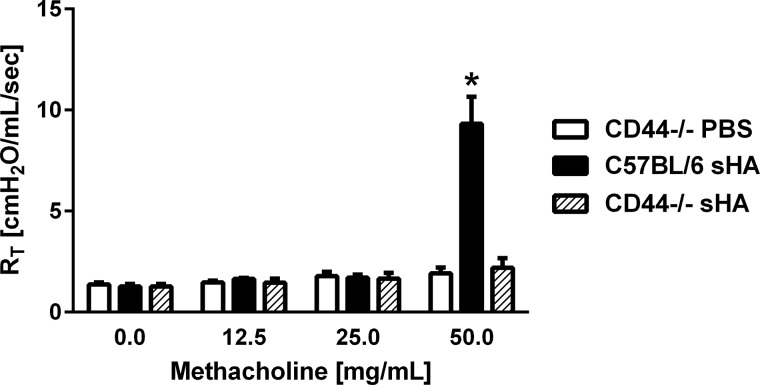
FIGURE 5.
(replication of original Fig. 9C). CD44-deficient mice are resistant to sHA-induced AHR compared with C57BL/5 mice (n = 4–8 mice per group; p < 0.05, sHA-treated C57 versus sHA-treated CD44−/−).
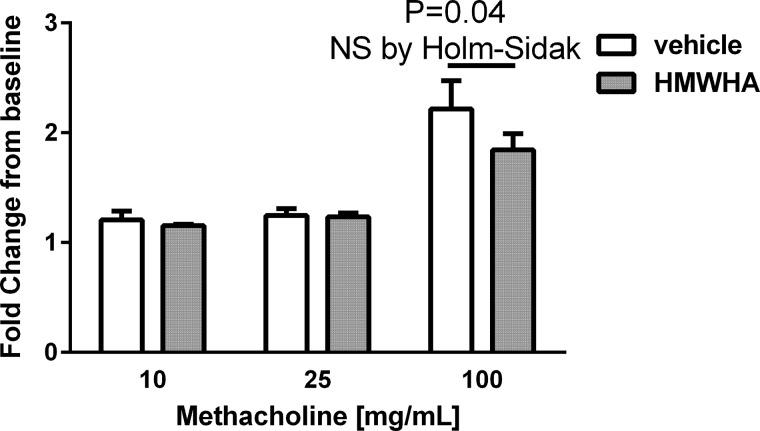
FIGURE 6.
(replication of original Fig. 9D). Instillation of HMW-HA before and after ozone exposure does not significantly ameliorate AHR, although a trend is observed (n = 9–10 mice per group).
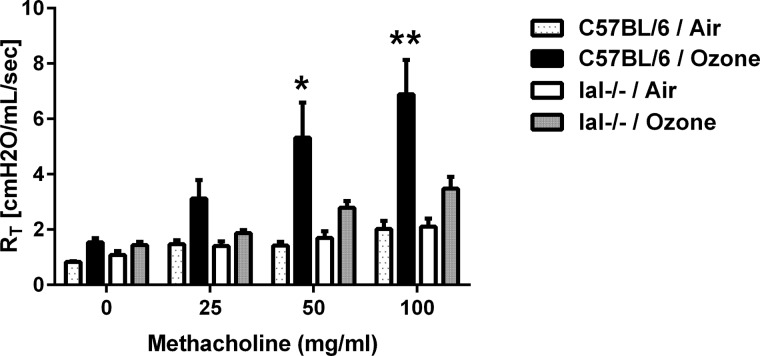
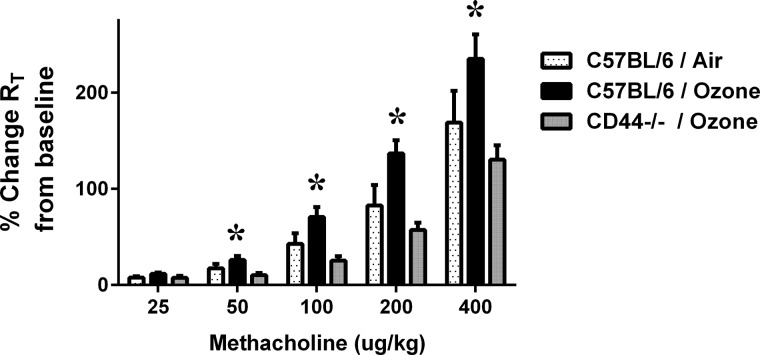
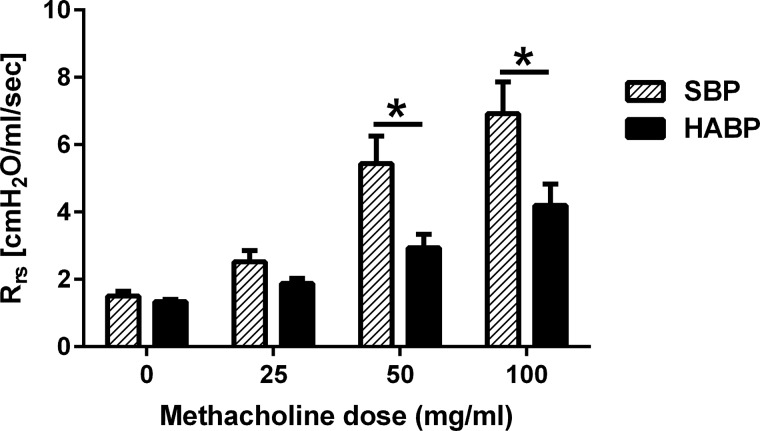
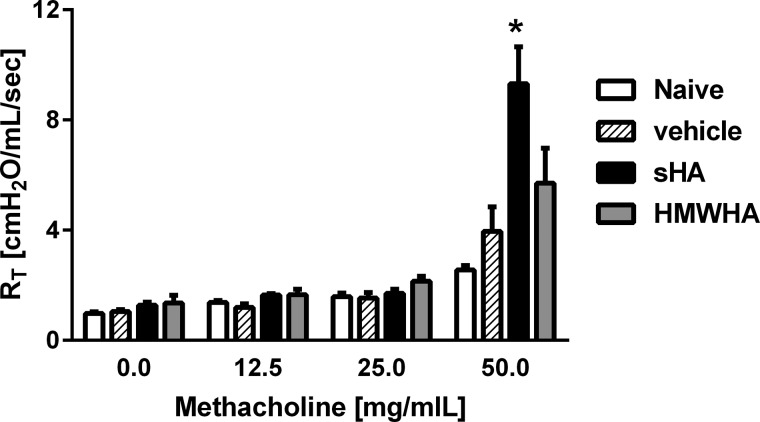
We therefore had two separate laboratories, one at Duke University under the supervision of Dr. Herman Staats, and the other at the National Institute of Environmental Health Sciences under the supervision of Dr. Stavros Garantziotis, repeat the experiments in question. These laboratories have replicated the key observation that hyaluronan mediates ozone-induced airway hyperresponsiveness. We again demonstrated that CD44 and inter-α-inhibitor (IαI) are necessary for the development of ozone-induced AHR (Figs. 1 and 2, n = 5–10 per group; p < 0.05). Furthermore, we confirmed that hyaluronan-binding protein (HABP) decreases AHR after ozone exposure (Fig. 3, n = 4–5 per group; p < 0.05). We showed that short fragment hyaluronan (sHA; molecular mass of 100–400 kDa) but not vehicle or high molecular weight hyaluronan (HMW-HA; molecular mass > 1,000 kDa) induces AHR in naïve C57BL/6 mice (Fig. 4, n = 4–6 mice per group; p < 0.05), but not in CD44-deficient mice (Fig. 5, n = 4–8 mice per group; p < 0.05). We were unable to confirm that HMW-HA ameliorates ozone-induced AHR, although there was a trend to that direction (Fig. 6, n = 8–10 mice per group; p = 0.04 but not significant by Holm-Sidak analysis and α = 5%).
FIGURE 1.
(replication of original Fig. 5A). IαI is essential for the development of ozone-induced airway hyperresponsiveness (n = 7–8 per group). *, p < 0.05; **, p < 0.01 compared to IaI−/− ozone.
FIGURE 2.
(replication of original Fig. 5A). CD44 is essential for the development of ozone-induced airway hyperresponsiveness (n = 5–10 per group). *, p < 0.05 compared to CD44−/− ozone.
FIGURE 3.
(replication of original Fig. 6C). Hyaluronan-binding protein (HABP), but not scrambled protein (SBP), significantly decreased AHR after ozone exposure (n = 4–5 per group). *, p < 0.05.
FIGURE 4.
(replication of original Fig. 9A). sHA but not HMW-HA or vehicle induces AHR in naïve C57BL/6 mice (n = 4–6 mice per group; p < 0.05 sHA versus HMW-HA).
In conclusion, we report that the repeated work largely validates the originally reported findings. Of note, the major conclusion of this article, i.e., that sHA mediates AHR after oxidative lung injury, has been independently validated in studies performed since this publication. For example, sHA mediates AHR after chlorine gas exposure, whereas HMW-HA or IαI blockade inhibits chlorine-induced AHR (2). Furthermore, exposure to ozone has been independently shown to result in increased levels of hyaluronan in the bronchoalveolar lavage fluid of mice (3) and humans (4, 5). Exposure to ozone was independently shown to fragment hyaluronan from HMW-HA to sHA (6). Furthermore, studies of murine asthma show that TSG-6, which links hyaluronan to IαI, is necessary for the development of inflammatory AHR (7). Finally, CD44 is necessary for the development of sHA-induced AHR in a tracheal ring model (2). Together, these studies support that several models of pulmonary inflammation result in increased levels of sHA, which mediates AHR.
In aggregate, our repeated studies confirm the original conclusions of the manuscript, and independent research also supports our originally reported conclusions. We therefore believe that our original report is accurate and valid.
References
- 1. Garantziotis S., Li Z., Potts E. N., Kimata K., Zhuo L., Morgan D. L., Savani R. C., Noble P. W., Foster W. M., Schwartz D. A., and Hollingsworth J. W. (2009) Hyaluronan mediates ozone-induced airway hyperresponsiveness in mice. J. Biol. Chem. 284, 11309–11317 [DOI] [PMC free article] [PubMed] [Google Scholar] [Research Misconduct Found]
- 2. Lazrak A., Creighton J., Yu Z., Komarova S., Doran S. F., Aggarwal S., Emala C. W. Sr., Stober V. P., Trempus C. S., Garantziotis S., and Matalon S. (2015) Hyaluronan mediates airway hyperresponsiveness in oxidative lung injury. Am. J. Physiol. Lung Cell. Mol. Physiol. 308, L891–L903 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Williams A. S., Mathews J. A., Kasahara D. I., Wurmbrand A. P., Chen L., and Shore S. A. (2015) Innate and ozone-induced airway hyperresponsiveness in obese mice: role of TNF-α. Am. J. Physiol. Lung Cell. Mol. Physiol. 308, L1168–L1177 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Bauer R. N., Müller L., Brighton L. E., Duncan K. E., and Jaspers I. (2015) Interaction with epithelial cells modifies airway macrophage response to ozone. Am. J. Respir. Cell Mol. Biol. 52, 285–294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hernandez M. L., Lay J. C., Harris B., Esther C. R. Jr., Brickey W. J., Bromberg P. A., Diaz-Sanchez D., Devlin R. B., Kleeberger S. R., Alexis N. E., and Peden D. B. (2010) Atopic asthmatic subjects but not atopic subjects without asthma have enhanced inflammatory response to ozone. J. Allergy Clin. Immunol. 126, 537–544.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wu Y. (2012) Preparation of low-molecular-weight hyaluronic acid by ozone treatment. Carbohydr. Polym. 89, 709–712 [DOI] [PubMed] [Google Scholar]
- 7. Swaidani S., Cheng G., Lauer M. E., Sharma M., Mikecz K., Hascall V. C., and Aronica M. A. (2013) TSG-6 protein is crucial for the development of pulmonary hyaluronan deposition, eosinophilia, and airway hyperresponsiveness in a murine model of asthma. J. Biol. Chem. 288, 412–422 [DOI] [PMC free article] [PubMed] [Google Scholar]