Abstract
Objective:
To determine mean change in visual acuity, central corneal thickness and symptoms in patients with pseudophakic bullous keratopathy after treatment with corneal collagen crosslinking.
Methods:
This quasi experimental study was conducted at Armed Forces Institute of Ophthalmology, Rawalpindi, Pakistan from April 2015 to Nov 2015. A total of 24 eyes of 24 patients were included in the study. Visual symptoms were graded in five grades (Grade 1-5), Grade-1 being very mild with decreased vision only while patients with all five symptoms (decreased vision, foreign body sensations, pain, watering and photophobia) were graded as Grade-5. Corneal collagen cross linking using topical isotonic riboflavin followed by UVA radiations (3mW/cm2 for 10 minutes) was performed in all the patients. Visual acuity (VA), visual symptoms and central corneal thickness (CCT) were recorded before and 04 weeks after the treatment.
Results:
A total of 24 eyes of 24 patients (18 male and 6 females) underwent surgery. Age of the patients ranged from 55 to 75 years with mean age 65.83 + 3.89 years. Mean visual acuity was 2.09 + 0.23 before treatment while after treatment it was 2.13 + 0.22. Mean CCT as measured by optical pachymetry (Galilae G6) was 753.96 + 55.16 and 641+ 29.25 before and after surgery respectively. Improvement of clinical symptoms was seen in all the patients.
Conclusion:
Corneal collagen cross linking is a temporary but effective symptomatic treatment of pseudophakic bullous keratopathy.
KEY WORDS: CXL, Pseudophakic bullous keratopathy, corneal transplantation
INTRODUCTION
Pseudophakic bullous keratopathy (PBK) is an important, visually significant, long term complication after cataract surgery that can render the patient legally blind. It results from dysfunction and loss of corneal endothelial cells leading to corneal edema, corneal opacification and epithelial bullae formation. Incidence of bullous keratopathy is 1-2% in various parts of world.1-3 Patient usually present with decreased vision initially but later on there is intense discomfort, pain, watering, irritation, photophobia due to rupture of bullae and exposure of corneal nerves. Symptomatic patients are commonly managed with topical hypertonic saline, mild topical steroids and bandage contact lens. However, keratoplasty is the eventual surgical management for improving visual outcome in eyes with good visual potential and isolated corneal disorders. Corneal grafting is a costly procedure, not readily available for all the patient and it is not a good treatment option for those cases where there is guarded visual prognosis.4-6 In such cases various treatment modalities have been tried for symptomatic relief such as PTK (phototherapeutic keratectomy), conjunctival rotation or free flaps, puncturing anterior corneal stroma, and transplantation of amniotic membrane.7
Corneal collagen cross linking (CXL) with Riboflavin and ultraviolet A (UVA) radiations is photochemical process that was introduced by Seiler and Spoerl at university of Dresden for treatment of corneal ectatic disorders such as keratoconus and post LASIK ectasias.8 The proposed mechanism of action is that riboflavin absorbs UVA light which results in production of free oxygen redicals. These highly reactive oxygen redicals then induce cross linking of corneal stromal collagen and strengthen the cornea.9
Over the past few years, CXL has been used in various corneal disorders other than keratoconus such as non-healing corneal ulcer, PBK and Fuch`s endothelial dystrophy.10,11 However, there is no established evidence of effectiveness of CXL in these conditions. Some authors claim its benefit in non-healing ulcer and symptomatic PBK while others consider this treatment ineffective.12,13
The rationale of conducting this study is to observe the effect of CXL in patients with symptomatic PBK in our population because corneal grafting is not readily available and if at all possible, most of the patients cannot afford the cost.
METHODS
This Quasi experimental study was conducted at Armed Forces Institute of Ophthalmology, Rawalpindi, Pakistan from April 2015 to October 2015. A total of 24 eyes of 24 patients suffering from pseudophakic bullous keratopathy were included in the study. Age of the patients ranged from 55-75 years. Those patients who were asymptomatic, had history of trauma, herpetic eye disease, bullous keratopathy secondary to other causes like Fuch`s endothelial dystrophy, advanced glaucoma were excluded from the study. Informed written consent was taken and detailed clinical examination of all the patients fulfilling the inclusion criteria was performed. It included unaided visual acuity and slit lamp examination. Visual symptoms were graded in five grades (Grade 1-5), Grade-1 being very mild with decreased vision only while patients with all five symptoms (decreased vision, foreign body sensations, pain, watering and photophobia) were graded as Grade-5. CXL with isotonic riboflavin was performed on all the patients following standard protocol. Visual acuity (VA), visual symptoms and central corneal thickness (CCT) were recorded before and 04 weeks after the treatment.
Procedure
All the patients underwent surgery under topical anesthesia. CCT was measured before surgery with optical pachymetery (Galilae G4 and Reichert, Angeled probe pachymeter). Central corneal epithelium was removed with the help of sterile blunt spatula followed by instillation of riboflavin eye drops (1 drop every 2 minutes) for 30 minutes. UVA radiations were delivered using (Vario, CCL-365) for 10 minutes at power settings of 9mW/cm2. Bandage contact lens was placed at the end of procedure and patients were advised with topical moxifloxacin, nepafenac and cyclopentolate eye drops three times a day for 01 week. Patients were reviewed at day 1, after 02 weeks and then 04 weeks.
Statistical analysis
Statistical package for social sciences (SPSS 21.0) was used for statistical analysis. Continuous variables such as age, VA and CCT were described in terms of mean ± SD (standard deviation) and analyzed statistically by paired sample t test while grading of symptoms was analyzed by frequency distribution and Wilcoxon test to determine the significance level (p≤0.05).
RESULTS
A total of 24 eyes of 24 patients (18 male and 6 females) underwent surgery. Age of the patients ranged from 55 to 70 years with mean age 65.83 ± 3.89 years. Mean visual acuity was 2.09 ± 0.23 before treatment while after treatment it was 2.13 ± 0.22. Mean CCT as measured by optical pachymetry (Galilae G4) was 753.96 ± 55.16 and 641± 29.25 before and after surgery respectively (Table-I). The magnitude of induced change in visual acuity was statistically insignificant, while there was significant change in CCT (Table-II). Grading of clinical symptoms and their frequencies before and after treatment is shown in Table-III. None of the patient had complications such as corneal ulcer and persistent epithelial defect.
Table-I.
Mean and Standard deviation.
| N | Mean ± SD | |
|---|---|---|
| Age | 24 | 65.83±3.89 |
| Pre CXL Visual acuity | 24 | 2.09±0.23 |
| Pre CXL Central corneal thickness | 24 | 753.96±55.16 |
| Post CXL Visual acuity | 24 | 2.13±0.22 |
| Post CXL Central corneal thickness | 24 | 641±29.25 |
Table-II.
Induced change in CCT and VA.
| Pre treatment | Post treatment | Induced change | P value | |
|---|---|---|---|---|
| Visual Acuity | 2.09 ± 0.23 | 2.13 ± 0.22 | 0.038 ± 0.16 | 0.26 |
| Central corneal thickness | 753.96 ± 55.16 | 641± 29.25 | 112.75 ± 52.32 | 0.01 |
Table-III.
Grades of clinical symptoms before and after CXL.
| Grade 1 | Grade 2 | Grade 3 | Grade 4 | Grade 5 | |
|---|---|---|---|---|---|
| Pre CXL | 0 (0 %) | 0 (0 %) | 3 (12.5 %) | 8 (33.3%) | 13 (64.2%) |
| Post CXL | 16 (66.6%) | 8 (33.3%) | 0 (0%) | 0 (0%) | 0 (0%) |
Fig.1.
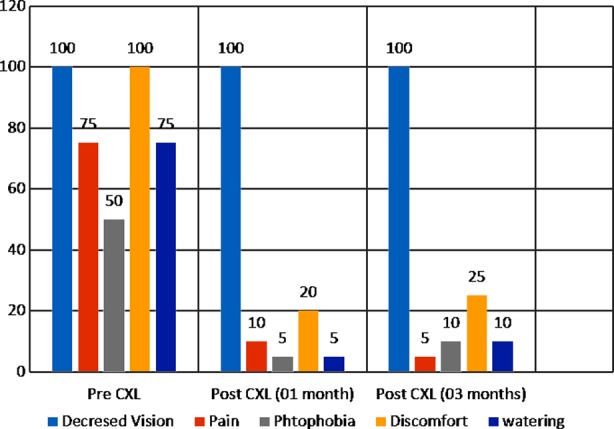
Percentage of symptoms in pre CXL and post CXL groups.
DISCUSSION
The role of CXL is well established in the treatment of keratoconus, however in recent years this modality has been tried in treatment of PBK. Wollensak and his colleagues observed the possible effectiveness of CXL in PBK and proposed the formation of chemical bonds between collagen fibrils that creates a mechanical barrier and reduce the edema.14,15 Various other studies also concluded the effectiveness of CXL in symptomatic treatment of PBK, however the effects are transient with recurrence of edema and bullae formation within few months.9,10,11,16,17
Despite using a different protocol with UVA radiations of 9mW/cm2 for 10 minutes instead of 3mW/cm2 for 30 minutes (Dresden protocol), we, in our study found out a remarkable and statistically significant improvement in the symptoms as well as CCT of patients at 01 month (Table II & III) which was also concluded by Wollensak et al. and Sharma N et al. in their studies.9,10,11 Some authors such as Ghanem et al. in their series of 14 patients and Arora et al. in 24 patients also found out a significant improvement in the visual acuity in addition to symptomatic relief.18,19 However, like Sharma et al, we could not find a statistically significant improvement in visual acuity and corneal clarity. The probable reason may be the severe visual loss and relatively advanced stage of disease at the time of presentation in our patients.
The transient effect of CXL in PBK has been claimed by almost all the authors in their studies. The primary reason for this is obviously the endothelial decompensation which is not catered for with CXL. Therefore, the persistent influx of aqueous subsequently overcome the strengthening effect of CXL within couple of months leading to corneal edema, increased thickness, bullae formation and recurrence of symptoms. To overcome this, various techniques are used to increase and prolong the effectiveness of CXL by using concurrent preoperative hypertonic glucose (40%) or glycerol (70%). Authors have concluded positive results with these modified techniques.10,20
Keratoplasty is the gold standard treatment for PBK, however, donor corneas are not readily available in our part of the world and patients usually have to wait for a period of about 8-12 months. Furthermore, patients who have good vision in the other eye are usually more concerned about the discomfort, pain and watering in the affected eye rather than decreased vision. Therefore, the effect of CXL on PBK which are claimed to be transient are nevertheless significantly effective as a temporary measure especially for patients awaiting definite treatment with corneal transplant.
We think our findings are important and comparable to other published literature, however, the long term effect of CXL on PBK and their subsequent effect on corneal grafting requires study on a larger cohort and a longer follow up.
Footnotes
Grant Support & Financial Disclosures: None.
Authors’ Contributions
MSK, IB conceived, designed and drafting the manuscript.
TS, AY, RI design and data collection.
MI did review and final approval of manuscript.
REFRENCES
- 1.Goncalves ED, Campos M, Paris F, Gomes JA, Farias CC. Bullous keratopathy: etiopathogenesis and treatment. Arq Bras Oftalmol. 2008;71(6 Suppl):61–64. doi: 10.1590/s0004-27492008000700012. [DOI] [PubMed] [Google Scholar]
- 2.Gomes JA, Haraguchi DK, Zambrano DU, Izquierdo Junior L, Cunha MC, de Freitas D. Anterior stromal puncture in the treatment of bullous keratopathy: six-month follow-up. Cornea. 2001;20(6):570–2. doi: 10.1097/00003226-200108000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Uchino Y, Goto E, Takano Y, Dogru M, Shinozaki N, Shimmura S, et al. Long-standing bullous keratopathy is associated with peripheral conjunctivalization and limbal deficiency. Ophthalmology. 2006;113(7):1098–1101. doi: 10.1016/j.ophtha.2006.01.034. [DOI] [PubMed] [Google Scholar]
- 4.Calix Netto MJ, Giustina ED GZ, Ramos Peccini RF, Nephew M, de Souza LB. Main indications for penetrating keratoplasty at a reference service in São Paulo (Sorocaba-SP, Brazil) Arch Ophthalmol. 2006;69(5):661–4. doi: 10.1590/s0004-27492006000500007. [DOI] [PubMed] [Google Scholar]
- 5.Pires RT, Tseng SC, Prabhasawat PV, Puangsricharern Maskin SL, Kim JC, et al. Amniotic membrane transplantation for symptomatic bullous keratopathy. Arch Ophthalmol. 1999;117(10):1291–1297. doi: 10.1001/archopht.117.10.1291. [DOI] [PubMed] [Google Scholar]
- 6.Rao GN, Aquavella JV, Goldberg SH, Berk SL. Pseudophakic bullous keratopathy. Relationship to preoperative corneal endothelial status. Ophthalmology. 1984;91(10):1135–1140. [PubMed] [Google Scholar]
- 7.Siu GD, Young AL, Jhanji V. Alternatives to corneal transplantation for the management of bullous keratopathy. Curr Opin Ophthalmol. 2014;25(4):347–352. doi: 10.1097/ICU.0000000000000062. doi:10.1097/ICU.0000000000000062. [DOI] [PubMed] [Google Scholar]
- 8.Spoerl E, Huhle M, Seiler T. Induction of cross-links in corneal tissue. Exp Eye Res. 1998;66(1):97–103. doi: 10.1006/exer.1997.0410. [DOI] [PubMed] [Google Scholar]
- 9.Wollensak G, Spoerl E, Seiler T. Riboflavin/ultraviolet-A-induced collagen cross-linking for the treatment of kertatoconus. Am J Ophthalmol. 2003;135:620–627. doi: 10.1016/s0002-9394(02)02220-1. [DOI] [PubMed] [Google Scholar]
- 10.Wollensak G, Aurich H, Wirbelauer C, Pham DT. Potential use of riboflavin/UVA cross-linking in bullous keratopathy. Ophthalmic Res. 2009;41:114–7. doi: 10.1159/000187630. doi:10.1159/000187630. [DOI] [PubMed] [Google Scholar]
- 11.Sharma N, Roy S, Maharana PK, Sehra SV, Sinha R, Tandon R, et al. Outcomes of corneal collagen crosslinking in pseudophakic bullous keratopathy. Cornea. 2014;33(3):243–6. doi: 10.1097/ICO.0000000000000004. doi:10.1097/ICO.0000000000000004. [DOI] [PubMed] [Google Scholar]
- 12.Krueger RR, Ramos-Esteban JC, Kanellopoulos AJ. Staged intrastromal delivery of riboflavin with UVA cross-linking in advanced bullous keratopathy: laboratory investigation and first clinical case. J Refract Surg. 2008;24(7):S730–6. doi: 10.3928/1081597X-20080901-17. doi:10.1155/2014/463905. [DOI] [PubMed] [Google Scholar]
- 13.Ucakhan OO, Saglik A. Outcome of two Corneal Collagen Crosslinking methods in Bullous Keratopathy due to Fuchs’ Endothelial Dystrophy. Case Rep Med. 2014;2014:463905. doi: 10.1155/2014/463905. doi:10.1155/2014/463905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wollensak G, Aurich H, Pham DT, Wirbelauer C. Hydration behavior of porcie cornea crossliked with riboflavin and ultraviolet A. J Cataract Refract Surg. 2007;33(3):516–21. doi: 10.1016/j.jcrs.2006.11.015. [DOI] [PubMed] [Google Scholar]
- 15.Cordeiro Barbosa MM, Barbosa JB, Jr, Hirai FE, Hofling-Lima AL. Effect of cross-linking on corneal thickness in patients with corneal edema. Cornea. 2010;29(6):613–7. doi: 10.1097/ICO.0b013e3181c296c2. doi:10.1097/ICO.0b013e3181c296c2. [DOI] [PubMed] [Google Scholar]
- 16.Ehlers N, Hjortdal J. Riboflavin-ultraviolet light induced cross-linking in endothelial decompensation. Acta Ophthalmol. 2008;86(5):549–51. doi: 10.1111/j.1600-0420.2007.01085.x. [DOI] [PubMed] [Google Scholar]
- 17.Bottós KM, Hofling-Lima AL, Barbosa MC, Barbosa JB, Jr, Dreyfuss JL, Schor P, et al. Effect of collagen cross-linking in stromal fibril organization in edematous human corneas. Cornea. 2010;29:789–93. doi: 10.1097/ICO.0b013e3181bd9f12. doi:10.1097/ICO.0b013e3181bd9f12. [DOI] [PubMed] [Google Scholar]
- 18.Arora R, Manudhane A, Saran RK, Goyal J, Goyal G, Gupta D. Role of corneal collagen cross-linking in pseudophakic bullous keratopathy: a clinicopathological study. Ophthalmology. 2013;120(12):2413–8. doi: 10.1016/j.ophtha.2013.07.038. doi:10.1016/j.ophtha.2014.06.004. [DOI] [PubMed] [Google Scholar]
- 19.Ghanem RC, Santhiago MR, Berti TB, Thomaz S, Netto MV. Collagen crosslinking with riboflavin and ultraviolet-A in eyes with pseudophakic bullous keratopathy. J Cataract Refract Surg. 2010;36(2):273–6. doi: 10.1016/j.jcrs.2009.07.041. doi:10.1016/j.jcrs.2009.07.041. [DOI] [PubMed] [Google Scholar]
- 20.Hafezi F, Dejica P, Majo F. Modified corneal collagen crosslinking reduces corneal oedema and diurnal visual fluctuations in Fuchs dystrophy. Br J Ophthalmol. 2010;94(5):660–661. doi: 10.1136/bjo.2009.162479. doi:10.1136/bjo.2009.162479s. [DOI] [PubMed] [Google Scholar]


