Abstract
CD147/EMMPRIN (extracellular matrix metalloproteinase inducer) plays an important role in tumor progression and a number of studies have suggested that it is an indicator of tumor prognosis. This current meta-analysis systematically reevaluated the predictive potential of CD147/EMMPRIN in various cancers. We searched PubMed and Embase databases to screen the literature. Fixed-effect and random-effect meta-analytical techniques were used to correlate CD147 expression with outcome measures. A total of 53 studies that included 68 datasets were eligible for inclusion in the final analysis. We found a significant association between CD147/EMMPRIN overexpression and adverse tumor outcomes, such as overall survival, disease-specific survival, progression-free survival, metastasis-free survival or recurrence-free survival, irrespective of the model analysis. In addition, CD147/EMMPRIN overexpression predicted a high risk for chemotherapy drugs resistance. CD147/EMMPRIN is a central player in tumor progression and predicts a poor prognosis, including in patients who have received chemo-radiotherapy. Our results provide the evidence that CD147/EMMPRIN could be a potential therapeutic target for cancers.
The incidence of various cancers has been increasing and cancer is the most deadly disease threatening human life. One of the main causes of deaths is the inherent metastatic property of malignant tumors. This poses great difficulty in developing clinical therapeutics. The multi-linked pathological processes of tumor metastasis include: basement membrane degradation, matrix permeability, forward movement of tumor cells including secondary growth, and interaction between tumor cells and host stromal cells. CD147/EMMPRIN, also known as basigin or M6 antigen, has been shown to play an important role in tumor metastasis by stimulating tumor stromal cells to produce matrix metalloproteinases (MMPs) and degrading basement membrane and stroma1.
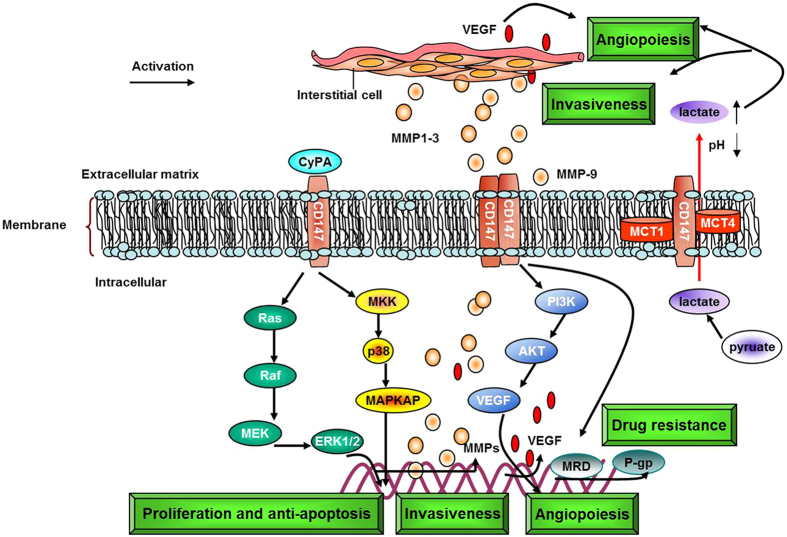
CD147/EMMPRIN is a member of the immunoglobulin family and is widely expressed in a variety of human tissues and cells1. CD147/EMMPRIN functions to: (1) facilitate secretion of MMP-1, MMP-3, MMP-9 and membrane-type 1-MMP from cancer cells, fibroblasts and endometrial cells, leading to degradation of basement membrane and extracellular matrix, thus promoting tumor proliferation, invasion and metastasis1,2; (2) drive tumor angiogenesis by enhancing MMPs and vascular endothelia growth factor (VEGF) levels in cancer cells and the mesenchyme3; (3) regulate expression and activity of monocarboxylate transporters-1 (MCT-1) and MCT-4, and form complexes on the membrane to transport lactic acid produced by anaerobic glycolysis4; (4) develop chemoresistance in many cancers, probably by mediating activation of phosphatidylinositol 3-hydroxy kinase (PI3K) and mitogen-activated protein kinase (MAPK) pathways5,6,7,8; and (5) interact with α3β1, α6β1 integrins to regulate adhesion with extracellular matrix proteins, collagen, laminin or fibronectin and also promote expression of cyclophilin A to induce cancer cell proliferation9. All of these functions are regulated by CD147/EMMPRIN and are summarized in Fig. 1. The outcomes of many of the pathways regulated by CD147 have been associated with the adverse outcomes highlighted in our study.
Figure 1.
It is highly upregulated in several malignant tumors10,11,12,13,14,15,16,17. A few recent studies10,15,16,17 have revealed a conflicting correlation between CD147/EMMPRIN and various outcomes in different cancers. A meta-analysis of the literature published previously suggests that elevated MCT-4 and CD147 expressions are associated with worse prognosis across many cancer types focusing on the aspect of tumor metabolism while the existing evidence lacks statistical power to draw a convincing conclusion18. The objective of this updated study was to systematically assemble all the existing CD147 literature, link the data to variable outcomes, perform a comprehensive meta-analysis to predict potential prognostic effects in different cancers, and provide further evidence to establish CD147/EMMPRIN as a key player in tumor progression from a number of perspectives.
Results
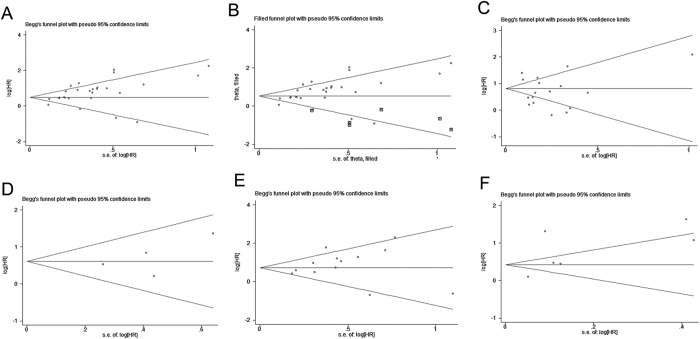
Our systematic literature search of CD147 and its correlation with different outcomes identified 910 articles. Among these, 836 articles were excluded and only 82 studies satisfied the inclusion eligibility for the meta-analysis. Upon further review of the full text articles, eight additional articles from reference sources were included. An additional 29 studies were excluded due to the following reasons: two articles were reviews; three were duplicate reports; four had insufficient data; four included only a few cases; nine explored the prognostic value of CD147/EMMPRIN in combination with other biomarkers, such as VEGF, MMP-2, CD44s, MCT-1; and seven studies were determined to be too complicated for subgroup analysis. The remaining 53 studies5,6,7,9,10,11,12,13,14,15,16,17,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59 containing 68 datasets that met our inclusion criteria were included in this review (Fig. 2). Among the eligible studies, 33 provided survival information about the correlation of CD147/EMMPRIN expression with tumor prognosis using a multivariate model and 20 presented the same information using a univariate model. The characteristics of these two models are summarized in Tables 1 and 2, respectively.
Figure 2.
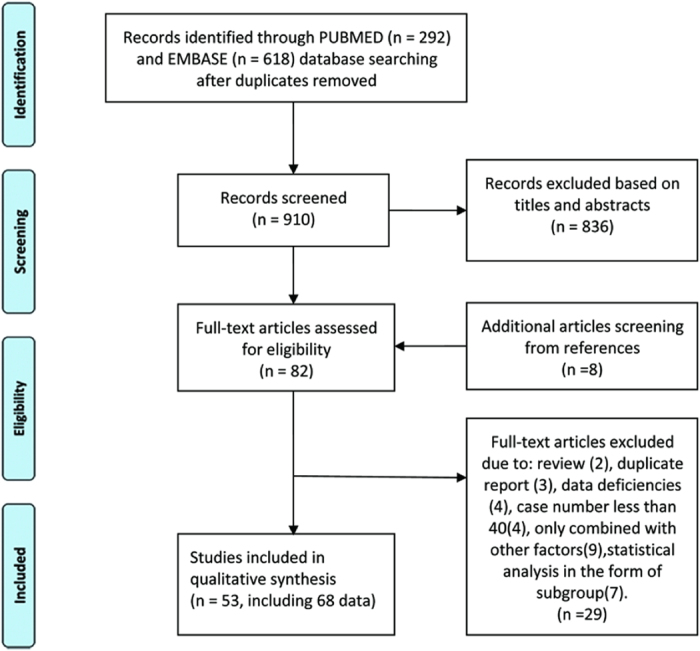
Table 1. Characteristics of studies exploring the relationship between CD147/EMMPRIN expression and tumor prognosis (Multivariate model).
| Author | Year | Country | Cancer type | Stage/grade | Number Median (range) | Age | Follow-up time Median (range) | Detection method | Cut-off | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|
| Natalie Reimers-10 | 2004 | Germany | Breast carcinoma | pT1-pT4 | 600 | >50y | 63m (1–176m) | TMA/IHC | score ≥ 1 | DSS |
| HC Zheng-19 | 2006 | Japan | Gastric carcinoma | 0–IV | 219 | 66.8y (38–88y) | 40.4m (0.2m–12.2y) | TMA/IHC | ≥5% | OS |
| Kazu Ueda-20 | 2006 | Japan | Endometrial carcinoma | I–IV | 112 | 55.3 ± 11.7 | NA | IHC | score > 2 | RFS |
| Qing Zhang-21 | 2007 | China | Hepatocellular carcinoma | I–IV | 111 | 47.47 ± 9.55 (24–66y) | 26m (30–1880d) | IHC | ≥1% | RFS |
| Anne B. Als-5 | 2007 | Denmark | Bladder Cancer | T4b, N2–3, M1 | 124 | 62.6y (31–78y) | 56.5 (19.5–129.8) m | IHC | κ values of 0.83 | OS |
| Wulf Sienel-22 | 2008 | Germany | Non-small-cell lung cancer | T1–T4 | 57 | 60y (37–80y) | 36 m (4–156) | IHC | score > 200 | OS |
| Xingzhu Ju-23 | 2008 | China | Cervical Cancer | Ib2–IIb | 75 | 49.7y (21–72y) | 52m (3–168m) | IHC | ≥1% | DSS |
| Yu Li-11 | 2009 | China | Breast carcinoma | infiltrating | 106 | NA | 63.5m (7–170) | TMA/IHC | ≥30% | RFS |
| Fangfang Liu-12 | 2010 | China | Breast carcinoma | Invasive | 186 | 52.5y (23–85y) | 64.8m (7–170m) | IHC | ≥1% | OS, PFS |
| Xinjie Yang-24 | 2010 | China | Adenoid cystic carcinoma of salivary glands | I–IV | 72 | NA | 76.76 ± 37.47 m; (9–178 m) | IHC | ≥5% | OS |
| Wei-De Zhong-25 | 2010 | China | Bladder cancer | T1–T4 | 101 | 68.1y (46–82y) | 36m | IHC | ≥5% | OS, PFS |
| Tongwei Chu-26 | 2011 | China | Pediatric Medulloblastoma | M0–M4 (Metastatic stage) | 56 | Paediatric patients | 5–y | IHC | ≥5% | OS |
| Yijun Xue-27 | 2011 | China | Bladder cancer | pT1–pT4 | 108 | 58.3y (31–82y) | 35.5 m (3–86m) | TMA/IHC | ≥1% | OS |
| Shaojun Zhu-28 | 2011 | China | Esophageal Squamous Cell Carcinoma | NA | 86 | 40–78y | 4–6 y | IHC | ≥5% | OS |
| Weide Zhong-29 | 2011 | China | Prostate cancer | pT2–pT3 | 240 | 61.81 ± 6.54y/61.94 ± 5.83y | NA | TMA/IHC | ≥5% | MFS, OS |
| Xuecheng Bi-30 | 2012 | China | Human seminomas | pT1–pT4 | 65 | 21.66 ± 10.18y | 5 y | IHC | ≥5% | OS |
| K Boye-31 | 2012 | Norway | Colorectal cancer | I–III | 242 | 70y (21–98 y) | 9.1y (8.2–10.0y) | IHC | ≥5% | MFS, DSS, OS |
| Zhangxuan Shou-32 | 2012 | China | Gastric Cancer | I–IV | 436 | 64y (30–91y) | >5y | TMA/IHC | ≥5% | OS |
| Albrecht Stenzinger -33 | 2012 | Germany | Colorectal cancer | I–IV | 285 | 66.6y | NA | TMA/IHC | score > 6 | OS |
| Shuhua Zhao-13 | 2013 | China | Ovarian cancer | I–IV | 146 | 52.8y (26–79y) | 36m (7–82m) | IHC | score ≥ 4 | OS, PFS |
| Ying Liu-34 | 2013 | China | Breast cancer | I–III | 189 | NA | NA | IHC | ≥10% | OS |
| Anja Rabien-35 | 2013 | Germany | Renal cell carcinoma | pN0/M0 | 181 | 60y (21–86y) | 112m (0–194m) | TMA/IHC | score ≥ 1 | OS |
| Xiaoyan Xu-36 | 2013 | China | Non-small lung cancer | I–IV | 136 | 60y (35–82y) | 28m (1–87m) | IHC | ≥1% | OS |
| Min Yang-37 | 2013 | China | Glioblastoma | NA | 206 | 53.6y (14–78y) | 12.3 m (1–60 m) | IHC | score ≥ 1 | OS |
| Yang Zhao-14 | 2013 | China | Ovarian carcinomas | I–IV | 88 | 51.2y (20–81y) | 52m (1–103m) | TMA/IHC | score ≥ 1 | RFS, OS |
| Qiang Lu-17 | 2013 | China | Osteosarcoma | IIA–III | 55 | NA | 32m (8–72m) | IHC | ≥5% | OS |
| Dake Chu-38 | 2014 | China | Gastric cancer | T1–T4 | 223 | NA | 41.8m (DFS)/58.0m (OS) | IHC | ≥5% | OS, PFS |
| Qin Xu-39 | 2014 | China | Cervical carcinoma | Ia1–IIb | 110 | NA | NA | IHC | ≥10% | OS, PFS |
| Shu Zhao-40 | 2014 | China | Breast cancer | I–III | 127 | 49y (30–68y) | NA | IHC | ≥10% | OS, PFS |
| Naohisa Futamura-16 | 2014 | Japan | Osteosarcoma | IIA–IIB | 53 | 20y (4–57y) | 72m (8–200m) | IHC | score ≥ 1 | OS, DFS |
| Jian Gao-43 | 2014 | China | Ovarian cancer | I–IV | 92 | NA | NA | IHC | ≥5% | OS |
| Luís Silva Monteiro-15 | 2014 | Portugal | Oral squamous cell carcinomas | I–IV | 74 | 62.3 ± 15.3y (25–96y) | 36.45 ± 31.7m | TMA/IHC | score > 3 | CSS |
| Shaojun Zhu-41 | 2015 | China | Hepatocellular carcinoma | NA | 50 | 31–76y | 4y | IHC | ≥5% | OS |
Table 2. Characteristics of studies exploring the relationship between CD147/EMMPRIN expression and tumor prognosis (Univariate model) V.
| Author | Year | Country | Cancer type | Stage/grade | Number | Age Median (range) | Follow-up time Median (range) | Detection method | Cut-off | Outcome |
|---|---|---|---|---|---|---|---|---|---|---|
| Hai-Gang Li-42 | 2005 | China | Hepatocellular carcinoma | grade1–4 | 51 | 51 ± 11y (24–69y) | 26m (5–90m) | IHC | ≥10% | DFS |
| Wen-Chiuan Tsai -43 | 2006 | China | Renal cell carcinoma | I–IV | 100 | NA | 5–year | TMA/IHC | score > 130 | OS |
| Nobuyuki Hakuma-44 | 2007 | Japan | Non-Small Cell Lung Cancers | stage I | 95 | 62.8 ± 9.1 | 5–y | IHC | score > 3 | OS |
| Wen Chiuan Tsai-45 | 2007 | China | Pancreatobiliary adenocarcinoma | T4 | 70 | NA | 2–y | IHC | score > 100 | OS |
| Wei Wu-46 | 2008 | China | Gallbladder carcinoma | I–IV | 108 | 51.63 ± 10.08y (35–76y) | 5–9y | IHC | ≥5% | OS |
| Daniel Buergy-47 | 2009 | Germany | Colorectal Cancer | I–IV | 40 | NA | 30 months | IHC | ≥5% | DSS |
| Ziming Du-48 | 2009 | China | Nasopharyngeal carcinoma | I–IV | 157 | 46y (14–86y) | 5–y | TMA/IHC | ≥5% | OS |
| Zhaodong Han-49 | 2010 | China | Renal/Bladder/Prostate carcinoma | I–IV | 52/58/101 | 57.26 ± 11.2y | 1–5y | IHC | ≥5% | OS |
| H. Z. Zeng-7 | 2011 | China | Non-small-cell lung cancer | III/IV | 118 | NA | NA | IHC | ≥25% | OS |
| Congfa Huang-9 | 2012 | China | Tongue squamous cell carcinoma | I–IV | 80 | NA | 69m (2–106m) | IHC | ≥10% | OS |
| Larissa Sweeny-50 | 2012 | USA | Cutaneous Squamous Cell Carcinoma | III–IV | 56 | 72 ± 12 (42–91) | >2y | IHC | ≥25% | OS |
| Keiichiro Nakamura-51 | 2012 | Japan | Endometrial cancer | I–IV | 134 | 57.7y (28–85) | NA | IHC | ≥10% | DFS, OS |
| Mototaka Sato-52 | 2013 | Japan | Renal cell carcinoma | I–IV | 50 | 27–82 (62) | 52 (1–114 m) | IHC | score ≥ 1 | OS, PFS |
| Wen Chiuan Tsai-53 | 2013 | China | Astrocytomas | III–IV | 77 | NA | NA | GDS1962 database | 1,500 | OS |
| Qing Yang-54 | 2013 | China | Hypopharyngeal Squamous Cell Carcinoma | I–IV | 80 | 60.73y (42–78) | IHC | ≥P90 level | RFS | |
| Xinwen Zhong-55 | 2013 | China | Lung cancer | T1 | 180 | 60y (37–75y) | 60m (3–96m) | IHC | ≥25% | OS |
| Jung-Woo Choi-56 | 2014 | Korea | Urothelial carcinoma of the bladder | Ta–T4 | 360 | 69y (23–97y) | 36m | TMA/IHC | score > 16 | OS |
| Xin-Qiong Huang-57 | 2014 | China | Cervical squamous cell carcinoma | IB-IVA | 132 | 51y (28–80y) | 45m (2–85.5m) | IHC | ≥5% | PFS |
| Céline Pinheiro-58 | 2014 | Portugal | Soft tissue sarcomas | I–III | 84 | NA | NA | IHC | score ≥ 3 | OS |
| Younghye Kim-59 | 2015 | Korea | Clear cell renal cell carcinoma | I–IV | 180 | 25–83y (58y) | 40.7m (1–173) | TMA/IHC | score > 17 | PFS |
The 53 eligible studies represented 26 different carcinomas or sarcomas and a median number of 204.5 patients (range, 40–600). CD147/EMMPRIN expression in these studies was mainly detected by immunohistochemistry (IHC). One publication had three groups of subjects from different cancers and was therefore considered as three different studies49. Ten publications12,13,14,16,25,29,38,39,51,52 presented two different prognostic results, while one publication31 presented three prognostic results. Some studies also investigated the link between CD147/EMMPRIN and chemotherapy5,6,7 or radiation resistance57. In terms of clinicopathological variables, most of the studies suggested that increased CD147/EMMPRIN expression correlated significantly with higher clinical grade, tumor size, invasion depth, lymphatic invasion, histological grade, and some additional parameters (Table 3).
Table 3. Relationship between CD147/EMMPRIN overexpression and clinical and pathological factors.
| Author | Cancer type | Relative to other factors | Relative to clinicopathologic variables |
|---|---|---|---|
| Multivariate | |||
| Natalie Reimers-10 | Breast carcinoma | ER, PR (inversely) | High tumor grade, histologically determined mitotic index, tumor size, inversely correlated to age |
| HC Zheng-19 | Gastric carcinoma | ki-67, MMP-2, MMP-9, VEGF, MVD | Tumour size, depth of invasion, lymphatic invasion, not with lymph node metastasis, UICC staging or differentiation |
| Kazu Ueda-20 | Endometrial carcinoma | Advanced stage, poorly differentiated carcinoma, lymph node metastasis, lymphatic vessel infiltration, pathological high risk group | |
| Qing Zhang-21 | Hepatocellular carcinoma | MVD-CD34; MMP-2 in pericancerous, not in cancerous lesions; VEGF | pTNM tumor stages, tumor size and venous invasion, IV stage and large tumor size, preoperative AFP level; not: viral hepatitis, the number of tumor nodules, lymph node metastasis |
| Anne B. Als-5 | Bladder Cancer | Visceral metastases | |
| Wulf Sienel-22 | Non-small-cell lung cancer | MMP-2 (no), MMP-9 (no) | |
| Xingzhu Ju-23 | Cervical Cancer | Pelvic lymph node metastasis, no correlation with clinical stage and histopathology | |
| Yu Li-11 | Breast carcinoma | ||
| Fangfang Liu-12 | Breast carcinoma | C-erbB-2; ER, PR (inversely) | Histological grade, local recurrence, distant metastasis and tumor mortality |
| Xinjie Yang-24 | Adenoid cystic carcinoma of salivary glands | MMP-2, MMP-9, VEGF, Ki-67 index, MVD | Tumor size, histotypes, clinical stage, perneural invasion, vascular invasion, metastasis |
| Wei-De Zhong-25 | Bladder cancer | Tumor stage and grade, status of carcinoma in situ, tumor recurrence, tumor progression | |
| Tongwei Chu-26 | Pediatric Medulloblastoma | Higher metastatic stage, aggressive histopathological type, necrosis, undifferentiated tumor | |
| Yijun Xue-27 | Bladder cancer | Lymph node status, tumor stage, histologic grade | |
| Shaojun Zhu-28 | Esophageal Squamous Cell Carcinoma | Lymph node metastasis cases, differentiation, depth of tumor invasion | |
| Weide Zhong-29 | Prostate cancer | Gleason score, positive surgical margin status, reduced PSA failure-free survival | |
| Xuecheng Bi-30 | Human seminomas | MMP-2 | advanced T, N and M stage, poor differentiation types |
| K Boye-31 | Colorectal cancer | S100A4 | no associations with any of the clinical or histopathological parameters |
| Zhangxuan Shou-32 | Gastric Cancer | ADAM17 | Age, tumor size, location, depth of invasion, TNM stage, Lauren’s classification, vessel invasion, and lymph node and distant metastasis of tumor |
| Albrecht Stenzinger -33 | Colorectal cancer | Trend correlation with stage, distant metastasis, blood vessel invasion, and Dukes classification | |
| Shuhua Zhao-13 | Ovarian cancer | Lymph-vascular space involvement, lymph node metastasis | |
| Ying Liu-34 | Breast cancer | ||
| Anja Rabien-35 | Renal cell carcinoma | pT stage and Fuhrman grading | |
| Xiaoyan Xu-36 | Non-small lung cancer | Tumor diameter, lymph node status, tumor stage | |
| Min Yang-37 | Glioblastoma | Karnofsky performance status (KPS) score | |
| Yang Zhao-14 | Ovarian carcinomas | Ki-67 | FIGO staging, dedifferentiation |
| Qiang Lu-17 | Osteosarcoma | Pathological classification, percentage of dead cells | |
| Dake Chu-38 | Gastric cancer | Invasion, metastasis and TNM stage | |
| Qin Xu-39 | Cervical carcinoma | FIGO clinical stage, lymph node metastasis, parametrium invasion, and differentiation | |
| Shu Zhao-40 | Breast cancer | MMP-9, Ki67 | Lymph node metastasis, high pathological grade, tumor size larger than 2 cm |
| Naohisa Futamura-16 | Osteosarcoma | MT1-MMP | Not associated with age, gender, anatomic location, necrosis after neoadjuvant chemotherapy, or surgical stage |
| Jian Gao-43 | Ovarian cancer | Lewis y antigen | Drug-resistant |
| Luís Silva Monteiro-15 | Oral squamous cell carcinomas | Ki-67 | Advanced tumor stages, histological grade |
| Shaojun Zhu-41 | Hepatocellular carcinoma | No relationship between differentiation, HBV infection, significantly opposite to cirrhosis | |
| Univariate | |||
| Hai-Gang Li-42 | Hepatocellular carcinoma | paxillin and syndecan-1 (no) | Not associated with serum AFP level, HBsAg status, presence of microsatellite nodule, tumor size, presence of cirrhosis and necrosis, differentiation, presence of portal vein thrombosis and extra-hepatic metastasis |
| Wen-Chiuan Tsai -43 | Renal cell carcinoma | fascin | Histological grades and clinical stages |
| Nobuyuki Hakuma-44 | Non-Small Cell Lung Cancers | Well differentiated, not associated with any of the following variables: age, gender, histology, pT or pN classification, and pathological stage | |
| Wen Chiuan Tsai-45 | Pancreatobiliary adenocarcinoma | fascin | Histologic grades and clinical stages |
| Wei Wu-46 | Gallbladder carcinoma | MMP-2 | Nevin stages of tumor tissues, histological differentiated degree, distant metastasis |
| Daniel Buergy-47 | Colorectal Cancer | pT or pN status, metastasis | |
| Ziming Du-48 | Nasopharyngeal carcinoma | Cav-1 | Metastasis of the disease |
| Zhaodong Han-49 | Renal/Bladder/Prostate carcinoma | TNM stages, histological subtypes | |
| H. Z. Zeng-7 | Non-small-cell lung cancer | No association (overall CD147); (membranous CD147) associated with a poor response to chemotherapy | |
| Congfa Huang-9 | Tongue squamous cell carcinoma | HIF-1a, VEGF-A, VEGF-C, CypA | Recurrence and node metastasis |
| Larissa Sweeny-50 | Cutaneous Squamous Cell Carcinoma | Node positive disease | |
| Keiichiro Nakamura-51 | Endometrial cancer | FIGO stage, histology, depth of myometrial invasion, cervical involvement, lymph node metastasis, lymph vascular space involvement, peritoneal cytology | |
| Mototaka Sato-52 | Renal cell carcinoma | anti-CD34 | Pathological T stage, clinical M stage, AJCC stage, Fuhrman grade, microvessel area of immature vessels |
| Wen Chiuan Tsai-53 | Astrocytomas | WHO grades | |
| Qing Yang-54 | Hypopharyngeal Squamous Cell Carcinoma | CD44v6; COX-2 | T classification, lymph node metastasis and clinical stage |
| Xinwen Zhong-55 | Lung cancer | RACK1 | Differentiation, Lymph node metastasis |
| Jung-Woo Choi-56 | Urothelial carcinoma of the bladder | MCT1, MCT4 | High World Health Organization grade, advanced tumor node metastatis stage, and nonpapillary growth type |
| Xin-Qiong Huang-57 | Cervical squamous cell carcinoma | GLUT-1 | Histopathological grade, Tumor diameter, radiation-resistant |
| Céline Pinheiro-58 | Soft tissue sarcomas | MCT1, MCT4 | Disease progression |
| Younghye Kim-59 | Clear cell renal cell carcinoma | High grade, tumor necrosis, larger tumor size | |
CD147/EMMPRIN and overall survival (OS)
The 44 studies, with data from a total of 5,813 patients, showed that CD147/EMMPRIN expression was associated with worse OS, both in multivariate (meta-hazard ratio (HR) = 1.92; 95% confidence interval (CI): 1.58–2.32) and in univariate models (meta-HR = 1.98; 95% CI: 1.53–2.57) (Table 4; Fig. 3A,B). In addition, separate analysis of solid and non-solid tumors suggested that the OS of solid tumors was significantly associated with CD147 in both multivariate (meta-HR = 1.73; 95% CI: 1.44–2.08) and univariate (meta-HR = 2.06; 95% CI: 1.57–2.70) models. In contrast, OS of non-solid tumors only displayed significant association in the multivariate model (meta-HR = 3.72; 95% CI: 2.23–6.22), while there was no significant association in the univariate model analysis (meta-HR = 1.34, 95% CI: 0.77–2.32) (Table 4).
Table 4. Meta-analysis of association between CD147/EMMPRIN expression and tumor prognosis.
| OS |
PFS |
DSS |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No/case | meta-HR (95CI%) P* | I2 (P#) | No/case | meta-HR (95CI%) P* | I% (P#) | No/case | meta-HR (95CI%) P* | I2 (P#) | ||||
| Multivariate | ||||||||||||
| Total | 27/3933 | 1.92 (1.58–2.32) 0.000 | 66.4 (0.000) | 13/1845 | 2.32 (1.67–3.21) 0.000 | 56.3 (0.007) | 4/991 | 1.83 (1.27–2.65) 0.001 | 0.00 (0.458) | |||
| Solid tumor | 23/3563 | 1.73 (1.44–2.08) 0.000 | 60.7 (0.000) | 12/1792 | 2.26 (1.61–3.18) 0.000 | 58.5 (0.005) | 4/991 | 1.83 (1.27–2.65) 0.001 | 0.00 (0.458) | |||
| Nun-solid tumor | 4/370 | 3.72 (2.23–6.22) 0.000 | 36.6 (0.192) | 1/53 | 3.52 (1.18–10.5) 0.024 | 0 | ||||||
| Breast carcinoma | 5/695 | 2.92 (1.85–4.60) 0.000 | 5.00 (0.378) | 3/419 | 2.50 (1.63–3.83) 0.000 | 0.00 (0.846) | ||||||
| Bladder cancer | 3/333 | 2.32 (1.63–3.29) 0.000 | 0.00 (0.860) | |||||||||
| Gastric carcinoma | 3/878 | 1.33 (0.99–1.80) 0.060 | 62.0 (0.072) | |||||||||
| Colorectal cancer | 2/527 | 2.14 (1.38–4.26) 0.035 | 77.9 (0.033) | |||||||||
| Ovarian cancer | 3/326 | 1.57 (1.23–2.01) 0.000 | 0.00 (0.982) | 2/234 | 1.72 (1.23–2.40) 0.002 | 0.00 (0.833) | ||||||
| Osteosarcoma | 2/108 | 7.83 (3.18–19.27) 0.000 | 0.00 (0.852) | |||||||||
| Total publish bias | 0.05 (Begg’ test) | 0.007 (Egger’ test) | 0.300 (Begg’ test) | 0.259 (Egger’ test) | 0.734 (Begg’ test) | 0.469 (Egger’ test) | ||||||
| Univariate | ||||||||||||
| Total | 17/1880 | 1.98 (1.53–2.57) 0.000 | 89.3 (0.000) | 6/627 | 2.18 (1.30–3.63) 0.003 | 96.7 (0.000) | 1/40 | 5.81 (4.16–7.46) 0.037 | ||||
| Solid tumor | 15/1719 | 2.06 (1.57–2.70) 0.000 | 90.4 (0.000) | 6/627 | 2.18 (1.30–3.63) 0.003 | 96.7 (0.000) | 1/40 | 5.81 (4.16–7.46) 0.037 | ||||
| Nun-solid tumor | 2/161 | 1.34 (0.77–2.32) 0.300 | 2.90 (0.310) | 0 | 0 | |||||||
| Renal cell carcinoma | 3/202 | 1.87 (1.37–2.56) 0.000 | 70.9 (0.032) | 2/230 | 1.58 (1.34–1.85) 0.000 | 0.00 (0.91) | ||||||
| Lung Cancer | 3/393 | 1.16 (0.63–2.12) 0.630 | 74.1 (0.021) | — | — | |||||||
| Bladder carcinoma | 2/418 | 2.51 (1.46–4.33) 0.001 | 81.9 (0.019) | — | — | |||||||
| Total publish bias | 0.773 (Begg’ test) | 0.228 (Egger’ test) | −0.707 (Begg’ test) | −0.304 (Egger’ test) | ||||||||
P* present P for HR, P# present P for I2.
Figure 3. Qualitative meta-analysis of the association between CD147/EMMPRIN over-expression and overall survival (OS) in cancer patients.
Panel A, represents the association of CD147/EMMPRIN positive expression with worse OS in multivariate model, while panel B, represents similar association by univariate model.
Furthermore, the subgroup analysis of tumors stratified by cancer type also demonstrated a significant association between higher CD147/EMMPRIN expression and adverse outcome of OS for breast carcinoma (meta-HR = 2.92; 95% CI: 1.85–4.60), bladder cancer (meta-HR = 2.32; 95% CI: 1.63–3.29), colorectal cancer (meta-HR = 2.14; 95% CI: 1.38–4.26), ovarian cancer (meta-HR = 1.57; 95% CI: 1.23–2.01) and osteosarcoma (meta-HR = 7.83; 95% CI: 3.18–19.27) in the multivariate model. However, an association was only observed in renal cell carcinoma (meta-HR = 1.87; 95% CI: 1.37–2.56) and bladder carcinoma (meta-HR = 2.51; 95% CI: 1.46–4.33), using the univariate model. In contrast, there was no association in gastric carcinoma (meta-HR = 1.33; 95% CI: 0.99–1.80) and lung cancer (meta-HR = 1.16; 95% CI: 0.63–2.12) (Table 4). We also found a similar association of CD147 with the adverse outcome (OS) in many other cancers, such as adenoid cystic carcinoma of salivary glands, esophageal squamous cell carcinoma, prostate cancer, pediatric medulloblastoma, glioblastoma, gallbladder carcinoma, nasopharyngeal carcinoma, tongue squamous cell carcinoma, endometrial cancer, uterine cervical carcinoma, hepatocellular carcinoma, pancreatobiliary adenocarcinoma, cutaneous squamous cell carcinoma, astrocytomas and soft tissue sarcomas (Supplementary Figure 1A,B).
CD147/EMMPRIN and progression free survival (PFS), metastasis-free survival (MFS) and recurrence-free survival (RFS)
Analysis of 19 studies, with a total of 2,472 patients, showed that CD147/EMMPRIN expression was associated with worse PFS/MFS/RFS, both in multivariate (meta-HR = 2.32; 95% CI: 1.67–3.21) and univariate (meta-HR = 2.18; 95% CI: 1.30–3.63) models (Table 3 and Fig. 4A,B). Moreover, the HR estimates derived specifically from the solid tumors by both models showed a similar pattern of association (multivariate: meta-HR = 2.26; 95% CI: 1.61–3.18; univariate: meta-HR = 2.18; 95% CI: 1.30–3.63). Exclusive analysis of non-solid tumors by a multivariate model suggested a significant association (meta-HR = 3.52; 95% CI: 1.18–10.5) (Table 4).
Figure 4. Qualitative meta-analysis of the association between CD147/EMMPRIN over-expression and PFS/MFS/RFS in cancer patients.
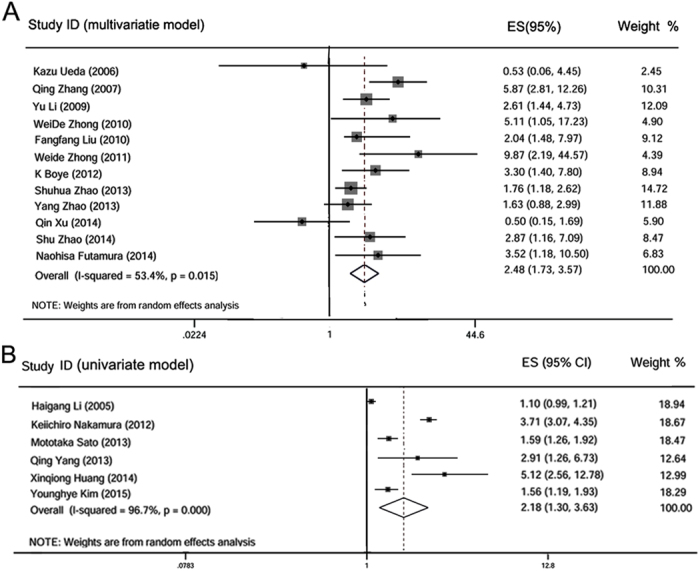
Panel (A) represents the overall association of CD147/EMMPRIN positive expression with worse PFS/MFS/RFS in multivariate model; panel (B) depicts similar association in univariate model.
Similarly, the subgroup analysis of tumors stratified by cancer type again demonstrated a significant association between CD147/EMMPRIN overexpression and adverse outcome of PFS/MFS/RFS in breast carcinoma (meta-HR = 2.50; 95% CI: 1.63–3.83) and ovarian cancer (meta-HR = 1.72; 95% CI: 1.23–2.40) in the multivariate model and renal cell carcinoma (meta-HR = 1.58; 95% CI: 1.34–1.85) in the univariate model. Similar associations were observed in hepatocellular carcinoma, bladder cancer, prostate cancer, colorectal cancer, osteosarcoma, gastric cancer and hypopharyngeal squamous cell carcinoma. However, we did not observe an association in cases of endometrial carcinoma, and the results were not consistent for cervical carcinoma (Supplementary Figure 2A,B).
CD147/EMMPRIN and disease-specific survival (DSS)
Quantitative analysis of five different studies, representing 1,031 patients, linked CD147/EMMPRIN overexpression with DSS in four different solid tumors, namely breast cancer2, colorectal cancer [24, 41], oral squamous cell carcinomas7 and cervical cancer16. Multivariate model analysis established that CD147/EMMPRIN expression was associated with a worse DSS (meta-HR = 1.83; 95% CI: 1.27–2.65) (Table 4; Fig. 5A). Similarly, univariate model analysis indicated that CD147 expression associated with worse DSS (meta-HR = 5.81; 95% CI: 4.16–7.46) (Table 4). This pattern was unchanged even in the subgroup analyses stratified by cancer type. Multivariate model analysis also identified the following associations with DSS: breast carcinoma (meta-HR = 1.70; 95% CI: 1.02–2.84), oral squamous cell carcinoma (meta-HR = 3.89; 95% CI: 1.11–13.71) and colorectal cancer (meta-HR = 2.30; 95% CI: 1.03–5.14). The only cancer for which we did not observe an association was uterine cervical carcinoma (meta-HR =1.23; 95% CI: 0.52–2.90) (Supplementary Figure 4).
Figure 5. Qualitative meta-analysis of the association between CD147/EMMPRIN over-expression and disease free survival (DSS) in cancer patients, and to predict easier recurrence of drug resistance.
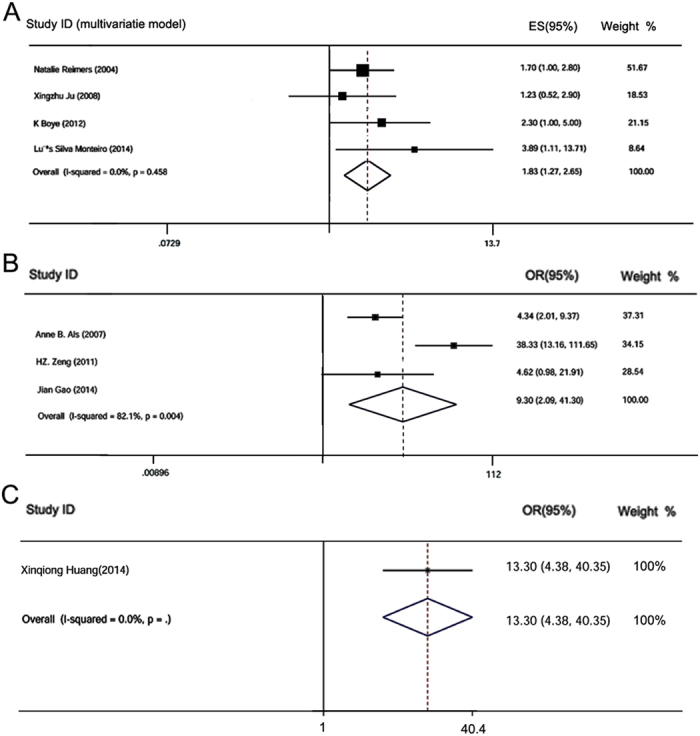
Panel A, represents the association of CD147/EMMPRIN positive expression with worse DSS in multivariate model. Panels B, represents the potential of CD147/EMMPRIN positive expression to predict easier recurrence of drug resistance.
CD147/EMMPRIN and chemotherapy drug/radiation resistance
Among the included articles, three studies5,6,7 reported risk for CD147/EMMPRIN overexpression and chemotherapy drug resistance, while only one study57 reported radiation resistance. Quantitative analysis of three articles revealed that positive expression of CD147/EMMPRIN predicted recurrence of drug resistance (meta-OR = 9.30; 95% CI: 2.09–41.30) (Fig. 5B). In addition, CD147/EMMPRIN overexpression appeared to be linked to high risk of radiation resistance (OR = 13.30; 95% CI: 4.38–40.35) in cervical squamous cell carcinomas, although this is just based on one study (Fig. 5C).
Heterogeneity analysis
There was evidence of significant heterogeneity (I2 > 50%) between OS and PFS studies, but not among DSS studies (Table 4). Therefore, the random-effect model was used in all analyses except for the DSS. For the OS and PFS studies, we conducted a meta-regression analysis using publication year, cancer type, sample size, and country as covariates. All covariates were entered into the meta-regression model simultaneously, and the covariates with the highest p values were omitted one at a time to identify sources of heterogeneity. The meta-regression did not identify any of these covariates as a significant source of heterogeneity for OS and PFS studies in multivariate, and indicated that cancer type may be the source of heterogeneity for OS studies in univariate analysis (Coef = 0.093, p = 0.042) (Supplementary Figure 4). Meta-regression was not used for univariate analysis of the PFS since these studies numbered less than 10.
Sensitivity analysis
We also performed a sensitivity analysis to evaluate the effects of individual studies on the pooled HR estimates by omitting one study at a time. The HR estimates for the DSS and PFS/MFS/RFS in the multivariate model were not altered. However, the HR estimates for the OS in the multivariate model, and OS and PFS/MFS/RFS in the univariate model were altered when one, one and two studies were excluded, respectively (data not shown).
Publication bias
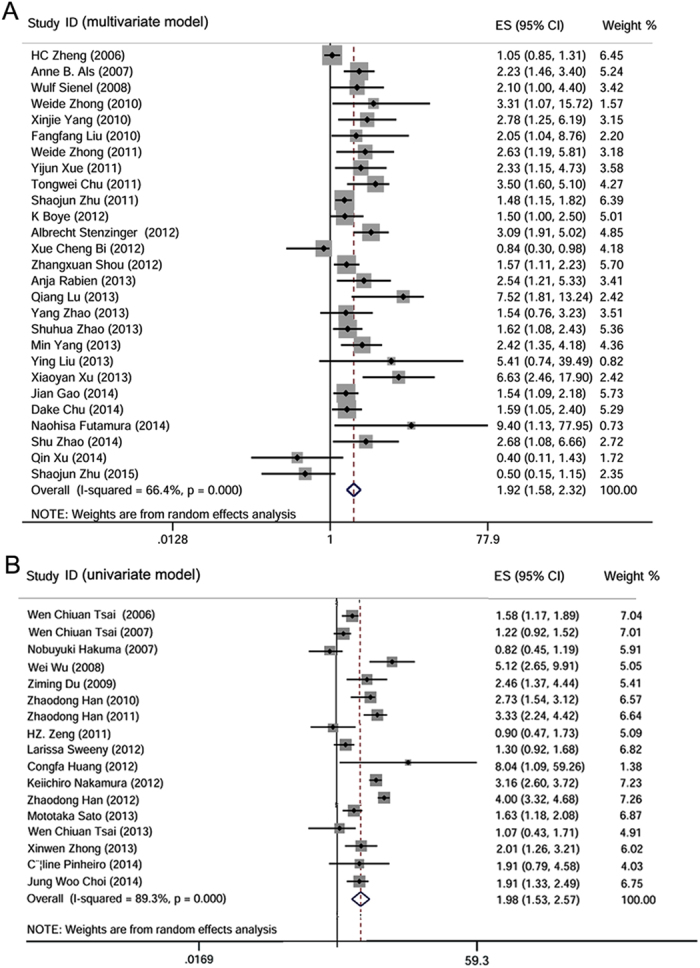
To assess confidence in our study, we performed a publication bias analysis using the funnel plot and Egger’s and Begg’s rank correlation tests. There was no significant publication bias in both models for the DSS and PFS/MFS/RFS groups (Table 4; Fig. 6D–F). In the case of the OS group, the univariate model (Table 4; Fig. 6C) suggested no publication bias, but in the multivariate model, results were inconsistent based on the p value obtained by Begg’s rank test (0.05) and Egger’s test (0.007) (Table 4; Fig. 6A). These test results were nonparametric and therefore the Trim and Fill method was used to further verify this analysis. After filling the deleted studies (square dots), we found no obvious asymmetry in the funnel plot (Fig. 6B). Thus, the HR estimates for the prognostic value of CD147/EMMPRIN were not notably altered (data not shown). This suggests that there was no publication bias even in the OS group in the multivariate model.
Figure 6. Assessment of publication bias for OS, DSS, and PFS/MFS/RFS studies.
Panel (A) depicts the assessment of publication bias for multivariate model studies, by funnel plot analysis, whereas panel (B) shows funnel plot analysis using nonparametric Trim and Fill method. Panel (C) represents the publication bias in univariate model studies. Panel (D) represents the assessment of publication bias for multivariate model. Panels (E,F) represents assessment of publication bias for multivariate and univariate model studies, respectively.
Discussion
CD147/EMMPRIN is a glycosylated, multifunctional molecule that participates in tumor progression61. In the present study, we quantitatively analyzed the data from 53 studies, including 68 datasets, to examine the associations between CD147/EMMPRIN expression and its prognosis predictive value in cancer. Previous studies have suggested that combination of CD147/EMMPRIN with other factors, especially VEGF60,62,63 and MMP-264,65,66, can predict the prognosis of some cancers. Here, we exclusively studied the role of CD147/EMMPRIN in tumor prognosis. Our meta-analysis revealed that the prognosis in three adverse outcomes was significantly poor in cases with CD147/EMMPRIN overexpression. This was further confirmed in subgroup analyses of tumors stratified by cancer type. Meanwhile, the predictive role of CD147/EMMPRIN in cervical cancer and hepatocellular carcinoma prognosis has been controversial and its result in cervical carcinoma, endometrial carcinoma, pancreatobiliary adenocarcinoma and some additional tumors did not consistently reach significance. However, the sample size and studies in our stratified analysis were small, and our findings should be further verified.
CD147/EMMPRIN has been shown to be involved in the regulation of tumor cell invasion, metastasis, angiogenesis, anti-apoptosis, adhesion and facilitation of drug resistance through its association with various proteins1, such as MMP-219, MMP-920, Ki-6714, VEGF19, microvessel density19, C-erbB-212, S100A431, a disintegrin and metalloproteinase 1732, lewis y antigen6, fascin43, caveolin-148, hypoxia inducible factor 1 alpha9, cyclophilin A9, CD44v654, cyclooxygenase-254, receptor for activated C kinase 155 and metabolism related factors like MCT-156, MCT-456, and glucose transporter -157. However, there is some conflicting literature refuting associations with paxillin42, syndecan-142, and MMP-2 and MMP-922. In addition, CD147 expression has been proposed to inversely correlate with estrogen and progesterone expression10,12. Furthermore, CD147/EMMPRIN was positively associated with clinicopathological variables in most studies (Table 3). It is speculated that CD147/EMMPRIN interacting with many proteins representing various molecular or biological pathways contributes to malignant progression, eventually causes adverse clinical outcomes.
Previous meta-analyses didn’t explore any significant association between CD147/EMMPRIN and susceptibility of radio-chemotherapy. In the view of more studies are warranted to validate CD147/EMMPRIN association with chemotherapy and radiation resistance prediction5,6,7,57. It has been suggested that chemotherapy drugs combined with CD147-targeted therapy may increase the sensitivity of tumor cells to several different chemotherapeutics, and can result in more effective inhibition of tumor proliferation and recurrence7,67. Our study also established that increased CD147/EMMPRIN expression is linked to high risk of drug resistance and our preliminary analysis linked CD147 to radiation resistance. It follows that CD147/EMMPRIN has been proposed to be an important potential therapeutic target.
The results of the present study must be interpreted with caution due to the presence of substantial heterogeneity. In addition, there were several limitations in this study. First, the composition of the cancer type or stage varied between studies, and the detection and corresponding cut-offs varied. For instance, some studies only included pediatric patients26 while others included older patients10. Also, in non-small-cell lung cancer, CD147/EMMPRIN was associated with poor survival in patients with adenocarcinoma only, but not with squamous cell carcinoma22. The scoring criteria were also inconsistent. Second, the follow-up time varied across studies, which may have contributed to the non-homogeneity of prognostic information. Sensitivity analysis results also showed instability within individual articles. Third, this study was based on published articles only and, since negative data are hard to publish, there could be publication bias, which is an inherent limitation of all meta-analyses, irrespective of outcomes from the Egger’s linear regression test and Begg’s rank correlation test.
Conclusion
In summary, this meta-analysis indicated that higher expression of CD147/EMMPRIN potentially may be a prognostic marker for most cancers, and thus can serve as a potential therapeutic target. We further verified that CD147/EMMPRIN had a complex role in tumor progression by crosstalk with numerous factors. However, additional multicenter prospective studies are warranted to confirm these findings, especially in various types of tumors.
Methods
Study identification
We searched PubMed and Embase databases through March 2015 to identify relevant studies for inclusion in our meta-analysis. The following keywords were used in the literature searches; “CD147”, “extracellular matrix metalloproteinase inducer”, “EMMPRIN”, “basigin”, “survival”, “prognosis”, “tumor”, “cancer”, “carcinoma”, “neoplasm”, or their combinations. Eligible articles were selected based on title, abstract and full text. If the same patient cohort was reported in multiple publications, only the most complete and most recent publication was selected. We also searched of the reference lists from electronically identified articles.
Inclusion and exclusion criteria
Based on the Reporting Recommendations for Tumor Marker Prognostic Studies (REMARK) guidelines, we included studies that met all of the following criteria: (1) written in English; (2) reported quantitative outcomes from prognostic association studies of tumor and CD147/EMMPRIN; (3) described outcomes as overall survival (OS), disease-specific survival (DSS), progression-free survival (PFS), metastasis-free survival (MFS) or recurrence-free survival (RFS), depending upon the study; (4) had a minimum of 40 case numbers describing prognosis; (5) provided a detailed protocol, including the source of raw materials, methodology, quantification methods, and scoring criteria; (6) precisely defined the time-to-event outcome, time to follow-up, and the median follow-up time; and (8) data were presented as the estimated hazard ratios (HRs) with 95% confidence intervals (CIs) or in the case where HRs or 95% CIs were not reported directly, a calculation was used to determine if the conditions of the study were suitable for inclusion68. Multivariate analyses were used for statistical analysis biomarkers that had independent prognostic factors for cancers after adjusting for one or more additional standard clinical prognostic variables like age, pathology, stage, grade, lymphatic metastasis or other biological marker variables. Studies were excluded if they were case reports, case-only studies, letters, reviews, reported insufficient data, lacked statistical analysis, combined with other factors, or were duplicate studies. All studies were independently reviewed by two authors, and in a case of conflict a third author resolved the issue after thorough discussion.
Data collection and analysis
We assessed heterogeneity using the Chi2 test and I2 test69. If heterogeneity was present, meta-regression was used to determine the source. We combined data from different trials using a fixed-effect model when there was no significant heterogeneity in populations (I2 < 50%) and a random-effect model when there was considerable heterogeneity. If heterogeneity was present, meta-regression was used to determine the source. Variables were synthesized using HR/OR. By convention, an overall HR (OR) > 1 with a 95% CI implied a poor outcome (high risk) for the group with either positive or negative biomarker expression. The high HR value corresponded with poor survival. To evaluate the effects of individual studies on the pooled HR estimates, we performed a sensitivity analysis omitting one study at a time. The statistical significance was set at 0.05. We used funnel plot asymmetry using Egger’s linear regression test and Begg’s rank correlation test to assess the publication bias. If both test results were inconsistent, Nonparametric Trim and Fill method was used to verify the results70. A P value of <0.05 suggested significant publication bias. All statistical analyses were performed using STATA 12.0 (StataCorp, College Station, TX) statistical software.
Additional Information
How to cite this article: Xin, X. et al. CD147/EMMPRIN overexpression and prognosis in cancer: A systematic review and meta-analysis. Sci. Rep. 6, 32804; doi: 10.1038/srep32804 (2016).
Supplementary Material
Footnotes
Author Contributions X.Y.X., X.Q.Z., H.J.G. and H.B.W. conceived and designed the experiments; X.Y.X., X.Q.Z., H.J.G., M.L., H.M.T., Z.S.J., T.H., R.S. and H.B.W. performed the experiments; X.Y.X., X.Q.Z., H.J.G., H.M.T., Z.S.J. and H.B.W. analyzed the data; X.Y.X., X.Q.Z., H.J.G., M.L., T.H., R.S. and H.B.W. contributed resources to facilitate the analyses; X.Y.X. and H.B.W. wrote the paper.
References
- Huang P. et al. RNA interference targeting CD147 inhibits the proliferation, invasiveness, and metastatic activity of thyroid carcinoma cells by down-regulating glycolysis. Int J Clin Exp Pathol. 8, 309–318 (2015). [PMC free article] [PubMed] [Google Scholar]
- Grass G. D. & Toole B. P. How, with whom and when: an overview of CD147 mediated regulatory networks influencing matrix metalloproteinase activity. Biosci Rep. 24, 36(1) (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinheiro C. et al. Reprogramming energy metabolism and inducing angiogenesis: co-expression of monocarboxylate transporters with VEGF family members in cervical adenocarcinomas. BMC Cancer. 15, 835 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li S., Nguyen T. T. & Bonanno J. A. CD147 required for corneal endothelial lactate transport. Invest Ophthalmol Vis Sci. 55, 4673–81 (2014) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Als A. B. et al. Emmprin and Survivin Predict Response and Survival following Cisplatin-Containing Chemotherapy in Patients with Advanced Bladder Cancer. Clin Cancer Res. 13, 4407–4414 (2007). [DOI] [PubMed] [Google Scholar]
- Gao J. et al. Expression of CD147 and Lewis y antigen in ovarian cancer and their relationship to drug resistance. Med Oncol. 31, 920–928 (2014). [DOI] [PubMed] [Google Scholar]
- Zeng H. Z. et al. Expression of CD147 in advanced non-small cell lung cancer correlated with cisplatin-based chemotherapy resistance. Neoplasma. 58, 449–454 (2011). [DOI] [PubMed] [Google Scholar]
- Hao J. et al. In vitro and In vivo prostate cancer metastasis and chemoresistance can be modulated by expression of either CD44 or CD147. PLoS ONE. 7, e40716 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang C. et al. Association of increased ligand cyclophilin A and receptor CD147 with hypoxia, angiogenesis, metastasis and prognosis of tongue squamous cell carcinoma. Histopathology. 60, 793–803 (2012). [DOI] [PubMed] [Google Scholar]
- Reimers N. et al. Expression of Extracellular Matrix Metalloproteases Inducer on micrometastatic and primary mammary carcinoma cells. Clinical Cancer Research. 10, 3422–3428 (2004). [DOI] [PubMed] [Google Scholar]
- Li Y. et al. HAb18G (CD147), a cancer-associated biomarker and its role in cancer detection. Histopathology. 54, 677–687 (2009). [DOI] [PubMed] [Google Scholar]
- Liu F. et al. Expression of HAb18G is associated with tumor progression and prognosis of breast carcinoma. Breast Cancer Res Treat. 124, 677–688 (2010). [DOI] [PubMed] [Google Scholar]
- Zhao S. H. et al. Basigin-2 is the predominant basigin isoform that promotes tumor cell migration and invasion and correlates with poor prognosis in epithelial ovarian cancer. Journal of Translational Medicine. 11, 92–103 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Y. et al. The role of EMMPRIN expression in ovarian epithelial carcinomas. Cell Cycle. 17, 2899–2913 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monteiro L. S. et al. EMMPRIN Expression in Oral Squamous Cell Carcinomas: Correlation with Tumor Proliferation and Patient Survival. BioMed Research International. 1–9 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Futamura N. et al. EMMPRIN co-expressed with matrix metalloproteinases predicts poor prognosis in patients with osteosarcoma. Tumor Biol. 35, 5159–5165 (2014). [DOI] [PubMed] [Google Scholar]
- Lu Q., Lv G., Kim A., Ha J. M. & Kim S. Expression and clinical significance of extracellular matrix metalloproteinase inducer, EMMPRIN/CD147, in human osteosarcoma. Oncology Letters 5, 201–207 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bovenzi C. D. et al. Prognostic Indications of Elevated MCT4 and CD147 across Cancer Types: A Meta-Analysis. Biomed Res Int. 2015, 242437 (2015). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng H. C. et al. Upregulated EMMPRIN/CD147 might contribute to growth and angiogenesis of gastric carcinoma: a good marker for local invasionand prognosis. British Journal of Cancer. 95, 1371–1378 (2006). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ueda K. et al. Association of extracellular matrix metalloproteinase inducer in endometrial carcinoma with patient outcomes and clinicopathogenesis using monoclonal antibody 12C3. Oncology Reports. 17, 731–735 (2007). [PubMed] [Google Scholar]
- Zhang Q. et al. Expression of CD147 as a significantly unfavorable prognostic factor in hepatocellular carcinoma. European Journal of Cancer Prevention. 16, 196–202 (2007) [DOI] [PubMed] [Google Scholar]
- Sienel W. et al. Cellular localization of EMMPRIN predicts prognosis of patients with operable lung adenocarcinoma independent from MMP-2 and MMP-9. Modern Pathology. 21, 1130–1138 (2008). [DOI] [PubMed] [Google Scholar]
- Ju X. Z., Yang J. M., Zhou X. Y., Li Z. T. & Wu X. H. EMMPRIN Expression as a Prognostic Factor in Radiotherapy of Cervical Cancer. Clin Cancer Res. 14, 494–501 (2008). [DOI] [PubMed] [Google Scholar]
- Yang X. et al. Expression of EMMPRIN in adenoid cystic carcinoma of salivary glands: correlation with tumor progression and patients’ prognosis. Oral Oncology. 46, 755–760 (2010). [DOI] [PubMed] [Google Scholar]
- Zhong W. D. et al. Extracellular matrix metalloproteinase inducer expression has an impact on survival in human bladder cancer. Cancer Epidemiology. 34, 478–482 (2010). [DOI] [PubMed] [Google Scholar]
- Chu T., Chen X., Yu J., Xiao J. & Fu Z. Extracellular Matrix Metalloproteinase Inducer is a Negative Prognostic Factor of Pediatric Medulloblastoma. Pathol. Oncol. Res. 17, 705–711 (2011). [DOI] [PubMed] [Google Scholar]
- Xue Y. J., Lu Q. & Sun Z. X. CD147 overexpression is a prognostic factor and a potential therapeutic target in bladder cancer. Med Oncol. 28, 1363–1372 (2011). [DOI] [PubMed] [Google Scholar]
- Zhu S. et al. Clinical Impact of HAb18G/CD147 Expression in Esophageal Squamous Cell Carcinoma. Dig Dis Sci. 56, 3569–3576 (2011). [DOI] [PubMed] [Google Scholar]
- Zhong W. D. et al. Expression of CD147 is associated with prostate cancer progression. Int. J. Cancer. 130, 300–308 (2012). [DOI] [PubMed] [Google Scholar]
- Bi X. C. et al. Extracellular matrix metalloproteinase inducer: a novel poor prognostic marker for human seminomas. Clin Transl Oncol. 14, 190–196 (2012). [DOI] [PubMed] [Google Scholar]
- Boye K. et al. EMMPRIN is associated with S100A4 and predicts patient outcome in colorectal cancer. British Journal of Cancer. 107, 667–674 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shou Z. X., Jin X. & Zhao Z. S. Upregulated Expression of ADAM17 Is a Prognostic Marker for Patients With Gastric Cancer. Ann Surg. 256, 1014–1022 (2012). [DOI] [PubMed] [Google Scholar]
- Stenzinger A. et al. High extracellular matrix metalloproteinase inducer/CD147expression is strongly and independently associated with poor prognosis in colorectal cancer. Human Pathology. 43, 1471–1481 (2012). [DOI] [PubMed] [Google Scholar]
- Liu Y. et al. CD147, MMP9 expression and clinical significance of basal-like breast cancer. Med Oncol. 30, 366 (2013). [DOI] [PubMed] [Google Scholar]
- Rabien A. et al. Renal cell neoplasias: reversion-inducing cysteine-rich protein with Kazal motifs discriminates tumor subtypes, while extracellular matrix metalloproteinase inducer indicates prognosis. Journal of Translational Medicine. 11, 258 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu X. Y., Lin N., Li Y. M., Zhi C. & Shen H. Expression of HAb18G/CD147 and its localization correlate with the progression and poor prognosis of non- small cell lung cancer. Pathology Research and Practice. 209, 345–352 (2013). [DOI] [PubMed] [Google Scholar]
- Yang M. et al. Prognostic significance of CD147 in patients with glioblastoma. J Neurooncol. 115, 19–26 (2013). [DOI] [PubMed] [Google Scholar]
- Chu D. et al. CD147 Expression in Human Gastric Cancer Is Associated with tumor recurrence and prognosis. PLOS ONE. 9, e101027 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Q. et al. ADAM17 is associated with EMMPRIN and predicts poor prognosis in patients with uterine cervical carcinoma. Tumor Biol. 35, 7575–7586 (2014). [DOI] [PubMed] [Google Scholar]
- Zhao S. et al. High expression of CD147 and MMP-9 is correlated with poor prognosis of triple-negative breast cancer (TNBC) patients. Med Oncol. 30, 335–349 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu S. et al. Expression and clinical implications of HAb18G/CD147 in hepatocellular carcinoma. Hepatology Research. 45, 97–106 (2015). [DOI] [PubMed] [Google Scholar]
- Li H. G. et al. Clinicopathological significance of expression of paxillin, syndecan-1 and EMMPRIN in hepatocellular carcinoma. World J Gastroenterol. 11, 1445–1451 (2005). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai W. C. et al. Association of EMMPRIN and fascin expression in renal cell carcinoma: correlation with clinicopathological parameters. World J Urol. 25, 73–80 (2007). [DOI] [PubMed] [Google Scholar]
- Hakuma N. et al. High Incidence of Extracellular Matrix Metalloproteinase Inducer Expression in Non-Small Cell Lung Cancers. Oncology. 72, 197–204 (2007). [DOI] [PubMed] [Google Scholar]
- Tsai W. C. et al. EMMPRIN and fascin overexpression associated with clinicopathologic parameters of pancreatobiliary adenocarcinoma in Chinese people. APMIS. 115, 929–938 (2007). [DOI] [PubMed] [Google Scholar]
- Wu W. et al. Prediction of prognosis in gallbladder carcinoma by CD147 and MMP-2 immunohistochemistry. Med Oncol. 26, 117–123 (2009). [DOI] [PubMed] [Google Scholar]
- Buergy D. et al. Prognostic Impact of Extracellular Matrix Metalloprotease Inducer: Immunohistochemical Analyses of Colorectal Tumors and Immunocytochemical Screening of Disseminated Tumor Cells in Bone Marrow From Patients With Gastrointestinal Cancer. Cancer. 115, 4667–4678 (2009). [DOI] [PubMed] [Google Scholar]
- Du Z. M. et al. Upregulation of caveolin-1 and CD147 expression in nasopharyngeal carcinoma enhanced tumor cell migration and correlated with poor prognosis of the patients. Int.J. Cancer. 125, 1832–1841 (2009). [DOI] [PubMed] [Google Scholar]
- Han Z. D. et al. Expression and Clinical Significance of CD147 in Genitourinary Carcinomas. Journal of Surgical Research. 160, 260–267 (2010). [DOI] [PubMed] [Google Scholar]
- Sweeny L. et al. CD147 Expression in Advanced Cutaneous Squamous Cell Carcinoma. J Cutan Pathol. 39, 603–609 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nakamura K., Kodama J., Hongo A. & Hiramatsu Y. Role of emmprin in endometrial cancer. BMC Cancer. 12, 191–201 (2012). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sato M. et al. EMMPRIN Promotes Angiogenesis, Proliferation, Invasion and Resistance to Sunitinib in Renal Cell Carcinoma, and Its Level Predicts Patient Outcome. PLOS ONE. 8, e74313 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai W. C. et al. EMMPRIN expression positively correlates with WHO grades of astrocytomas and meningiomas. J Neurooncol. 114, 281–290 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang Q. et al. Expression of COX-2, CD44v6 and CD147 and Relationship with Invasion and Lymph Node Metastasis in Hypopharyngeal Squamous Cell Carcinoma. PLOS ONE 8, e71048 (2013). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong X. et al. Overexpressions of RACK1 and CD147 Associated with Poor Prognosis in Stage T1 Pulmonary Adenocarcinoma. Ann Surg Oncol. 20, 1044–1052 (2013). [DOI] [PubMed] [Google Scholar]
- Choi J. W., Kim Y., Lee J. H. & Kim Y. S. Prognostic Significance of Lactate/Proton Symporters MCT1, MCT4, and Their Chaperone CD147 Expressions in Urothelial Carcinoma of the Bladder. Urology. 84, 245.e9e–245. e15 (2014). [DOI] [PubMed] [Google Scholar]
- Huang X. Q. et al. Co-expression of CD147 and GLUT-1 indicates radiation resistance and poor prognosis in cervical squamous cell carcinoma. Int J Clin Exp Pathol. 7, 1651–1666 (2014). [PMC free article] [PubMed] [Google Scholar]
- Pinheiro C. et al. Characterization of monocarboxylate transporters (MCTs) expression in soft tissue sarcomas: distinct prognostic impact of MCT1 sub-cellular localization. Journal of Translational Medicine. 12, 118–128 (2014). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Y., Choi J. W., Lee J. H. & Kim Y. S. Expression of lactate/H+ symporters MCT1 and MCT4 and their chaperone CD147 predicts tumor progression in clear cell renal cell carcinoma:immunohistochemical and The Cancer Genome Atlas data analyses. Human Pathology. 46, 104–112 (2015). [DOI] [PubMed] [Google Scholar]
- Liang Y. X. et al. CD147 and VEGF Expression in Advanced Renal Cell Carcinoma and Their Prognostic Value. Cancer Invest. 27, 788–93 (2009). [DOI] [PubMed] [Google Scholar]
- Yang H. & Chen B. CD147 in ovarian and other cancers. Int J Gynecol Cancer. 23, 2–8 (2013). [DOI] [PubMed] [Google Scholar]
- Fu J. et al. CD147 and VEGF co-expression predicts prognosis in patients with acute myeloid leukemia. pn J Clin Oncol. 40, 1046–52 (2010). [DOI] [PubMed] [Google Scholar]
- Zhou Q. et al. VEGF and EMMPRIN expression correlates with survival of patients with osteosarcoma. Surg Oncol. 20, 13–19 (2011). [DOI] [PubMed] [Google Scholar]
- Chen T. & Zhu J. Evaluation of EMMPRIN and MMP-2 in the prognosis of primary cutaneous malignant melanoma. Med Oncol. 27, 1185–1191 (2010). [DOI] [PubMed] [Google Scholar]
- Gu J. et al. Clinical implications and prognostic value of EMMPRIN/CD147 and MMP2 expression in pediatric gliomas. Eur J Pediatr. 168, 705–710 (2009). [DOI] [PubMed] [Google Scholar]
- Zhang C., Tu Z., Du S., Wang Y. & Wang Q. Expression of matrix metalloproteinase 2 and extracellular matrix metalloproteinase inducer are unfavorable postoperative prognostic factors in intrahepatic cholangiocarcinoma. Pathol Oncol Res. 16, 47–53 (2010). [DOI] [PubMed] [Google Scholar]
- Kuang Y. H. et al. RNA interference targeting the CD147 induces apoptosis of multi-drug resistant cancer cells related to XIAP depletion. Cancer Letters. 276, 189–195 (2009). [DOI] [PubMed] [Google Scholar]
- Parmar M. K., Torri V. & Stewart L. Extracting summary statistics to perform meta-analysis of the published literature for survival endpoints. Journal of the Statist Med. 17, 2815–2834 (1998). [DOI] [PubMed] [Google Scholar]
- Higgins J. P. & Thompson S. G. Quantifying heterogeneity in a meta-analysis. Stat Med. 15, 1539–1558 (2002). [DOI] [PubMed] [Google Scholar]
- Duval S. Publication Bias in Meta-Analysis: Prevention, Assessment and Adjustments (eds Rothstein H. R. et al.) 127–144 (John Wiley & Sons, 2005). [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.