Abstract
A 72-year-old male is diagnosed with paradoxical embolus after he presented with concurrent deep vein thrombosis, stroke, and multiple arterial emboli in the presence of a patent foramen ovale (PFO). Paradoxical embolus requires the passage of a thrombus from the venous into the arterial circulation through a right-to-left shunt leading to systemic embolism. But, despite the high incidence of PFO (27.3% across all age groups by autopsy), paradoxical embolism (PDE) is uncommon, representing <2% of all arterial emboli. We present a case report where a thrombus has been directly observed passing through the PFO during an echocardiogram study; thus, clearly delineating the true cause of multiple thromboemboli and stoke in our patient. Subsequent Transesophageal Echocardiography (TEE) also interestingly showed the thrombus in transit in the aorta and pulmonary artery.
Keywords: paradoxical embolism, patent foramen Ovale, transesophageal echocardiogram, tissue plasminogen activator, deep venous Thrombosis
Paradoxical embolism (PDE) was first described by Julius Friedrich Cohnhein (1839–1884), a student of Virchow and Traube, who rose to become the Professor of Pathology and Pathologic Anatomy at the Universities of Leipzig and Breslau. In 1877, while performing an autopsy of a 35-year-old woman, he noticed the simultaneous presence of a thrombus in the lower extremity vein, a clot in the middle meningeal artery, and the presence of a patent foramen ovale (PFO). Thus, he first contemplated an astounding but undeniable connection between these three phenomena and coined the phrase paradoxical embolism to describe the possible pathophysiology (1).
Diagnosis of PDE is made based on the following criteria: 1) presence of a systemic arterial embolism, 2) detection of a thrombus in the venous circulation, 3) a communication between the right and left heart, and 4) a thrombus traversing such a communication or evidence of reversal of the intracardiac flow (2). Presence of an arterial or venous embolism is rather easily demonstrated; however, even though PFOs represent the majority of all right-to-left shunts (70%), the visualization of a thrombus through this shunt continues to evade most diagnosis (3). This is due to the fact that direct evidence of a PDE can only be obtained by the detection by echocardiography of a thrombus crossing the inter-atrial communication (4, 5). As timing and technician proficiency are the most important factors, in most cases, a presumptive diagnosis of PDE is made rather than a definitive one (2).
Case presentation
A 72-year-old male with a past medical history of coronary artery disease, hypertension, and diabetes was brought to the emergency department by his daughter for acute onset of left-sided weakness, confusion, and speech changes. The patient was initially evaluated in emergency room and was found to have a large acute right Middle Cerebral Artery (MCA) stroke with a small area of hemorrhagic infarct (5 mm) in the right frontal area on imaging. The patient did not receive tissue Plasminogen Activator (TPA) due to hemorrhagic conversion of stroke. Electrocardiogram showed normal sinus rhythm with left ventricular hypertrophy. Computed tomography of the head without contrast showed large evolving infarct in the right middle cerebral artery distribution with punctate focus of hemorrhagic transformation resulting in mildly increased mass effect together with evolving infarct in the left occipital lobe involving the left posterior cerebral artery distribution. Also, present were chronic infarcts in the bilateral thalami and cerebellar hemispheres. Magnetic resonant imaging of the head confirmed the same findings. A surface echocardiogram was done showing long mobile mass representing a thrombus extending from the right atria via the patent foramen ovale to the left atrium and prolapsing into the left ventricle (Fig. 1).
Fig. 1.
Biventricular thrombus.
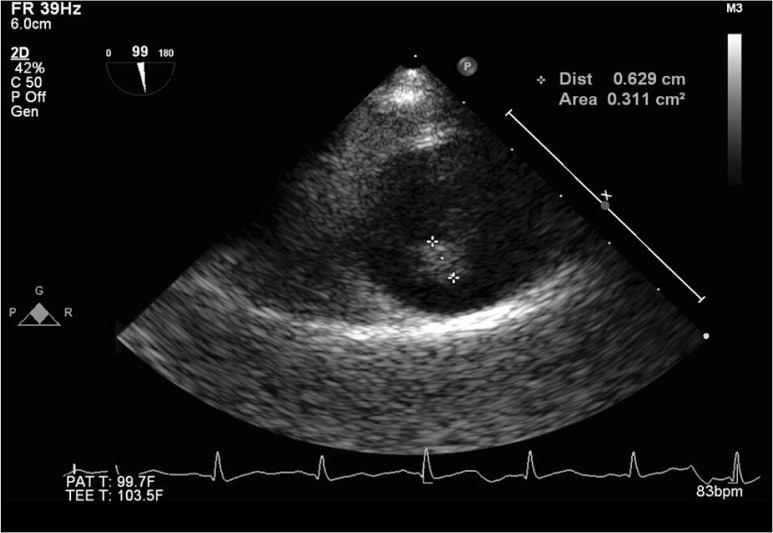
Transesophageal ECHO was done revealing large PFO with right-to-left shunt (Fig. 2).
Fig. 2.
Thrombus in patent foramen ovale (PFO).
Also, multiple mobile emboli were seen in the aortic arch (Fig. 3), and large emboli in transit were seen in the pulmonary artery as well (Fig. 4). Lower extremity arterial and venous Doppler demonstrated bilateral deep vein thrombosis (DVT) with acute left femoral artery occlusion as well. Patient was critically ill, and despite supportive care, he succumbed to the large thrombus burden affecting multiple organ systems and causing pulmonary embolism, major stroke, and acute limb ischemia.
Fig. 3.
Thrombus in descending aorta.
Fig. 4.
Thrombus in pulmonary artery.
Discussion
Paradoxical embolism is presumptive diagnosis from the presence of DVT, embolic phenomenon and PFO but it is rarely visualized. But in our case, the capture of a thrombus in transit across a PFO by echocardiogram as well as a second echocardiogram demonstrating movement of the thrombi confirms paradoxical embolism. Although paradoxical embolism most commonly causes stroke, it can also involve the other arterial circulation in the body as in our patient who had femoral arterial embolism causing acute limb ischemia.
Given the high morbidity and mortality associated with frank evidence of embolus in PFO, urgent anti-coagulation, thrombolysis, and/or embolectomy is required. Unfortunately, anti-coagulation or thrombolysis was contraindicated in our patient as he had cerebral hemorrhage and he ultimately succumbed to the sequelae of thromboembolism. Our case demonstrates a rare situation of a harrowingly large thrombus burden visualized on the transesophageal echocardiogram.
Conflicts of interest and funding
The authors have no conflicts of interest to declare.
References
- 1.Lippmann H, Rafferty T. Patent foramen ovale and paradoxical embolization: A historical perspective. Yale J Biol Med. 1993;66(1):11–17. [PMC free article] [PubMed] [Google Scholar]
- 2.Delvigne M, Vermeersch P, van den Heuvel P. Thrombus-in-transit causing paradoxical embolism in cerebral and coronary arterial circulation. Acta Cardiol. 2004;59(6):669–72. doi: 10.2143/AC.59.6.2182837. [DOI] [PubMed] [Google Scholar]
- 3.Cardim N, Toste J, Carvalho V, Nunes I, Ferreira D, Carmelo V, et al. Playing games with a thrombus: A dangerous match. Paradoxical embolism from a huge central venous catheter thrombus: A case report. Cardiovasc Ultrasound. 2010;8:6. doi: 10.1186/1476-7120-8-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kouskov OS, Nichols DJ, O'Hearn DJ. Paradoxical arterial embolism involving both upper extremities in a patient with pulmonary embolism and a patent foramen ovale. Clin Appl Thomb Hemost. 2011;17(6):E98–101. doi: 10.1177/1076029610387123. [DOI] [PubMed] [Google Scholar]
- 5.Forkmann M, Tugtekin SM, Strasser RH, Schrotter H. Impending paradoxical thromboembolism: Thrombus caught in transit. A case report. Clin Res Cardiol. 2012;101:497–8. doi: 10.1007/s00392-012-0418-4. [DOI] [PubMed] [Google Scholar]